Abstract
Surgical treatment of fractures involving the proximal humeral head is hampered by complications. Screw cutout is the major pitfall seen in connection with rigid plating. We have exploited a bony explanation for this phenomenon.
Materials and Methods:
We examined the convex surface of the humeral head looking at the density and the topographical strength of the subchondral bone using mechanical testing of bone cylinders harvested from the humeral head. We also studied the osseous architecture of the subchondral bone and thickness of the boneplate of the humeral head using a 3-dimensional serial sectioning technique.
Results:
The bone strength and bone density correlated well and revealed large regional variations across the humeral head. Bone strength and stiffness of the trabecular bone came to a maximum in the most medial anterior and central parts of the humeral head, where strong textural anisotropy was also found. We found in particular a lower bone strength and density in the posterior and inferior regions of the humeral head. A rapid decline in bone strength within a few mm below a relatively thin subchondral plate was also reported.
Clinical Relevance:
We have in this paper explored some of the most important factors connected with screw stability at the cancellous bone level. We discovered large variations in bone density and bone strength across the joint surface rendering certain areas of the humeral head less suitable for screw placement. The use of rigid plate constructs with divergent screw directions will predictably place screws in areas of the humeral head comprising low density and low strength cancellous bone. New concepts of plates and plating techniques for the surgical treatment of complex fractures of the proximal humerus should take bone distribution, strength, and architecture into account.
Keywords: Bone architecture, bone strength, humeral head, screw cutout
INTRODUCTION
Proximal humeral fractures are one of the most common fractures, mainly affecting elderly people. The fractures are often associated with underlying osteoporosis[1] and surgical treatment of this injury remains a challenge.[2] Several operative treatment modalities of proximal humeral fractures have been developed over the years.[3] Currently, the locking plate systems have become gold standard in the treatment of these complex fractures.[4,5,6] This modality offers multiple locking screws oriented in different directions to maximize screw number, position, and resistance to displacement and it is generally believed that the plates provide more secure fixation, especially in weak bone.[7]
The stability of this implant is achieved at the screw-bone interface and the success of the procedure is highly dependant on the quality of the juxta-articular bone of the humeral head.[2,7,8] An alarming failure rate due to screw cutout and intra-articular penetration of screws through the subchondral bone of the humeral head has been reported.[3,7] In elderly patients, failure rates as high as 48% were seen,[7] indicating that locking screws may be an important risk factor in cases of poor bone quality.
This study was initiated to investigate the biomechanical properties of the trabecular bone of the humeral head adjacent to the bone-screw interface in order to get insight into screw stability. We question that divergent screws does increase screw stability when placed in weak bone and our secondary goal was to explore the capacity of the humeral head to resist screw cutout.
MATERIALS AND METHODS
A series of 12 complete pairs of fresh shoulders (24 specimens) with intact soft tissues were obtained at autopsy within 24 hours of death. There were 6 male and 6 female donors. Mean age was 56 years (range 40-74 years). Pre-test CT scans were performed to exclude concurrent pathology.
In the first series two humeral head specimens, donor age of 52 years and 65 years were used for serial sectioning in order to study qualitative and quantitative architectural features of the humeral head. Mapping of the textural anisotropy made it possible theoretically to perform compression tests and bone strength analyses parallel to the main trabecular direction of the humeral head. The second series comprised protocolled mechanical testing of bone cylinders harvested from ten pairs of humeral head specimens.
Osseous architecture
An automated imaging technique, based upon three-dimensional serial sectioning, was used for qualitative examination of the composite architecture of the humeral head.[9] Approximately 800 binary (black Epoxy resin and white bone) digital images of 1024 × 1024 voxel size were generated from each head specimen. Graphical reconstructions were used to qualitatively describe the bone morphology of each humeral head in three dimensions [Figure 1a–d]. The thickness of the subchondral plate was also assessed from these graphical reconstructions. In practice, the subchondral plate is not a completely solid structure, but contains vascular channels and small marrow spaces. The thickness of subchondral plate was assessed using a threshold of 95% bone volume defined from the binary images.
