Abstract
Objective To investigate the effect of systematic screening for risk factors for ischaemic heart disease followed by repeated lifestyle counselling on the 10 year development of ischaemic heart disease at a population level.
Design Randomised controlled community based trial.
Setting Suburbs of Copenhagen, Denmark
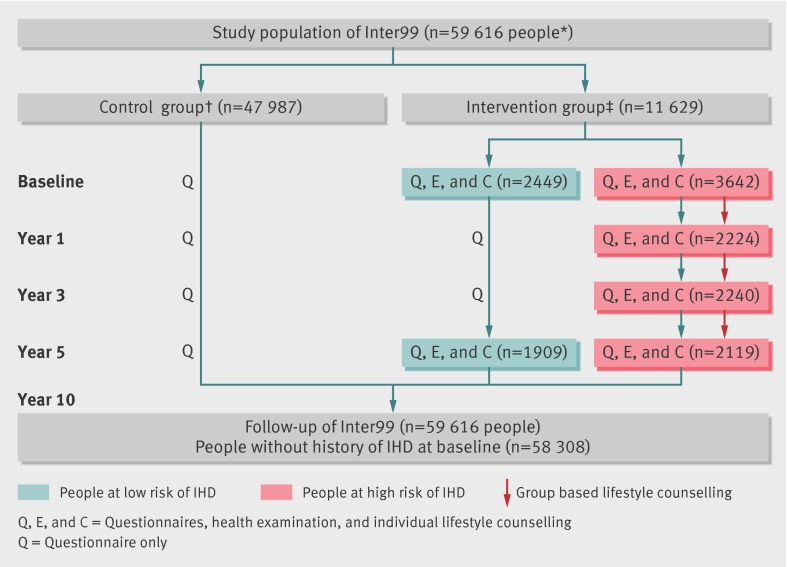
Participants 59 616 people aged 30-60 years randomised with different age and sex randomisation ratios to an intervention group (n=11 629) and a control group (n=47 987).
Intervention The intervention group was invited for screening, risk assessment, and lifestyle counselling up to four times over a five year period. All participants with an unhealthy lifestyle had individually tailored lifestyle counselling at all visits (at baseline and after one and three years); those at high risk of ischaemic heart disease, according to predefined criteria, were furthermore offered six sessions of group based lifestyle counselling on smoking cessation, diet, and physical activity. After five years all were invited for a final counselling session. Participants were referred to their general practitioner for medical treatment, if relevant. The control group was not invited for screening.
Main outcome measures The primary outcome measure was incidence of ischaemic heart disease in the intervention group compared with the control group. Secondary outcome measures were stroke, combined events (ischaemic heart disease, stroke, or both), and mortality.
Results 6091 (52.4%) people in the intervention group participated at baseline. Among 5978 people eligible at five year follow-up (59 died and 54 emigrated), 4028 (67.4%) attended. A total of 3163 people died in the 10 year follow-up period. Among 58 308 without a history of ischaemic heart disease at baseline, 2782 developed ischaemic heart disease. Among 58 940 without a history of stroke at baseline, 1726 developed stroke. No significant difference was seen between the intervention and control groups in the primary end point (hazard ratio for ischaemic heart disease 1.03, 95% confidence interval 0.94 to 1.13) or in the secondary endpoints (stroke 0.98, 0.87 to 1.11; combined endpoint 1.01, 0.93 to 1.09; total mortality 1.00, 0.91 to 1.09).
Conclusion A community based, individually tailored intervention programme with screening for risk of ischaemic heart disease and repeated lifestyle intervention over five years had no effect on ischaemic heart disease, stroke, or mortality at the population level after 10 years.
Trial registration Clinical trials NCT00289237.
Introduction
Ischaemic heart disease remains a leading cause of morbidity and mortality worldwide.1 The main causes of ischaemic heart disease have been well known for decades, and smoking, physical inactivity, and unhealthy diet (the last two partly mediated through high blood pressure, high cholesterol, overweight, and type 2 diabetes) can explain most new cases.2 Studies of selected groups of people have shown that changes in these risk factors influence development of ischaemic heart disease,3 but what is effective at an individual level under ideal circumstances may not work when scaled up to the population level. A systematic review of randomised clinical trials of multiple risk factor interventions for preventing ischaemic heart disease had a modest effect on changes in lifestyle factors, cholesterol concentrations, and blood pressure—the last two mainly owing to the drug treatment used—but no significant effect on long term mortality due to ischaemic heart disease.4 The quality of the studies varied considerably; many studies were old, and few of the published studies provided sufficient detail to replicate the intervention used. Often a theoretical framework for the lifestyle counselling was missing, and in some studies the intensity and duration of interventions were limited. Mostly, only single risk factors were considered without an assessment of absolute risk. Also, a maintenance programme was seldom part of the intervention. Further major drawbacks were the possibility of spill over effects to the control group,5 lack of intention to treat analyses due to loss of follow-up, and no information on non-fatal cases.4
Because of these shortcomings, the Inter99 study was started in 1999.6 The guidelines at that time recommended the Framingham risk score as an appropriate measure of absolute risk taking into account all major risk factors,7 but use of existing foreign risk scores on a Danish population had shown poor results.8 9 A risk score should be developed in a population that resembles the one where it is applied.10 Therefore, we developed the Copenhagen risk score on the basis of data from two large epidemiological studies in the Copenhagen area.11 The relative risks found in the Copenhagen risk score were comparable to international findings,11 but comparing it with the Framingham risk score confirmed that the latter could not be used in a Danish population.12 Furthermore, existing risk scores had the drawback that they were solely based on epidemiological data, which may not correctly estimate the effect of changing risk factor status.13 Therefore, we developed a risk assessment computer program (PRECARD) combining the Copenhagen risk score with data from randomised clinical trials.11 This computer based program, which is now registered as HeartScore and recommended by the European Society of Cardiology,14 was not only a risk score based on national data but also one of the world’s first computer based health educational tools. We developed it as a new pedagogical approach, to be used as an aid to explain risk to participants and to tailor a personal intervention for each participant. We avoided a spill over effect on the control group by means of the randomisation procedure, whereby people who formed the control group were not invited for the screening and not informed about an ongoing intervention. The intensity of the intervention was high, with repeated screening followed by counselling aimed at behavioural changes over a five year period. We used accepted and well described behavioural change theories. The maintenance plan exceeded the five year period, and follow-up was almost complete (except those who emigrated) for the whole study population through registers.
