Abstract
Objectives: To examine whether maternal–child interaction during feedings was suboptimal in dyads in which the infant had gastroesophageal reflux disease (GERD) and to compare massage therapy to a nonmassage therapy sham treatment in improving the mother–child interaction in these dyads.
Design: In this randomized, controlled pilot study, infants received massage therapy (n=18) or a nonmassage touch/holding sham treatment (n=18). Mothers, data collectors, and the investigator who scored the feeding observations were blinded to group assignment.
Settings/Location: Dyads were recruited from pediatric care providers in the Denver metropolitan area and online advertisements at the University of Colorado. Treatments were given in the home of the dyad.
Participants: Healthy infants, born at 38–42 weeks gestational age, were 5–10 weeks of age at enrollment; had a score of at least 16 on the Infant Gastroesophageal Reflux Questionnaire-Revised; and were diagnosed with GERD by their pediatric provider. Mothers were English speaking and at least 18 years of age.
Interventions: Treatments were given for 30 minutes twice weekly for 6 weeks. A certified infant massage therapist administered massage, and a registered nurse or physical therapist experienced with infants administered the control treatment.
Outcome Measures: Maternal and infant scores on the Nursing Child Assessment of Feeding Scale (NCAFS).
Results: NCAFS scores were significantly lower than national norms. Small to moderately sized effects showing improvement in the massage group relative to the nonmassage group were seen for Sensitivity to Cues, Social-Emotional Growth Fostering, Cognitive Growth Fostering, and Clarity of Cues (Cohen d) and ranged from 0.24 to 0.56.
Conclusions: Mothers and infants with GERD experience significantly worse interactions than those without GERD. Massage given twice weekly by a professional trended toward improved interaction during feeding. Daily maternal administration of massage may have a positive effect on the relationship.
Introduction
Spitting and regurgitation are normal behaviors in young infants and are associated with gastroesophageal reflux (GER). GER typically occurs after meals when the lower esophageal sphincter that creates a barrier between the stomach and esophagus transiently relaxes and allows gastric contents to flow back into the esophagus.1 GER can become problematic in approximately 25% of infants, with symptoms of frequent regurgitation, irritability (crying and fussing), and feeding difficulties (refusal, coughing, choking, gagging) and is then considered gastroesophageal reflux disease (GERD).2–4
GERD most often resolves during the first year of life, but heightened irritability and feeding difficulty may severely tax the early mother–infant relationship. Mothers of infants with GERD reported that their infants were more demanding, recounted more feelings of anger and frustration, and perceived their children as more behaviorally problematic than other mothers.3 Early feeding problems are reported to persist into early childhood, accompanied by externalizing and internalizing problems.5,6
Feeding is an important social event between mothers and their infants. Young infants gaze at their mothers and smile and vocalize during feedings.7,8 Infants need to clearly signal when hungry and satiated.9 When mothers recognize and appropriately respond to infant cues and model changes in affect, infants learn to regulate emotions, develop trust, and form an emotional bond with the parent.10–12
Infant irritability during feedings may interfere with the amount taken during feeding, transmission of clear cues, or interaction with the mother and may result from discomfort from acid reflux. Reports that the frequently prescribed antireflux medications decrease acid but not other symptoms of GERD any more effectively than a placebo suggest a behavioral component to irritability and feeding difficulty.13–15 Maternal characteristics, such as depression, anxiety, or insecurity, also have been associated with feeding problems in the infant.16–19 Others have found negative life events, beliefs about feeding, and/or controlling (force-feeding), unresponsive, overstimulating, or unpredictable maternal behaviors to be more important.20–22
Maternal–infant interaction during feedings in young infants with GERD has not been investigated. A treatment that has potential to improve the relationship is massage. In massage therapy, rhythmic pressure and stroking is used to mechanically manipulate body tissues.23,24 When administered by a professional therapist 15 minutes twice a week for 6 weeks, infants receiving massage displayed longer periods of alertness, cried less, and were more sociable and more easily soothed than infants who experience rocking by the professional.25 In other studies, when mothers provided massage twice a day for 10–15 minutes for 4 weeks to 6 months, improved development, such as enhanced infant growth,26–31, decreased crying,32 and better sleep,33,34 compared with control groups were reported. Jing and colleagues26 also found superior fine motor cognitive, language, and social development at 6 months in infants receiving massage compared with control infants.
