Abstract
This study compared pretreatment addiction severity profiles of 339 abusers in three diagnostic groups: cocaine dependence only (CO), cocaine dependence with substance-induced major depression (SIMD), and cocaine dependence with independent major depression (IMD). Depressed subjects reported more severe problems than non-depressed subjects across numerous domains, regardless of diagnostic etiology. These findings support the need for specialized treatment approaches targeting depressive symptoms or life stress for cocaine-dependent patients with IMD or SIMD, though patients with IMD may require additional attention for chronic and comorbid psychiatric and medical problems.
INTRODUCTION
Comorbid depression in individuals with cocaine dependence is common1 and associated with greater psychosocial difficulties than cocaine dependence alone.2–4 Because the clinical characteristics associated with comorbid depression may interact with treatment, it is important to understand the clinical profiles of single diagnosis and dual diagnosis cocaine users.
Comorbid depression manifests as either primary (independent) or secondary (substance-induced), but the clinical relevance of this distinction for cocaine dependence remains unclear and relatively understudied. Cocaine abusers with current cocaine-induced depression have been shown to be less depressed than those with independent major depression5,6 and not different from those without a mood disorder.6 In these studies, a cocaine-induced depression diagnosis required only the presence of clinically significant depressed mood or anhedonia. Thus, it is unclear whether individuals who currently meet the temporal (ie, two or more weeks) and symptomatic (ie, at least five symptoms) criteria of major depression demonstrate differing clinical profiles depending on depressive etiology.
Thus, the substance-induced vs. independent depression distinction in cocaine dependence is of considerable clinical interest but has generated limited empirical conclusions. To address remaining questions from earlier research, the present study examined clinical profiles across Addiction Severity Index (ASI) problem areas (medical, employment, drug use, alcohol use, legal, family/social, and psychiatric) in three diagnostic groups:
cocaine dependence only (CO)
cocaine dependence with current substance-induced major depression (SIMD)
cocaine dependence with current independent major depression (IMD)
Profile analysis (PA)7 was used as the primary analytic technique to evaluate differences between diagnostic groups across the ASI domains. PA is a MANOVA-based tool that allows the examination of group differences over a set of dependent variables. PA tests three hypotheses regarding the shape, level, and flatness of profiles. If group profiles are different in shape (the rejection of the parallelism hypothesis of PA), it suggests that groups have different domains that are particularly problematic. Thus, the rejection of the parallelism hypotheses suggests group differences in quality. If the profile of at least one group is elevated or depressed in comparison with the others (the rejection of the levels hypothesis), it suggests differences in overall severity. If profiles are uneven across the ASI domains (the rejection of the flatness hypothesis), it suggests that there are particular domains that are especially problematic for all groups.
Based upon prior findings2–4 and the projected differences between SIMD and IMD patients due to differing etiology, asymmetrical profile shapes were expected across groups, leading to the rejection of the parallelism hypothesis of PA. Specifically, the IMD group was expected to report more severe problems in non-substance use domains due to psychosocial stressors precipitating mood symptoms, as compared to the SIMD group, in which cocaine-evoked physiological changes are thought to precipitate depressive symptoms. It was also hypothesized that the IMD group would display higher levels of psychiatric difficulty, followed by the SIMD and CO groups, respectively; this was based on the expectation that IMD patients are more likely to have comorbid psychiatric problems (as many individuals with primary depression do), whereas SIMD individuals experience primarily mood symptoms. To further characterize these three groups, the associations of depressive diagnostic status with other relevant diagnostic, substance use, and psychiatric variables were examined.
METHOD
Participants and Procedures
Data for the present study were collected as part of larger treatment studies for cocaine dependence and comorbid cocaine dependence and depression conducted at the Treatment Research Clinic (TRC) in Houston, Texas. The TRC is a university medical center-based research facility.8 IMD and SIMD participants in the current sample were drawn primarily from two larger treatment studies for comorbid cocaine dependence and major depression, while the remaining participants, including all of the CO participants, were drawn from larger treatment studies for cocaine dependence only. All studies used the same advertisement and phone-screening procedures and employed nearly identical intake procedures and eligibility criteria, with the exception of the depressive diagnosis criteria. Participants were cocaine-dependent, English-speaking, between the ages of 18 and 50, able to participate in 12 weeks of outpatient treatment, and competent to give informed consent. Prior to enrollment, potential participants were excluded if they met diagnostic criteria for other current DSM-IV substance use disorders (except nicotine, cannabis, and alcohol) or non-substance use disorders (except major depression), used psychotropic medications, or experienced unstable or serious medical illnesses. All participants signed an informed consent form that was reviewed and approved by the Committee for the Protection of Human Subjects of The University of Texas—Houston, Health Science Center.