Figure 1.
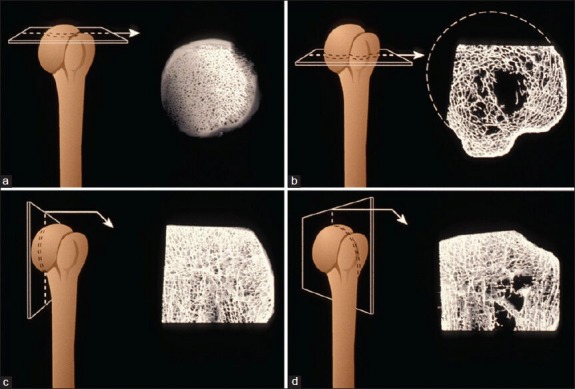
Graphical reconstructions of the humeral head. (a) The dense tubular arranged trabeculae formed the subchondral bone texture at the top of the head. Note the few connecting trabeculae. (b) The shift from plate-like trabeculae forming the greater tuberosity toward the center of the head is abrupt. (c) The wave-like remnants of the epiphyseal scar separates the subchondral bone from the trabeculae at the center of the head. (d) This section demonstrates the complex trabecular bone texture underneath the “footprint” of the rotator cuff tendons
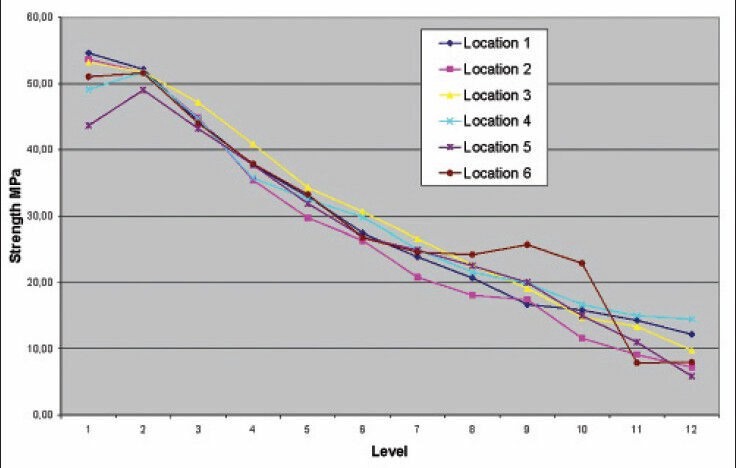
Architectural measurements
The structural anisotropy of the bone of humeral head[10] was only assessed in the most medial and central part. Symmetry around the main trabecular axis was calculated to express the degree of structural anisotropy expressed by the 3 Eigenvalues [Table 1].[11] The eigenvectors are defined as polar coordinates on the hemispherical humeral head. The main trabecular direction is perpendicular to the subchondral plate. The secondary direction and tertiary trabecular directions are dependent on the arm position and oriented from medial to lateral or from superior to inferior.
Table 1.
Structural anisotropy of cancellous bone (specimen one)
Mechanical testing
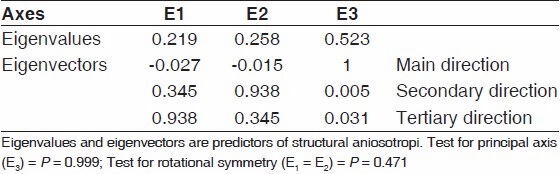
One-hundred (100) bone cylinders were harvested from 20 (10 pairs) humeral head specimens [Figure 2]. Seven (7) cylinders were lost during testing procedures. The first cylinder was harvested from the very center of the head. The other 4 test positions were defined at a distance halfway between the center of the head and the rim of the humeral head. Drilling was started with the 7.0 mm trephine drill burr having circumferential contact with the cartilage of the humeral head. This technique ensured that the cylinders could be harvested orthogonal to the subchondral plate. Following harvesting, the cartilage and subchondral plate was cut 1 mm below the subchondral plate using an ExaktR cutting grinding machine.
Figure 2.