After five years of counselling a significant effect on lifestyle was seen, with a substantial reduction in the prevalence of smoking,15 improved dietary habits,16 sustained physical activity (among men),17 18 and a decrease in binge drinking.19 Furthermore, a significant improvement in self reported mental health and sustained self reported physical health occurred.20 These findings indicate that counselling promotes beneficial changes at the individual level for at least a limited period of time. However, these findings do not show whether screening and lifestyle counselling will reduce ischaemic heart disease at the population level. Although they are part of a randomised trial, the participants represent a selected group of people who have chosen to participate and who attended the follow-up. This leaves the question about a possible effect in the general population unanswered. From a public health perspective, we need to show whether screening for cardiovascular risk and individual counselling actually lead to a reduction in the diseases in question, not only in those who participated in the intervention but in the study population as a whole. This is one of the main criteria for introducing screening programmes in the general population and is a requirement in cancer screening programmes.21 22
The main aim of the Inter99 study was to investigate whether a decrease in the incidence of ischaemic heart disease could be achieved in a general population offered repeated screening for risk of ischaemic heart disease and repeated lifestyle counselling.6 The primary outcome measure was the incidence of ischaemic heart disease. Secondary outcome measures were stroke, combined events (ischaemic heart disease, stroke, or both), and total mortality.
Methods
The study population
The study population has previously been described in detail.6 It comprised all 61 301 people born in 1939-40, 1944-45, 1949-50, 1954-55, 1959-60, 1964-65, and 1969-70 living in 11 municipalities in the southwestern part of Copenhagen County on 2 December 1998 (fig 1). The area had a total population of 330 293. We identified people in the civil registration system, in which all inhabitants in Denmark are registered with unique 10 digit numbers, making the linkage across time and registers very accurate. We selected the birth years and chose the intervention procedure to ensure that participants were as close as possible to 30, 35, 40, 45, 50, 55, and 60 years of age at the baseline examination, which took place between 15 March 1999 and 31 January 2001.6
Fig 1 Flow chart of randomised Inter99 study showing distribution and participation of 59 616 people in various groups during four contacts (baseline, one year, three years, and five years) over five year period. IHD=ischaemic heart disease. *59 993 people were drawn for study population, but 377 emigrated, died, changed their personal identification number, or disappeared before baseline, leaving 59 616. †Random sample of control group (n=5264) received questionnaires. ‡1308 people were randomly allocated to low intensity intervention group; this intervention group was only used to investigate whether lower intensity intervention was effective to achieve changes in lifestyle (described in detail in appendix 1); this group is not included in endpoint analyses, as power calculations were based on large high intensity intervention group, as shown in this figure (for fuller flow chart including low intensity intervention group see www.Inter99.dk)
The 61 301 people were randomised by computer generated random numbers with different randomisation ratios in the different age and sex groups to secure a predefined number in the intervention group including an equal number of men and women at each age and an oversampling of middle aged people (40, 45, 50, and 55 years), as previously described.6 We oversampled people aged 40-55 years, as we expected a higher motivation to change lifestyle in this age group, in which early symptoms often start to manifest. A total of 11 708 people were allocated to the intervention group and 48 285 to the control group (a small group of 1308 people were randomly allocated to a low intensity intervention group to investigate whether a less comprehensive lifestyle intervention had similar effect on lifestyle changes as the planned high intensity intervention; this group will not be dealt with in this paper but is described in web appendix 1). People in the control group had no knowledge of an ongoing intervention.
With an expected participation rate of 70%, we calculated that a difference in 10 year incidence of ischaemic heart disease between the intervention and control groups of 15% should be detectable with a type 1 error of 0.05 and 1–power of 0.20.6
Each person was given a date indicating the time of start of the 10 year observational period. For participants in the intervention group, the date of the first examination at baseline was the start date. Invitations followed a systematic procedure starting with people born on 1 January and ending with those born on 31 December. We defined the start date for non-participants and for people in the control group (who were not invited) born in a specific month as the median date of that month, when the largest number of the participants born in the same month were examined.
Screening and lifestyle counselling
People allocated to the intervention group were invited to the Research Centre for Prevention and Health and were screened with a comprehensive questionnaire (lifestyle, motivation to change lifestyle, symptoms, history of diseases, family history of diseases, psychosocial factors), physical measurements (electrocardiography, blood pressure, height and weight, waist and hip circumference, spirometry), blood samples (total cholesterol measured instantly using a Reflotron, total lipid profile), and a two hour oral glucose tolerance test. To assess the absolute risk of the participants, non-modifiable risk factors (age, sex, height, personal history of ischaemic heart disease and diabetes, history of ischaemic heart disease in parents) and modifiable risk factors (weight, smoking, blood pressure, instant cholesterol) were entered into the PRECARD program.7 On the basis of this information, an individual 10 year risk of fatal and non-fatal ischaemic heart disease was calculated. People were defined as being at risk if they belonged to the upper fifth (sex and age stratified) of the total risk of ischaemic heart disease. Each person was simulated in the computer program as 60 years old to reach a substantial level of risk. We did this partly to distinguish better between levels of risk and partly for pedagogical reasons as, for example, no young women have a high risk of ischaemic heart disease even if they have very unhealthy lifestyle and have several risk factors such as high blood pressure and high cholesterol. We included people in the lower four fifths in the high risk group if they had one or more of the following risk factors: daily smoking, a systolic blood pressure of 160 mm Hg or more (the lowest value of at least three measurements) or on antihypertensive treatment, total cholesterol of 7.5 mmol/L or more or in treatment with lipid lowering drugs, body mass index of 30 or more, history of diabetes or ischaemic heart disease, and detected diabetes or impaired glucose tolerance on the basis of the oral glucose tolerance test. In total, we classified 60% as being at high risk.6
On the basis of the personal risk estimate, each person had a personal lifestyle counselling session varying from 15 to 45 minutes immediately after their health examination and risk assessment. Counselling was given to all participants who were daily smokers, had less than 30 minutes’ physical activity per day, had a diet dominated by high intake of saturated fat, consumed less than 300 g of fruit and vegetables daily, or had an alcohol consumption above the recommended maximum levels (14 drinks a week for women and 21 for men) on the basis of the current national guidelines (www.Inter99.dk).6 Written material on physical activity, smoking cessation, diet, and alcohol was given when appropriate. Participants at high risk were further offered group based counselling with six sessions over a four to six month period. Three types of group based counselling were offered: a smoking cessation course (daily smokers willing to quit), a smoking reduction course (daily smokers unwilling to quit but willing to reduce), and a course on diet and physical activity. The choice of group based counselling depended on the risk factors and the preference and motivation of the participant. A plan for referral to their general practitioner or medical department, based on incidental findings of potentially life threatening values (such as very high blood pressure) was followed.6 Participants at high risk were given a letter to their general practitioner with information on the results of the examination.