Potential subjects took part in a two-week intake evaluation process to determine study eligibility, which included a physical examination, laboratory work-up, HIV and TB testing, structured clinical interviews, and self-report instruments. All participants were of outpatient status at the onset of treatment. Participants were reimbursed ($5/day) for travel to the clinic and completion of study assessment procedures. Of the initial sample of 417 participants, 76 were excluded because of incomplete data on ASI or diagnostic variables, resulting in a final sample with 339 participants (CO = 179, SIMD = 57, and IMD = 103). To examine whether there were any systematic differences between the 76 excluded participants and the 339 participants in the final sample, status (excluded vs. included) by diagnostic group interactions (CO vs. SIMD vs. IMD) were examined on the seven ASI composite scores. A 2 × 3 MANOVA showed no main effect of status, λ = 0.98, F(7, 392) = .88, p = .52, or status by group interaction, λ = 0.96, F(14, 784) = 1.26, p = .23, suggesting the absence of systematic bias in the selection of participants for the current study.
Measures
Diagnosis
Current and past diagnostic information was obtained through the Structured Clinical Interview for the DSM-IV (SCID).9 All Axis-I and Axis-II modules for borderline, dependent, and antisocial personality disorders were administered. Masters and doctoral level clinicians conducted SCID assessments after undergoing training to establish competence and interrater reliability. Provisional SCID-based diagnoses were confirmed by the study psychologist or psychiatrist.
For patients who met criteria for a current major depressive episode, an additional evaluation was performed to make the differential diagnosis of independent or cocaine-induced major depression. The SCID module includes a detailed set of queries to assess the possible etiological role of substance use in a major depressive episode. A diagnosis of IMD was assigned to patients who provided evidence of past depression in the absence of drug use, reported symptoms substantially in excess of what would be expected given the severity of substance use, or reported that the onset of the current depressive episode preceded cocaine use and was not exclusively associated with cocaine use initiation or increased use of cocaine. A diagnosis of SIMD was given when no evidence of a depressive episode without drug use was reported, the onset of the current depressive episode developed within a month of cocaine intoxication or withdrawal, and depressive severity was in accordance with the amount or duration of use.
Clinical Characteristics
Author-constructed forms were administered to collect sociodemographic information. The ASI was used to assess severity of difficulty in seven areas: medical, employment, drug use, alcohol use, legal, family/social, and psychiatric. In each area, a composite score ranging from 0.00 (no problem) to 1.00 (extremely severe problem) was computed. All interviewers received standard ASI training procedures and underwent ongoing supervision. The ASI has demonstrated good internal consistency, stability, and interrater reliability in various substance-abusing samples.10,11
A composite measure of cocaine use severity, based on McKay et al.'s12 methods of categorizing treatment outcomes and their sensitivity to group differences, was used. This composite score reflects cocaine problem severity in the past 30 days and has demonstrated strong associations with measures of baseline cocaine use and treatment outcomes.12,13 This measure was constructed from four self-reported items in the ASI: days of cocaine use in the past 30 days, days experiencing drug-related (cocaine) problems in the past 30 days, amount bothered by drug-related (cocaine) problems in the past 30 days, and self-rating of the importance of treatment for drug-related (cocaine) problems. Each item was rescaled to range from 0 to 1 by dividing each raw score by its maximum possible score (eg, the maximum score for days of cocaine use in the past 30 days is 30). These values were averaged to create a composite with a range from 0.00 (no problem) to 1.00 (severe problem). Internal consistency of this four-item composite was adequate (α = .67).
The severity of depression was assessed by the Beck Depression Inventory (BDI).14
Data Analysis
PA7 was used as the primary analytic technique, with diagnostic status serving as the group variable and the seven ASI composite scores serving as the set of dependent (profile) variables. Prior investigations have demonstrated that PA is a useful tool for investigating group differences in substance-abusing populations.15 In PA, three main hypotheses can be tested:
The parallelism hypothesis (shape) states that the patterns of values over the variables are the same for each group, although some groups may be elevated or depressed in comparison to others. Rejection of this hypothesis indicates that the shape of the profile for at least one group differs from the others and supports the position that there are group differences in kind.
The levels hypothesis (magnitude) states that group averages over the profile variables are the same, regardless of whether individuals score differently across profile variables. Rejection implies that the profile of at least one group, although parallel to the others, is elevated or depressed in comparison. This supports the position that there are group differences in magnitude of profiles.
