Abstract
Background.
Depressive symptoms are predictive of multiple degenerative diseases in older age adults. However, the association of depressive symptoms with onset and progression of disability have not been studied.
Methods.
In a cohort of community-dwelling, older black and white adults, 5,446 initially nondisabled subjects were followed annually for disability between 2000 and 2008. Depressive symptoms were assessed at baseline using a summary measure of 10-item version of the Center for Epidemiologic Survey-Depressive symptoms scale. The disability outcome was based on a summary measure of 13 basic and instrumental activities of daily living, and analyzed using a two-part regression model for onset and progression of disability.
Results.
During follow-up, 44% of blacks and 35% of whites reported onset of disability. After adjusting for confounders, depressive symptoms were associated with increased odds of disability onset in blacks (odds ratio = 1.12, 95% confidence interval, 1.07–1.18) and whites (odds ratio = 1.21, 95% confidence interval, 1.08–1.36). The odds of disability onset associated with depressive symptoms also increased significantly over time in whites (odds ratio = 1.06, 95% confidence interval, 1.04–1.09), but not in blacks. In addition, depressive symptoms were associated with an increasing rate of progression of disability in whites (rate ratio = 1.08, 95% confidence interval, 1.06–1.09), but not in blacks.
Conclusions.
Depressive symptoms increased the risk of onset of disability in blacks and whites. This risk tended to increase over time only among whites. A similar race-specific pattern was observed for time-dependent changes due to depressive symptoms in the rate of progression in disability after onset.
Key Words: Activities of daily living, Instrumental activities of daily living, Onset of disability, Progression of disability, Racial/Ethnic differences, Depressive symptoms.
Disability represents the impact of multiple comorbid conditions on a person’s ability to maintain essential activities of daily living (1,2). This impact can be understood in terms of two distinguishable mechanisms. The first mechanism emphasizes the need to maintain of the ability to live in the community independently and to perform basic self-care tasks (3,4). The second approach focuses on late-life disability as a process that results from deteriorating functional abilities due to the progression of underlying chronic disease processes (5,6). Hence, disability can be described in terms of a gradual two-part process of onset and progression. Few studies have compared and contrasted this two-part process in relation to important determinants of disability in older adults.
A better understanding of the disability process has resulted in noninstitutionalized older adults being able to live longer and healthier lives (7). Despite general improvements in overall health among older adults, substantial differences in disability exist between blacks and whites (8,9). Most studies that have examined racial disparities in disability have tended to focus on differences in socioeconomic status (10–12); but even after matching on socioeconomic status, disparities often persist. Several psychological factors have been shown to increase the risk of disability in blacks and whites (13–15). One important psychological factor that may be related to racial differences in the disability process is depressive symptoms (16,17). Previous data suggest that the prevalence of depressive symptoms is higher among older blacks than whites (18,19) although other findings have not shown such racial differences (20,21). In addition, previous studies suggest that depressive symptoms may have a more adverse association with health outcomes among blacks relative to whites (22–25). In this study, we extend this work and test racial differences in the association of depressive symptoms on the onset and progression of disability. Although recent studies have used the two-part process characterization of disability to estimate the effects of race and socioeconomic status on onset and progression of activities of daily living (ADL) disability (26,27), no study, to our knowledge, has investigated the effect of depression on the onset and progression of disability in older blacks and whites.
Methods
Study Design and Participants
Data for this article comes from the Chicago Neighborhood and Disability Study. This is a study of neighborhood conditions and disability in older adults that is fully integrated within the Chicago Health and Aging (CHAP) parent study. CHAP is an ongoing, population-based, longitudinal study of Alzheimer’s disease and other common health conditions in older adults (28). The CHAP study includes in-person interviews that were conducted in the subjects’ homes in approximately 3-year cycles, with each subsequent cycle starting immediately after completion of the previous one. The Chicago Neighborhood and Disability Study was performed from 2000 through 2008 in three adjacent neighborhoods on the south side of Chicago. Of the 7,545 study subjects, 5,446 were not disabled and included in this study. The average age of study sample was 73.2 (standard deviation [SD] = 6.4) years with an average follow-up time of 6.8 (SD = 2.2) years. Disability data were collected as part of the CHAP in-home interviews conducted every 3 years and during annual telephone interviews conducted in intervening years.
Measure of Depressive Symptoms
Depressive symptoms were assessed using the 10-item version of the Center for Epidemiological Studies-Depressive symptoms (CES-D) scale. The 10-item form was developed as part of the Established Populations for the Epidemiologic Studies of the Elderly (EPESE) site in East Boston, and found to cover the same four dimensions as the original 20-item CES-D and to have acceptable reliability (29). In the CHAP data, this version of the CES-D has good internal consistency with an alpha coefficient of .75. Each item in this scale was scored as presence or absence of a symptom. A summary score was derived by adding the number of positive responses. For the purpose of this analysis, we used the baseline CES-D summary score as measure of depressive symptoms, with a range from 0 to 10 (maximum observed score of 10).
