Abstract
Background:
The goal of the study was to evaluate the efficacy of physical therapy in restoring function and mobility after a pediatric supracondylar humeral fracture.
Methods:
The study included sixty-one patients from five to twelve years of age with a supracondylar humeral fracture that was treated with casting or with closed reduction and pinning followed by casting. Patients were randomized to receive either no further treatment (no-PT group) or six sessions of a standardized hospital-based physical therapy program (PT group). The ASK-p (Activities Scale for Kids-performance version) and self-assessments of activity were used to assess function at one, nine, fifteen, and twenty-seven weeks after injury. Motion was measured at nine and fifteen weeks after injury by a blinded therapist. Anxiety was measured at one and nine weeks after injury with a self-assessment. Differences in ASK-p scores and anxiety level were analyzed with use of multivariate generalized estimating equations.
Results:
ASK-p scores were significantly better in the no-PT group at nine and fifteen weeks after injury (p = 0.02 and 0.01, respectively) but the difference at twenty-seven weeks was not significant. There were no differences between groups with respect to performance of activities of daily living or time to return to sports. Anxiety at nine weeks was associated with worse ASK-p scores at nine and fifteen weeks in the PT group and with better ASK-p scores in the no-PT group at these time points (p = 0.01 and 0.02, respectively). There were no differences between the groups with respect to elbow motion in the injured arm at any time. Severity of injury had no impact on function or elbow motion in either the PT or the no-PT group.
Conclusions:
Children undergoing closed treatment of a supracondylar humeral fracture that was limited to approximately three weeks of cast immobilization received no benefit involving either return of function or elbow motion from a short course of physical therapy.
Level of Evidence:
Therapeutic Level I. See Instructions for Authors for a complete description of levels of evidence.
Physical therapy contributes to restoration of normal function in patients deconditioned by disease, surgery, or trauma1-6. The utility of physical therapy for adults following lower-extremity injury or surgery is generally accepted. However, the evidence for its utility in adults is not strong7-14, and there is a dearth of evidence that physical therapy makes a positive impact on the return of function in children who have sustained musculoskeletal trauma15.
Supracondylar humeral fractures rank among the most common fractures treated by pediatric orthopaedists, and they are the most frequently treated fracture at our institution; nearly equal numbers of patients undergo nonoperative and operative management of these fractures. Displaced fractures are typically treated operatively under general anesthesia by closed reduction and pinning, followed by a short period of immobilization. Pins are removed in the clinic approximately three weeks after surgery. Nondisplaced or minimally displaced fractures are treated by casting without reduction, with a similar duration of immobilization. After cast removal, a stiff elbow and hesitant patient are the norm. Parents of patients undergoing cast removal after an elbow fracture frequently have questions regarding the best next step for their child. Although a study of return of motion with and without therapy after open treatment of a supracondylar humeral fracture has been reported previously15, return of function after closed management of the fracture, as measured with use of a patient-centered instrument, has not.
In 1955, Walter Blount wrote the following in Fractures in Children, a classic textbook from which generations of orthopaedists were trained in the essentials of pediatric fracture care: “Physical therapy, which is invaluable in the treatment of injured adults, is almost never necessary in the management of uncomplicated children’s fractures...At the elbow where there is frequently a delay in return of motion, a ‘hands off policy’ must be followed for many months...The child knows instinctively better than his parents, physical therapist, or doctor what he may do without harm...If left to his own devices, he will recover in the shortest possible time.”16
The aim of the present study was to determine which treatment serves children with a supracondylar humeral fracture better following cast removal: a few days of sling wear followed by a few weeks of activity restriction (which leaves the children to their own devices to manage return of motion and function) or a guided program of physical therapy designed to encourage early movement and restoration of function. Our null hypothesis was that physical therapy would provide no benefit with respect to recovery of function or return of motion except in a subset of patients with anxiety.
Materials and Methods
This single-center study was approved by the institutional review board at our tertiary care pediatric hospital and was registered at ClinicalTrials.gov (NCT00871793). The study included sixty-one patients, five to twelve years of age, who sustained a supracondylar humeral fracture treated either with casting or with closed reduction and pinning followed by casting. Patients were excluded if they were less than five or more than twelve years of age; had a fracture that was comminuted, was open, or required open reduction; had polytrauma or multiple fractures; had a developmental delay; or did not speak either English or Spanish. Enrollment was performed within a week of injury, from April 2009 to August 2011, by four research assistants. A block randomization scheme with a block size of six was used. Envelopes were prepared by our Biostatistics Department for concealed random assignment of enrolled participants and were opened following enrollment. Treating physicians were not informed of the participation status of patients. As there is some overlap between the diagnoses treated by physical and occupational therapists, we refer to the certified occupational therapists who worked with our patients in this study as physical therapists and to the therapy performed as physical therapy.
Patients were randomized to receive either no physical therapy (no-PT group) or an intended treatment program of six sessions of physical therapy performed by any of three therapists over a five-week period beginning the week after cast removal (PT group). Patients were given few instructions after cast removal, with the most detailed including “wear a sling when awake for a few days immediately after cast removal, then wear the sling only when outside of the house for a few additional days, avoid play at heights, play on wheeled objects, participation in contact sports, or play with animals on leashes for four weeks to follow.” Patients in the PT group were assessed during the first week after cast removal and were treated with a series of sessions involving heat, progressive splinting, strengthening exercises, and functional activities. Each session lasted approximately thirty minutes. The physical therapy sessions were discontinued when flexion within 15° of that in the uninjured elbow and full extension were achieved.