The flatness hypothesis states that all individuals score the same across profile variables, regardless of whether groups differ in magnitude. Rejection implies that subjects are notably high or low on any of the profile variables.
The SAS GLM Procedure16 program was used for PA, with the multivariate repeated measures option to test profile differences. To follow up on PA hypothesis testing, between-subjects ANOVA and Tukey's HSD procedures were used to assess for overall and pairwise group differences on ASI variables. Separate analyses were performed using the SAS GLM and FREQ procedure16 programs to assess group differences on sociodemographic, diagnostic, and substance use characteristics. Alternative PA follow up analyses were performed using sociodemographic characteristics with group differences as covariates.
A family-wise probability level of 0.05 (two-tailed) was selected a priori to indicate rejection of PA hypotheses and tests of overall group differences. If univariate omnibus tests showed statistically significant differences, pairwise chi-square tests or Tukey's HSD procedure was used to assess for pairwise group differences. Tukey's HSD procedure or Bonferonni corrections were applied when appropriate to control family-wise type-I error rates from exceeding 0.05 on post-hoc analysis. All count variables were logarithmically transformed for hypothesis testing; however, means were back transformed for the presentation of descriptive statistics.
RESULTS
Sample Characteristics
The groups differed significantly (p < .05) with regard to ethnicity and employment status (see Table 1). Of the entire sample, 12.8% and 7.4% met criteria for current alcohol and cannabis dependence, respectively. Rates of lifetime alcohol dependence were highest in the IMD group. There were no differences in the prevalence of current alcohol dependence or lifetime and current cannabis dependence. The IMD group had significantly higher prevalence rates than the CO group for all three personality disorders assessed. The groups differed significantly on current and lifetime drug use. For cocaine, the SIMD group reported more days of using in the past 30 compared to the CO group. For lifetime cocaine use, the SIMD group reported more years of using than the IMD group. Depressed groups scored higher on the cocaine severity composite than the CO group but did not differ from each other (see Table 1).
TABLE 1.
Sociodemographic and clinical characteristics, expressed as percents or means (SD)
| Variable | CO (n = 179) | SIMD (n = 57) | IMD (n = 103) | F/χ 2 |
|---|---|---|---|---|
| Sociodemographics | ||||
| Age | 39.6 (10.7) | 38.4 (7.1) | 38.2 (7.5) | ns |
| Education | 12.6 (2.4) | 12.4 (1.9) | 12.9 (2.3) | ns |
| Gender (%) | — | — | — | ns |
| Male | 79.9 | 73.7 | 81.6 | — |
| Female | 20.1 | 26.3 | 18.4 | — |
| Married (%) | 40.0 | 36.8 | 32.7 | ns |
| Race (%) | — a | — ab | — b | 25.03** |
| White | 21.8 | 28.1 | 48.5 | — |
| Black | 70.1 | 63.2 | 41.8 | — |
| Hispanic | 7.3 | 8.8 | 9.7 | — |
| Employed (%) | 55.5a | 39.2a | 40.7a | 7.4* |
| DSM-IV Diagnosis | ||||
| Alcohol dependence (% ) | ||||
| Current | 9.0 | 17.9 | 16.8 | ns |
| Lifetime | 26.8a | 43.2b | 52.5b | 19.39** |
| Cannabis dependence (% ) | ||||
| Current | 7.2 | 7.0 | 7.8 | ns |
| Lifetime | 17.2 | 21.0 | 23.8 | ns |
| Personality disorders (% ) | ||||
| Antisocial | 12.4a | 16.7ab | 29.4b | 12.74* |
| Borderline | 3.9a | 11.1ab | 19.6b | 18.00* |
| Dependent | 2.8a | 1.9ab | 10.8b | 9.94* |
| Substance use Characteristics | ||||
| Drug use, days in past 30 | ||||
| Cocaine | 12.7 (8.6)a | 16.3 (9.4)b | 15.2 (9.2)ab | 4.80*** |
| Alcohol | 11.1 (10.2) | 11.2 (10.1) | 8.5 (9.2) | ns |
| Cannabis | 3.5 (7.8) | 6.6 (14.1) | 4.2 (8.8) | ns |
| Lifetime drug use, years | ||||
| Cocaine | 11.5 (6.3)ab | 12.9 (6.6)a | 10.1 (6.5)b | 3.85* |
| Alcohol | 17.9 (9.9) | 16.1 (9.9) | 15.6 (9.3) | ns |
| Cannabis | 10.1 (9.1)b | 14.1 (13.7)a | 10.7 (9.2)ab | 3.59* |
| Cocaine severity composite | 0.64 (0.21)a | 0.76 (0.18)b | 0.78 (0.16)b | 19.19** |
Note. CO = Cocaine Dependence Only; SIMD = cocaine dependence with substance-induced depression; IMD = cocaine dependence with independent major depression. Groups with different letter superscripts demonstrated statistically significant differences when tested by Tukeys’ HSD procedure for pairwise comparisons or pairwise post-hoc Chi-square tests (αFW = .05).
p < 0.05
p < 0.01
p < 0.0001.
