Abstract
Objective
To estimate the cost-effectiveness of a trial of labor after one previous cesarean delivery (TOLAC).
Study Design
A model comparing TOLAC with elective repeat cesarean delivery (ERCD) was developed for a hypothetical cohort with no contraindication to a TOLAC. Probabilistic estimates were obtained from women matched on their baseline characteristics using propensity scores. Cost data, quality adjusted-life-years (QALYs) and data on cerebral palsy were incorporated from the literature.
Results
The TOLAC strategy dominated the ERCD strategy at baseline, with $138.6 million saved and 1703 QALYs gained per 100,000 women. The model was sensitive to five variables; the probability of uterine rupture, the probability of successful TOLAC, the QALY of failed TOLAC, the cost of ERCD and the cost of successful TOLAC without complications. When the probability of TOLAC success was at the base value, 68.5%, TOLAC was preferred if the probability of uterine rupture was 4.2% or less. When the probability of uterine rupture was at the base value, 0.8%, the TOLAC strategy was preferred as long as the probability of success was 42.6% or more.
Conclusion
A TOLAC is less expensive and more effective than an ERCD in a group of women with balanced baseline characteristics.
Keywords: cost-effectiveness, elective repeat cesarean, trial of labor, propensity scores
In 2003 the Agency for Healthcare Research and Quality (AHRQ) published the results of an evidence report and technology assessment comparing the harms and benefits of delivery options for women after a prior cesarean delivery.1 Incorporated in this report was a review of the economic literature on this topic. Of thirteen papers reviewed only two had methodology that were highly rated.2, 3 These two papers compared the cost-effectiveness of a trial of labor after a previous cesarean (TOLAC) with an elective repeat cesarean delivery (ERCD). Both concluded that TOLAC could be cost-effective when the probability of a successful TOLAC was sufficiently high.
Inherent to these analyses was the assumption that the probabilistic data used in the decision analytical models was derived from two groups (i.e. those women who had TOLAC and those who had ERCD) with similar baseline characteristics. However, this assumption was not accurate, as the studies from which the probabilistic data were derived actually were composed of two groups of women – those who underwent TOLAC and those who underwent ERCD –with different baseline characteristics.4–7 Consequently, it is uncertain whether the data used in the decision analytic models were biased and led to a bias in the ultimate results.
Ideally, a trial in which women were randomized to one of the delivery approaches would balance observed as well as unobserved baseline covariates, and would produce the true treatment effect, but such a trial is unlikely to be undertaken. In the absence of a randomized trial, propensity score analysis may be used in an observational study to derive two groups with similar baseline characteristics. The data from these groups can then be used in decision analytic models with less concern for biased outcomes. Thus, this analysis was undertaken to determine whether TOLAC or ERCD is the more cost-effective strategy after one prior cesarean based on data derived from groups of women with similar baseline characteristics.
Methods
We developed a decision analysis model comparing a TOLAC with an ERCD for a hypothetical cohort of 100,000 women with no contraindication to a TOLAC. The analysis was based on the societal perspective, incorporating all health outcomes and economic costs regardless of who experienced the outcome or paid the costs.8 The primary outcome was cost-effectiveness, measured as the marginal cost per quality adjusted-life-year (QALY) gained, with a marginal cost per QALY ratio of less than $50,000 used to indicate a strategy is cost effective.
The decision tree was developed using TreeAge Pro 2009 (TreeAge Software, Inc. Williamstown, MA). The initial decision represented a woman’s approach to delivery; either a TOLAC or an ERCD. Women in the TOLAC arm experienced either a successful vaginal delivery, required a repeat cesarean during labor, or had a uterine rupture in association with a successful or failed TOLAC. Additional maternal and neonatal morbidity that occurred was dependent upon these outcomes or upon the alternate choice of an ERCD.
The probabilities for the decision tree primarily were obtained from data collected from 1999 through 2002 in a registry (the Cesarean Registry) by the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network. Nineteen academic centers comprising of 32 hospitals throughout the United States participated in this observational study, in which data were collected on all women with a prior cesarean delivery. Institutional review board approval at each participating center was obtained. Study personnel at the medical centers abstracted data from patient charts under a waiver of informed consent. Further detail on specific methods of the study can be obtained from previously published articles.5, 9
Women who were eligible to have either an ERCD or a TOLAC, and who had a singleton, term, vertex gestation and one prior low transverse incision (n=22,068) comprised the population that was analyzed in order to obtain probabilities requisite for the model. A gestation was considered “term” if delivery occurred at or beyond 37 weeks’ gestation. An ERCD was defined as a cesarean delivery without any indication other than the prior cesarean. Thus, women who had a repeat cesarean for indications such as placenta previa or active herpes were excluded from this analysis (n=759). In order to ensure that women who underwent ERCD truly had no indication for the cesarean other than their choice, those who were reported to have a cesarean that was elective but who had an additional reported indication implying this was not the case (i.e. cephalopelvic disproportion, failure to progress, cord prolapse, non-reassuring tracing or abruption) were excluded (n=262). Also, women were ineligible for the cohort if they had an ERCD prior to 39 weeks without spontaneous labor or premature rupture of membranes given that elective delivery prior to 39 weeks is associated with known adverse outcomes unrelated to mode of delivery (n=3188).10 Women who underwent ERCD, after experiencing spontaneous labor or rupture of membranes prior to 39 weeks, were included since they were eligible for, and would need to choose between, either ERCD or labor. Women who underwent a TOLAC but whose labors were induced also were excluded (n=3235) since this intervention has been associated with a lower probability of success and a higher probability of uterine rupture, and is not a probabilistic possibility but a choice that a woman and her provider make.11, 12 Women with fetuses with major congenital malformations were not included since these conditions, unrelated to mode of delivery, would influence the newborn outcome (n=120). Consequently, 14,504 women were available for analysis, of whom 8297 had a TOLAC and 6207 had an ERCD.