(a) Penetrometer test spots. (b) Location of bone cylinders harvested from the subchondral bone of the humeral head.
All the bone cylinders were stored in an airtight plastic container with physiologic saline before CT scanning. The container and the specimens were vacuumed before CT scanning. Average CT number in Hounsfield units was calculated within a circular region of interest for each bone cylinder and expressed bone mineralization.
Destructive compression tests
We used the principles of biomechanical testing reported by Linde et al. in the Journal of Biomechanics[12] eliminating as many restraints and biases as possible. A 4302 INSTRONR materials testing machine equipped with a 1 kN load cell was used for axial compression tests of the bone cylinders. The longitudinal strain was calculated instantly. A 3rd degree polynomial fit was performed on the data sets and the elastic modulus (Emax) was determined from the maximal slope of the destructive test curve.
Indentation tests
A 4302 INSTRONR materials testing machine equipped with a 10 kN load cell was used for indentation tests. A steel needle, with a base diameter of 2.5 mm and the needle shaft milled to 2.3 mm, was driven into the cancellous bone at a constant speed of 1 mm s-1.[13] During testing, the humeral head specimens were fixed to the distal steel column of the Instron machine using acrylic cement around the remaining parts of the proximal humerus. The resulting load-depth curves [Figure 3] yield an expression of the bone strength in Mpa.
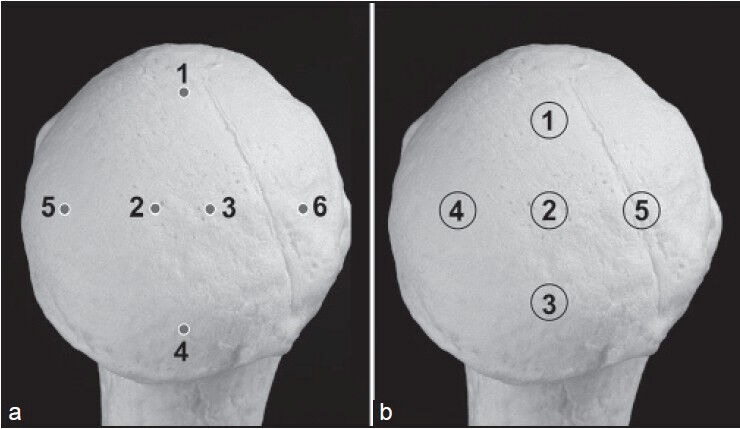
Figure 3.
Penetration test curves with penetration strength from 6 different locations of a humeral head specimen from a 65-year-old male. The level markers indicate consecutive 1 mm depth intervals below the subchondral plate. Note that maximum strength is connected with the subchondral plate. Note also the rapid decline in bone strength below the subchondral plate. Locations 2 and 3 represent the center of the humeral head
Statistics
SOLO Power Analysis (BMDP Statistical Software Inc) was used for statistical evaluation. Wilcoxons rank sum test was used to analyze the penetration tests. Unpaired students t-test was used for evaluation of the destructive tests.[14] Correlation analyses were made for the CT vs ultimate strength and stiffness using SPSS Statistical software package. For the penetration tests, we examined if there was a statistical significant reduction with depth. For all locations, we compared the penetration strength measurements at level 1 with the penetration strength for all locations at level 5. This does not give a risk for alpha error cumulation.
Trabecular distribution tests were performed using non-parametric methods described by Fisher et al.[15] Estimations of uniformity (Fisher, paragraph 6.3.1.ia), estimations of the architectural principal axis (Fisher, paragraph 6.3.1.iv), and the determination of rotational symmetry (degree of anisotropy) of the secondary and tertiary directions (Fisher, paragraph 6.3.1.iii) was performed at a 5% level of significance.
RESULTS
Studies of the trabecular bone texture revealed great variations from the humeral head surface to the lateral cortex [Figure 1a–d].