Profile Analysis
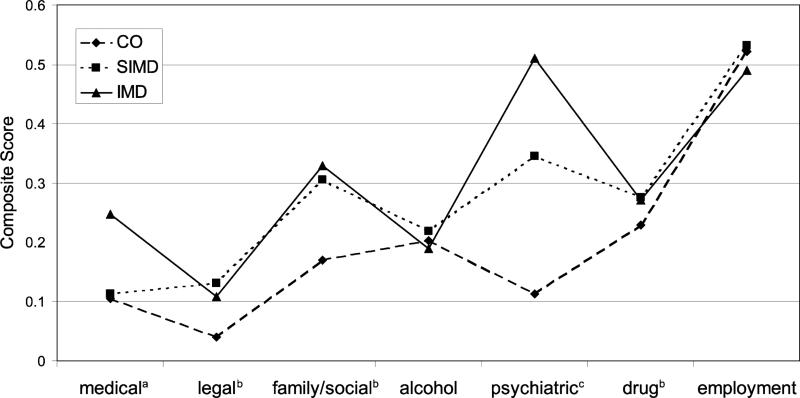
The parallelism hypothesis was rejected, λ = 0.49, F(12, 662) = 23.62, p < 0.0001, partial η2 = .30. Bonferroni-corrected pairwise comparisons indicated that there were clear differences in profile shape among groups (all p's < 0.001). Further analyses led to rejection of both the flatness (λ = 0.49, F[6, 331] = 109.50, p < 0.0001, η2 = .51) and levels (F[2, 336] = 45.59, p < 0.0001, η2 = .21) hypotheses, indicating that reliable differences were found among groups when scores were averaged over all ASI domains and that mean scores differed across domains when groups were collapsed. Figure 1 shows the mean profiles of each of the three diagnostic groups.
FIGURE 1.
Addiction Severity Profiles. CO = Cocaine Dependence only, SIMD = Cocaine Dependence with Substance-Induced Depression, IMD = Cocaine Dependence with Independent Major Depression. *Overall Test was Statistically Significant at p < .05; **Overall Test was Statistically Significant at p < .01. aPost-hoc pairwise contrasts demonstrated significant differences between IMD and SIMD as well as IMD and CO groups. bPost-hoc pairwise contrasts demonstrated significant differences between IMD and CO as well as SIMD and CO groups. cPost-hoc pairwise contrasts demonstrated significant differences between all groups
To better understand the ASI domains in which groups differed, between-group ANOVAs were performed for each composite score. As illustrated in Figure 1, these tests indicated statistically significant overall differences among groups in medical (d = .32), legal (d = .34), family/social (d = .44), psychiatric (d = 1.54), and drug (d = .40) domains, (all ps < 0.001), but no differences in alcohol and employment domains. Pairwise comparisons revealed significant differences between IMD and SIMD groups in medical (d = .44) and psychiatric (d = .96) domains, with the IMD group being more severe. Both IMD and SIMD groups were more severe than CO participants in legal, family/social, and drug domains (see Figure 1 for a more comprehensive description of pairwise comparisons). Employment, race, and other psychiatric diagnosis analyses that varied between groups as covariates did not change the pattern outcomes of any overall or pairwise tests, with the exception that pairwise differences between SIMD and IMD groups on the medical composite fell below significance (p = .09).
Because the ASI psychiatric composite includes several items related to psychiatric symptoms experienced in the past 30 days that are not drug induced, it is possible that artifactual differences between SIMD and IMD groups on the depression item in the ASI may have affected results (ie, SIMD patients by definition are unlikely to endorse depressive symptoms that are not drug-related). Therefore, psychiatric composite scores were reconstructed following the standard formula, though the depression item was omitted from the calculations. The correlation between the adjusted psychiatric composite and the original composite score was very high (r = .99). Results using the newly constructed composite were almost identical to the original analyses [parallelism: λ = 0.55, F(12, 662) = 19.44, p < 0.0001, partial η2 = .26; flatness: λ = .36, F(6, 331) = 98.04, p < 0.0001, η2 = .64; levels: F(2, 336) = 38.81, p < 0.0001, η2 = .19].