The propensity score methodology (R MatchIt library, http://www.r-project.org/) of one-toone matching without replacement using the nearest Mahalanobis distance13 was used to derive 3981 matched pairs of women who underwent either ERCD or TOLAC and who were balanced according to 43 baseline characteristics. This final cohort, approximately 80% of whom had no previous vaginal delivery, had a TOLAC success rate of 68.1%. All 31 cases of uterine rupture occurred in the TOLAC group, 27 in association with TOLAC failure. Further detailed information on the development of this cohort and the propensity score methodology can be found in Gilbert et al.14
The maternal outcomes recorded through delivery included: endometritis (clinical diagnosis of puerperal uterine infection in the absence of findings suggesting another source), wound complication (seroma, hematoma or infection), operative injury (broad ligament hematoma, cystotomy, or bowel or ureteral injury), peripartum hysterectomy, thromboembolism (deep vein thrombosis or pulmonary embolus) and maternal death. Cases of uterine rupture, modeled as a separate branch of the decision tree, were defined as a disruption or tear of the uterine muscle and visceral peritoneum or a uterine muscle separation with extension to adjacent structures. Neonatal outcomes recorded up to 120 days after delivery or hospital discharge (whichever occurred first) were: acidemia (arterial cord pH less than 7.0), transient tachypnea of the newborn (TTN), respiratory distress syndrome (RDS), proven or confirmed sepsis, hypoxic ischemic encephalopathy (HIE), and infant death. A separate maternal and infant mutually exclusive hierarchy incorporating these outcomes was developed following the reverse order above, with death first. Since the Cesarean Registry was a short-term observational study and cerebral palsy (CP) could occur as a long-term consequence of an event (HIE) at the time of delivery, the probability of CP also was incorporated in the model by estimating that 12% of infants with HIE would ultimately be diagnosed with CP.15
The probabilities used in the model are shown in Table 1. The ranges were obtained from the 95% Blyth-Still-Casella binomial confidence intervals (from Stat-Xact, Cytel Software) based on the proportion of events in the matched data set.16 Since the probability of successful TOLAC and uterine rupture have previously been shown to be variables to which the results are sensitive, these two variables were varied across a range wider than that which would have been derived from the data set alone; 34.0–100% and 0–5.0%, respectively.
Table 1.
Probability Estimates in the Model
| Outcomes | ERCD N = 3981 |
Uterine Rupture N = 31 |
Failed TOLAC N = 1244 |
Successful TOLAC N = 2706 |
||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Baseline | Range | Baseline | Range | Baseline | Range | Baseline | Range | |
|
| ||||||||
| Maternal | ||||||||
| Death | 0.025 | 0.001–0.138 | 0 | 0–9.733 | 0 | 0–0.278 | 0 | 0–0.128 |
| Thromboembolism | 0.025 | 0.001–0.138 | 0 | 0–9.733 | 0 | 0–0.278 | 0 | 0–0.128 |
| Hysterectomy | 0.277 | 0.138–0.489 | 3.226 | 0.165–16.060 | 0.161 | 0.028–0.558 | 0 | 0–0.128 |
| Operative injury | 0.126 | 0.050–0.288 | 12.900 | 4.530–28.600 | 1.206 | 0.676–1.967 | 0 | 0–0.128 |
| Wound complication | 0.855 | 0.601–1.175 | 0 | 0–9.733 | 1.206 | 0.676–1.967 | 0.074 | 0.013–0.256 |
| Endometritis | 2.111 | 1.705–2.599 | 12.900 | 4.530–28.600 | 7.556 | 6.149–9.103 | 1.516 | 1.090–2.023 |
| Infant | ||||||||
| Death | 0.025 | 0.001–0.138 | 3.226 | 0.165–16.060 | 0.080 | 0.004–0.443 | 0 | 0–0.128 |
| HIE | 0 | 0–0.087 | 3.226 | 0.165–16.060 | 0.080 | 0.041–0.443 | 0 | 0–0.128 |
| Sepsis | 3.115 | 2.597–3.687 | 29.030 | 15.760–46.650 | 6.758 | 5.426–8.292 | 4.250 | 3.521–5.054 |
| RDS | 0.528 | 0.327–0.804 | 0 | 0–9.733 | 1.046 | 0.558–1.767 | 0.517 | 0.300–0.841 |
| TTN | 1.181 | 0.879–1.552 | 0 | 0–9.733 | 2.172 | 1.436–3.140 | 0.628 | 0.366–0.996 |
| Acidemia | 0.226 | 0.112–0.427 | 6.452 | 1.159–20.030 | 0.724 | 0.360–1.340 | 0.037 | 0.002–0.203 |
Data presented as percent; ERCD, elective repeat cesarean delivery; TOLAC, trial of labor after a previous cesarean; HIE, hypoxic ischemic encephalopathy; RDS, respiratory distress syndrome; TTN, transient tachypnea of the newborn
With an exception for CP, the following costs were incorporated into the model and based on mode of delivery: hospital, obstetrician, pediatrician, anesthesiologist, maternal and caregiver opportunity costs. A summary of these costs is provided in Table 2 with further detail regarding the basis for these costs provided in the Appendix. Hospital costs were obtained from the 2009 AHRQ’s Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUPnet), a nationwide database of hospital inpatient stays containing approximately 95% of all hospital discharges in the United States.17 Based on the International Classification of Diseases (ICD-9) codes these costs represent direct and indirect costs. Obstetrician and pediatrician costs were obtained from the 2010 Current Procedural Terminology (CPT) from the American Medical Association (AMA).18 Since the Cesarean Registry did not contain data that would allow estimation of anesthesia costs, these costs were derived from the literature.3 Maternal and caregiver postpartum opportunity costs were derived from the Bureau of Labor Statistics using the 2009 median hourly wage and salary averages for women 25 to 34 years old and for all individuals 16 years and older, respectively.19 Since the costs associated with maternal and infant death are hard to quantify, as these events occur in such a large variety of circumstances, a range of 0 to $1 million was used, with baseline estimates of $20,000 and $50,000 respectively. For CP, hospital costs after delivery were estimated as twice the base cost of HIE, with the addition of approximately $9000 for pediatrician fees and $23,800 per year for the next 49 years.20–22
Table 2.