The humeral head is covered by a thin and convex subchondral plate. Thickness of the plate averaged 0.6 mm (range 0.3-0.8 mm), the plate being thickest centrally. The plate grows thinner toward the anchor site to cortical bone at the margins of the head. The subchondral plate overlies a transitional zone of cancellous bone [Figure 1a] characterized by strong architectural anisotropy [Table 1]. The main trabeculae in the central and medial section of the humeral head were orientated in a radial direction aiming from the subchondral plate toward the center of the humeral head. Our tests also demonstrated very few connecting trabeculae perpendicular to the main axis. The stable transitional zone of organized trabeculae was separated from the central part of the humeral head by remnants of the epiphyseal scar [Figure 1c].
In contrast to the head, the greater tuberosity comprises plate-like trabeculae mostly orientated in parallel to the lateral cortex of the humerus [Figure 1b and 1d].
Mechanical tests of the bone cylinders from the humeral head revealed average ultimate strength values ranging from 3.21 MPa to 6.17 Mpa [Figure 4a]. The variations of CT-density [Figure 4b] expressed as average CT units (Hounsfield units) correlated (Pearson correlation) well with stiffness [Figure 4c] (r = 0.64) and strength (r = 0.84). The ultimate strength and CT-density measurements revealed that the humeral head was significantly stronger (P < 0.001) and more dense (P < 0.01) in the anterior and central regions. The weakest part of the humeral head was located posteriorly and inferiorly of the humeral head. This monocentric strength pattern was seen in all the tested specimens and therefore seemed to be independent of age. The measured strength and stiffness was not statistical different between left and right shoulders (P < 0.001)
Figure 4.
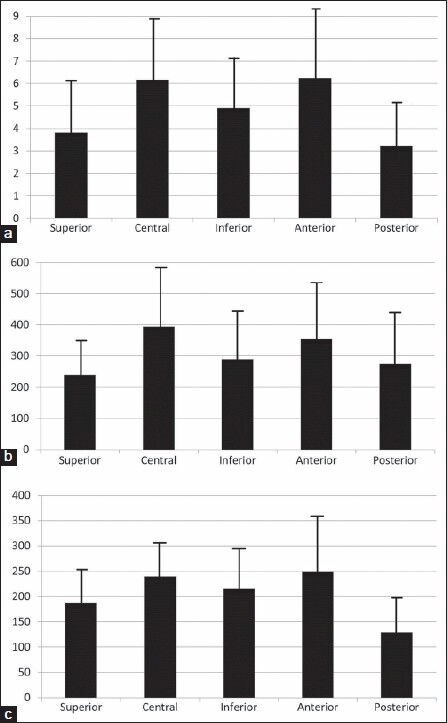
(a) Normalized strength (MPa) in loading of bone cylinders from 5 different sites at the humeral head (mean ± SD). (b) CT-density (Hounsfield Units) from 5 different sites at the humeral head (mean ± SD). (c) Stiffness (MPa) and in loading of bone cylinders from 5 different sites at the humeral head (mean ± SD).
Penetration tests revealed a characteristic profile of strength [Figure 3]. Penetrations strength decreased by 25% from level 1 at the level of the subchondral plate to a level 5 mm below the plate. Strength 7-8 mm below the subchondral plate was reduced by a factor 2 (P < 0.000).
DISCUSSION
Failure of osteosynthesis of proximal humeral fractures due to screw cutout has become a problem of significance.[7,8] A key issue in every successful osteosynthesis is that the screws have to remain entirely in the cancellous bone and should not penetrate the subchondral plate upfront.[7,16] Consequently, primary screw cutout or screw penetration is thought to be related to perforation of the subchondral plate and several guidelines on how to avoid primary screw cutout have been published.[5,17]
The morphology and mechanical properties of the subchondral plate and juxtaarticular bone is only scarcely described in the literature. Indentation tests are to our knowledge a suitable method to test the strength of the subchondral bone complex. A recent study by Zumstein et al.[18] using indentation testing could identify a monocentric strength pattern in the majority of their cases as well as a more bipolar pattern in a few cases. Our results revealed a monocentric and rather uniform strength profile of the plate and the adjacent cancellous bone. Lower strength was confirmed in the caudal parts of the humeral head. A rapid decline of bone strength was endeavored as the penetrometer needle had penetrated the subchondral plate. This suggests that the strength of the convex joint surface is more dependent on an intact subchondral plate than the cancellous bone comprising the transitional zone. Remnants of the epiphyseal scar seemed to be the anatomical landmark separating well-structured cancellous bone from low strength cancellous bone beneath the epiphyseal scar. This is in accordance with the results of Tingart et al.[19] who found a tendency of trabecular thinning located 1 and 2 cm underneath the top of the humeral head.