Overall differences on the newly constructed psychiatric item were still large (d = 1.39 overall; IMD vs. SIMD: d = .83).
Secondary Analyses
To more closely examine differences in psychiatric severity among groups, individual items used in calculating the ASI psychiatric composite were analyzed (see the results reported in Table 2). The IMD group reported experiencing more days of psychological problems and higher levels of distress about psychological problems, and rated the need for treatment as more important than SIMD and CO groups, respectively. As expected, for specific symptoms experienced in the past 30 days that they felt were not drug-induced, IMD patients were more likely to report serious depression, anxiety or tension, and concentration and memory problems than SIMD and CO patients, respectively. IMD patients were more likely to have suicidal thoughts (either drug-related or independent) than SIMD and CO patients, respectively. More IMD than CO patients had been prescribed medication for psychological problems in the past 30 days. Although reports of suicide attempts were infrequent in the entire sample, the depressed groups were significantly more likely to have attempted suicide in the past 30 days than non-depressed subjects. More SIMD patients indicated having trouble controlling violent behavior in the past 30 days.
TABLE 2.
Psychological and emotional problems experienced in the past thirty days, expressed as percents or means (SD)
| Variable | CO (n = 179) | SIMD (n = 57) | IMD (n = 103) | F/χ 2 |
|---|---|---|---|---|
| Days experiencing psychological problems | 4.72 (8.91)a | 16.81 (10.52)a | 25.05 (8.03)c | 161.6*** |
| Been prescribed medication for psychological problems (%) | 1.1a | 1.8ab | 8.7b | 11.82*** |
| Level of distress about psychological problems | 0.93 (1.43)a | 2.84 (1.40)b | 3.40 (0.87)c | 136.4*** |
| Importance of treatment for psychological problems | 0.98 (1.58)a | 3.14 (1.44)b | 3.68 (0.84)c | 145.6*** |
| Type of psychological problems (%) | ||||
| Serious depression† | 14.4a | 52.6b | 90.3c | 155.2*** |
| Serious anxiety or tension† | 16.1a | 40.4b | 68.0c | 77.1*** |
| Hallucinations† | 1.1 | 0.0 | 1.9 | 1.2 |
| Concentration and memory problems† | 16.1a | 36.8b | 68.9c | 79.8*** |
| Trouble controlling violent behavior | 6.2a | 21.1b | 11.7ab | 8.6* |
| Suicidal thoughts | 3.9a | 17.5b | 40.8c | 62.2*** |
| Suicide attempts | 0.0a | 3.5b | 9.7b | 18.1 |
Note. Items from the psychiatric section of the Addiction Severity Index. CO = cocaine dependence only; SIMD = cocaine dependence with substance-induced major depression; IMD = cocaine dependence with independent major depression. Groups with different letter superscripts demonstrated statistically significant differences when tested by Tukeys’ HSD procedure for pairwise comparisons (αEW = .05) or pairwise post-hoc chi-square tests α = .05.
p < .05
< .001.
Not drug-related.
Differences were found in total BDI scores across groups, F(2, 337) = 20.11, p < .0001: CO (M = 14.4; SD = 10.0); SIMD (M = 25.7; SD = 11.4); IMD (M = 28.8; SD = 10.1). Pairwise tests indicated that SIMD and IMD patients reported more severe depression than CO patients but did not significantly differ from each other.
DISCUSSION
The primary hypothesis of this study was supported. There were differences in the shapes of addiction severity profiles among cocaine-dependent groups; however, differences were not in the expected pattern. Psychosocial stressors related to employment, legal, and family/social sources were similar in IMD and SIMD, with both showing greater severity than the CO group. Taken together, these results suggest that cocaine abusers with major depression have poorer psychosocial functioning than non-depressed cocaine users, regardless of diagnostically determined depressive etiology. However, there are a few notable exceptions.