Cost Estimates in the Model
| Outcomes | ERCD | Uterine Rupture | Failed TOLAC | Successful TOLAC | ||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Baseline | Range | Baseline | Range | Baseline | Range | Baseline | Range | |
|
| ||||||||
| Maternal | ||||||||
| Death | 27.41 | 0–1,000.0 | 27.9 | 0–1,000.0 | 27.9 | 0–1,000.0 | 24.1 | 0–1,000.0 |
| Thromboembolism | 16.61 | 8.3–66.4 | 19.1 | 9.6–76.5 | 18.4 | 9.2–73.5 | 13.3 | 6.7–53.3 |
| Hysterectomy | 17.9 | 8.9–71.5 | 20.4 | 10.2–81.5 | 19.6 | 9.8–78.6 | 14.6 | 7.3–58.4 |
| Operative injury | 13.9 | 6.9–55.6 | 16.4 | 8.2–65.6 | 15.7 | 7.8–62.6 | 10.6 | 5.3–42.5 |
| Wound complication | 15.6 | 7.8–62.3 | 18.1 | 9.0–72.3 | 17.3 | 8.7–69.4 | 12.3 | 6.2–49.2 |
| Endometritis | 15.7 | 7.9–63.0 | 18.2 | 9.1–73.0 | 17.5 | 8.8–70.0 | 12.5 | 6.2–49.9 |
| Well (no adverse outcome) | 11.4 | 5.7–17.0 | 13.9 | 6.9–20.8 | 13.1 | 6.6–19.7 | 8.1 | 4.0–12.1 |
| Infant | ||||||||
| Death | 52.2 | 0–1,000.0 | 52.2 | 0–1,000.0 | 52.2 | 0–1,000.0 | 52.2 | 0–1,000.0 |
| Cerebral palsy | n/a | n/a | 688.4 | 344.2–2,753.6 | 688.4 | 344.2–2,753.6 | 688.4 | 344.2–2,753.6 |
| HIE | 40.9 | 20.4–163.5 | 40.9 | 20.4–163.5 | 40.9 | 20.4–163.5 | 40.9 | 20.4–163.5 |
| Sepsis | 8.6 | 4.3–34.2 | 8.6 | 4.3–34.2 | 8.6 | 4.3–34.2 | 8.6 | 4.3–34.2 |
| RDS | 25.5 | 12.7–101.9 | 25.9 | 12.9–103.5 | 25.5 | 12.7–101.9 | 25.5 | 12.7–101.9 |
| TTN | 8.7 | 4.3–34.6 | 9.1 | 4.5–36.3 | 8.7 | 4.3–34.6 | 8.7 | 4.3–34.6 |
| Acidemia | 7.3 | 3.7–29.3 | 7.7 | 3.9–30.9 | 7.3 | 3.7–29.3 | 7.3 | 3.7–29.3 |
| Well (no adverse outcome) | 0.9 | 0.5–1.3 | 0.9 | 0.5–1.4 | 0.9 | 0.4–1.3 | 0.9 | 0.4–1.3 |
Currency in dollars ($thousands); n/a, not applicable, ERCD, elective repeat cesarean delivery; TOLAC, trial of labor after a previous cesarean; HIE, hypoxic ischemic encephalopathy; RDS, respiratory distress syndrome ; TTN, transient tachypnea of the newborn
In sensitivity analysis, costs were ranged from 50% to 400% of the base-case estimate with the exception of those associated with maternal and well infant discharge, in which cases a range of 50% to 150% was used. Although such ranges included values that appeared beyond plausible in some cases, such a wide range ensured that the plausible range was contained within the interval and that threshold analyses could be judiciously performed.23
With the exception of CP, all outcomes (e.g. wound infection) occurred and were resolved during the initial hospitalization. Correspondingly, for the costs associated with these variables, no discounting was performed. Conversely, CP continued to affect a child and incur health care costs through the child’s life, and thus these costs were discounted at 3% annually in the base-case. All costs are presented in 2009 dollars, with adjustments used, when needed, according to the medical care component of the Consumer Price Index.24
Distutilities or utility decrements were assigned based on the literature (Table 3).3, 25–26 Since information was limited, infants were assigned full utility (1) except in the case of infant death, CP and HIE where disutilities of 0, 0.44, and 0.75, respectively, were assigned. QALYs were determined based on the disutilities and life expectancy, discounted at 3% in the base case. It was assumed mode of delivery per se did not alter maternal or neonatal life expectancy. Maternal and infant life expectancy was estimated to be 78 years except for in the case of CP where 50 years was assumed.21, 27
Table 3.