Research suggests that behaviors of infants with GERD (e.g., frequent regurgitation and irritability)2–4 and resultant maternal feelings of frustration and anger3 have the potential to severely affect the mother–infant relationship.5,6,10–12 The relationship may be most affected during feedings, although this has not been studied. Because of the potential serious negative effects of poor maternal-infant interaction10–12 and equivocal effects on irritability of antireflux medications,13–15 massage was investigated as a nonpharmaceutical intervention to improve infant well-being and improve interaction of the dyad during feedings.
Materials and Methods
Design
In this randomized, controlled pilot study, massage therapy was compared with a non–massage therapy sham treatment. Massage was administered by a professional as a first step in this investigation. Research hypotheses were as follows: In dyads in which the infants have symptoms of GERD, (1) maternal–child interaction during feedings will be suboptimal and (2) maternal–infant interaction will improve more after 6 weeks of massage therapy than after 6 weeks of nonmassage sham therapy.
Sampling plan and recruitment
Infant inclusion criteria were the following: (1) born at gestational age of 38–42 weeks, (2) age 6–10 weeks at enrollment, (3) score of at least 16 on the Infant Gastroesophageal Reflux Questionnaire-Revised,2 and (4) diagnosis of GERD by their pediatric provider. Maternal inclusion criteria were (1) English speaking and (2) at least 18 years of age. Infant exclusion criteria were as follows: (1) major surgery, (2) chronic illness other than GERD, (3) congenital anomaly, or (4) bilious or projectile vomiting or bloody stool.
Pediatric care providers referred infants on the basis of history and symptoms of frequent regurgitation, irritability during and/or between feedings and feeding difficulties (refusal, coughing, choking, gagging) and excluded other medical conditions (e.g., feeding allergy, pyloric stenosis, obstructions). In addition, the research team used the Infant Gastroesophageal Reflux Questionnaire-Revised (I-GERQ-R)2 to screen infants. Twelve questions address GERD symptoms that occurred during the past week. Scores range from 0 to 42 (most severe). The I-GERQ-R was validated in seven countries. Internal consistency reliability was 0.86–0.87 and test–retest reliability was 0.85. A cutoff score of 16 yielded a sensitivity of 0.65 and specificity of 1.0.
Recruitment
Infants were recruited from pediatric care providers and through online advertisements at the university campus. Human subjects approval was obtained and mothers signed informed consent forms before randomization. A computerized table of random numbers was used to assign participants to massage or nonmassage therapy. Opaque envelopes concealed group allocation. Mothers, research assistants who videotaped feedings and collected and entered other data, and the investigator who scored the feeding observations were blinded to group assignment.
Treatment procedures
The two therapists performing massage were certified and experienced with infants. They used the 15-minute massage protocol described by Field and colleagues.25 In their practice, the therapists performed infant massage for 30 minutes and thus lengthened the Field25 protocol by administering each of the six steps in the session (face and head, chest, abdomen, legs and feet, arms and hands, back) for 5 minutes. A graduate nursing student or a pediatric physical therapist experienced in infant care performed the nonmassage sham protocol for 30 minutes. After placing one hand over the other and using light, consistent pressure for 1 minute each on the infant's forehead, upper arms (one at a time), right and left chest, and center of abdomen; on each thigh and each shoulder; and the center of the infant's back, the therapist held the infant vertically on her shoulder for the remaining 20 minutes.
Therapists scheduled treatments in the late afternoon or evening twice a week for 6 weeks, 90 minutes after the last feeding. Treatments were administered in a quiet room in the infant's home without the presence of family members. All sessions were videotaped to monitor protocol adherence. Therapists placed infants on a warming pad covered with a blanket if the room seemed cool. They responded to smiles, eye contact, and infant vocalizations but avoided initiating verbalization. Mothers were reimbursed $40.00 at each assessment. They were informed of their infant's group assignment and were offered a massage demonstration after the infant's therapy sessions were completed.