Measure of Disability
Disability was assessed based on 13 questions measuring disabilities in ADL and instrumental activities of daily living (IADL). Previous studies suggest that a combined ADL/IADL measure has higher reliability and less age-related bias than each measure individually (30). ADL disability was measured using six items assessing the need for help with or inability to perform basic ADLs, bathing, dressing, eating, showering, toileting, and getting out of bed to chair (31). IADL disability was measured using seven items assessing the degree of difficulty in using the phone, shopping for groceries, preparing meals, house-keeping, laundering, taking medication, and managing finances (32). Responses indicating disability in ADLs (need help or unable to do) or IADLs (at least some difficulty) were summed across tasks to create the outcome measure of ADL/IADL disability.
Race and Other Covariates
Covariates in our study included age at baseline (centered at age 75), gender, self-reported race, coded as black versus white (subjects who identified themselves as non-Hispanic blacks and non-Hispanic whites), education, coded as the number of years of formal schooling completed (centered at 12 years), standardized cognitive function, physical function, and body mass index (kilogram/square meter); and time-varying measure of total number of chronic health conditions (stroke, myocardial infarction, cancer, hypertension, diabetes, and hip fracture) as these comorbid conditions are closely associated with disability.
Statistical Analysis
Standard descriptive analyses were provided using means, standard deviations, and percentages for each variable. The ADL/IADL disability outcome variable was considered to represent a number of task disabilities, and therefore to follow a count (Poisson) distribution. We modeled changes in disability as a two-part process, with the first part representing onset and the second part as progression. Transition to onset of disability was modeled using a logit link function with binomial distribution, and progression was modeled using a log link function with Poisson distribution. Thus, the parameters of the logistic model can be interpreted as the change in odds ratio (OR) and the parameters of the log-linear model can be interpreted as the change in rate ratio (RR). Changes in onset and progression were analyzed using a two-part regression model, which were fitted stratified by race. We also fitted a model after combining data for blacks and whites to perform a formal test of racial differences in the association of depressive symptoms with either onset or progression of ADL/IADL disability. All models included depressive symptoms, time since baseline (time), age, gender, education, cognitive function, physical function, body mass index, number of chronic health conditions, and interaction of time with age and depressive symptoms. The interpretation for main effect of depressive symptoms, also referred to as marginal associations, is the underlying average OR for onset of ADL/IADL disability at any follow-up period because we excluded subjects disabled at baseline from our analysis. The interpretation for interaction of depressive symptoms and time, also referred to as longitudinal associations, is the average increase in OR for depressive symptoms for each additional year of follow-up.
The specific formulation of this two-part regression is as follows: For the first (onset) part, let y i be a vector of binary variables denoting the onset of ADL/IADL disability for the ith individual. The probability of onset of ADL/IADL given the random effect b i can be described using a binomial distribution of the form (33):
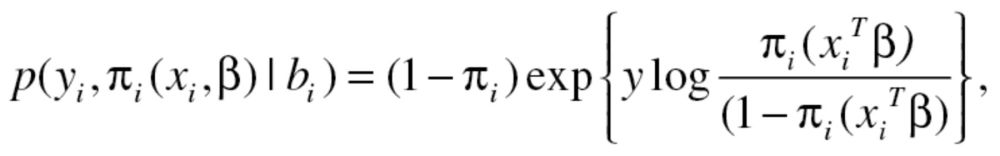 |
for y i = 0 and 1 and follows the natural exponential family with a canonical logit link function.
The second part analyzes change in number of ADL/IADL disabilities modeled using a log-linear (Poisson) model for count data (33). Given the random effect , the log-linear model for number of ADL/IADL disabilities (s
i) is obtained by:
, the log-linear model for number of ADL/IADL disabilities (s
i) is obtained by:
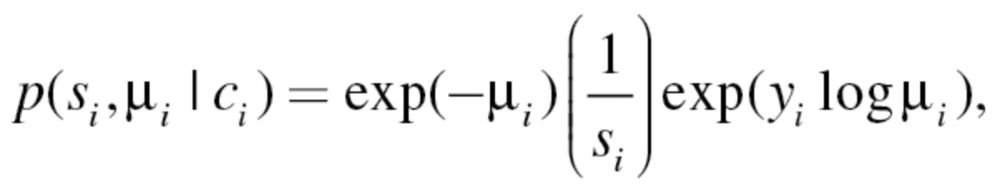 |
where s i is the number of ADL/IADL disabilities (range 0–13), and μi is the parameter of interest describing the progression of ADL/IADL disability scores over time.