Participants at high risk were re-invited after one and three years, when the screening, risk assessment, and lifestyle counselling procedures as described above were repeated. Those still at high risk were again offered group based counselling. Participants at low risk received a questionnaire but were not invited to the centre. After five years, all eligible participants at baseline were re-invited for final screening, individual counselling, and a plan for maintenance. The 10 year follow-up period ended on 31 January 2011, 10 years after the last person attended the baseline investigation. Minor changes in procedures during the study are described at www.inter99.dk.
The staff (nurses, dietitians, doctors) who did the health examinations, individual counselling, and group based counselling were taught the common health behaviour models (health belief model, Bandura’s social cognitive theory, the transtheoretical model)23 24 25 and were trained in lifestyle counselling, including the use of motivational interviewing and the stages of change model,25 26 as described earlier.6 15 16 17 18 19 20
We retrieved the following data from the central registries by means of the unique person number: emigration or death (civil registration system); baseline comorbidity index and incident ischaemic heart disease and stroke (national patient registry, which contains data on all admissions to non-psychiatric hospitals in Denmark since 1977 and on all outpatient contacts since 1995); causes of death (national registry of causes of death, where all causes of death have been registered since 1970); surgical procedures (Nordic classification of surgical procedures); socioeconomic data (Integrated Database for Labour Market Research); and ethnicity and cohabitation (national population registry). These registries have a very high validity and include close to 100% of people in the study population, as long as they had not emigrated.27
Endpoints and co-variables
We defined ischaemic heart disease as either admission to hospital (inpatient or outpatient) or causes of death with ICD-8 (international classification of diseases, 8th revision) codes 410-414 and ICD-10 codes I20-I25 (since 1994; ICD-9 was never used in Denmark) or surgery codes 300.09-304.99 and KFNC-KFNH (since 1996; bypass, recanalisation, or reconstruction of coronary arteries). We defined stroke events as either admission to hospital (inpatient or outpatient) or causes of death with ICD-8 codes 430-434 plus 436 and ICD-10 codes I60-I64 plus I69.
We defined the event date as the day of admission to or contact with the hospital, date of surgery, or date of death of the patient with the diagnosis in question. For people with several events, we used the date of the first event. The primary endpoint was ischaemic heart disease; secondary endpoints were stroke, combined events (ischaemic heart disease, stroke, or both), and total mortality.
We used age as a categorical variable in seven classes according to the chosen birth cohorts. We assessed socioeconomic status by cohabitation (yes, no) and education—basic (primary school only), low (1-2 years of education/vocational training; for example, hair dresser, gardener), intermediate (3-4 years of education/vocational training, for example, teacher, nurse), and high (>4 years of education; for example, academic). We categorised ethnicity as Danish, other Western countries, and non-Western countries. We developed a comorbidity score (web appendix 2) that included potentially life shortening diseases from all organ systems comprising hospital contacts in the period from 1978 to start date. We categorised the variable as zero, one, two, and three or more diseases.
Statistical analysis
We used logistic regression for comparison of baseline characteristics. In the analyses of incident cases of ischaemic heart disease and stroke, we excluded people who were diagnosed as having ischaemic heart disease before the study start (n=1308) from the analyses of ischaemic heart disease and the combined endpoint, and we excluded those who were diagnosed as having stroke before study start from the analyses of stroke and the combined endpoint (n=676). We did supplementary analyses without these exclusions.
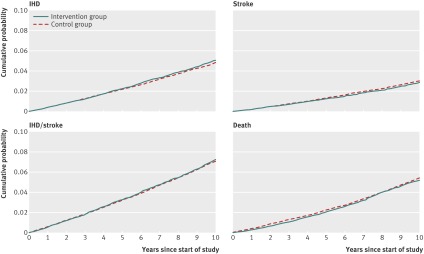
We calculated cumulative incidence curves illustrating the probability of a person having had an event at a given time, when the risk of a competing event (death) was taken into account.28 The cumulative incidence curves do not take age, sex, and other co-variables into account. We calculated cumulative incidences for each age and sex group, but they did not show any deviation in results (data not shown). We calculated cumulative incidence curves for each outcome and further investigated them with Gray’s test for equality.29
To investigate the effect of the intervention, we used three Cox regression models. The first model was adjusted for sex and age; the second included additional adjustment for education, ethnicity, and co-habitation; and the third also included adjustment for comorbidity. The analyses followed intention to treat principles with 10 year follow-up on all people unless they had an event, died, or emigrated in the period from inclusion to 10 years after. Given the study design, the main analyses were the models that only included sex and age, as the random assignment in the Inter99 study was weighted on sex and age.
We initially used a Cox regression model assuming proportional hazards (constant hazard ratio) over time for all variables. Whenever the proportional hazards assumption was not compatible with the data, we extended the Cox model by time dependent coefficients. The time dependent coefficient for a given variable allows the hazard ratio of an event to change during the 10 year study period. This was necessary for age when looking at ischaemic heart disease and the combined endpoint. We did all analyses for these endpoints both with and without time dependent coefficients for age. This optimisation of the model did not substantially change the results regarding associations between group and endpoints. All results presented are from Cox regression models assuming proportional hazards. Furthermore, we examined any two way interactions between intervention group, sex, and age; whenever one of these was statistically significant, we included it in the model. Finally, we examined possible three way interactions. For each of the four endpoints, we evaluated the fit of the survival regression models in all models.
We used SAS version 9.2 for survival curves and survival models. We used the software package R for cumulative incidence curves and Gray’s test. We considered P values below 0.05 to be statistically significant.
Results
Between the date of randomisation (2 December 1998) and the defined start date (which could be between 15 March 1999 and 31 January 2001), a total of 377 people (79 in the intervention group and 298 in the control group) either emigrated (n=184), disappeared (for example, homeless; n=4), died (n=187), or changed their personal identification number (for example, changed sex; n=2) and thus were not eligible for follow-up, leaving a study population of 59 616 people (intervention group, n=11 629; control group, n=47 987). The distribution of the 377 non-included people in the intervention and control groups was equal as regards age and sex.
Comparison of the intervention group and control group at baseline (table 1) showed no sex difference but a significantly different age distribution, which was expected because of the sampling procedure. As regards the possible confounders, ethnicity and comorbidity showed no differences between the groups, whereas significantly more people in the control group were cohabiting and had a lower education compared with those in the intervention group, even after adjustment for age and sex (table 1).
Table 1.