Instruments
NCAST Nursing Child Assessment of Feeding Scale
The NCAST Nursing Child Assessment of Feeding Scale (NCAFS)9 is an observational tool widely used with infants from birth through 12 months of age. Four maternal subscales (Sensitivity to Cues, Response to Distress, Social-Emotional Growth Fostering, and Cognitive Growth Fostering) consist of a total of 50 items and contain observable behaviors that describe maternal caregiving during a feeding. Two infant subscales (Clarity of Cues, Responsiveness to Caregiver) consist of a total of 26 observable behaviors that describe infant ability to display clear feeding cues and respond to mother's overtures. Test–retest reliability from baseline to follow-up assessments was reported as 0.75 for the total maternal score and 0.51 for the infant score. Concurrent validity with Bradley and Caldwell's Home Observation for Measurement of the Environment scale was rs=0.48, 0.36, and 0.54 with the caregiver, child, and dyadic scores, respectively. The tool has been normed on 1914 feeding cases.9
Demographic data collection
A demographic form was used to record ethnicity, age, pregnancy, and birth history. Mothers completed a weekly diary in which they recorded infant medications and any additional treatments that they used to relieve infant GERD symptoms.
State Trait Anxiety Index
The State Trait Anxiety Index is a 40-item questionnaire used to assess the presence of temporary state anxiety and more stable trait anxiety.33
Edinburgh Post-natal Depression Scale
The Edinburgh Post-natal Depression Scale is a 10-item self-report scale (score range, 0–30) that was used to assess postpartum depression.34
Infant Behavior Questionnaire-Revised
The Infant Behavior Questionnaire-Revised (IBQ-R) is a 91-item parent-report questionnaire that was used to measure differences in infants' emotional reactivity and regulation. Questions are presented as a 7-point Likert scale. Although the IBQ-R measures 13 behaviors, only behaviors related to infant ability to focus attention (Low Intensity Pleasure, Cuddliness, Duration of Orienting, Soothability) were analyzed.35
Data collection
A research assistant videotaped a feeding in the infant's home, at baseline a week before treatments began and a week after the last therapy session. Mothers were instructed to feed the infant as usual. The research assistant was instructed to avoid initiating conversation with the mother during the feeding. Mothers completed the demographic questionnaire at baseline, the IBQ after the second therapy session in week 6, and the State Trait Anxiety Index and Edinburgh Post-natal Depression Scale at both collection times. The investigator scoring the feeding observations was a certified NCAFS instructor.
Statistical analysis
Statistical analyses were performed by using SAS software, version 9.2 (SAS Institute Inc., Cary, NC). Table 1 presents descriptive statistics as the mean±standard deviation for continuous measures or percentages for categorical responses. Independent sample t-tests or chi-square tests were used to examine the equivalence of baseline NCAFS scores and demographic characteristics between the massage and nonmassage groups. Mean NCAFS scores obtained in the current sample were compared with normative values9 by using independent sample t-tests to determine whether feeding scores in this GERD sample could be considered suboptimal. Feeding outcomes were examined by treatment group in a multilevel modeling framework as a linear mixed model. The parameter of interest in these models was the group-by-time interaction, which addressed the hypothesis of whether changes over time differed by group. Effect size estimates were calculated as Cohen d values on the basis of a comparison of the mean residualized change score between massage and nonmassage groups.
Table 1.
Comparison of Change in Nursing Child Assessment of Feeding Scale Scores from Baseline to 6 Weeks
| Characteristic | Group | Baseline | 6-week follow-up | p-Value | Effect sizea |
|---|---|---|---|---|---|
| Sensitivity to Cues | MT | 13.3±2.0 | 13.6±2.3 | .063 | 0.56 |
| NMT | 13.8±1.6 | 12.6±2.8 | |||
| Social-Emotional Growth Fostering | MT | 9.7±2.4 | 9.9±2.9 | .094 | 0.43 |
| NMT | 10.7±1.8 | 9.2±2.7 | |||
| Cognitive Growth Fostering | MT | 4.8±2.0 | 5.8±1.8 | .130 | 0.37 |
| NMT | 5.5±1.7 | 5.4±1.9 | |||
| Response to Distress | MT | 10.1±1.3 | 9.9±1.5 | .282 | −0.18 |
| NMT | 9.4±2.0 | 9.9±1.3 | |||
| Response to Caregiver | MT | 5.0±2.0 | 5.6±2.2 | .121 | 0.24 |
| NMT | 6.4±1.8 | 5.6±2.8 | |||
| Clarity of Cues | MT | 9.7±2.8 | 10.6±3.4 | .471 | 0.02 |
| NMT | 10.9±2.5 | 10.8±3.5 |
Values expressed with a plus/minus sign are the mean±standard deviation. Subscales were continuous measures.