Secondary screw cutout represents failure at the screw-bone interphase in the transitional zone. Several factors contribute to this phenomenon but implant stability at the screw-bone interphase is important to a successful treatment of proximal humeral fractures. Pullout test seems to be the preferred method to test screw stability and has also been used to simulate screw cutout. Simple pullout tests as performed by Tingart et al.[20] revealed that the antero-superior region of the humeral head had the lowest bone mineral density and the lowest pull-out strength and they recommended placement of screws in areas with the highest bone density. Liew et al.[21] demonstrated that screw location significantly influenced the fixation strength, which was best when the screw tip was placed subchondrally in the center of the humeral head. This strategy to purchase as much bone as possible coupled with more and thicker screws may possibly increase screw stability and potentially increase fixation strength.[5,22] Barvencik et al.[23] showed in a histomorphometric study that women over 60 years of age had a significant age-related decrease in bone mass. They also found that the most superior and medially located part of the humeral head showed, independent from age and sex, the highest bone mass. Using histomorphometric analyses and indentation tests, Hepp et al.[24] found peak values of bone strength in the medial and dorsal section and decreasing bone strength caudally in the humeral head.
There has been some dispute about optimal placement of screws in the humeral head.
Based on the four studies and in agreement with our results, the medial and superior part of the humeral head should be considered the best location for screw placement. Currently, the angle stable plate is the preferred method to stabilize proximal humeral fractures. Technically, the screw in angle stable plating originates from the neck of the head and is directed toward the subchondral plate in a sequence of divergence and convergence. A divergent screws configuration leads to screw placement into areas of low strength and density in the humeral head, whereas parallel or convergent screw configurations theoretically place screws in the most medial and strongest bone of the humeral head. Current evidence therefore implicates that screws should converge toward areas of strong bone within the humeral head. Interestingly, Wähnert et al.[25] showed the biomechanical disadvantage of a divergent locking screw angle under static and cyclic loading compared to the more advantageous parallel screw configuration.
Next to bone density, the trabecular bone architecture is the most important factor determining the mechanical properties of bone.[20] The study by Hepp et al.[24] found a significant correlation between histomorphometric parameters and bone strength. We studied trabecular anisotropy using a method that allowed us to estimate the trabecular, three-dimensional orientation in contrast to the surface measurements of trabecular orientation generated from histomorphometric methods. The architectural measures from our study predicted strong textural anisotropy in the central and most medial section of the humeral head. No firm conclusions should be drawn from the analyses of only 2 specimens but in this particular area of the humeral head, the trabeculae has been shown by other authors to radiate from the convex subchondral plate toward the center of the head.[24]
Our study on anisotropy also indicated that only a limited number of trabecular connections exist in the subchondral regions to support the primary trabeculae. Furthermore, the trabecular orientation seems not to be affected by age. In their study, Hepp et al.[24] suggested that bone strength was related primarily to the number of trabecular connections. This hypothesis was also supported by Guo and Kim[20] who found that bone loss due to loss of trabeculae was much more detrimental to Young's modulus and strength of the trabecular bone stock than bone loss due to trabecular thinning, indicating the importance of trabecular number and connectivity in the mechanical integrity of trabecular bone.
Osteoporotic bone is more prone to cutout, probably due lower density and a low number of connecting trabeculae associated with aging. Trabecular comminution and sometimes large bone voids in the fractured humeral head could enhance these phenomenons. Attempts have been made to predict the quality of bone of the humeral head in fracture cases from BMD measurements at the contralateral shoulder.[26] As we could not prove in our bilateral test design the significant differences of strength and stiffness between left and right shoulders, this could be a valid option in the daily clinic.