In line with predictions, IMD patients experienced considerably more overall comorbid psychopathology than the SIMD and CO groups, as evidenced by ASI-psychiatric scores and Axis-II pathology. Item-level analyses of the ASI-psychiatric responses showed that the IMD patients reported more frequent and troubling affective symptoms (eg, anxiety, depression, and suicidal ideation) than the SIMD and CO groups. While subjects with IMD appeared to have a higher prevalence of personality disorders than those with SIMD (p's 0.04–0.17), the combination of the smaller number of patients diagnosed with SIMD and Bonferonni corrections may have reduced the power to detect significant differences in post-hoc pairwise comparisons. An inspection of Table 1 reveals a higher prevalence of antisocial and borderline personality disorder in the IMD group, followed by SIMD and CO groups, respectively. These findings may be related to the criteria used to identify independent depression (ie, the history of recurrent independent major depressive episodes), which might have produced an IMD group that demonstrated more severe and chronic comorbid psychopathology than patients with SIMD and non-depressed patients.
In concordance with previous findings,2–4 both groups with major depression had more overall psychological and emotional distress than individuals diagnosed with cocaine dependence alone. The current results contrast Siqueland et al.'s6 findings that individuals with cocaine-induced mood disorder (ie, clinically significant substance-induced dysphoria or anhedonia) reported psychiatric symptomatology equivalent to those without a mood disorder. The requirement that patients with substance-induced depression meet the temporal and symptomatic criteria of major depression likely contributed to the large differences found between SIMD and CO groups on the ASI psychiatric composite and BDI. Differences between SIMD and CO groups on ASI items assessing “independent” depression and anxiety (see Table 2) suggest that although SIMD patients did not qualify for independent major depression, they appeared to experience some emotional disturbance not related to drug use.
Consistent with recent reviews on the comorbidity of medical illness and depression in non-substance abusing populations,17,18 IMD patients indicated more severe medical problems than CO patients. This suggests that medical problems may serve as a source of stress contributing to depressive symptoms, or that depression may hinder immune system function or lead to poor physical self-care in cocaine abusers.17,18 An interesting finding, however, was that IMD patients reported more medical difficulty than SIMD patients. Katon et al.17 found that high utilizers of medical care were more likely to be diagnosed with recurrent major depressive episodes and chronic dysthymia. Therefore, the current findings may be indicative of the increased chronicity and overall severity of psychiatric distress in IMD subjects in comparison to the other groups.
Observed differences indicated that depressed subjects regardless of depressive etiology had more severe drug problems than non-depressed subjects. A more specific measure of current cocaine severity, which includes one objective (ie, cocaine use in the past 30 days) and three subjective (ie, cocaine problems in the past 30 days, importance of treatment, and amount bothered by drug problems) indices produced similar results. Additional analyses indicated that depressed patients’ beliefs regarding their cocaine severity were elevated in comparison to non-depressed subjects on the more subjective items (all ps < 0.004). These findings correspond with prior investigations revealing that in comparison to non-depressed cocaine abusers, those with depression perceive a greater need for drug abuse treatment, have less abstinence efficacy, and believe that there are more advantages to continued drug use.2,4
Alcohol and employment problems did not differ among groups. This finding contrasts with two prior studies showing that among male veterans entering continuing care and non-treatment-seeking crack-cocaine users from the community, depressed subjects report more alcohol problems.2,3 These samples may differ from the one in the current study, which included subjects who were willing to be randomized to placebo or drug interventions targeting only cocaine dependence or comorbid cocaine dependence and depression. While alcohol dependence was allowed, individuals with more severe alcohol problems might have been deterred. The failure to find differences in employment problems has been reported before3,4 and may be a function of the overall poor functioning of the treatment-seeking cocaine-dependent population, regardless of depressive status.
Rigorous efforts were made to distinguish a substance-induced and independent mood disorder using the DSM-based Structured Clinical Interview for DSM-IV (ie, the SCID). However, the SCID may be problematic for analysis and interpretation of the current data because it assumes a relation between etiology and severity of depression. That is, satisfying the criteria “depressive severity in accordance with the amount of duration of use” suggests a substance-induced depression diagnosis. Conversely, “symptoms substantially in excess of what would be expected given the severity of substance use” suggests an independent disorder. As a result, for individuals at the same level of cocaine use, those reporting higher levels of depression might tend to be diagnosed with independent depression. Because we did not find differences between the SIMD and IMD groups on levels of depression and recent cocaine use, it seems unlikely that problems related to this diagnostic criterion produced the current results. Nevertheless, other diagnostic interviews provide more detailed instruction for differentiating depressive etiology in substance users.19,20 For example, the Psychiatric Research Interview for Substance and Mental Disorders19 concept of a substance-induced disorder is more specific and more carefully assesses the temporal nature of psychiatric symptoms and substance use than the SCID definition. Future examinations of cocaine-induced depressive features using other assessment techniques (eg, other diagnostic interviews, clinician rating scales, and biological measures) may be useful.