Effect size calculated as Cohen d value on the basis of on the mean residualized change score in massage therapy versus nonmassage therapy groups.
MT, massage therapy; NMT, nonmassage therapy.
Results
Participants characteristics
Of 70 dyads referred to the study, 21 were randomly assigned to the massage group and 22 to the nonmassage group. Twenty-seven did not enroll because they wanted to be in the room during therapy or did not want to complete the diaries. Three from the massage group withdrew because of moving out of state or family issues. Four withdrew from the nonmassage group because of family illness, moving, or dislike of the study. The final study groups consisted of 18 dyads in the massage groups and 18 dyads in the nonmassage group.
The treatment groups did not differ at baseline in terms of demographic characteristics or background variables (e.g., infant sex; ethnicity; presence of birth complications; birth weight; baseline I-GERQ-R score; Apgar score; maternal or paternal education; and maternal, paternal, and infant age). NCAFS scores also did not differ between groups at baseline, with the exception of the Responsiveness to Caregiver subscale, for which those in the nonmassage group scored higher at baseline than those in the massage group. All NCAFS analyses considered change from baseline to week 6, so this baseline difference was explicitly addressed in the statistical modeling.
Infant age ranged from 4 to12 weeks and averaged 7±2 weeks for the first feeding observation and 15±2 weeks at the last observation, with a range of 11–20 weeks. Infant age was unrelated to NCAFS scores (all p>.26). Twenty-three infants (64%) were male and 20 (56%) were non-Hispanic white. The I-GERQ-R score ranged from 16 to 29, with a mean of 23±4. Ninety-one percent of the infants were receiving antireflux medication, and results were the same when analyses were limited to those taking medication. Mean age of mothers and fathers was 31±2 and 32±6 years, respectively. Twenty-eight mothers (78%) and 22 fathers (61%) had completed college or graduate school. Only one father was not involved with the family. Most mothers positioned their infants upright during sleeping, holding, or feeding; reduced dairy, caffeine, and spices in their diet if breast-feeding; or thickened infant feeding with cereal. Two mothers (one in each group) took their infant to a chiropractor. Overall, 44.4% of infants were breast-fed and 55.6% were bottle-fed. Feeding type was not significantly related to NCAFS scores (all p>.12) and did not influence intervention response.
Trait anxiety ranged from 20 to 53 (mean, 34±9) while state anxiety ranged from 20 to 55 (mean, 32±9). Mean depression score was 5.6±4 and ranged from 0 to 16. No significant correlations were observed among NCAFS outcomes with state or trait anxiety, depression, or the temperament subscales of the IBQ, indicating ability to focus attention (of 42 correlations, all p>.12).
Hypothesis 1: In dyads in which the infants have symptoms of GERD, maternal–child interaction during feedings will be suboptimal.
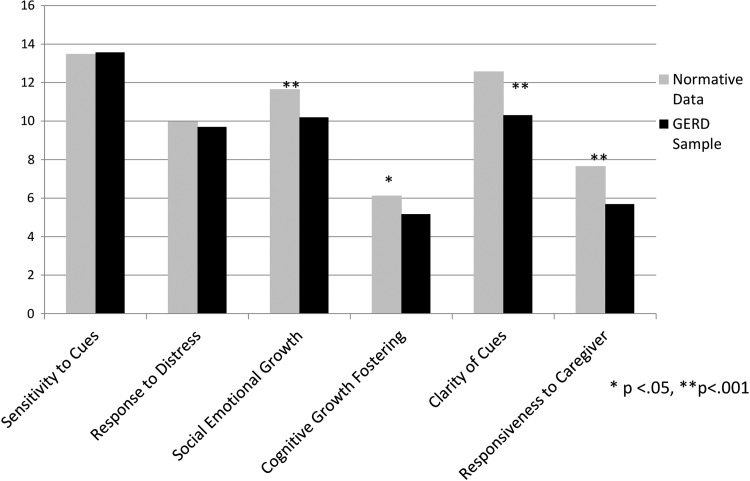
Figure 1 compares mean scores of NCAFS national norms9 and baseline scores of dyads in this study. The participants in this study were highly educated, so the normative data were from highly educated mothers (defined as having at least high school completion).9 Scores from the GERD sample were significantly lower than national normative values for Social Emotional Growth Fostering (p<.001), Cognitive Growth Fostering (p<.05), Clarity of Cues (p<.001), and Responsiveness to Caregiver (p<.001). These findings are the first to identify suboptimal maternal infant interaction during feedings in GERD dyads.