The joint log-likelihood for the two-part model with random intercept is expressed as follows:
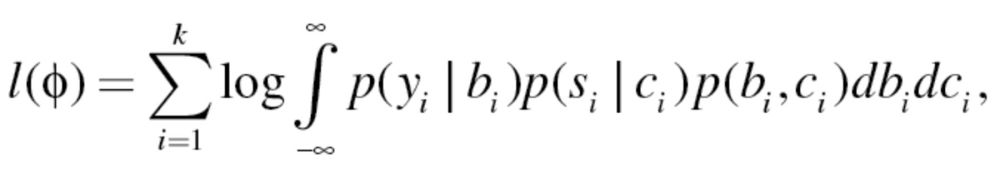 |
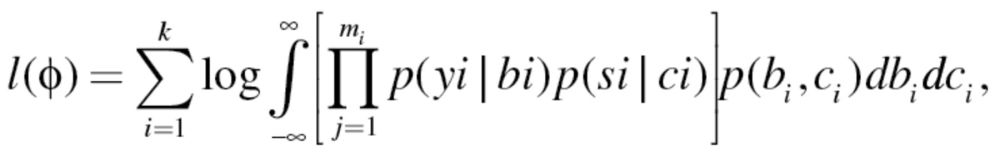 |
where p(y
i
|b
i) comes from a binomial distribution, p(s
i
|c
i) comes from a Poisson distribution, and m
i denotes the number of repeated assessments within the ith subject. The distribution of the random effects p(b
i
,c
i) is assumed to follow jointly normal distribution of the form N(0,Σ). Maximization of the likelihood with respect to the parameters 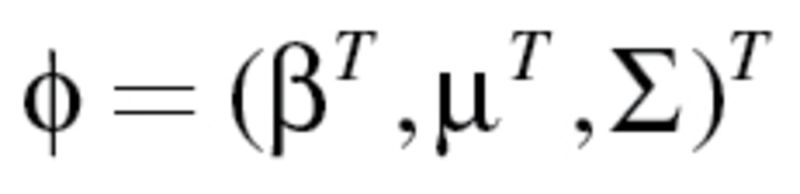 does not have a closed form solution. Hence, we used Laplace approximation to estimate the parameters of the joint log-likelihood function (27). As a numerical approximation, we implemented the maximization of the likelihood using PROC NLMIXED in SAS software (34).
does not have a closed form solution. Hence, we used Laplace approximation to estimate the parameters of the joint log-likelihood function (27). As a numerical approximation, we implemented the maximization of the likelihood using PROC NLMIXED in SAS software (34).
At baseline, 2,099 subjects reported at least one ADL/IADL disability and were excluded from analysis. For the progression model, ADL/IADL disability scores of nondisabled subjects were set to missing until the last data assessment before onset of disability. Thus, progression in disability reflects change from a nondisabled state and not from the first level of disability that was observed. We also performed a sensitivity analysis using principal stratification based on survival status at each time point to examine the influence of truncation by death. This approach has been developed for analysis of longitudinal data truncated by death during follow up with specific application for causal models (35).
Results
Baseline characteristics of subjects with no ADL/IADL disability at the first assessment (N = 5,446) stratified by race are shown in Table 1. On average, blacks were more likely to be younger, females, and reported lower levels of education, cognitive and physical functions, and higher levels of body mass index. A total of 45% of blacks and 59% of whites reported no depressive symptoms; blacks were also more likely to report higher symptom levels than whites. Table 2 shows the number (proportion) of subjects with new onset of ADL/IADL disability and average number of ADL/IADL disabilities at the time of onset for each follow-up interview. During the entire follow-up period, a total of 44% of blacks and 35% of whites reported onset of ADL/IADL disability (data not shown in the table). The proportion of subjects reporting onset of ADL/IADL disability was different for those with and without depressive symptoms at baseline: Among the latter, 37% of blacks and 31% of whites developed ADL/IADL disability during follow up. Among subjects with one or more depressive symptoms at baseline, 50% of blacks and 40% of whites developed onset of ADL/IADL disability during follow up. In contrast, the average number of ADL/IADL disabilities after onset was roughly similar in blacks and whites, and the number of disabilities after onset were not substantially different as a function of depressive symptom status at baseline.
Table 1.
Baseline Characteristics of Subjects in a Random Sample of the Population Aged 65 and Older of a Biracial Community in Chicago
| Characteristics | Black Subjects, Mean (SD) | White Subjects, Mean (SD) |
|---|---|---|
| Age (years) | 71.9 (5.6) | 74.9 (7.1) |
| Education (years) | 12.3 (3.1) | 14.3 (3.1) |
| Body mass index (kg/m2) | 28.9 (5.8) | 27.1 (5.2) |
| Physical function | 11.0 (2.6) | 11.9 (2.6) |
| Cognitive function | 0.31 (0.58) | 0.69 (0.47) |
| N (%) | N (%) | |
| Sample size | 3,498 (64%) | 1,948 (36%) |
| Gender | ||
| Male | 1,352 (39%) | 791 (41%) |
| Female | 2,146 (61%) | 1,157 (59%) |
| Medical conditions | ||
| 0 | 927 (27%) | 604 (31%) |
| 1–2 | 2,357 (67%) | 1,248 (64%) |
| 3–5 | 214 (6%) | 96 (5%) |
| Depressive symptoms | ||
| 0 symptoms | 1,579 (45%) | 1,151 (59%) |
| 1–3 symptoms | 1,479 (42%) | 708 (36%) |
| 4–6 symptoms | 359 (10%) | 80 (4%) |
| >7 symptoms | 78 (2%) | 9 (1%) |
Table 2.