There were several limitations to the present study. All of the profile variables were taken from a single assessment tool, the ASI. Ideally, multiple methods of assessment should be utilized to examine clinical profiles to control for potential measurement variability. In addition, the ASI was designed primarily for treatment purposes rather than as a tool for clinical profiling. Nevertheless, it is practical to utilize the ASI to describe clinical profiles of patient groups because this instrument is widely used in substance abuse research and treatment settings. All participants were treatment seeking and most were crack-cocaine smokers (80.2%) without other substance dependence problems, suggesting that the sample may not represent the total population of cocaine-dependent individuals. However, because the current study was primarily concerned with examining the nature of differences between SIMD and IMD, a diagnostically homogenous sample was necessary to control for potential threats to internal validity (eg, the influence of other psychiatric disorders that may be comorbid with depression, or the depressogenic effects of other substances). Future studies may examine whether differences between SIMD and IMD are moderated by comorbid mental or substance use disorders.
Despite challenges in differentiating depressive etiology, the present study reports new information regarding the clinical profiles of DSM-IV-diagnosed, comorbid and single diagnosis cocaine-dependent patients. The present sample of participants with cocaine-induced depression (n = 57) was relatively large in comparison to previous studies (Kush & Sowers,5 n = 31; Siqueland et al.,6 n = 15). In addition, the present utilization of a profile analysis, a unique analytic approach for describing patient groups, may be useful for other investigators interested in the clinical profiles of substance abusers.
The substance-induced versus independent depression distinction is of considerable clinical interest because it is typically thought to have implications for treatment planning, execution, and outcome. Investigations of the differential effect of IMD and SIMD on addiction treatment in heterogeneous substance-dependent samples have produced significant findings that vary across studies and outcome measures but nevertheless implicate depressive diagnostic specificity as a factor affecting substance abuse treatment.21,22 However, results from the current study employing a homogenous cocaine-dependent sample indicate that the distinction may not be as pertinent for clinical practice.
Cocaine abusers with clinical depression (induced or independent) may benefit from acute treatments targeting depressive symptoms or life stress, although patients diagnosed with IMD may require additional attention for chronic and comorbid psychiatric and medical problems. Cocaine abusers with either IMD or SIMD appear to have more negative thoughts about their drug dependence and view their cocaine problems as more severe than patients without mood disorders when entering treatment. Interventions designed to counteract cognitive distortions about drug abuse and motivate behavior change15 may be especially necessary, irrespective of diagnosed depressive etiology. Further investigation of the causes and correlates of independent and substance-induced major depression among cocaine-dependent individuals will inform the development of more refined and targeted treatment approaches for this common comorbidity.
Acknowledgments
This research was supported by grants DA09262 and DA08654 (Dr. Schmitz) from the National Institute on Drug Abuse, Bethesda, Md.
The investigators thank Shelly Sayre and Patricia Hokanson for data collection and management that contributed to this study.
Footnotes
Some data used in this paper were presented at the Association for the Advancement of Behavioral Therapy's annual meeting, New Orleans, Louisiana, November 18–21, 2004.
REFERENCES
- 1.Rounsaville BJ, Anton SF, Carroll K, Budde D. Psychiatric diagnoses of treatment-seeking cocaine abusers. Arch Gen Psychiatry. 1991;48:43–51. doi: 10.1001/archpsyc.1991.01810250045005. [DOI] [PubMed] [Google Scholar]
- 2.Falck RS, Wang J, Carlson RG, Eddy M, Siegal HA. The prevalence and correlates of depressive symptomatology among a community sample of crack-cocaine smokers. J Psychoactive Drugs. 2002;34:281–288. doi: 10.1080/02791072.2002.10399964. [DOI] [PubMed] [Google Scholar]