FIG. 1.
Comparison of baseline NCAST feedings scores between normative and gastroesophageal reflux disease (GERD) samples.
Hypothesis 2: Maternal–infant interaction will improve more after 6 weeks of massage therapy than after 6 weeks of nonmassage sham therapy.
Table 1 shows the means and standard deviations by condition at baseline and 6 weeks for the six NCAFS subscales and presents the p-value capturing group differences in change over time and corresponding effect size. No significant differences were identified between massage and nonmassage treated dyads. Scores for Sensitivity to Cues (p=.06) and Social-Emotional Growth Fostering (p=.09) trended toward increasing in the massage group and decreasing in the nonmassage group. Given the small sample size for this pilot study, it is more meaningful to examine the effect sizes associated with the change than to assess the significance level. Effect sizes were small to moderate (ranging from d=0.24 to d=0.56) and in the expected direction favoring the massage group for Sensitivity to Cues, Social-Emotional Growth Fostering, Cognitive Growth Fostering, and Response to Caregiver. Effect size for Clarity of Cues was essentially zero, and it was small and in an unintended direction for Response to Distress (d=−0.18).
Exploratory analyses were conducted on caregiver and infant NCAFS total scores as a secondary approach toward examining effects of massage. Although groups did not differ significantly, 60% of mothers in the massage group compared with 28.6% of mothers in the nonmassage group improved their total NCAFS score; for infant scores, these values were 50% and 53%, respectively. Scores of massage and nonmassage groups were separated and compared with the national NCAFS values. Maternal total score for the massage group was significantly lower than the highly educated norm at baseline (p=.026), but not after the intervention (p=.22), while the score for the nonmassage group did not differ from the highly educated norms at baseline (p=.24) but was lower after the intervention (p=.008). Infant scores were lower than national norms at both time points and across both groups.
Discussion
Our results show for the first time that mothers and infants with GERD experience suboptimal feeding interactions when compared with national norms. Although several studies have examined the effect of GERD on infant growth, no previous study has prospectively addressed this critical measure of mother–infant interactions. These findings support studies directed at understanding contributive factors and the beneficial aspects of treatment of GERD. In this regard, our findings showed that a limited trial of massage treatment in infants with GERD did not significantly change NCAFS scores but did begin to improve maternal–infant interaction. These results are particularly important in light of our recent findings that indicate massage treatment can reduce systemic infant cortisol levels, a measure of infant stress.36
Maternal caregiving scores in the NCAFS subscales of Sensitivity and Response to Distress items equaled national norms.9 These scores indicate that the mothers positioned their infants appropriately for feedings and responded to infant cues of hunger and satiation. Mothers of infants with GERD also responded adequately to their infants' distress behaviors during the feeding by stopping the feeding, changing position, or making soothing verbal vocalizations. However, as a group, mothers did not engage in eye contact to actively communicate with their infants or smile at their infants at the same level as the normative sample. Infants neither attempted to engage their mothers in interaction except by showing distress, nor displayed clear feeding cues relative to the national sample.
