Abstract
Context:
Spontaneous thrombosis of renal artery is extremely rare. Its presentation is that of commonly encountered problem of acute abdomen underscoring the need for a clinician to be aware of it.
Case Report:
We report a case of a 56-year-old male with no previous health problems presented with complaint of abdominal pain and nausea. Computed tomography angiogram (CTA) of the abdomen and pelvis confirmed thrombus in left renal artery. He showed good response to the treatment with resolution of the thrombus and improvement in the renal perfusion.
Conclusion:
Our case does conform to the others experience of good outcome when treatment is initiated in a timely manner. This patient had resolution of symptoms and restoration of perfusion with anticoagulation. The purpose of this case report is to remind busy practicing physicians to keep spontaneous renal thromboembolism in differential diagnosis in a patient with acute abdomen.
Keywords: Abdomen, Acute, Flank Pain, Infarction, Renal, Renal Artery, Thrombosis
Introduction
Most cases of renal artery thrombosis are due to thromboemboli which usually originate in heart or aorta. In-situ thrombosis of renal artery is uncommon. Most common causes of in-situ thrombosis are blunt abdominal trauma[1] and atherosclerotic lesion of the renal artery. There are case reports of it being associated with polycythemia vera,[2] pregnancy, hypercoagulability, renal transplantation,[3] intra-aortic balloon placement,[4] renal angiography, oral contraceptives,[5] cocaine injection,[6] nephrotic syndrome, systemic lupus erythematosus,[7] renovascular hypertension, infective endocarditis,[8] Ehlers-Danlos syndrome, renal surgery. However, spontaneous renal artery thrombosis without any known cause is extremely rare.
Case Presentation
A 56-year-old man was referred to the authors’ hospital with severe, unremitting abdominal pain of 3 days duration associated with nausea and vomiting. He denied history of trauma. Review of rest of the systems was negative. He had no prior medical history, no prior hospitalizations, and no prior surgery. Specifically, he had no history of diabetes mellitus, hypertension, hyperlipidemia, heart disease, or atrial fibrillation.
On examination, the patient was afebrile, normotensive and in normal sinus rhythm. Abdominal examination was remarkable for tenderness and guarding over the left flank area.
A computed tomography angiogram (CTA) of the abdomen and pelvis revealed a thrombus at the origin of the left renal artery, a normal caliber aorta with near complete infarction of the kidney [Figure 1], and no evidence of aortic plaques [Figure 2]. Positron emission tomography 3-dimensional (3D) emission scan with a median activity of 346 MBq (range 225–391 MBq) of FDG 18Fluoro-deoxy-Glucose (GlucoRos® Helmholtz Center, Dresden-Rossendorf, Germany) were taken to measure glomerular filtration rate of kidneys. The GFR of left kidney was determined to be 9 ml/min and of right kidney 67 ml/min. Echocardiogram was normal with no evidence of clots in the cardiac chambers. CT scans of the chest and head were negative. Other tests, specifically white blood cells, platelets, LDH in blood and urine analysis were normal.
Figure 1.
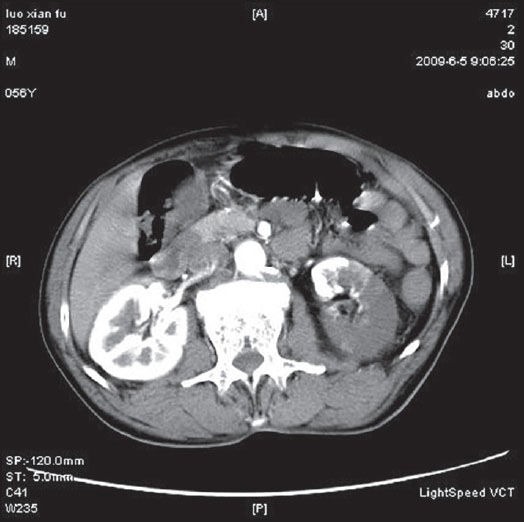
CT scan showing left renal infarct
Figure 2.
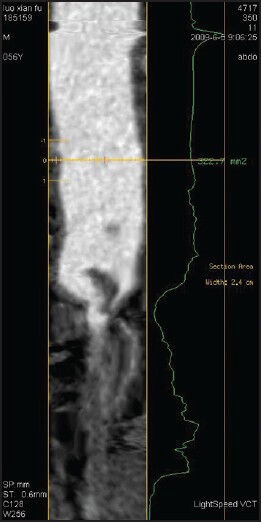
Focal thrombus at the origin of left renal artery
Anticoagulation was started with full dose low-molecular-weight heparin. Thrombolytics were not used because it had already been 3 days since the onset of symptoms. Anticoagulation was later switched to warfarin. Patient's symptoms gradually resolved, and a repeat CT scan on 7th day of hospitalization showed resolution of the thrombus and restoration of the left kidney perfusion [Figure 3]. Plan is to treat with warfarin for total of 6 months.
Figure 3.