Baseline characteristics for intervention and control groups in Inter99 study (n=59 616). Values are percentages (numbers)
| Characteristic | Intervention group (n=11 629) | Control group (n=47 987) | P value* | Adjusted P value† |
|---|---|---|---|---|
| Age (years): | <0.01 | <0.01 | ||
| 30 | 7.6 (889) | 13.2 (6343) | ||
| 35 | 11.5 (1340) | 17.4 (8363) | ||
| 40 | 19.2 (2234) | 13.5 (6480) | ||
| 45 | 19.3 (2243) | 12.8 (6119) | ||
| 50 | 19.3 (2242) | 12.6 (6023) | ||
| 55 | 15.4 (1788) | 16.9 (8088) | ||
| 60 | 7.7 (893) | 13.7 (6571) | ||
| Male sex | 49.9 (5805) | 49.1 (23 565) | 0.12 | 0.13 |
| Ethnicity: | (n=11 619) | (n=47 939) | 0.31 | 0.85 |
| Danish | 88.5 (10 285) | 88.4 (42 397) | ||
| Western country | 2.8 (330) | 2.6 (1262) | ||
| Non-Western countries | 8.6 (1004) | 8.9 (4280) | ||
| Cohabitation with partner | 73.7 (8571) | 74.5 (35 760) | 0.07 | 0.02 |
| Education: | (n=11 324) | (n=46 746) | <0.01 | 0.04‡ |
| Basic | 29.8 (3379) | 30.1 (14 088) | ||
| Low | 52.0 (5890) | 53.0 (24 773) | ||
| Intermediate | 13.6 (1543) | 12.4 (5797) | ||
| High | 4.5 (512) | 4.5 (2088) | ||
| Comorbidity: | 0.98 | 0.88 | ||
| 0 serious diseases | 88.6 (10 299) | 88.6 (42 517) | ||
| 1 serious disease | 9.4 (1088) | 9.4 (4500) | ||
| 2 serious diseases | 1.7 (198) | 1.7 (796) | ||
| ≥3 serious diseases | 0.4 (44) | 0.4 (174) |
*Estimated in χ2 test (categorical variables).
†Estimated in logistic regression models; adjusted for age and sex.
‡Model includes interaction between education and sex, for model fit reasons.
A total of 6091 (52.4%) people in the intervention group accepted the invitation and were examined at baseline (fig 1). More young women than young men participated, and the participation rate increased with increasing age up to age 50, after which it declined. Besides the 60% (n=3642) at high risk, an additional 10% (n=608) had an individual lifestyle counselling due to unhealthy lifestyle according to the criteria mentioned. A total of 92% (n=3352) among those at high risk were offered group based counselling, as 8% (n=290) already received appropriate help (for example, overweight people receiving counselling from a dietitian or smokers who had signed up for smoking counselling elsewhere). Owing to a clerical error, 88 people (of whom 33 were occasional smokers) at low risk were also offered group based counselling and were invited after one and three years.
In the five year follow-up period, 59 (46 at high risk) of the 6091 (3642 at high risk) people died and 54 (36 at high risk) emigrated. At one year follow-up, 2224 people participated; at three year follow-up, 2240 participated. At the final screening after five years, 4028 (2119 from the high risk group) participated. At baseline, a total of 1489 people accepted participation in group counselling and 1293 eventually attended (for example, many smokers had quit on their own after the individual counselling). Among those who attended after one and three years, 335 and 295 participated in group based counselling.
Among 58 308 people without a history of ischaemic heart disease at baseline, 2782 developed ischaemic heart disease (565 in the intervention group and 2217 in the control group). Among 58 940 people without a history of stroke at baseline, 1726 developed stroke (326 in the intervention group and 1400 in the control group). Among the 59 616 people in the study population at baseline, 3163 died (595 in the intervention group and 2568 in the control group) in the 10 year follow-up period (table 2) and 1312 emigrated. The number of person years of follow-up varied between 527 754 and 574 638 (table 2).
Table 2.
Hazard ratios for incident cases of ischaemic heart disease, stroke, or combined cardiovascular events and total mortality in whole population of Inter99 study 10 years after study start
| Outcome | No of participants | No of person years | No of events (intervention/control group) | Hazard ratio* (95% CI) | Interactions: group*age/group*sex/group*age*sex (P values) |
|---|---|---|---|---|---|
| Ischaemic heart disease | |||||
| Model 1 | 58 308 | 551 627 | 565/2217 | 1.03 (0.94 to 1.13) | 0.21/0.68 |
| Model 2 | 56 801 | 537 808 | 545/2139 | 1.04 (0.94 to 1.14) | |
| Model 3 | 56 801 | 537 808 | 545/2139 | 1.04 (0.94 to 1.14) | |
| Stroke | |||||
| Model 1 | 58 940 | 562 255 | 326/1400 | 0.98 (0.87 to 1.11) | —/—/0.30† |
| Model 2 | 57 412 | 547 940 | 321/1364 | 0.99 (0.88 to 1.12) | |
| Model 3 | 57 412 | 547 940 | 321/1364 | 0.99 (0.88 to 1.11) | |
| Ischaemic heart disease and/or stroke | |||||
| Model 1 | 57 715 | 541 345 | 806/3243 | 1.01 (0.93 to 1.09) | —/—/0.63† |
| Model 2 | 56 226 | 527 754 | 782/3143 | 1.01 (0.94 to 1.10) | |
| Model 3 | 56 226 | 527 754 | 782/3143 | 1.01 (0.93 to 1.09) | |
| Total mortality | |||||
| Model 1 | 59 616 | 574 638 | 595/2568 | 1.00 (0.91 to 1.09) | 0.98/0.25 |
| Model 2 | 58 070 | 560 032 | 583/2517 | 1.00 (0.91 to 1.09) | |
| Model 3 | 58 070 | 560 032 | 583/2517 | 0.98 (0.90 to 1.08) | |
Model 1 adjusted for age and sex; model 2 adjusted for age, sex, education, ethnicity, and cohabitation; model 3 adjusted for age, sex, education, ethnicity, cohabitation, and comorbidity.
*Reference=control group.
†Significant interaction occurred between age and sex in analyses with stroke or combined events as outcomes; therefore, three way interaction between age, sex, and group is shown here.