The lack of interaction and/or the lack of the infant's receiving the mother's interaction attempts are similar to the interaction style seen in dyads when mothers have symptoms of depression.16–19,37 Neither depression nor anxiety was associated with feeding scores in this study, however. Examining maternal feelings during feedings was beyond the scope of this study, but mothers may have felt rejected by their infant's nonresponsiveness or had preconceived beliefs about feeding.20–22 The suboptimal interaction pattern found in these infants may contribute to the reports of maternal anger and frustration with their infants with GERD and subsequent perception of childhood behavior problems.3,5,6 Whatever the reason, lack of regulation from the infant's caregiver can disrupt subsequent engagement with their mothers and others.37 Negative effects of the nonresponsive interactional style has been reported to persist from infancy to adolescence as children display limited affective expression, negative affect, chronic illness, intense negative feeding interactions, school anxiety, conduct difficulties, and hyperactive behavior.38–42
Maternal scores in the massage group increased marginally even though mothers were blind to group assignment of their infants and did not perform massage. In other research, massage therapy provided by professionals was reported to improve infant behavior in areas such as alertness, irritability, and sociability25 that may enhance maternal–infant interaction during feedings. Infant scores in this study were not significantly different from scores in the nonmassage group but were slightly higher after the intervention (Table 1). It is possible that even this slight improvement in infant responsiveness helped mothers to become more interactive. Findings of other studies have shown enhanced developmental outcomes in infants massaged daily by their mothers,26–32 indicating the feasibility and value of maternal adminstration of massage.
It is concerning that maternal scores in the nonmassage group decreased; this finding suggests that an effective intervention is needed for infants with GERD. Maternal interaction improved significantly in studies in which mothers considered to be high risk administered massage and were taught to recognize the cues of their infant for adaptation of the massage.43–45 In this study, massage as a touch therapy was assessed, so interaction between therapist and infant were kept to a minimum. Massage was given only twice a week. Future research in which mothers administer daily massage, interact with their infant, and adapt massage on the basis of their infant's behaviors may more positively influence maternal–infant interaction during massage and in other venues, including feedings. This merits investigation.
This study had some limitations. It was a pilot study, with a small sample of highly educated and intact families. It is unknown how other mothers with lower education and weaker family structure would interact during feedings and respond to massage. Significance may have been found in a larger sample. The fact that the infants in the control group received 10 minutes of concentrated touch plus holding for 20 minutes may have reduced the difference between groups as both massage and nonmassage interventions involved touch. Although each infant received their treatments from the same therapist, more than one therapist provided treatment for each group. A standardized protocol was followed for both the massage and sham treatment. All treatments were videotaped, and the project director and two research assistants watched the videotapes to ensure consistency. Nevertheless, subtle differences in therapist demeanor or touch could have influenced findings. Because of the small number of infants treated by each of the therapists, statistical analysis for this problem was not feasible. Feedings were observed only at baseline and after 6 weeks of treatment. More frequent assessments would have provided a more accurate evaluation of change over time. Maternal feelings during feedings were not explored; this would be important to include in future research, using both quantitative and qualitative designs.
The strength of this study is the focus on the feeding interaction in infants with GERD and their mothers that has been an understudied but potentially important area in this population. Massage given by a professional had marginal influence in improving the dyad interaction during feeding, especially in the mother. Maternal administration of massage may have more impact on the relationship than massage given by a professional therapist.