- 3.McKay JR, Pettinati HM, Morrison R, Feeley M, Mulvaney FD, Gallop R. Relation of depression diagnoses to two-year outcomes in cocaine-dependent patients in a randomized continuing care study. Psychol Addict Behav. 2002;16:225–235. [PubMed] [Google Scholar]
- 4.Schmitz JM, Stotts AL, Averill PM, et al. Cocaine dependence with and without comorbid depression: a comparison of patient characteristics. Drug Alcohol Depend. 2000;60:189–198. doi: 10.1016/s0376-8716(99)00157-x. [DOI] [PubMed] [Google Scholar]
- 5.Kush FR, Sowers W. Acute dually diagnosed inpatients: the use of self-report symptom severity instruments in persons with depressive disorders and cocaine dependence. J Subst Abuse Treat. 1997;14:61–66. doi: 10.1016/s0740-5472(96)00067-0. [DOI] [PubMed] [Google Scholar]
- 6.Siqueland L, Horn A, Moras K, et al. Cocaine-induced mood disorder: prevalence rates and psychiatric symptoms in an outpatient cocaine-dependent sample. Am J Addict. 1999;8:165–169. doi: 10.1080/105504999305974. [DOI] [PubMed] [Google Scholar]
- 7.Tabachnick G, Fidell LS. Using Multivariate Statistics. 4th ed. Allyn & Bacon; Needham Heights, Mass: 2001. [Google Scholar]
- 8.Grabowski J, Arnoni G, Elk R, Rhoades H, Schmitz J. Baseline assessment, study entry, and stabilization: double-blind clinical trials in drug dependence. NIDA Res Monogr. 1997;175:158–181. [PubMed] [Google Scholar]
- 9.First MB, Spitzer RL, Gibbon M, Williams JB. Structured Clinical Interview for DSM-IV Axis I Disorders—Patient Edition (SCID -I=P, Version 2.0) Biometric Research Department; New York: 1995. [Google Scholar]
- 10.Alterman AI, Brown LS, Zaballero A, McKay JR. Interviewer severity ratings and composite scores of the ASI: a further look. Drug Alcohol Depend. 1994;34:201–209. doi: 10.1016/0376-8716(94)90157-0. [DOI] [PubMed] [Google Scholar]
- 11.McLellan AT. New data from the Addiction Severity Index: reliability and validity in three centers. J Nerv Ment Dis. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- 12.McKay JR, Alterman AI, Koppenhaver JM, Mulvaney FD, Bovasso GB, Ward K. Continuous, categorical, and time to event cocaine use outcome variables: degree of intercorrelation and sensitivity to treatment group differences. Drug Alcohol Depend. 2001;62:19–30. doi: 10.1016/s0376-8716(00)00156-3. [DOI] [PubMed] [Google Scholar]
- 13.Reiber C, Ramirez A, Parent D, Rawson RA. Predicting treatment success at multiple timepoints in diverse patient populations of cocaine-dependent individuals. Drug Alcohol Depend. 2002;68:35–48. doi: 10.1016/s0376-8716(02)00103-5. [DOI] [PubMed] [Google Scholar]
- 14.Beck A, Ward C, Mendelson M, Mack J, Erbaugh J. An inventory of measuring depression. Arch Gen Psychiatry. 1961;49:599–608. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 15.Newman CF, Ratto CL. Cognitive therapy of substance abuse. In: Dowd ET, Rugle L, editors. Comparative Treatments of Substance Abuse. Springer Publishing Co; New York: 1999. pp. 96–126. [Google Scholar]
- 16.The SAS System for Windows [computer program]. Version 8.2. SAS Institute Inc.; Cary, NC: 2003. [Google Scholar]
- 17.Katon W, Ciechanowski P. Impact of major depression on chronic medical illness. J Psychosom Res. 2002;53:859–863. doi: 10.1016/s0022-3999(02)00313-6. [DOI] [PubMed] [Google Scholar]
- 18.Cassano P, Fava M. Depression and public health: an overview. J Psychosom Res. 2002;53:849–857. doi: 10.1016/s0022-3999(02)00304-5. [DOI] [PubMed] [Google Scholar]
- 19.Hasin D, Trautman K, Endicott J. Psychiatric research interview for substance and mental disorders: phenomenologically based diagnosis in patients who abuse alcohol or drugs. Psychopharmacol Bull. 1998;34:3–8. [PubMed] [Google Scholar]
- 20.Nunes EV, Goehl L, Seracini A, Deliyannides D. A modification of the Structured Clinical Interview for DSM-III-R to evaluate methadone patients: test-retest reliability. Am J Addict. 1996;5:241–248. [Google Scholar]
- 21.Hasin D, Liu X, Nunes E, McCloud S, Samet S, Endicott J. Effects of major depression on remission and relapse of substance dependence. Arch Gen Psychiatry. 2002;59:375–380. doi: 10.1001/archpsyc.59.4.375. [DOI] [PubMed] [Google Scholar]
- 22.Charney DA, Paraherakis AM, Negrete JC, Gill KJ. The impact of depression on the outcome of addictions treatment. J Subst Abuse Treat. 1998;15:123–130. doi: 10.1016/s0740-5472(97)00183-9. [DOI] [PubMed] [Google Scholar]