The intervention had no effect on the incidence of the primary outcome, ischaemic heart disease (Gray’s test: P=0.30) (fig 2). Cox regression analysis showed no effect after adjustment for age and sex (hazard ratio 1.03, 95% confidence interval 0.94 to 1.13) (table 2, model 1). The hazard ratio was not affected by additional adjustment for education, ethnicity, cohabitation (model 2), and co-morbidity (model 3) (table 2). In supplementary analyses including the 1308 people with a history of ischaemic heart disease at baseline, similar results were observed (hazard ratio 1.04, 0.95 to 1.13, adjusted for age and sex). As regards the secondary outcome measures (stroke, combined endpoint, and death), similar negative results were observed (Gray’s test: P=0.48, P=0.56, and P=0.29, respectively) (fig 2). Cox regression models (table 2) adjusted for age and sex showed no effect of the intervention on stroke (hazard ratio 0.98, 0.87 to 1.11), the combined endpoint (1.01, 0.93 to 1.09), or death (1.00, 0.91 to 1.09). Supplementary analyses including the 676 people with a history of stroke and the 1901 with a history of either ischaemic heart disease or stroke gave similar results (hazard ratio 0.96 (0.86 to 1.08) and 1.00 (0.94 to 1.08), respectively). Cox regression analysis including only people with full information on all co-variables did not give different results.
Fig 2 Cumulative incidence curves of 10 year incidence of ischaemic heart disease (IHD), stroke, combined events (IHD, stroke, or both), and total mortality in intervention and control groups
We found no significant interaction between group and age or group and sex (table 2). As we anticipated a greater effect for the 40, 45, 50, and 55 year old people, we did sub-analyses for these age groups without any changes in results (Cox regression adjusted for age and sex: hazard ratios were 1.02 (0.91 to 1.13) for ischaemic heart disease, 1.03 (0.89 to 1.18) for stroke, 1.01 (0.93 to 1.11) for the combined endpoint, and 1.01 (0.91 to 1.12) for death). As we saw an interaction between age and sex in relation to stroke and combined events (table 2), we did sex specific analyses that showed no significant effect of the intervention in either sex for either primary or secondary outcomes (web appendix 3).
Discussion
This study is among the world’s largest intervention studies investigating the effect of screening for high risk of ischaemic heart disease followed by intensive repeated lifestyle counselling during a five year period. Although significant changes in lifestyle were described among participants after five years,15 16 17 18 19 20 we found no effect on development of ischaemic heart disease, stroke, combined events, or death in the entire study population over a 10 year period. No side effects were observed; in particular, no adverse psychological reactions were seen.30
Strengths and limitations of study
The study has both strengths and limitations. The participation rate was lower than we expected when we did the power calculations6; however, taking into account the fact that more people than expected had an increased risk and received counselling and that not even a trend to a reduction in ischaemic heart disease was observed, we doubt that a participation rate of 70% would have made any difference. Furthermore, the number of events was sufficient to show a possible effect. Important questions concern whether the intervention had sufficient quality and intensity. Staff were trained and supervised in accepted behavioural change theories and lifestyle counselling, were very committed, and consisted of a small number of people, most of whom stayed until the end of the five year follow-up. The participants had up to four individual face to face counselling sessions with a health professional, and people at high risk were additionally offered group based counselling of four to six months’ duration. The intensity of the intervention might of course be too low to achieve a change in unhealthy habits built up over a lifetime, but if an individualised intervention should be offered to 60% of the population its intensity must have limits. Even if better models for risk prediction for ischaemic heart disease existed (for example, using a stepwise screening procedure), we have no reason to believe that a larger number of people at risk would attend, especially not those with the highest risk. Also, we have no good reason to believe that more people would stick to lifelong lifestyle changes if the prediction model was improved. The intervention was primarily counselling, whereas medical treatment was left to general practice, which might result in low intensity treatment; but other studies using both counselling and medical treatment did not show an effect either.31
The possibility that a 10 year follow-up is too short must also be considered. According to our power analyses, we obtained a sufficient number of events, so a longer follow-up time would most probably not change the results. Furthermore, the results from studies of societal changes (for example, public smoking bans32) have shown an immediate effect on ischaemic heart disease events, indicating that if the intervention has an effect such changes should be expected within a short timeframe. The setting was a research clinic located in one of the large hospitals in the suburbs of Copenhagen. A general practice might be a more suitable place for lifestyle intervention, as general practitioners know their patients and patients have a high level of trust in their doctor. However, some of the lifestyle related randomised clinical trials were actually done in general practice as cluster randomised studies and showed no effect.33 Finally, the general practitioners in the area were informed about the study, and some of the participants were referred to them for medical treatment, further counselling, or both.
The strengths of the study are several: the size of the study and its population based design; the use of a tailored computer program (PRECARD), which took into account the effect of changing behaviour; the use of acknowledged health behaviour theories; and the use of an intensive programme of repeated counselling that could be applied in daily practice. Valid central registers allowed us to follow all people in the study, independent of participation and identifying both fatal and non-fatal cases. This enabled us to analyse data according to intention to treat, and the randomisation strategy ensured no spill over effect on the control group, as neither the control group nor their doctors knew that they formed a control group. Use of data from central registers further blinded the assessment of endpoints in relation to randomisation group. The generalisability of the results is thus high.
Comparison with other studies
To our knowledge, only one published study of sufficient size has used a similar approach to Inter99 looking both at fatal and non-fatal endpoints. Wilhelmsen et al invited a random sample from the background population and carried out a five year intervention.31 They identified another random sample as a control group without inviting them, followed the two groups in central registers, and analysed the results according to intention to treat. In contrast to our study, their population (10 000 people in each group) comprised only middle aged men (47-55 years), and their criteria for people at high risk were different from ours (but probably in accordance with the definition of high risk in the 1970s): blood pressure 175/115 mm Hg or above, cholesterol 7.8 mmol/L or above, and smoking at least 15 cigarettes a day. This identified nearly 37% of the study population as being at high risk of ischaemic heart disease, compared with our 60%, as we had a broader definition of people at high risk. The intervention included individual lifestyle counselling and medical treatment of high blood pressure and hyperlipidaemia. As in our study, they found no effect on the development of ischaemic heart disease, stroke, or death. Furthermore, they found no effect on the development of cancer.