Disclosure Statement
Glenn T. Furuta served as a consultant to Receptos and Pfizer.
References
- 1.Vandenplas Y, Salvatore S, Hauser B. The diagnosis and management of gastro-oesophageal reflux in infants. Early Hum Devel 2005;8:1011–1124 [DOI] [PubMed] [Google Scholar]
- 2.Kleinman L, Rothman M, Strauss R, et al. The infant gastroesophageal reflux questionnaire revised: development and validation as an evaluative instrument. Clin Gastroenterol Hepatol 2006;4:588–596 [DOI] [PubMed] [Google Scholar]
- 3.Mathisen B, Worrall L, Masel J, et al. Feeding problems in infants with gastro-oesophageal reflux disease: a controlled study. J Paediatr Child Health, 1999;35:163–169 [DOI] [PubMed] [Google Scholar]
- 4.Sherman PM, Hassall E, Fagundes-Neto U, et al. A global, evidence-based consensus on the definition of gastroesophageal reflux disease in the pediatric population. Am J Gastroenterol 2009;104:1278–1295 [DOI] [PubMed] [Google Scholar]
- 5.McDermott BM, Mamun AA, Najman JM, et al. Preschool children perceived by mothers as irregular eaters: physical and psychosocial predictors from a birth cohort study. J Dev Behav Pediatr 2008;29:197–205 [DOI] [PubMed] [Google Scholar]
- 6.Ostberg M, Hagelin E. Feeding and sleeping problems in infancy—a follow-up at early school age. Child Care Health Dev 2010;37:11–25 [DOI] [PubMed] [Google Scholar]
- 7.Henning A, Striano T, Lieven EVM. Maternal speech to infants at 1 and 3 months of age. Infant Behav Dev 2005;28:519–536 [Google Scholar]
- 8.Lumeng JC, Patil N, Blass EM. Social influences on formula intake via suckling in 7 to 14-week-old-infants. Dev Psychobiol 2007;49:351–361 [DOI] [PubMed] [Google Scholar]
- 9.Sumner G, Spietz A. Caregiver/Parent-Child Interaction Feeding Manual. Seattle, WA: NCAST, 1996 [Google Scholar]
- 10.Black MM, Aboud FE. Responsive feeding is embedded in a theoretical framework of responsive parenting. J Nutr 2011;141:490–494 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Crockenberg SE, Leerkes EM, Barrig JPS. Predicting aggressive behavior in the third year from infants reactivity and regulation as moderated by maternal behavior. Dev Psychopathol 2008;20:37–54 [DOI] [PubMed] [Google Scholar]
- 12.Kochanska G, Woodard J, Kim S, et al. Positive socialization mechanisms in secure and insecure parent-child dyads: two longitudinal studies. J Child Psychol Psychiatry 2010;51:998–1009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jordan B, Heine RG, Meehan M, et al. Effect of antireflux medication, placebo and infant mental health intervention on persistent crying: a randomized clinical trial. J Paediatr Child Health 2006;42:49–58 [DOI] [PubMed] [Google Scholar]
- 14.Moore DJ, Tao BS, Lines DR, et al. Double-blind placebo-controlled trial of omeprazole in irritable infants with gastroesophageal reflux. J Pediatr 2003;143:219–223 [DOI] [PubMed] [Google Scholar]
- 15.Neu M, Corwin E, Lareau SC, Marchegianni-Howard C. A review of nonsurgical treatment for the symptom of irritability in infants with GERD. J Spec Pediatr Nurs 2012;17:177–192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Denis CL, McQueen K. Does maternal postpartum depressive symptomatology influence infant feeding outcomes? Acta Paediatr 2007;96:590–594 [DOI] [PubMed] [Google Scholar]
- 17.Douglas J. Behavioral approaches to the assessment and management of feeding problems in young children. In: Southall A, Schwartz A, eds. Feeding Problems in Children. Oxford, UK: Radcliffe Medical Press, 2010 [Google Scholar]
- 18.Karacetin G, Demir T, Erkan T, et al. Maternal psychpathology and psychomotor development of children with GERD. J Pediatr Gastroenterol Nutri 2011;53:380–385 [DOI] [PubMed] [Google Scholar]
- 19.Boyd RC, Zayas LH, McKee MD. Mother-infant interaction, life events and prenatal and postpartum depressive symptoms among urban minority women in primary care. Matern Child Health J 2006;10:139–148 [DOI] [PubMed] [Google Scholar]
- 20.Bryant-Waugh R, Markham L, Kriepe RE, Walsh BT. Feeding and eating disorders in childhood. Int J Eat Disorder 2010;43:98–111 [DOI] [PubMed] [Google Scholar]
- 21.Farrow C, Blisssett J. Maternal cognitions, psychopathologic symptoms, and infant temperament as predictors of early infant feeding problems: a longitudinal study. Int J Eat Disorder 2006;39:128–134 [DOI] [PubMed] [Google Scholar]