Utility and QALY Estimates by Mode of Delivery or Outcome
| Disutility | Disutility Days | QALY | ||||
|---|---|---|---|---|---|---|
|
| ||||||
| Mode of Delivery/Outcome | Baseline | Baseline | Range | Baseline | Range | Reference |
| ERCD | 0.45 | 21 | 14–180 | 27.140 | 26.944–27.149 | 3 |
| Uterine rupture | 0.49 | 21 | 14–180 | 27.138 | 26.925–27.147 | 3 |
| Failed TOLAC* | 0.47 | 21 | 14–180 | 27.139 | 26.934–27.148 | 3 |
| Successful TOLAC | 0.35 | 7 | 2–42 | 27.160 | 27.126–27.164 | 3 |
| Hysterectomy† | 0.49 | 21 | 14–180 | 24.355 | 22.724–25.894 | 3, 25 |
| Cerebral palsy‡ | 0.44 | All | All | 14.840 | 10.336–19.611 | 26 |
| HIE | 0.75 | 42 | 14–180 | 30.824 | 30.787–30.901 | Assumed |
| Infant§ | n/a | n/a | n/a | 30.910 | 7.728–23.183 | Assumed |
QALY, quality adjusted life-years; ERCD, elective repeat cesarean delivery; TOLAC, trial of labor after a previous cesarean; HIE, hypoxic ischemic encephalopathy; n/a, not applicable
Extrapolated from Chung et al., midway between ERCD and rupture3;
Blend of Harris et al. and Chung et al. at 55% and 45% respectively to represent the proportion of women with a hysterectomy that would and would not have desired another pregnancy3, 25 For Chung et al. assumed the disutility and disutility days in the Table and from Harris et al. disutilities of 0.31 (0.14–0.48) until age 50;
Disutility range for cerebral palsy of 0.26–0.61;
Baseline utility of 1 for all infants without cerebral palsy or HIE, with a range of (0.25–1) tested in sensitivity analysis.
To test the robustness of the results obtained from the base-case model, sensitivity analyses were performed. One-way sensitivity analysis was conducted on all probabilities, costs and QALYs by varying one variable at a time from the low to high value in its range, while holding other variables fixed. Multivariable sensitivity analysis also was conducted by varying more than one probability at a time. This included bivariable as well as probabilistic sensitivity analysis (PSA) using Monte Carlo simulation with 10,000 iterations to determine how often the base-case strategy was preferred. Simulation was conducted using the beta or uniform distribution for the probabilities where appropriate and the gamma distribution for costs. Sensitivity analysis was also conducted on the discount rate, using 0%, 5% and 7%.
Results
The base-case analysis revealed that, for a hypothetical cohort of 100,000 women, the choice of TOLAC resulted in 68,077 fewer cesarean deliveries, 201 fewer hysterectomies and 25 fewer maternal deaths (Table 4). Conversely, TOLAC was associated with 779 additional uterine ruptures, as well as adverse neonatal outcomes of sepsis, RDS and acidemia. Additionally, among those undergoing TOLAC, CP was estimated to occur in an additional 6 offspring. The TOLAC strategy, therefore, was dominant, and resulted in $138.6 million saved and 1703 QALYs gained per 100,000 women.
Table 4.
Maternal and Infant Outcomes per 100,000 Women
| TOLAC | ERCD | |
|---|---|---|
|
| ||
| Deliveries | 100,000 | 100,000 |
| Cesarean deliveries | 31,923 | 100,000 |
| Maternal | ||
| Uterine rupture | 779 | 0 |
| Maternal death | 0 | 25 |
| Hysterectomy | 76 | 277 |
| Endometritis | 3492 | 2111 |
| Infant | ||
| Infant Death | 51 | 25 |
| Cerebral palsy | 6 | 0 |
| HIE | 51 | 0 |
| Sepsis | 5227 | 3115 |
| RDS | 679 | 528 |
| Acidemia | 302 | 226 |
TOLAC, trial of labor after a previous cesarean; ERCD, elective repeat cesarean delivery; HIE, hypoxic ischemic encephalopathy; RDS, respiratory distress syndrome
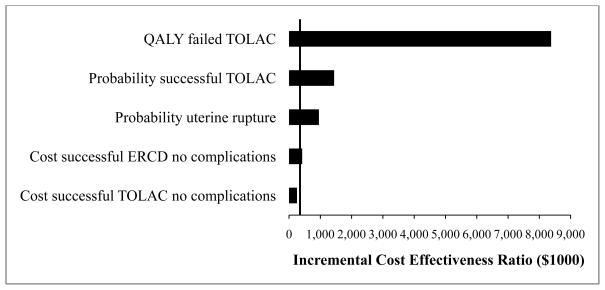
One-way sensitivity analysis was performed across the full range for all the variables. The results were robust to all changes except for five variables (Figure 1). These variables and their thresholds, or where the preferred strategy changed were; the probability of uterine rupture (4.2%), the probability of successful TOLAC (42.2%), and without any complications the cost of ERCD ($9040) and the cost of successful TOLAC ($11,428) as well as the QALY of failed TOLAC (27.00) which represented a disutility of 0.47 for 132 days or more. Bivariable analysis on the probability of uterine rupture and successful TOLAC indicated that when the probability of uterine rupture was at 0% the TOLAC strategy was preferred if the probability of success was 36.6% or more. When the probability of uterine rupture was at the base value, 0.8%, the TOLAC strategy was preferred as long as the probability of success was 42.6% or more. With the uterine rupture rate set at 1.5% and 3.0%, the probability of success had to be 47.2% and 58.4% or less respectively for the preferred strategy to change to an ERCD. When the probability of success was at the base value, 68.5%, TOLAC was preferred when the probability of rupture was 4.2% or less. When the probability of TOLAC success was 36.0% or less, ERCD was preferred over the entire range of the probability of uterine rupture (0–5.0%).
Figure 1.
Tornado Diagram of Five Variables with Thresholds.
