Abstract
Context:
Retroperitoneal fibrosis is a rare but severe disease. The diagnosis is usually late when a patient is evaluated for renal insufficiency. Untreated cases may develop serious complications or advance to end-stage renal disease.
Case Report:
We report a 66-year-old man who presented with worsening kidney function. He was successfully given the diagnosis of idiopathic retroperitoneal fibrosis. Prednisone (1 mg/kg per day) was initiated. The patient's symptoms continued to improve at 1 month with stable kidney function.
Conclusion:
Clinicians should have high index of suspicion for retroperitoneal fibrosis when patients present with an elevated erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP) and renal insufficiency from obstructive uropathy. The diagnosis of retroperitoneal fibrosis is primarily made from imaging by computed tomography (CT) scan. Biopsy should be performed in patients who do not have typical findings on CT scan and to exclude the possibility of immunoglobulin G4 (IgG4)-related disease.
Keywords: Idiopathic retroperitoneal fibrosis, Obstructive uropathy, Renal insufficiency
Introduction
Retroperitoneal fibrosis is a rare but severe disease and often makes the diagnosis difficult. The diagnosis is usually late when a patient is evaluated for renal insufficiency and obstructive uropathy. There are idiopathic and secondary forms of retroperitoneal fibrosis. Immunoglobulin G4 (IgG4)-related disease, drugs, infections, malignancies, prior surgeries, and radiation therapy should be investigated for secondary causes. We report a challenging and difficult to diagnose case of an older man with anasarca, back pain, and renal insufficiency secondary to idiopathic retroperitoneal fibrosis. The patient's symptoms responded well with steroid treatment.
Case Presentation
A 66-year-old man with a history of coronary artery disease, status post-coronary artery bypass graft (CABG), chronic kidney disease (CKD) stage 3, and hypertension presented to the hospital with anasarca, back pain, abdominal distension, and nausea for 2 months. On physical examination, he was normotensive (blood pressure of 137/72 mmHg). He had signs of fluid overload with severe generalized edema, jugular venous distension, and increased abdominal girth. Blood tests demonstrated acute kidney injury (AKI) on CKD with elevated serum creatinine of 2.1 mg/dl, elevated C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) of 20 mg/l and 25 mm/1 h, respectively. Serum albumin was 3.6 g/dl (normal value 3.4-4.7 g/dl). Serum protein electrophoresis (SPEP) showed no monoclonal protein. Urine microscopy was unremarkable with urine protein to osmolality ratio of 0:16. A renal ultrasound for evaluation for his renal insufficiency interestingly showed atypical appearance with rounded configuration with an echogenic rim surrounding both kidneys and hydronephrosis [Figure 1]. Suspicion for infiltrative was raised. The patient underwent positron emission tomography/computed tomography (PET/CT) that demonstrated soft tissue rim around both kidneys [Figure 2a] and diffuse retroperitoneal infiltrative process [Figure 2b].
Figure 1.
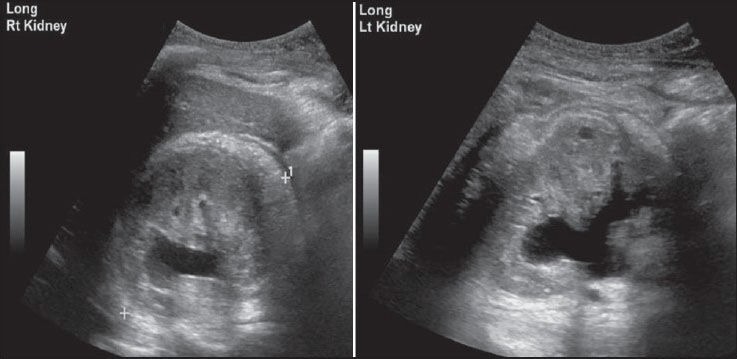
A renal ultrasound showed atypical appearance with rounded configuration with an echogenic rim surrounding both kidneys and hydronephrosis
Figure 2.