Number (Percent) of Subjects With Onset of ADL/IADL Disability and Number (Median, Range) of ADL/IADL Disabilities at the Time of Onset in a Random Sample of the Population Aged 65 and Older of a Biracial Community in Chicago
| Data Collection | Black Subjects Only | White Subjects Only | ||
|---|---|---|---|---|
| No. of Onset (%) | No. of Disabilities, Median (Range) | No. of Onset (%) | No. of Disabilities, Median (Range) | |
| Follow-up year 1* | 495 (16) | 2 (1–12) | 212 (12) | 2 (1–13) |
| Follow-up year 2* | 333 (14) | 1 (1–13) | 147 (10) | 1 (1–13) |
| Follow-up year 3 | 183 (10) | 2 (1–13) | 95 (9) | 2 (1–13) |
| Follow-up year 4* | 168 (10) | 1 (1–13) | 76 (9) | 1 (1–12) |
| Follow-up year 5* | 138 (10) | 2 (1–13) | 62 (9) | 1 (1–12) |
| Follow-up year 6 | 109 (13) | 2 (1–13) | 39 (9) | 2 (1–13) |
| Follow-up year 7* | 74 (12) | 1 (1–13) | 27 (7) | 1 (1–13) |
| Follow-up year 8* | 40 (13) | 2 (1–11) | 19 (7) | 1 (1–11) |
Note: ADL = activities of daily living; IADL = instrumental activities of daily living.
*Telephone interviews.
We assessed the association of baseline depressive symptoms with onset of ADL/IADL disability stratified by race and with adjustments for demographic variables and health-related control variables (Table 3). With each year of age, the odds of onset of disability increased in blacks (odds ratio [OR] = 1.06, 95% confidence interval [CI], 1.04–1.07) and whites (OR = 1.10, 95% CI, 1.08–1.13) at any given time. The odds of onset of disability in black males was lower (OR = 0.79, 95% CI, 0.68–0.92) than black females. However, no significant gender differences were observed among whites. Higher levels of education were associated with lower odds of onset in blacks (OR = 0.97, 95% CI, 0.94–0.99), but showed no association in whites. Number of medical conditions was positively associated with onset of ADL/IADL disability in blacks and whites, and cognitive and physical functions were negatively associated with onset of ADL/IADL disability in blacks and whites. More importantly, for each unit of depressive symptom, the odds of onset of ADL/IADL disability increased in blacks (OR = 1.12, 95% CI, 1.07–1.18) and whites (OR = 1.21, 95% CI, 1.08–1.36). In sum, we see an emerging pattern of differences in marginal associations between blacks and whites, in terms of demographic variables and depressive symptoms.
Table 3.
Estimates From Two-Part Models for Odds of Onset of Combined ADL/IADL Disability in a Random Sample of the Population Aged 65 and Older of a Biracial Community in Chicago
| Parameter | Coefficient | SE | Odds Ratio (95% CI) |
|---|---|---|---|
| Black subjects only (N = 3,498) | |||
| Intercept | −2.88* | .100 | — |
| Age | .056* | .008 | 1.06 (1.04–1.07) |
| Males | −.231‡ | .075 | 0.79 (0.68−0.92) |
| Education | −.033‡ | .012 | 0.97 (0.94−0.99) |
| Body mass index | .014‡ | .006 | 1.01 (1.00−1.03) |
| Medical conditions | .365* | .041 | 1.44 (1.33−1.56) |
| Cognitive function | −.519* | .070 | 0.60 (0.52−0.68) |
| Physical function | −.162* | .015 | 0.85 (0.83−0.88) |
| Depressive symptoms | .116* | .025 | 1.12 (1.07–1.18) |
| Time | .250* | .023 | 1.28 (1.23–1.34) |
| Age × time | .010* | .002 | 1.01 (1.01−1.01) |
| Depressive symptoms × time | .010 | .007 | 1.01 (0.99–1.02) |
| Onset variation | .996* | .088 | — |
| White subjects only (N = 1,948) | |||
| Intercept | −3.87* | .197 | —- |
| Age | .100* | .012 | 1.10 (1.08–1.13) |
| Males | −.078 | .120 | 0.92 (0.73−1.18) |
| Education | −.003 | .019 | 1.00 (0.96−1.04) |
| Body mass index | .029‡ | .011 | 1.03 (1.01−1.05) |
| Medical conditions | .200‡ | .067 | 1.22 (1.07−1.40) |
| Cognitive function | −.822* | .137 | 0.44 (0.33−0.58) |
| Physical function | −.199* | .024 | 0.82 (0.78−0.86) |
| Depressive symptoms | .191* | .060 | 1.21 (1.08–1.36) |
| Time | .294* | .036 | 1.34 (1.25–1.44) |
| Age × time | .018* | .003 | 1.02 (1.01–1.02) |
| Depressive symptoms × time | .059* | .012 | 1.06 (1.04–1.09) |
| Onset variation | 1.414* | .149 | —- |
Note: ADL = activities of daily living; IADL = instrumental activities of daily living.
*p < .0001; † p < .01; ‡ p < .05.