QALY, quality-adjusted life years; TOLAC, trial of labor after a previous cesarean; ERCD, elective repeat cesarean delivery
Monte Carlo simulation of the five sensitive variables at cost-effectiveness thresholds of $25, $50 and $100 thousand found TOLAC to be preferred 91.2%, 91.9% and 91.1% of the time, respectively.
Discussion
Under base-case assumptions, after one cesarean with a low transverse incision, TOLAC was the most cost-effective strategy and would save approximately $138.6 million per 100,000 women when compared with ERCD. This analysis improves upon prior analyses in several ways. First, we utilized an observational study specifically conducted to answer questions related to modes of delivery after a previous cesarean to obtain maternal and perinatal outcome probabilities. Second, the probabilities used for the decision analytic model were derived using propensity sores. This allowed us to uniquely develop TOLAC and ERCD groups with well balanced baseline covariates with minimal bias. Moreover, whereas previous studies have relied on cost data that was derived from a single institution, the cost data for this analysis were obtained from US national sources, the AHRQ and the AMA.
Of the two economic reports noted to have the most methodological rigor in the 2003 AHRQ technology report, the present analysis is most comparable to the manuscript by Chung et al. since both consider outcomes of the current pregnancy.3 A main criticism of the Chung et al. work was that minimal sensitivity analysis was used.1 The present analysis demonstrates that although TOLAC is cost-effective under many circumstances, this conclusion is highly dependent upon several key variables which, if altered sufficiently, result in the alternate strategy of ERCD being preferred.
Indeed, this finding reveals that the cost-effectiveness of TOLAC is dependent upon the characteristics of women who choose to attempt a vaginal birth. For example, TOLAC will no longer be cost-effective when the chance of VBAC success is low. One-way sensitivity analyses found TOLAC not cost-effective when the probability of successful TOLAC was below 42%.
Limitations of this analysis should be noted. For feasibility and clarity, the maternal and infant outcome probabilities were based on a hierarchy and therefore no more than one complication could be experienced by an individual. However, the effect this would have on the cost-effectiveness results would be de minimus at best since less than 0.03% and 2.5% of the mothers and neonates, respectively, experienced more than one outcome. In addition, this study did not include the potential long-term maternal outcomes of fecal and urinary incontinence due to the fact that the marginal increase in these outcomes due to TOLAC is not well known.1, 28–29 The 2003 AHRQ Evidence report specifically criticized Chung et al. for including incontinence because no conclusive evidence linking the probability of incontinence outcomes to delivery approach could be found.1 Unfortunately, conclusive evidence is still lacking and consequently they were not incorporated in the present model.
This analysis also excluded the important long term outcomes of placenta accreta and previa in subsequent pregnancies. The determination of the exact cost-effectiveness over the life course would require a separate more complex model taking into account uncertainties of future reproduction. Nevertheless, including these data inputs would only make the cost effectiveness of TOLAC greater. Additionally, the base case of this analysis did not include women undergoing labor induction and instead was predicated on women in spontaneous labor and included probabilities of success and rupture consistent with this type of labor. The sensitivity analysis, however, allows insight into whether induction would be cost-effective as well. The 2010 AHRQ evidence report estimated that the frequency of rupture for those induced at any gestational age was approximately 1.5%.30 Even at this frequency, the preferred strategy changes to an ERCD only when the probability of success was approximately less than 47%. Most women induced, and particularly those with a favorable cervix, would be expected to have a chance of success greater than that threshold.
In conclusion, using an analytic framework designed to minimize bias, we found that a trial of labor after one previous low transverse cesarean is more cost-effective than an ERCD under a wide range of circumstances. This conclusion is strengthened in particular for women who undergo a spontaneous TOLAC with a high chance of success.
Table A1.
Additional Detail on Maternal Cost Estimates
| Maternal Outcomes | Hospital | Obstetrician | Anesthesia | Subtotal | Maternal | Caregiver | Total |
|---|---|---|---|---|---|---|---|
|
| |||||||
| Uterine rupture | 2,325 | 728 | 3,840 | 1,008 | |||
| Maternal death | 20,000 | 23,053 | 27,901 | ||||
| Thromboembolism | 11,218 | 14,271 | 19,119 | ||||
| Hysterectomy | 12,486 | 15,539 | 20,387 | ||||
| Operative injury | 8,496 | 11,549 | 16,397 | ||||
| Wound infection | 10,184 | 13,237 | 18,085 | ||||
| Endometritis | 10,348 | 13,401 | 18,249 | ||||
| Maternal no other morbidity | 5,964 | 9,017 | 13,865 | ||||
| Failed TOLAC | 2,325 | 728 | 3,840 | 1,008 | |||