Several population based intervention studies have used a more traditional randomisation approach known from clinical trials. In these trials, a random sample from the background population was invited and screened against certain criteria, identifying those at high risk, and then the participants were randomised into intervention and control groups. This design faces a high risk of spill over effect to the control group, which has been suggested as one of the explanations for the lack of effect.5 A more fundamental problem is that it cannot assess the effect of the intervention at a population level, only among people who choose to participate in the screening, so it cannot contribute to the evidence for or against systematic screening from a public health perspective. Finally, many of the studies had loss to follow-up, which makes them vulnerable to attrition bias. The studies have been summarised in Cochrane reviews, which have concluded that the interventions had no effect on the development of ischaemic heart disease.33 In our study, we could not compare people who attended the study with a comparable control group (owing to our design), so this study cannot contribute to these selected studies. Similar studies have focused on the effect of lifestyle counselling as regards the development of breast cancer and colorectal cancer, likewise without any effect.34 35 A recent Cochrane review based on 14 randomised clinical trials, including more than 180 000 people, concluded that general health checks have no effect on the number of admissions to hospital, disability, stress, number of referrals to specialists, additional visits to the physician, or absence from work.36
Policy implications
In spite of the consistently negative results of screening and lifestyle counselling, general health checks remain a popular political tool for combating the burden of ischaemic heart disease and other chronic diseases. Lately, the British government has started a general health check for the population.37 Danish left wing parties went to the polls in 2011 promising the same but changed their minds shortly after gaining power. In 1968 the World Health Organization proposed that several criteria should be fulfilled before systematic screening could be recommended.21 These criteria have often been interpreted as criteria for screening for early stages of diseases, but they also apply to systematic screening for high risk of diseases. Some of the main criteria are that the disease in question should be serious and that a valid screening instrument is available, both of which are fulfilled for ischaemic heart disease. However, the most important criterion is that screening should reduce morbidity and mortality in the target population. This has repeatedly been documented not to be the case for ischaemic heart disease. Distinguishing between the effect on the population as a whole and the effect on individuals participating in a study is important. Both our study and several others show that counselling has an effect for some people.15 16 17 18 19 20 38 Therefore, counselling should still be a natural part of the everyday practice of health professionals. But the literature clearly shows that adding a systematic approach to everyday practice, by performing health checks in a general population followed by lifestyle counselling, does not reduce the incidence of chronic diseases.
One reason for this may be that primary care physicians are already able to identify patients at high risk of developing diseases, when they see them for other reasons, and they already intervene when needed. Another reason could be that participation rates in such screening programmes are far from 100%, and obtaining an effect at the population level is difficult if the participation rate is low. Non-responders and people who drop out from the programmes have been shown to be more often from the lower social classes and to have a less healthy lifestyle, and these are actually the people who potentially could benefit most.39 This social inequality is also well known from cardiac rehabilitation and cancer screening.40 41 Furthermore, only a small proportion of those who participate are able to make the change to a healthier lifestyle. Adopting a lifestyle different from that of people in your surroundings is often difficult. Those who succeed in lifestyle changes have difficulties in maintaining the healthier lifestyle over the long term, resulting in further dilution of a possible effect of the intervention.42 Some authors report a significant effect of some cancer screening programmes,22 but this is very different from screening for risk of ischaemic heart disease. Cancer screening results in treatment performed by the healthcare system and does not require lifelong changes in lifestyle, whereas screening for risk of ischaemic heart disease leads to lifestyle recommendations, which should be adhered to for the rest of the person’s life. Finally, it could be argued that our risk estimation does not identify those at the highest risk. However, we used a Danish validated risk score, which was the most appropriate at the time when the study started. Both the high and low risk SCORE program has now been tested in a Danish population and found not to be suitable.43
During the past 10-15 years an increasing number of scientific articles have shown that even small changes in society are potent determinants of changes in incidence of ischaemic heart disease.44 In Cuba and Poland, the dramatic changes after the collapse of the Soviet Union gave rise to a marked reduction in deaths from ischaemic heart disease as a result of societal changes in physical activity and diet.45 46 Another example was the smoke-free laws leading to a marked decline in mortality due to ischaemic heart disease.32 The effect of these small societal changes revives Rose’s prevention paradox and indicates that they are a much more powerful tool to combat ischaemic heart disease than are screening and counselling of individuals.47 48 For decades, the focus has been on weakness of the will of the smoker or the overweight person—a “blame the victim” approach encouraged by big corporations.49 50 51 However, people face major barriers to making healthy choices and powerful pressures to adopt unhealthy ones.44 52 According to the United Nation’s high level meeting on non-communicable diseases, sufficient evidence is available for action, and this action should be on the political level,53 where it is necessary to balance the vested interests of big corporations. Increases in tobacco and alcohol taxes have been shown to reduce consumption as well as raise revenue for governments,54 55 and the regulation of salt intake could save billions in healthcare costs annually through reduction in blood pressure and, thereby, possibly the risk of stroke and ischaemic heart disease.56 Finally, a tax on unhealthy foods and subsidies for healthy foods could change the choices people make, which would have an effect on the development of ischaemic heart disease. This is further supported by studies on individual counselling in which the intervention group is given the healthy food options for free.57 This growing literature on changes in society as the main driver of unhealthy lifestyles indicates that the way towards a healthier population is, to a great extent, the responsibility of politicians and health administrators, supported by health professionals.
Conclusions
Systematic screening of the general population for high risk followed by lifestyle counselling has, in this large randomised population based study and in all previous similar studies, not been able to reduce the incidence of ischaemic heart disease. Therefore, health checks with systematic screening and counselling cannot be recommended. Lifestyle counselling should continue in everyday practice but should not be implemented as a systematic programme in the general population.
What is already known on this topic
Screening for risk factors for ischaemic heart disease (IHD) followed by lifestyle counselling leads to small changes in risk factors, but not to reduced mortality from IHD
Trials have been criticised for lack of theoretical framework, spill over effects on the control group, insufficient intervention, and lack of intention to treat analyses
Most trials have looked only at fatal cases among men
What this study adds
Systematic screening and intensive lifestyle counselling had no effect on development of fatal and non-fatal IHD in the general population, in either women or men
This study confirms that health checks followed by lifestyle counselling in a general population are not effective in reducing the burden of IHD in society and should not be part of a country’s health policy
We thank the whole Inter99-staff and all people participating in the study. The Inter99 study was initiated by Torben Jorgensen (principal investigator), Knut Borch-Johnsen (principal investigator on the diabetes part), Troels Thomsen, and Hans Ibsen. The current steering committee of the Inter99 study comprises Torben Jorgensen (principal investigator) and Charlotta Pisinger.
Contributors: TJ was responsible for the conception and design of the study. TJ, CG, and CP were involved in the design of the study and development of the intervention. TJ, RKJ and CP analysed data and wrote the first draft of the manuscript. All authors discussed data analyses and interpretation and contributed to subsequent versions of the manuscript, and all critically revised the manuscript and approved the final version of the manuscript. TJ is the guarantor.
Funding: The Inter99 study was funded by the Danish Research Councils, Health Foundation, Danish Centre for Evaluation and Health Technology Assessment, Copenhagen County, Danish Heart Foundation, Ministry of Health and Prevention, Association of Danish Pharmacies, Augustinus Foundation, Novo Nordisk, Velux Foundation, Becket Foundation, and Ib Henriksens Foundation. The researchers are independent of the founders, who had no influence on study design or conduct, analyses, or interpretation of results.
Competing interests: All authors have completed the ICMJE uniform disclosure form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work other than those listed above; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: The study was approved by the Regional Scientific Ethics Committee (KA 98 155) and the Danish Data Protection Agency.