In addition to the marginal association of depressive symptoms, we also assessed the longitudinal association on onset of ADL/IADL disability using time since baseline variable and its interaction with age and baseline depressive symptoms. Among subjects with no depressive symptoms, the main time coefficient indicates that the odds of ADL/IADL disability onset increased over time in blacks (OR = 1.28, 95% CI, 1.22–1.34) and whites (OR = 1.34, 95% CI, 1.25–1.44). The age and time interaction terms indicate that the yearly increase in disability onset odds increased as a function of baseline age among both blacks (OR = 1.01, 95% CI, 1.01–1.01) and whites (OR = 1.02, 95% CI, 1.01–1.02). For each unit of depressive symptom, the association of onset of ADL/IADL disability increased over time in whites (OR = 1.06, 95% CI, 1.04–1.09), but not in blacks (OR = 1.01, 95% CI, 0.99–1.02). A model of the combined data yielded a significant three-way interaction race, depressive symptoms, and time for onset of ADL/IADL disability (p = .012) (data not shown), suggesting that the time-dependent association of depressive symptoms with onset of disability was different among blacks and whites.
To graphically illustrate the association of depressive symptoms on disability, we computed the predicted probability of onset of disability at depressive symptoms scores of 0 (10th percentile) and 3 (90th percentile) (Figure 1). Graphs for onset were plotted for black and white females with 12 years of education and 75 years of age at baseline. Among subjects with no depressive symptoms, the predicted probability of onset increased more over time in blacks than whites. Among subjects with three depressive symptoms, the predicted probability of onset in whites crossed the predicted probability in blacks by the 5th year of follow up. In summary, blacks had a higher probability of onset of ADL/IADL disability than whites in the absence of depressive symptoms. However, the predicted probability of disability onset showed a greater increase in whites than in blacks with each additional depressive symptom.
Figure 1.
Predicted probability of combined activities of daily living/instrumental activities of daily living disability in blacks and whites.
The coefficients in the progression models represent the effect on the rate ratio (RR) of the number of ADL/IADL disabilities, expressed on a log scale (Table 4). Higher age was associated with higher rate of progression of disability in whites (RR = 1.03, 95% CI, 1.01–1.05), but not in blacks at any given time (RR = 1.01, 95% CI, 0.99–1.02). Black males had a significantly faster rate of progression than black females (RR = 1.13, 95% CI, 1.02–1.27). However, gender was not significantly associated with progression of disability in whites. Number of medical condition was positively associated with progression of ADL/IADL disability. Cognitive and physical functions were negatively associated with progression of ADL/IADL disability. The marginal association of depressive symptoms was not significantly associated with the rate of progression of disability in blacks or whites.
Table 4.
Estimates From Two-Part Model for Progression of Combined ADL/IADL Disability in a Random Sample of the Population Aged 65 and Older of a Biracial Community in Chicago
| Parameter | Coefficient | SE | Rate Ratio (95% CI) |
|---|---|---|---|
| Black subjects only (N = 1,543) | |||
| Intercept | −.264† | .081 | — |
| Age | .007 | .007 | 1.01 (0.99–1.02) |
| Males | .124‡ | .053 | 1.13 (1.02–1.26) |
| Education | .020‡ | .008 | 1.02 (1.00–1.04) |
| Body mass index | −.013† | .004 | 0.99 (0.98–1.00) |
| Medical conditions | .090† | .028 | 1.09 (1.03–1.16) |
| Cognitive function | −.361* | .044 | 0.70 (0.64–0.76) |
| Physical function | −.048* | .009 | 0.95 (0.94–0.97) |
| Depressive symptoms | .006 | .017 | 1.01 (0.97–1.04) |
| Time | .195* | .011 | 1.21 (1.19–1.24) |
| Age × time | .009* | .001 | 1.01 (1.01–1.01) |
| Depressive symptoms × time | .004 | .004 | 1.00 (0.99–1.01) |
| Progression random effect | .703* | .032 | — |
| White subjects only (N = 677) | |||
| Intercept | −.672* | .153 | — |
| Age | .032† | .010 | 1.03 (1.01–1.05) |
| Males | .019 | .078 | 1.13 (0.97–1.32) |
| Education | .021 | .012 | 1.02 (1.00–1.04) |
| Body mass index | −.007 | .007 | 0.99 (0.97–1.00) |
| Medical conditions | .085 | .041 | 1.09 (1.01–1.19) |
| Cognitive function | −.638* | .078 | 0.70 (0.60–0.81) |
| Physical function | −.051† | .014 | 0.95 (0.93–0.98) |
| Depressive symptoms | .009 | .036 | 1.01 (0.94–1.08) |
| Time | .157* | .018 | 1.17 (1.13–1.21) |
| Age × time | .012* | .002 | 1.01 (1.01–1.02) |
| Depressive symptoms × time | .076* | .009 | 1.08 (1.06–1.09) |
| Progression random effect | .607* | .077 | — |
Note: ADL = activities of daily living; IADL = instrumental activities of daily living.
*p < .0001; † p < .01; ‡ p < .05.
In terms of the longitudinal associations, the predicted rate of progression over time was slightly higher in blacks (RR = 1.21, 95% CI, 1.19–1.24) compared with whites (RR = 1.17, 95% CI, 1.13–1.21). Older age at disability onset was associated with a higher rate of progression over time after onset among blacks (RR = 1.01, 95% CI, 1.01–1.01) and whites (RR = 1.01, 95% CI, 1.01–1.02). The rate of progression in ADL/IADL disability as a function of depressive symptoms did not increase over time for blacks (RR = 1.00, 95% CI, 0.99–1.01), but did so for whites (RR = 1.08, 95% CI, 1.06–1.09). A model of the combined data showed a significant race × depressive symptoms × time interaction term for progression of disability (p = .008) (data not shown), suggesting that the time-dependent effect of each additional depressive symptom on progression of disability was different among blacks and whites.