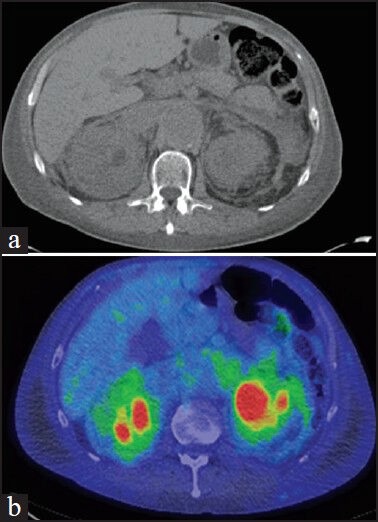
A PET/CT demonstrated soft tissue rim around both kidneys (a) and diffuse retroperitoneal infiltrative process (b). PET/CT = Positron emission tomography/computed tomography
The patient underwent CT-guided tru-cut biopsy of right perinephric soft tissue, which showed nonspecific fibroinflammatory process. IgG4 immunohistochemistry was negative. The patient was diagnosed with idiopathic retroperitoneal fibrosis. Prednisone (1 mg/kg per day) was initiated. The patient's symptoms continued to improve at 1 month with stable kidney function.
Discussion
Retroperitoneal fibrosis is a rare disease. There are idiopathic and secondary forms of retroperitoneal fibrosis. Idiopathic retroperitoneal fibrosis accounts for over 70% of cases.[1] The incidence of the idiopathic form was reported to be 0.1 per 100,000 person-years with its prevalence of 1.4 per 100,000 residents.[2]
Symptoms may occur such as low back pain, nonspecific systemic complaints, and lower extremity edema. The diagnosis is usually late when a patient is evaluated for renal insufficiency and obstructive uropathy. ESR or CRP is usually high. The diagnosis of retroperitoneal fibrosis is primarily made from imaging by CT scan.[3] Biopsy should be performed in patients who do not have typical findings on CT scan to exclude malignancy and IgG4-related disease.
Untreated cases may develop serious complications or advance to end-stage renal disease.[4] Medical treatment of retroperitoneal fibrosis depends upon the cause. In patients with idiopathic retroperitoneal fibrosis, glucocorticoids are traditionally considered the mainstay of therapy.[4]
Our case presentation demonstrates that with appropriate treatment, promptly initiated for idiopathic retroperitoneal fibrosis, the patient's symptoms can improve. Clinicians should have high index of suspicion for retroperitoneal fibrosis when patients present with an elevated ESR or CRP and renal insufficiency from obstructive uropathy.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Cronin CG, Lohan DG, Blake MA, Roche C, McCarthy P, Murphy JM. Retroperitoneal fibrosis: A review of clinical features and imaging findings. AJR Am J Roentgenol. 2008;191:423–31. doi: 10.2214/AJR.07.3629. [DOI] [PubMed] [Google Scholar]
- 2.Uibu T, Oksa P, Auvinen A, Honkanen E, Metsärinne K, Saha H, et al. Asbestos exposure as a risk factor for retroperitoneal fibrosis. Lancet. 2004;363:1422–6. doi: 10.1016/S0140-6736(04)16100-X. [DOI] [PubMed] [Google Scholar]
- 3.Feinstein RS, Gatewood OM, Goldman SM, Copeland B, Walsh PC, Siegelman SS. Computerized tomography in the diagnosis of retroperitoneal fibrosis. J Urol. 1981;126:255–9. doi: 10.1016/s0022-5347(17)54466-3. [DOI] [PubMed] [Google Scholar]
- 4.Vaglio A, Salvarani C, Buzio C. Retroperitoneal fibrosis. Lancet. 2006;367:241–51. doi: 10.1016/S0140-6736(06)68035-5. [DOI] [PubMed] [Google Scholar]