| Maternal death | 20,000 | 23,053 | 27,901 | ||||
| Thromboembolism | 10,475 | 13,528 | 18,376 | ||||
| Hysterectomy | 11,743 | 14,796 | 19,644 | ||||
| Operative injury | 7,753 | 10,806 | 15,654 | ||||
| Wound infection | 9,441 | 12,494 | 17,342 | ||||
| Endometritis | 9,605 | 12,658 | 17,506 | ||||
| Maternal well discharge | 5,221 | 8,274 | 13,122 | ||||
| Successful TOLAC | 2,068 | 297 | 1,280 | 432 | |||
| Maternal death | 20,000 | 22,365 | 24,077 | ||||
| Thromboembolism | 9,260 | 11,625 | 13,337 | ||||
| Hysterectomy | 10,528 | 12,893 | 14,605 | ||||
| Operative injury | 6,538 | 8,903 | 10,615 | ||||
| Wound infection | 8,226 | 10,591 | 12,303 | ||||
| Endometritis | 8,390 | 10,755 | 12,467 | ||||
| Maternal well discharge | 4,006 | 6,371 | 8,083 | ||||
| ERCD | 2,222 | 342 | 3,840 | 1,008 | |||
| Maternal death | 20,000 | 22,564 | 27,412 | ||||
| Thromboembolism | 9,198 | 11,762 | 16,610 | ||||
| Hysterectomy | 10,466 | 13,030 | 17,878 | ||||
| Operative injury | 6,476 | 9,040 | 13,888 | ||||
| Wound infection | 8,164 | 10,728 | 15,576 | ||||
| Endometritis | 8,328 | 10,892 | 15,740 | ||||
| Maternal well discharge | 3,944 | 6,508 | 11,356 | ||||
Currency in dollars ($)
Hospital costs were obtained from HCUPnet17, ICD-9 codes; ERCD, 669.71; rupture, 665.11; failed TOLAC, 660.61; successful TOLAC, 654.21; thromboembolism, 671.44; hysterectomy, 68.49 (procedure code); operative injury, 665.54; wound infection, 674.34; endometritis 670.02; maternal well discharge represents the cost of the mode of delivery whereas maternal outcomes represent the cost for the mode of delivery plus the cost of the outcome. For example, the cost of an ERCD was $3944 and the cost of thromboembolism was $5254 resulting in an ERCD with thromboembolism cost of $9198
Obstetrician costs were obtained from the 2010 American Medical Association Current Procedural Terminology codes adjusted to 2009 dollars.18 ERCD CPT code 59510; Rupture 59618; Failed TOLAC 59618; Successful TOLAC 59610
Anesthesia costs were obtained from Chung et al. by mode of delivery and translated into 2009 dollars.3
Maternal and Caregiver postpartum opportunity costs were derived from the Bureau of Labor Statistics using the 2009 median hourly wage and salary averages for women 25 to 34 years old and for all sexes 16 years and older, respectively.19 For ERCD, rupture, failed TOLAC maternal opportunity costs were included for 6 weeks at 40 hours per week at $16 per hour whereas for caregiver costs were included for 7 days, 8 hours per day at $18 per hour. For successful TOLAC, maternal opportunity costs were included for 2 weeks, 40 hours per week at $16 per hour and caregiver costs were included for 3 days, 8 hours per day at $18 per hour.
Table A2.
Additional Detail on Infant Cost Estimates
| Infant Outcome | Hospital | Pediatrician | Total |
|---|---|---|---|
|
| |||
| Failed TOLAC/ERCD | |||
| Neonatal death | 50,000 | 2,151 | 52,151 |
| CP (Failed TOLAC only) | 73,438 | 8,976 | 82,414 |
| HIE | 36,719 | 4,158 | 40,877 |
| Sepsis | 5,597 | 2,954 | 8,551 |
| RDS | 23,317 | 2,151 | 25,468 |
| TTN | 6,509 | 2,151 | 8,660 |
| Acidemia | 5,183 | 2,151 | 7,334 |
| Infant well discharge | 771 | 124 | 895 |
| Uterine rupture | |||
| Neonatal death | 50,000 | 2,151 | 52,151 |
| CP | 73,438 | 8,976 | 82,414 |
| HIE | 36,719 | 4,158 | 40,877 |
| Sepsis | 5,597 | 2,954 | 8,551 |
| RDS | 23,317 | 2,552 | 25,869 |
| TTN | 6,509 | 2,552 | 9,061 |
| Acidemia | 5,183 | 2,552 | 7,735 |
| Infant well discharge | 771 | 156 | 927 |
| Successful TOLAC | |||
| Neonatal death | 50,000 | 2,151 | 52,151 |
| CP | 73,438 | 8,976 | 82,414 |
| HIE | 36,719 | 4,158 | 40,877 |
| Sepsis | 5,597 | 2,954 | 8,551 |
| RDS | 23,317 | 2,151 | 25,468 |
| TTN | 6,509 | 2,151 | 8,660 |
| Acidemia | 5,183 | 2,151 | 7,334 |
| Infant well discharge | 771 | 91 | 862 |
Currency in dollars ($); TOLAC, trial of labor after a previous cesarean; CP, cerebral palsy; HIE, hypoxic ischemic encephalopathy; RDS, respiratory distress syndrome; TTN, transient tachypnea of the newborn
Hospital costs were obtained from HCUPnet17, ICD-9 codes; HIE, 768.7; infection, 771.81; RDS, 769; TTN, 770.6; infant well 795 (DRG)
Pediatrician costs based on length of stay from the Cesarean Registry and 2010 CPT codes18 adjusted to 2009 dollars; 99460, 99466, 99468, 99469; for no other infant morbidity, pediatrician coverage was assigned in the base-case as 4 days for rupture, 3 days for ERCD and failed TOLAC, 2 days for successful TOLAC. For ERCD, rupture, failed TOLAC, an additional day was added for the outcomes RDS, TTN, acidemia and an additional 2 days for successful TOLAC. For all modes of delivery, infection, HIE and CP were assumed to have a pediatrician coverage of 6, 9 and 21 days respectively. CP costs through hospital discharge.
Acknowledgments
The project described was supported by grants from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) of the National Institutes of Health (NIH) [HD21410, HD21414, HD27860, HD27861, HD27869, HD27905, HD27915, HD27917, HD34116, HD34122, HD34136, HD34208, HD34210, HD40500, HD40485, HD40544, HD40545, HD40560, HD40512, and HD36801] and its contents are solely the responsibility of the authors and do not necessarily represent the official view of NICHD or the NIH.