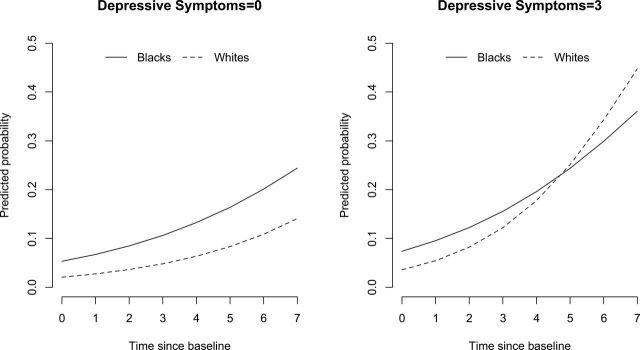
To demonstrate progression of disability in blacks and whites, we plotted the predicted disability scores at depressive symptom scores of 0 (10th percentile) and 3 (90th percentile; Figure 2). Graphs were plotted for black and white females with 12 years of education and 75 years of age at onset. From the figure, we can see that blacks had a higher rate of progression in disability than whites for depressive symptoms score of 0. When subjects had a depressive symptoms score of 3, the trajectory of progression crossed for blacks and whites after the 3-year follow-up interview. In conclusion, blacks had a higher number of disability symptoms than whites for lower levels of depressive symptoms. However, as depressive symptoms got worse, the rate of progression of disability in whites was much worse than blacks. This was formally tested using a model with interaction of race with depressive symptoms and time.
Figure 2.
The rate of progression of combined activities of daily living/instrumental activities of daily living disability in blacks and whites.
In our cohort, 748 (21%) black and 440 (23%) white subjects died during follow up, with 426 (28%) black and 226 (33%) white subjects of these dying after onset of ADL/IADL disability. A sensitivity analysis aimed at exploring the attrition due to death in separate models for onset and progression showed that the coefficients for the main effect of depressive symptoms and time since baseline, and the interaction between time and depressive symptoms, increased by 6%–8% in blacks and 11%–14% in whites, respectively, compared with the primary models (data not shown). Racial differences in the association of depressive symptoms with onset and progression of ADL/IADL disability were larger and remained statistically significant.
Discussion
Disability is a complex process associated with aging. Our findings suggest that the effect of depressive symptoms on onset of disability is different than its effect on progression of disability. Depressive symptoms are often studied in terms of a single process of increase in disability. In this article, we studied depressive symptoms in terms of a two-part mechanism, specifically, an onset and a progression mechanism. The main difference between our study and other studies pertain to the fact that disability was studied in terms of a two-part process with depressive symptoms being able to influence the onset and progression process differently. Thus, we were able to establish that the association of depressive symptoms with onset of disability was different from the association of depressive symptoms with progression process.
In general, blacks were more depressed than whites, and blacks had higher odds of onset of disability and progression than whites independent of depressive symptoms, consistent with several previous reports (36–39). Even though depressive symptoms were associated with disability in blacks and whites, it had stronger association in whites than in blacks. Specifically, depressive symptoms increased the odds of onset of disability over time in whites more than blacks. Also, depressive symptoms seemed to have no effect on progression of disability in blacks, but were moderately associated with progression of disability over time in whites. The stronger effect of depressive symptoms on the odds of incident disability in whites compared with blacks is inconsistent with at least two previous studies (40,41), but neither of these used a two-part process to characterize disability. The reasons for the apparently greater sensitivity to depressive symptoms among whites relative to blacks are unclear. Although older blacks are often assumed to have greater network support systems and higher levels of spirituality (42), which might mitigate the adverse effects of depression, they also report higher levels of depressive symptoms compared with whites (38). However, other evidence indicates that the link between poor mental health and physical health outcomes is weaker among older blacks than whites, suggesting that a more depressed state may be less consequential for older blacks in terms of long-term disability trajectories (43,44). Another possibility is that the adverse effect of depressive symptoms on disability in blacks is overshadowed by other important risk factors, such as low income and high levels of comorbidity.
To further understand the influence of depressive symptoms on the disability process, we included an interaction of age with depressive symptoms to see if higher levels of depressive symptoms among older subjects were driving the association of depressive symptoms in whites. However, the influence of age on the association of depressive symptoms with disability was not significant and did not change the coefficient of depressive symptoms. In terms of gender, black men had lower odds of onset of disability but faster progression than black women. This could be due to the fact that black men had lower comorbidity at baseline and were less likely to have an onset of disability. Future studies can investigate the role of comorbidities in black males and females. Depressive symptoms can also be closely related to other social factors that were not included in this study. Perhaps, there were other physiological mechanisms that can be used to describe the association between depressive symptoms and disability in blacks and whites that were not explored here.