Transparency: The lead author affirms that the manuscript is an honest, accurate, and transparent account of the study being reported. No important aspects of the study have been omitted, and any discrepancies from the study as planned have been explained.
Data sharing: Technical appendix, statistical codes, and dataset are available from the corresponding author.
Cite this as: BMJ 2014;348:g3617
Web Extra. Extra material supplied by the author
Appendix 1
Appendix 2
Appendix 3
References
- 1.World Health Organization. European health report: health and health systems. WHO, 2009.
- 2.Stamler J, Stamler R, Neaton JD, Wentworth D, Daviglus ML, Garside D, et al. Low risk-factor profile and long-term cardiovascular and non-cardiovascular mortality and life expectancy: findings for 5 large cohorts of young adult and middle-aged men and women. JAMA 1999;282:2012-8. [DOI] [PubMed] [Google Scholar]
- 3.Hjermann I, Holme I, Leren P. Oslo Study Diet and Antismoking Trial: results after 102 months. Am J Med 1986;80:7-11. [DOI] [PubMed] [Google Scholar]
- 4.Ebrahim S, Davey Smith G. A systematic review and meta-analysis of randomised controlled trials of health promotion for prevention of coronary heart disease in adults. BMJ 1997;314:1666-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Multiple Risk Factor Intervention Trial Research Group. Mortality rates after 10.5 years for participants in the Multiple Risk Factor Intervention Trial: findings related to a priori hypotheses of the trial. JAMA 1990;263:1795-801. [DOI] [PubMed] [Google Scholar]
- 6.Jørgensen T, Borch-Johnsen K, Thomsen TF, Ibsen H, Glümer C, Pisinger C. A randomized non-pharmacological intervention study for prevention of ischaemic heart disease: baseline results Inter99 (1). Eur J Cardiovasc Prev Rehabil 2003;10:377-86. [DOI] [PubMed] [Google Scholar]
- 7.Wood D, Backer GD, Faergeman O, Graham I, Mancia G, Pyörälä K. Prevention of coronary heart disease in clinical practice: recommendations of the Second Joint Task Force of European and other Societies on Coronary Prevention. Atherosclerosis 1998;140:199-270. [DOI] [PubMed] [Google Scholar]
- 8.Schroll M, Larsen S. A ten-year prospective study, 1964-1974, of cardiovascular risk factors in men and women from the Glostrup population born in 1914: multivariate analyses. Dan Med Bull 1981;28:236-51. [PubMed] [Google Scholar]
- 9.Truelsen T, Lindenstrøm E, Boysen G. Comparison of probability of stroke between Copenhagen City Heart Study and the Framingham Study. Stroke 1994;25:802-7. [DOI] [PubMed] [Google Scholar]
- 10.Justice AC, Covinsky KE, Berlin JA. Assessing the generalizability of prognostic information. Ann Intern Med 1999;130:515-24. [DOI] [PubMed] [Google Scholar]
- 11.Thomsen T, Davidsen M, Ibsen H, Jørgensen T, Jensen G, Borch-Johnsen K. A new method for CHD prediction and prevention based on regional risk scores and randomized clinical trials: PRECARD and the Copenhagen Risk Score. J Cardiovasc Risk 2001;8:291-7. [DOI] [PubMed] [Google Scholar]
- 12.Thomsen TF, McGee D, Davidsen M, Jørgensen T. A cross validation of risk-scores for CHD mortality based on data from the Glostrup Population Studies and Framingham Heart Study. Int J Epidemiol 2002;31:817-22. [DOI] [PubMed] [Google Scholar]
- 13.Collin R, Peto R, MacMahon S, Herbert P, Fiebach NH, Eberlein KA, et al. Blood pressure, stroke, and coronary heart disease: part 2. Short term reductions in blood pressure: overview of randomised drug trials in their epidemiological context. Lancet 1990;335:827-38. [DOI] [PubMed] [Google Scholar]
- 14.Thomsen T. HeartScore: a new web-based approach to European cardiovascular disease risk management. Eur J Cardiovasc Prev Rehabil 2005;12:424-6. [DOI] [PubMed] [Google Scholar]
- 15.Pisinger C, Glümer C, Toft U, von Huth Smith L, Aadahl M, Borch-Johnsen K, et al. High risk strategy in smoking cessation is feasible on a population-based level: the Inter99 study. Prev Med 2008;46:579-84. [DOI] [PubMed] [Google Scholar]
- 16.Toft U, Kristoffersen L, Ladelund S, Ovesen L, Lau C, Borch-Johnsen K, et al. The impact of a population-based multi-factorial lifestyle intervention on changes in long-term dietary habits: the Inter99 study. Prev Med 2008;47:378-83. [DOI] [PubMed] [Google Scholar]
- 17.Smith LV, Ladelund S, Borch-Johnsen K, Jørgensen T. A randomized multifactorial intervention study for prevention of ischaemic heart disease (Inter99): the long-term effect on physical activity. Scand J Public Health 2008;36:380-8. [DOI] [PubMed] [Google Scholar]
- 18.Aadahl M, von Huth Smith L, Toft U, Pisinger C, Jørgensen T. Does a population-based multifactorial lifestyle intervention increase social inequality in physical activity? Br J Sport Med 2011;45:209-15. [DOI] [PubMed] [Google Scholar]
- 19.Toft U, Pisinger C, Aadahl M, Lau C, Linneberg A, Ladelund S, et al. The impact of a population-based multi-factorial lifestyle intervention on alcohol intake: the Inter99 study. Prev Med 2009;49:115-21. [DOI] [PubMed] [Google Scholar]
- 20.Pisinger C, Toft U, Aadahl M, Glümer C, Jørgensen T. The relationship between lifestyle and self-reported health in a general population: the Inter99 study. Prev Med 2009;49:418-23. [DOI] [PubMed] [Google Scholar]
- 21.Wilson JMG, Jungner G. Principles and practice of screening for disease. World Health Organization, 1968.
- 22.Kramer BS, Gohagan JK, Prorok PC. Cancer screening: theory and practice. CRC Press, 1999.
- 23.Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q 1984;11:1-47. [DOI] [PubMed] [Google Scholar]
- 24.Bandura A. Social foundation of thoughts and action: a social cognitive theory. Prentice Hall, 1986.
- 25.Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: application to addictive behaviours: readings on etiology, prevention, and treatment. American Psychological Association, 1997:671-96.