The authors thank the following core committee Network members who participated in protocol development and coordination between clinical research centers (Francee Johnson, BSN, Julia Gold BSN/APN), data management (Sandra Meadows), protocol/data management and statistical analysis (Elizabeth Thom, PhD and John C. Hauth, MD), and manuscript review (Yasser El-Sayed, MD).
Abbreviations
- AHRQ
Agency for Healthcare Research and Quality
- TOLAC
Trial of labor after a previous cesarean
- ERCD
Elective repeat cesarean delivery
- QALY
Quality-adjusted life-years
- TTN
Transient tachypnea of the newborn
- RDS
Respiratory distress syndrome
- HIE
Hypoxic ischemic encephalopathy
- CP
Cerebral palsy
- HCUPnet
AHRQ’s Healthcare Cost and Utilization Project Nationwide Inpatient Sample
- ICD-9
International Classification of Diseases codes
- CPT
Current Procedural Terminology
- AMA
American Medical Association
In addition to the authors, other members of the Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal-Fetal Medicine Units Network are as follows:
The George Washington University Biostatistics Center — E. Thom, H. Juliussen-Stevenson, M. Fischer, L. Leuchtenburg
Northwestern University — A. Peaceman, M. Socol, D. Gradishar, G. Mallett
The Ohio State University — J. Iams, F. Johnson, S. Meadows, H. Walker
University of Alabama at Birmingham — J. Hauth, A. Northen, S. Tate
University of Texas Southwestern Medical Center — S. Bloom, J. Gold, D. Bradford
University of Utah — M. Belfort (Utah Valley Regional Medical Center), F. Porter (Intermountain Healthcare), B. Oshiro (McKay-Dee Hospital Center), K. Anderson (University of Utah Health Sciences Center), A. Guzman (McKay-Dee Hospital Center)
University of Pittsburgh — S. Caritis, K. Lain, M. Cotroneo, D. Fischer, M. Luce
Wake Forest University Health Sciences — P. Meis, M. Harper, M. Swain, C. Moorefield, K. Lanier, L. Steele
Thomas Jefferson University — A. Sciscione, M. DiVito, M. Talucci, M. Pollock
Wayne State University — M. Dombrowski, G. Norman, A. Millinder, C. Sudz, B. Steffy
University of Cincinnati — M. Miodovnik, T. Siddiqi, H. How, N. Elder
Columbia University — M. Miodovnik, F. Malone, M. D’Alton, V. Pemberton, V. Carmona, H. Husami
Brown University — M. Carpenter, H. Silver, J. Tillinghast, D. Catlow, D. Allard
University of Miami — G. Burkett, J. Gilles, J. Potter, F. Doyle, S. Chandler
University of Tennessee — W. Mabie, R. Ramsey
University of Texas at San Antonio — O. Langer, D. Conway, S. Barker, M. Rodriguez
University of North Carolina — K. Moise, K. Dorman, S. Brody, J. Mitchell
The University of Texas Health Science Center at Houston — L. Gilstrap, M. Day, M. Kerr, E. Gildersleeve
Case Western Reserve University-MetroHealth Medical Center — P. Catalano, C. Milluzzi, B. Slivers, C. Santori
University of Chicago — A. Moawad, J. Hibbard, P. Jones, M. Ramos-Brinson, M. Moran, D. Scott
Eunice Kennedy Shriver National Institute of Child Health and Human Development — D. McNellis, K. Howell, S. Tolivaisa
MFMU Steering Committee Chair (Vanderbilt University Medical Center) - S. Gabbe
Footnotes
Disclosure: None of the authors have a conflict of interest.
Presented at the 32nd Annual Meeting of the Society for Maternal-Fetal Medicine. February 6-11, 2012. Dallas, TX.
Reprints will not be available
References
- 1.Guise J-M, McDonagh M, Hashima J, Kraemer DF, Eden KB, Belin M, et al. Vaginal birth after cesarean (VBAC). Evidence report/technology. Rockville, MD: Agency for Healthcare Research and Quality; Mar, 2003. assessment No. 71 (prepared by the Oregon Health & Science University Evidence-based Practice Center under Contract no. 290-97-0018). AHRQ Publication No. 03-E018. [Google Scholar]
- 2.Grobman WA, Peaceman AM, Socol ML. Cost-effectiveness of elective cesarean delivery after one prior low transverse cesarean. Obstet Gynecol. 2000;95:745–751. doi: 10.1016/s0029-7844(00)00783-3. [DOI] [PubMed] [Google Scholar]
- 3.Chung A, Macario A, El-Sayed YY, Riley ET, Duncan B, Druzin ML. Cost-effectiveness of a trial of labor after previous cesarean. Obstet Gynecol. 2001;97:932–941. doi: 10.1016/s0029-7844(01)01355-2. [DOI] [PubMed] [Google Scholar]
- 4.Macones GA, Peipert J, Nelson DB, Odibo A, Stevens EJ, Stamilio M, et al. Maternal complications with vaginal birth after cesarean delivery: A multicenter study. Am J Obstet Gynecol. 2005;193:1656–1662. doi: 10.1016/j.ajog.2005.04.002. [DOI] [PubMed] [Google Scholar]
- 5.Landon MB, Hauth JC, Leveno KJ, Spong CY, Leindecker S, Varner MW, et al. Maternal and perinatal outcomes associated with a trial of labor after prior cesarean delivery. N Engl J Med. 2004;351(12):2581–2589. doi: 10.1056/NEJMoa040405. [DOI] [PubMed] [Google Scholar]
- 6.McMahon MJ, Luther ER, Bowes WA, Jr, Olshan AF. Comparison of a trial of labor with an elective repeat cesarean section. N Engl J Med. 1996;335:689–695. doi: 10.1056/NEJM199609053351001. [DOI] [PubMed] [Google Scholar]