- 22.Sirvinskiene G, Zemaitiene N, Zaborskis A, et al. Infant difficult behaviors in the context of perinatal biomedical conditions and early child environment. BMC Pediatrics 2012;12:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cafarelli E, Flint F. The role of massage in preparation for and recovery from exercise. Sport Med 1992;14:19. [DOI] [PubMed] [Google Scholar]
- 24.Field T, Diego M, Hernandez-Reif Moderate pressure is essential for massage therapy effects. Int J Neurosci 2010;120:381–385 [DOI] [PubMed] [Google Scholar]
- 25.Field T, Grizzle N, Scafidi F, et al. Massage therapy for infants of depressed mothers. Infant Behav Dev 1996;19:107–112 [Google Scholar]
- 26.Jing J, Li X, Feng L, et al. Massage and motion training for growth and development of infants. World J Pediatr 2007;3:295–299 [Google Scholar]
- 27.Kim TI, Shin YH, White-Traut AC. Multisensory intervention improves physical growth and illness rates in Korean orphaned newborn infants. Res Nurs Health 2003;2:424–433 [DOI] [PubMed] [Google Scholar]
- 28.Liu C, Liu J, Lin X. Effects of touch on growth and mentality development in normal infants. Chin Med J 2001;81:1420–1423 [PubMed] [Google Scholar]
- 29.Narenji F, Rosbahany N. The effects of massage therapy on weight gain and sleep behaviors in infants. J Semnan Univ Med Sci (Koomesh) 2008;9:279–284 [Google Scholar]
- 30.Serano MS, Doren FM, Wilson L. Teaching Chilean mothers to massage their full-term infants: effects on maternal breast-feeding and infant weight gain at age 2 and 4 months. J Perinat Neonatal Nurs 2010;24:172–181 [DOI] [PubMed] [Google Scholar]
- 31.Xua LS, Qing GR, Ye MY. Study of touch intervention on infant sleep disorder. J Nurs Contin Educ 2004;19:973–976 [Google Scholar]
- 32.Ferber SG, Laudon M, Kuint J, et al. Massage therapy by mothers enhances the adjustment of circadian rhythms to the nocturnal period in full-term infants. Devel Behav Pediatr 2002;23:410–415 [DOI] [PubMed] [Google Scholar]
- 33.Spielberger CD. State-Trait Anxiety Inventory Manual. Redwood City, CA: Mind Garden, 1983 [Google Scholar]
- 34.Murray L, Carothers AD. The validation of the Edinburgh Post-Natal Depression Scale on a community sample. Br J Psychiatry 1990;157:288–290 [DOI] [PubMed] [Google Scholar]
- 35.Gartstein MA, Rothbart MK. Studying infant temperament via the Revised Infant Behavior Questionnaire. Infant Behav Dev 2003;26:64–86 [Google Scholar]
- 36.Neu M, Pan Z, Workman R, et al. Benefits of massage therapy for infants with symptoms of gastroesophageal reflux disease. J Biol Res Nurs 2013December30. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 37.Tronick E, Reck C. Infants of depressed mothers. Harvard Rev Psychiatry, 2009;17:147–156 [DOI] [PubMed] [Google Scholar]
- 38.Essex MJ, Klein MH, Miech R, Smider NA. Timing of initial exposure to maternal major depression and children's mental health symptoms in kindergarten. Br J Psychiatry 2001;179:151–156 [DOI] [PubMed] [Google Scholar]
- 39.Hanington L, Ramchandani P, Stein A. Parental depression and child temperament: assessing child to parent effects in a longitudinal population study. Infant Behav Dev 2010;33:88–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Landry SH, Smith KE, Swank PR. Responsive parenting: establishing early foundations for social, communication, and independent problem-solving skills. Dev Psychol 2006;42:627–642 [DOI] [PubMed] [Google Scholar]
- 41.Reck C, Hunt A, Fuchs T, et al. Interactive regulation of affect in postpartum depressed mothers and their infants: an overview. Psychopathology 2004;37:272–280 [DOI] [PubMed] [Google Scholar]
- 42.Tikotzky L, Chambers AS, Gaylor E, Manber R. Maternal sleep and depressive symptoms: links with infant negative affectivity. Infant Behav Dev 2010;33:605–612 [DOI] [PubMed] [Google Scholar]
- 43.O'Higgins M, St. James Roberts I, Glover V. Postnatal depression and mother and infant outcomes after infants massage. J Affect Disord 2008;109:189–192 [DOI] [PubMed] [Google Scholar]
- 44.Onozawa K, Glover V, Adams D, et al. Infant massage improves mother-infant interaction for mothers with postnatal depression. J Affect Dis 2001;63:201–207 [DOI] [PubMed] [Google Scholar]
- 45.Oswalt K, Biasani F. Effects of infant massage on HIV-infected mothers and their infants. J Spec Pediatr Nurs 2011;16:169–178 [DOI] [PubMed] [Google Scholar]