We have in this paper explored some of the most important factors connected with screw stability at the cancellous bone level. We discovered large variations in bone density and bone strength across the joint surface. Respecting the limitations of our study from the use of specimens with a great variation in age, we suggest that stability of screw-bone interphase is particular compromised in the peripheral zones of the humeral head. We found in particular a lower bone strength and density in the posterior and inferior regions which makes these areas of the humeral head less suitable for screw placement.
New concepts of plates and plating techniques for the surgical treatment of complex fractures of the proximal humerus should take bone distribution, strength, and architecture into account.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Konrad G, Bayer J, Hepp P, Voigt C, Oestern H, Kääb M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Surgical technique. J Bone Joint Surg Am. 2010;92(Suppl 1):85–95. doi: 10.2106/JBJS.I.01462. [DOI] [PubMed] [Google Scholar]
- 2.Miranda MA. Locking plate technology and its role in osteoporotic fractures. Injury. 2007;38(Suppl 3):S35–9. doi: 10.1016/j.injury.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 3.Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: A systematic review. J Shoulder Elbow Surg. 2009;18:837–44. doi: 10.1016/j.jse.2009.06.004. [DOI] [PubMed] [Google Scholar]
- 4.Ring D. Current concepts in plate and screw fixation of osteoporotic proximal humerus fractures. Injury. 2007;38(Suppl 3):59–68. doi: 10.1016/j.injury.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 5.Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma. 2007;21:185–91. doi: 10.1097/BOT.0b013e3180333094. [DOI] [PubMed] [Google Scholar]
- 6.Schulte LM, Matteini LE, Neviaser RJ. Proximal periarticular locking plates in proximal humeral fractures: Functional outcomes. J Shoulder Elbow Surg. 2011;20:1234–40. doi: 10.1016/j.jse.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 7.Owsley KC, Gorczyca JT. Fracture displacement and screw cutout after open reduction and locked plate fixation of proximal humeral fractures. J Bone Joint Surg Am. 2008;90:233–40. doi: 10.2106/JBJS.F.01351. [DOI] [PubMed] [Google Scholar]
- 8.Meier RA, Messmer P, Regazzoni P, Rothfischer W, Gross T. Unexpected high complication rate following internal fixation of unstable proximal humerus fractures with an angled blade plate. J Orthop Trauma. 2006;20:253–60. doi: 10.1097/00005131-200604000-00004. [DOI] [PubMed] [Google Scholar]
- 9.Odgaard A, Andersen K, Melsen F, Gundersen HJ. A direct method for fast three-dimensional serial reconstruction. J Microsc. 1990;159:335–42. doi: 10.1111/j.1365-2818.1990.tb03038.x. [DOI] [PubMed] [Google Scholar]
- 10.Odgaard A. Three-dimensional methods for quantification of cancellous bone architecture. Bone. 1997;20:315–28. doi: 10.1016/s8756-3282(97)00007-0. [DOI] [PubMed] [Google Scholar]
- 11.Odgaard A, Kabel J, van Rietbergen B, Dalstra M, Huiskes R. Fabric and elastic principal directions of cancellous bone are closely related. J Biomech. 1997;30:487–95. doi: 10.1016/s0021-9290(96)00177-7. [DOI] [PubMed] [Google Scholar]
- 12.Linde F, Nørgaard P, Hvid I, Odgaard A, Søballe K. Mechanical properties of trabecular bone. Dependency on strain rate. J Biomech. 1991;24:803–9. doi: 10.1016/0021-9290(91)90305-7. [DOI] [PubMed] [Google Scholar]