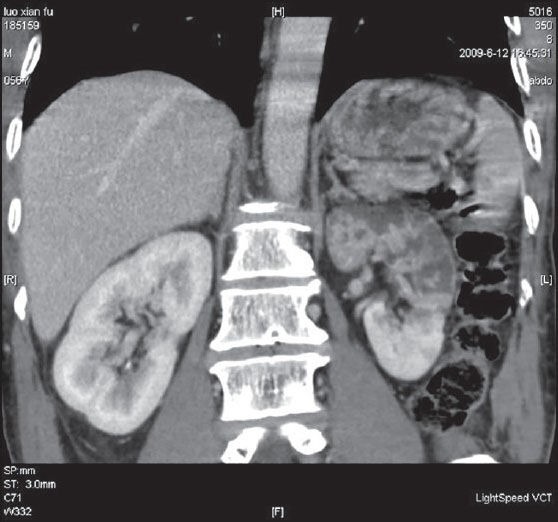
CT image shows improved left kidney perfusion after 7 days
Discussion
Renal artery thrombosis usually occurs in adults aged between 30 and 50 years although it can occur in other age groups also. Most patients suffer a sudden, sharp unremitting pain in the flank or upper abdomen or lower back pain. This may be associated with fever, nausea, vomiting and leukocytosis. Hematuria and proteinuria can also be present.
This case is unique as there is no underlying known disease process triggering the formation of thrombus in the renal artery. This patient was previously healthy, with no evidence of trauma, atherosclerotic disease or any of the other disease associations described in the introduction above. With reporting of our case, we want to raise the awareness of the possibility of spontaneous renal artery thrombosis in patients presenting with acute abdomen. This diagnosis may be underreported because there are no specific symptoms, signs or tests short of contrast imaging of the renal artery to make the diagnosis. In fact, in our own case the diagnosis was missed at the outlying hospital and even after the patient was referred to our hospital, the diagnosis was first considered only when the thrombus was seen on the CT imaging study done as part of generic work up for acute abdomen. Besides CT imaging, magnetic resonance imaging can also be used to confirm the diagnosis.[9]
Our case is also unique in that it does not conform to the commonly held belief that LDH is elevated in patients with renal infarction.[10] Even though our patient had sizeable renal infarction but the LDH was normal. Thus, a normal LDH cannot be relied upon to rule out renal infarction.
Our case does conform to the others experience of good outcome when treatment is initiated in a timely manner. This patient had resolution of symptoms and restoration of perfusion with anticoagulation. Thrombolytics can also be considered in cases that are diagnosed within about 6 hours of onset of symptoms. Surgical interventions such as autotransplantation or nephrectomy can be avoided with timely diagnosis and initiation of thrombolysis and/or anticoagulation. Excellent outcomes with timely diagnosis underscore the need to consider renal artery thrombosis in differential diagnosis of acute abdomen. The purpose of this case report is to remind busy practicing physicians to keep spontaneous renal thromboembolism in differential diagnosis in a patient with acute abdomen. When index of suspicion is high in such patients, CT abdomen can be done to establish the diagnosis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Cosby RL, Miller PD, Schrier RW. Traumatic renal artery thrombosis. Am J Med. 1986;81:890–4. doi: 10.1016/0002-9343(86)90363-3. [DOI] [PubMed] [Google Scholar]
- 2.Chagnac A, Zevin D, Weinstein T, Gafter U, Korzets A, Levi J, et al. Erythrocytosis associated with renal artery thrombosis in a patient with polycystic kidney disease on hemodialysis. Acta Haematol. 1990;84:40–2. doi: 10.1159/000205025. [DOI] [PubMed] [Google Scholar]
- 3.Dimitroulis D, Bokos J, Zavos G, Nikiteas N, Karidis NP, Katsaronis P, et al. Vascular complications in renal transplantation: A single-center experience in 1367 renal transplantations and review of the literature. Transplant Proc. 2009;5:1609–14. doi: 10.1016/j.transproceed.2009.02.077. [DOI] [PubMed] [Google Scholar]
- 4.Baciewicz FA, Jr, Kaplan BM, Murphy TE, Neiman HL. Bilateral renal artery thrombotic occlusion: A unique complication following removal of a transthoracic intraaortic balloon. Ann Thorac Surg. 1982;33:631–4. doi: 10.1016/s0003-4975(10)60826-0. [DOI] [PubMed] [Google Scholar]
- 5.Golbus SM, Swerdlin AR, Mitas JA, 2nd, Rowley WR, James DR. Renal artery thrombosis in a young woman taking oral contraceptives. Ann Intern Med. 1979;90:939–40. doi: 10.7326/0003-4819-90-6-939. [DOI] [PubMed] [Google Scholar]
- 6.Wohlman RA. Renal artery thrombosis and embolization associated with intravenous cocaine injection. South Med J. 1987;80:928–30. doi: 10.1097/00007611-198707000-00033. [DOI] [PubMed] [Google Scholar]
- 7.Tsugawa K, Tanaka H, Kudo M, Nakahata T, Ito E. Renal artery thrombosis in a pediatric case of systemic lupus erythematosus without antiphospholipid antibodies. Pediatr Nephrol. 2005;20:1648–50. doi: 10.1007/s00467-005-2009-3. [DOI] [PubMed] [Google Scholar]
- 8.Liao WB, Bullard MJ, Liaw SJ. Widespread embolism in a patient with infective endocarditis: A case report. Changgeng Yi Xue Za Zhi. 1995;18:82–7. [PubMed] [Google Scholar]
- 9.Yamanouchi Y, Yamamoto K, Noda K, Tomori K, Kinoshita T. Renal infarction in a patient with spontaneous dissection of segmental arteries: Diffusion-weighted magnetic resonance imaging. Am J Kidney Dis. 2008;52:788–91. doi: 10.1053/j.ajkd.2008.07.002. [DOI] [PubMed] [Google Scholar]
- 10.Huang CC, Kao WF, Yen DH, Huang HH, Huang CI, Lee CH, et al. Renal infarction without hematuria: Two case reports. J Emerg Med. 2006;30:57–61. doi: 10.1016/j.jemermed.2005.03.013. [DOI] [PubMed] [Google Scholar]