- 26.Burke BL, Arkowitz H, Menchola M. The efficacy of motivational interviewing: a meta analysis of controlled trials. J Consult Clin Psychol 2003;71:843-61. [DOI] [PubMed] [Google Scholar]
- 27.Lynge E, Sandegaard JL, Rebolj M. The Danish national patient register. Scand J Public Health 2011;39(suppl 7):30-3. [DOI] [PubMed] [Google Scholar]
- 28.Andersen PK, Geskus RB, deWitte T, Putter H. Competing risks in epidemiology: possibilities and pitfalls. Int J Epidemiol 2012;41:861-70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gray RJ. A class of K-sample tests for comparing the cumulative incidence of competing risk. Ann Stat 1988;16:1141-54. [Google Scholar]
- 30.Jørgensen T, Ladelund S, Borch-Johnsen K, Pisinger C, Schrader AM, Thomsen T, et al. Screening for risk of cardiovascular disease is not associated with mental distress: the Inter99 study. Prev Med 2009;48:242-6. [DOI] [PubMed] [Google Scholar]
- 31.Wilhelmsen L, Berglund G, Elmfeldt D, Tibblin G, Wedel H, Pennert K, et al. The multifactor primary prevention trial in Göteborg, Sweden. Eur Heart J 1986;7:279-88. [DOI] [PubMed] [Google Scholar]
- 32.Lightwood JM, Glantz SA. Declines in acute myocardial infarction after smoke-free laws and individual risk attributable to secondhand smoke. Circulation 2009;120:1373-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ebrahim S, Taylor F, Ward K, Beswick A, Burke M, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease. Cochrane Database Syst Rev 2011;(1):CD001561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Prentice RL, Caan B, Chlebowski RT, Patterson R, Kuller LH, Ockene JK. Low-fat dietary pattern and risk of invasive breast cancer: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 2006;295:629-42. [DOI] [PubMed] [Google Scholar]
- 35.Beresford SA, Johnson KC, Ritenbaugh C, Lasser NL, Snetselaar LG, Black HR, et al. Low-fat dietary pattern and risk of colorectal cancer: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial. JAMA 2006;295:643-54. [DOI] [PubMed] [Google Scholar]
- 36.Krogsbøll LT, Jørgensen KJ, Grønhøj Larsen C, Gøtzsche PC. General health check in adults for reducing morbidity and mortality from disease. Cochrane Database Syst Rev 2012;(10):CD009009. [DOI] [PubMed] [Google Scholar]
- 37.McCartney M. Where’s the evidence for NHS health checks? BMJ 2013;347:f5834. [DOI] [PubMed] [Google Scholar]
- 38.Rees K, Dyakova M, Ward K, Thorogood M, Brunner E. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst Rev 2013;(3):CD002128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bender AM, Jørgensen T, Hansen BH, Linneberg A, Pisinger C. Socioeconomic position and participation in baseline and follow-up visits: the Inter99 study. Eur J Prev Cardiol 2012; published online 11 Dec. [DOI] [PubMed]
- 40.Grace SL, Abbey SE, Shnek ZM, Irvine J, Franche RL, Stewart DE. Cardiac rehabilitation II: referral and participation. Gen Hosp Psychiatry 2002;24:127-34, [DOI] [PubMed] [Google Scholar]
- 41.Frederiksen BL, Jorgensen T, Brasso K, Holten I, Osler M. Socioeconomic position and participation in colorectal cancer screening. Br J Cancer 2010;103:1496-501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Holme I, Hjermann I, Helgeland A, Leren P. The Oslo study: diet and antismoking advice: additional results from a 5-year primary preventive trial in middle-aged men. Prev Med 1985;14:279-92. [DOI] [PubMed] [Google Scholar]
- 43.Saidj M, Jørgensen T, Prescott E, Borglykke A. Poor predictive ability of the risk chart SCORE in a Danish population. Dan Med J 2013;60:A4609. [PubMed] [Google Scholar]
- 44.Jørgensen T, Capewell S, Prescott E, Allender S, Sans S, Zdrojewski T, et al. Population-level changes to promote cardiovascular health. Eur J Prev Cardiol 2013;20:409-21. [DOI] [PubMed] [Google Scholar]
- 45.Franco M, Ordunez P, Caballero B, Tapia-Granados JA, Lazo M, Bernal JL, et al. Impact of energy intake, physical activity, and population-wide weight loss on cardiovascular disease and diabetes mortality in Cuba, 1980-2005. Am J Epidemiol 2007;166:1374-80. [DOI] [PubMed] [Google Scholar]
- 46.Zatonski WA, McMichael AJ, Powles JW. Ecological study of reasons for sharp decline in mortality from ischaemic heart disease in Poland since 1991. BMJ 1998;316:1047-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rose G. The strategy of preventive medicine. Oxford University Press, 1992.
- 48.Cooney MT, Dudina A, Whincup P, Capewell S, Menotti A, Jousilahti P, et al. Re-evaluating the Rose approach: comparative benefits of the population and high-risk preventive strategies. Eur J Cardiovasc Prev Rehabil 2009;16:541-9. [DOI] [PubMed] [Google Scholar]
- 49.Wiist WH. The bottom line or public health: tactics corporations use to influence health and health policy, and what we can do to counter them. Oxford University Press, 2010.
- 50.Jahiel RI, Babor TF. Industrial epidemics, public health advocacy and the alcohol industry: lessons from other fields. Addiction 2007;102:1335-9. [DOI] [PubMed] [Google Scholar]
- 51.Proctor RN. The golden holocaust: origins of the cigarette catastrophe and the case of abolition. University of California Press, 2011.
- 52.Chan M. WHO Director-General addresses health promotion conference. 2013. www.who.int/dg/speeches/2013/health_promotion_20130610/en/.
- 53.Stuckler D, Basu S, McKee M. Commentary: UN high level meeting on non-communicable diseases: an opportunity for whom? BMJ 2011;343:d5336. [DOI] [PubMed] [Google Scholar]
- 54.Ding A. Curbing adolescent smoking: a review of the effectiveness of various policies. Yale J Biol Med 2005;78:37-44. [PMC free article] [PubMed] [Google Scholar]
- 55.Wagenaar AC, Salois MC, Komro KA. Effects of beverage alcohol price and tax levels on drinking: a meta-analysis of 1003 estimates from 112 studies. Addiction 2009;104:179-90. [DOI] [PubMed] [Google Scholar]
- 56.He FJ, MacGregor GA, A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens 2009;23:363-84. [DOI] [PubMed] [Google Scholar]
- 57.Estruch R, Ros E, Salas-Salvadó J, Covas MI, Corella D, Arós F, et al, for the PREDIMED Study Investigators. Primary prevention of cardiovascular disease with a Mediterranean diet. N Engl J Med 2013;368:1279-90. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix 1
Appendix 2
Appendix 3