- 7.Flamm BL, Goings JR, Liu Y, Wolde-Tsadik G. Elective repeat cesarean delivery versus trial of labor: a prospective multicenter study. Obstet Gynecol. 1994;83:927–932. doi: 10.1097/00006250-199406000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Gold MR, Siegel JE, Russell LB, Weinstein MC for the Panel on Cost-Effectiveness in Health and Medicine. Cost-Effectiveness in Health and Medicine. New York, NY: Oxford University Press; 1996. p. 6. [Google Scholar]
- 9.Spong CY, Landon MB, Gilbert S, Rouse DJ, Leveno KJ, Varner MW, et al. Risk of uterine rupture and adverse perinatal outcome at term after cesarean delivery. Obstet Gynecol. 2007;110(4):801–807. doi: 10.1097/01.AOG.0000284622.71222.b2. [DOI] [PubMed] [Google Scholar]
- 10.Cesarean delivery on maternal request. ACOG Committee Opinion No.394. American College of Obstetricians and Gynecologists. Obstet Gynecol. 2007;110:1501–1514. doi: 10.1097/01.AOG.0000291577.01569.4c. [DOI] [PubMed] [Google Scholar]
- 11.Induction of labor. ACOG Practice Bulletin No. 107. American College of Obstetricians and Gynecologists. 2009;114:386–397. doi: 10.1097/AOG.0b013e3181b48ef5. [DOI] [PubMed] [Google Scholar]
- 12.Grobman WA, Gilbert S, Landon MB, Spong CY, Leveno KJ, Rouse DJ, et al. Outcomes of induction of labor after one prior cesarean. Obstet Gynecol. 2007;109:262–269. doi: 10.1097/01.AOG.0000254169.49346.e9. [DOI] [PubMed] [Google Scholar]
- 13.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 14.Gilbert SA, Grobman WA, Landon MB, Spong CY, Rouse DJ, Leveno KJ, et al. Elective repeat cesarean delivery compared with spontaneous trial of labor after a prior cesarean delivery: a propensity score analysis. Am J Obstet Gynecol. 2012;206:311, e1–9. doi: 10.1016/j.ajog.2012.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baldawi N, Felix JF, Kurinczuk JJ, Dixon G, Watson L, Keogh JM, et al. Cerebral palsy following term newborn encephalopathy: a population-based study. Dev Med Child Neurol. 2005;47:293–298. doi: 10.1017/s0012162205000575. [DOI] [PubMed] [Google Scholar]
- 16.Casella G. Refining binomial confidence intervals. Can J Stat. 1986;14:113–129. [Google Scholar]
- 17.HCUPnet. Healthcare Cost and Utilization Project. Agency for Healthcare Research and Quality; Rockville, MD: [Accessed July 7, 2011]. Available at: http://hcupnet.ahrq.gov/ [Google Scholar]
- 18.American Medical Association. [Accessed September 28, 2010]; Available at: https://catalog.ama-assn.org/Catalog/cpt/cpt_search.jsp.
- 19.United States Department of Labor, Bureau of Labor Statistics. [Accessed November 6, 2010]; Available at: http://www.bls.gov/cps/cpswktabs.htm.
- 20.CDC. Economic costs associated with mental retardation, cerebral palsy, hearing loss, and vision impairment-United States, 2003. MMWR. 2004;53(3):57–59. [PubMed] [Google Scholar]
- 21.Katz RT. Life expectancy for children with cerebral palsy and mental retardation: implications for life care planning. NeuroRehabilitation. 2003;18:261–270. [PubMed] [Google Scholar]
- 22.Cerebral Palsy Source. [Accessed October 25, 2009]; Available at: http://www.cerebralpalsysource.com/About_CP/life_cp/index.html.
- 23.Haddox AC, Teutsch SM, Corso PS. Prevention effectiveness a Guide to Decision Analysis and Economic Evaluation. New York, NY: Oxford University Press; 2003. p. 115. [Google Scholar]
- 24.United States Department of Labor, Bureau of Labor Statistics. [Accessed July 7, 2011]; Available at: http://www.bls.gov/cpi/
- 25.Harris RA, Washington AE, Nease RF, Kupperman M. Cost utility of prenatal diagnosis and the risk-based threshold. The Lancet. 2004;363:276–282. doi: 10.1016/S0140-6736(03)15385-8. [DOI] [PubMed] [Google Scholar]
- 26.Carroll AE, Downs SM. Comprehensive cost-utility analysis of newborn screening strategies. Pediatrics. 2006;117:S287–S295. doi: 10.1542/peds.2005-2633H. [DOI] [PubMed] [Google Scholar]
- 27.Arias E. United States life tables, 2006. National vital statistics reports. 21. Vol. 58. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 28.NIH State-of-the-Science Conference Statement on Cesarean Delivery on Maternal Request. NIH Consens Sci Statements. 2006 Mar 27–29;23(1):1–29. [PubMed] [Google Scholar]
- 29.Vintzileos AM, Beazoglou T. Design, execution, interpretation, and reporting of economic evaluation studies in obstetrics. AM J Obstet Gynecol. 2004;191:1070–1076. doi: 10.1016/j.ajog.2004.05.021. [DOI] [PubMed] [Google Scholar]
- 30.Guise JM, Eden K, Emeis C, Denman MA, Marshall N, Fu RR, et al. Vaginal birth after cesarean: new insights. Evidence/report technology. Rockville, MD: Agency for Healthcare Research and Quality; Mar, 2010. assessment no. 191. (Prepared by the Oregon Health & Science University Evidence-based Practice Center under contract no. 290-2007-10057-I. AHRQ publication no. 10-E003. [Google Scholar]