The main shortcoming of this study is that only two patterns of the disability mechanism, namely onset and progression of disability, were studied. However, future research is needed to develop analytical methods that can study several patterns of disability mechanism. We also used two modes of data collection, in-home interviews and telephone interviews, which might have introduced additional bias in our disability assessment. However, we adjusted for interview type using an indicator variable for telephone survey in our analytical models. About 20% of subjects had deceased during the follow up that might introduce additional bias. However, our sensitivity analysis showed that the association of depressive symptoms with onset and progression of disability was slightly higher than models unadjusted for death, thus, no selection bias was observed due to death.
In conclusion, we found that depressive symptoms were associated with onset of ADL/IADL disability in blacks and whites. However, the odds of onset of ADL/IADL disability increased significantly higher over time among whites compared with blacks. In addition, the rate of progression of ADL/IADL disability was associated with depressive symptoms among whites, but showed no association among blacks. The findings of this research suggest that depressive symptoms shows stronger association with ADL/IADL disability among whites when compared with blacks. This study has strong implications in terms of racial differences of mental disorders such as depressive symptoms that show markedly different associations by ethnic groups. Understanding these ethnic differences may play an important role on ethnic specific intervention and/or prevention programs.
Funding
This work was supported by grants from the National Institute for Aging (R01 AG11101 and R01 AG032247) and National Institute for Environmental Health Sciences (R01 ES10902).
References
- 1. Pope AM, Tarlov AR. Disability in America: Toward a National Agenda for Prevention. Washington, DC: National Academy Press; 1991. [Google Scholar]
- 2. Manton KG, Corder LS, Stallard E. Chronic disability trends in elderly United States populations: 1982–1994. Nat Acad Sci. 1997;94:2593–2598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291:1596–1602 [DOI] [PubMed] [Google Scholar]
- 4. Wolf DA, Hunt K, Knickman J. Perspectives on the recent decline in disability at older ages. Milbank Q. 2005;83:365–395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Jette AM. Disentangling the process of disablement. Soc Sci Med. 1999;48:471–472 [DOI] [PubMed] [Google Scholar]
- 6. Mendes de Leon CF, Guralnik JM, Bandeen-Roche K. Short-term change in physical function and disability: The Women’s Health and Aging Study. J Gerontol Soc Sci. 2002;57B:S355–S–365 [DOI] [PubMed] [Google Scholar]
- 7. Cutler DM. Declining disability among the elderly. Health Aff. 2001;20:11–27 [DOI] [PubMed] [Google Scholar]
- 8. Dunlop DD, Manheim LM, Song J, Chang RW. Gender and ethnic/racial disparities in health care utilization among older adults. J Gerontol B Psychol Sci Soc Sci. 2002;57:S221–S233 [DOI] [PubMed] [Google Scholar]
- 9. Haas S, Rohlfsen L. Life course determinants of racial and ethnic disparities in functional health trajectories. Soc Sci Med. 2010;70:240–250 [DOI] [PubMed] [Google Scholar]
- 10. Matthews RJ, Smith LK, Hancock RM, Jagger C, Spiers NA. Socioeconomic factors associated with the onset of disability in older age: a longitudinal study of people aged 75 years and over. Soc Sci Med. 2005;61:1567–1575 [DOI] [PubMed] [Google Scholar]
- 11. Thorpe RJ, Jr, Kasper JD, Szanton SL, Frick KD, Fried LP, Simonsick EM. Relationship of race and poverty to lower extremity function and decline: findings from the Women’s Health and Aging Study. Soc Sci Med. 2008;66:811–821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32:20–47 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Alexopoulos GS, Vrontou C, Kakuma T, et al. Disability in geriatric depression. Am J Public Health. 1999;89:1346–1352 10474551 [Google Scholar]
- 14. Mills TL, Henretta JC. Racial, ethnic, and sociodemographic differences in the level of psychosocial distress among older Americans. Res Aging. 2001;23:131–152 [Google Scholar]
- 15. Smalbrugge M, Pot AM, Jongenelis L, Gundy CM, Beekman AT, Eefsting JA. The impact of depression and anxiety on well being, disability and use of health care services in nursing home patients. Int J Geriatr Psychiatry. 2006;21:325–332 [DOI] [PubMed] [Google Scholar]
- 16. Penninx BW, Leveille S, Ferrucci L, van Eijk JT, Guralnik JM. Exploring the effect of depression on physical disability: longitudinal evidence from the established populations for epidemiologic studies of the elderly. Am J Public Health. 1999;89:1346–1352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Thorpe RJ, Koster A, Kritchevsky S, et al. Race, socioeconomic resources and late life mobility and decline: findings from the health aging and body composition study. J Gerontol Med Sci. 2011;66:1114–1123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Husaini BA, Moore ST. Arthritis disability, depression, and life satisfaction among black elderly people. Health Soc Work. 1990;15:253–260 [DOI] [PubMed] [Google Scholar]