- 13.Hvid I, Andersen K, Olesen S. Cancellous bone strength measurements with the osteopenetrometer. Eng Med. 1984;13:73–8. doi: 10.1243/emed_jour_1984_013_019_02. [DOI] [PubMed] [Google Scholar]
- 14.Armitage P, Berry G. Statistical Methods in Medical Research. Oxford, London, Edinburgh: Blackwell Scientific Publications; 1987. pp. 104–12. 408-20. [Google Scholar]
- 15.Fisher NI, Lewis T, Embleton BJ. Statistical Analysis of Spherical Data. Cambridge: Cambridge University Press; 1987. pp. 160–170. [Google Scholar]
- 16.Südkamp N, Bauer J, Hepp P, Voigt C, Oestern H, Kääb M, et al. Open reduction and internal fixation of proximal humeral fractures with use of the locking proximal humerus plate. Results of a prospective, multicenter, observational study. J Bone Joint Surg Am. 2009;91:1320–8. doi: 10.2106/JBJS.H.00006. [DOI] [PubMed] [Google Scholar]
- 17.Lescheid J, Zdero R, Shah S, Kuzyk PR, Schemitsch EH. The biomechanics of locked plating for repairing proximal humerus fractures with or without medial cortical support. J Trauma. 2010;69:1235–42. doi: 10.1097/TA.0b013e3181beed96. [DOI] [PubMed] [Google Scholar]
- 18.Zumstein V, Kraljevic M, Wirz D, Hügli R, Müller-Gerbl M. Correlation between mineralization and mechanical strength of the subchondral bone plate of the humeral head. J Shoulder Elbow Surg. 2012;21:887–93. doi: 10.1016/j.jse.2011.05.018. [DOI] [PubMed] [Google Scholar]
- 19.Tingart MJ, Lehtinen J, Zurakowski D, Warner JJ, Apreleva M. Proximal humeral fractures: Regional differences in bone mineral density of the humeral head affect the fixation strength of cancellous screws. J Shoulder Elbow Surg. 2006;15:620–4. doi: 10.1016/j.jse.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 20.Guo XE, Kim CH. Mechanical consequence of trabecular bone loss and its treatment: A three-dimensional model simulation. Bone. 2002;30:404–11. doi: 10.1016/s8756-3282(01)00673-1. [DOI] [PubMed] [Google Scholar]
- 21.Liew AS, Johnson JA, Patterson SD, King GJ, Chess DG. Effect of screw placement on fixation in the humeral head. J Shoulder Elbow Surg. 2000;9:423–6. doi: 10.1067/mse.2000.107089. [DOI] [PubMed] [Google Scholar]
- 22.Schulte LM, Matteini LE, Neviaser RJ. Proximal periarticular locking plates in proximal humeral fractures: Functional outcomes. J Shoulder Elbow Surg. 2011;20:1234–40. doi: 10.1016/j.jse.2010.12.015. [DOI] [PubMed] [Google Scholar]
- 23.Barvencik F, Gebauer M, Beil FT, Vettorazzi E, Mumme M, Rupprecht M, et al. Age- and sex-related changes of humeral head microarchitecture: Histomorphometric analysis of 60 human specimens. J Orthop Res. 2010;28:18–26. doi: 10.1002/jor.20957. [DOI] [PubMed] [Google Scholar]
- 24.Hepp P, Lill H, Bail H, Korner J, Niederhagen M, Haas NP, et al. Where should implants be anchored in the humeral head? Clin Orthop Relat Res. 2003;415:139–47. doi: 10.1097/01.blo.0000092968.12414.a8. [DOI] [PubMed] [Google Scholar]
- 25.Wähnert D, Windorlf M, Brianza S, Rothstock S, Radtke R, Brighenti V, et al. A comparison of parallel and diverging screw angles in the stability of locked plate constructs. doi: 10.1302/0301-620X.93B9.26721. [DOI] [PubMed] [Google Scholar]
- 26.Diederichs G, Korner J, Goldhahn J, Linke B. Assessment of bone quality in the proximal humerus by measurement of the contralateral site: A cadaveric analyze. Arch Orthop Trauma Surg. 2006;126:93–100. doi: 10.1007/s00402-006-0103-z. [DOI] [PubMed] [Google Scholar]