- 19. Williams DR, Gonzalez HM, Neighbors H, et al. Prevalence and distribution of major depressive/disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites. Arch Gen Psych. 2007;64: 305–315 [DOI] [PubMed] [Google Scholar]
- 20. Simpson SM, Krishnan LL, Kunik ME, Ruiz P. Racial disparities in diagnosis and treatment of depression: a literature review. Psychiatr Q. 2007;78:3–14 [DOI] [PubMed] [Google Scholar]
- 21. Blazer DG, Kessler RC, McGonagle KA, Swartz MS. The prevalence and distribution of major depression in a national community sample: the National Comorbidity Survey. Am J Psychiatry. 1994;151:979–986 [DOI] [PubMed] [Google Scholar]
- 22. Kessler RC, Berglund P, Demler O, et al. ; National Comorbidity Survey Replication. The epidemiology of major depressive disorder. JAMA. 2003;289:3095–3105 [DOI] [PubMed] [Google Scholar]
- 23. Stecker T, Fortney JC, Steffick DE, Prajapati S. The triple threat for chronic disease: obesity, race, and depression. Psychosomatics. 2006;47: 513–518 [DOI] [PubMed] [Google Scholar]
- 24. Fuller-Thomson E, Nuru-Jeter A, Minkler M, Guralnik JM. Black- white disparities in disability among older Americans: further untangling the role of race and socioeconomic status. J Aging Health. 2009;21:677–698 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Lewis TT, Guo H, Lunos S, et al. Depressive symptoms and cardiovascular mortality in older black and white adults: evidence for a differential association by race. Circ Cardiovasc Qual Outcomes. 2011;4:293–299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Taylor MG. Capturing transitions and trajectories: the role of socioeconomic status in later life disability. J Gerontol B Psychol Sci Soc Sci. 2010;65:733–743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Rajan KB, Hebert LE, Scherr P, et al. Cognitive and physical functions as determinants of delayed age at onset and progression of disability. J Gerontol A Biol Sci Med Sci. 2012;67:1419–1426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Bienias JL, Beckett LA, Bennett DA, Wilson RS, Evans DA. Design of the Chicago Health and Aging Project (CHAP). J Alzheimers Dis. 2003;5:349–355 [DOI] [PubMed] [Google Scholar]
- 29. Kohout FJ, Berkman LF, Evans DA, Cornoni-Huntley J. Two shorter forms of the CES-D depression symptoms index. J Aging Health. 1993;5:179–193 [DOI] [PubMed] [Google Scholar]
- 30. LaPlante MP. The classic measure of disability in activities of daily living is biased by age but an expanded IADL/ADL measure is not. J Gerontol B Psychol Sci Soc Sci. 2010;65:720–732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Katz S, Akpom CA. A measure of primary sociobiological functions. Int J Health Serv. 1976;6:493–508 [DOI] [PubMed] [Google Scholar]
- 32. Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9: 179–186 [PubMed] [Google Scholar]
- 33. Agresti A. Categorical Data Analysis. 2 nd ed. New York, NY: John Wiley & Sons; 2002 [Google Scholar]
- 34. SAS. SAS 9.2 software. Cary, NC: SAS Institute Inc; 2009 [Google Scholar]
- 35. Frangakis CE, Rubin DB, An MW, MacKenzie E. Principal stratification designs to estimate input data missing due to death. Biometrics. 2007;63:641–649 [DOI] [PubMed] [Google Scholar]
- 36. Mendes de Leon CF, Barnes LL, Bienias JL, Skarupski KA, Evans DA. Racial disparities in disability: recent evidence from self-reported and performance-based disability measures in a population-based study of older adults. J Gerontol Psych Sci. 2003;60:263–271 [DOI] [PubMed] [Google Scholar]
- 37. Kelly-Moore JA, Ferraro KF. The black white disability gap. Persistent inequality in late life? J Gerontol Psych Sci. 2003;59:34–43 [DOI] [PubMed] [Google Scholar]
- 38. Skarupski KA, Mendes de Leon CF, Bienias JL, et al. Black-white differences in depressive symptoms among older adults over time. J Gerontol B Psychol Sci Soc Sci. 2005;60:136–142 [DOI] [PubMed] [Google Scholar]
- 39. Dunlop DD, Manheim LM, Song J, Lyons JS, Chang RW. Incidence of disability among preretirement adults: the impact of depression. Am J Public Health. 2005;95:2003–2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kelley-Moore JA, Ferraro KF. A 3-D model of health decline: disease, disability, and depression among black and white older adults. J Health Soc Behav. 2005;46:376–391 [DOI] [PubMed] [Google Scholar]
- 41. Cummings SM, Neff JA, Husaini BA. Functional impairment as a predictor of depressive symptomatology: the role of race, religiosity, and social support. Health Soc Work. 2003;28:23–32 [DOI] [PubMed] [Google Scholar]
- 42. Skarupski KA, Fitchett G, Evans DA, Mendes de Leon CF. Daily spiritual experiences in a biracial, community-based population of older adults. Aging Ment Health. 2010;14:779–789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. McMullen CK, Luborsky MR. Self-rated health appraisal as cultural and identity process: African American elders’ health and evaluative rationales. Gerontologist. 2006;46:431–438 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Gitlin LN, Hauck WW, Dennis MP, Schulz R. Depressive symptoms in older African-American and white adults with functional difficulties: the role of control strategies. J Am Geriatr Soc. 2007;55: 1023–1030. [DOI] [PMC free article] [PubMed] [Google Scholar]