The primary outcome of interest was function, assessed by means of a number of instruments. The first of these instruments was the ASK-p (Activities Scale for Kids-performance version), which is a validated assessment of activity in children five through fifteen years of age that displays excellent reliability, minimal ceiling and floor effects, and sensitivity to clinically important changes in function17. As described by Plint et al., an ASK-p score difference of ≥5 points was deemed clinically important, as children who are normal and uninjured typically score in the mid-90s, mildly disabled children score in the mid-80s, and moderately disabled children score in the mid-50s (out of a possible 100 points)18. We also used a self-rating scale for activities of daily living18; this consisted of a simplified questionnaire with five questions regarding ease of performance of activities of daily living and a yes-or-no question regarding return to sports. The enrolled patient or a parent completed a baseline questionnaire one week after injury to roughly assess function prior to injury; questionnaires were also completed at nine, fifteen, and twenty-seven weeks after injury, with all but the last completed by the parent and child together during visits to our Clinical Research Center. The final questionnaire at twenty-seven weeks was completed by mail. We utilized an anxiety self-assessment instrument validated by Crandall et al.19 to identify a subset of patients who were anxious at various stages in the treatment (one and nine weeks after injury); the goal was to determine whether these patients represented a group that would benefit more from physical therapy than nonanxious children would. Finally, a physiotherapist blinded to the patient’s treatment group assessed motion at nine and fifteen weeks after injury.
Fracture type was classified by the treating physician with use of the Wilkins modification of the Gartland system of pediatric supracondylar humeral fracture classification20. Type-I fractures were those that were nondisplaced, type-II fractures were displaced with limited cortical contact, and type-III fractures were displaced with essentially no cortical contact21. Type-I fractures generally have an obvious transverse fracture line, but the initial radiographic findings may occasionally be limited to a posterior fat pad sign. Our standard protocol after supracondylar fracture included three weeks of cast immobilization (in <90° of elbow flexion) following initiation of treatment, regardless of the severity of the fracture or the type of treatment.
Statistical Methods
A power analysis prior to the study suggested that, with use of a two-sided t test and an alpha of 0.05, a sample size of sixty patients would provide 80% power to detect a difference of ≥5 points between groups at the nine-week assessment of our primary outcome (ASK-p) if the standard deviation was ≤6.5 points22. Similarly, a sample size of forty-six patients at the fifteen and twenty-seven-week time points would provide 80% power to detect a difference of ≥6 points between the two groups.
Baseline demographic and injury-related characteristics were assessed for balance between the study groups with use of the two-sample t test (for continuous variables) or chi-square test (for categorical variables). Univariate logistic regression models were used to examine whether any of these baseline characteristics were predictive of retention or nonretention at nine, fifteen, or twenty-seven weeks. Missing data were not imputed so as to avoid biasing estimates of the missing outcomes23,24. None of the baseline characteristics were associated with retention at nine, fifteen, or twenty-seven weeks, and retention did not differ significantly according to treatment group (see Appendix). Therefore, all subsequent analyses were restricted to the evaluable study population that completed the nine, fifteen, and/or twenty-seven-week follow-up assessments.
Following the intent-to-treat approach25,26, participants were analyzed in the study arm to which they were randomized, regardless of exposure to physical therapy. Differences in the ASK-p, activities of daily living, and return to sports were estimated with use of a multivariate generalized estimating equation to simultaneously model all time points and account for the correlation due to repeated measures for each patient. A p value of ≤0.05 was considered significant. The paired t test was used to compare the range of motion in the injured and uninjured arms at each time point. Additionally, linear regression models were used to investigate the effect of anxiety at one and nine weeks on function assessments and to test for differences in the effect of anxiety in the two treatment arms. The statistician was blinded to the treatment groups.
Source of Funding
No external funding was secured for this study.
Results
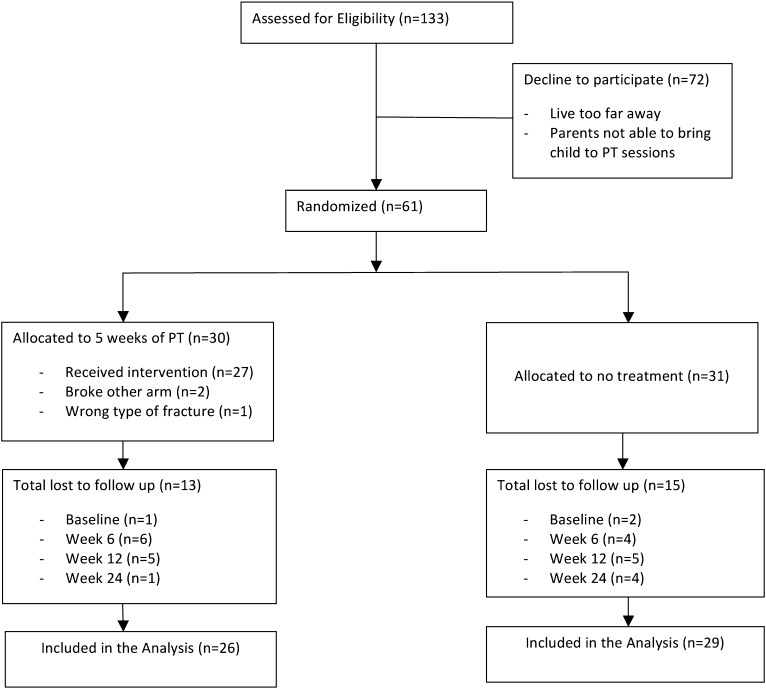
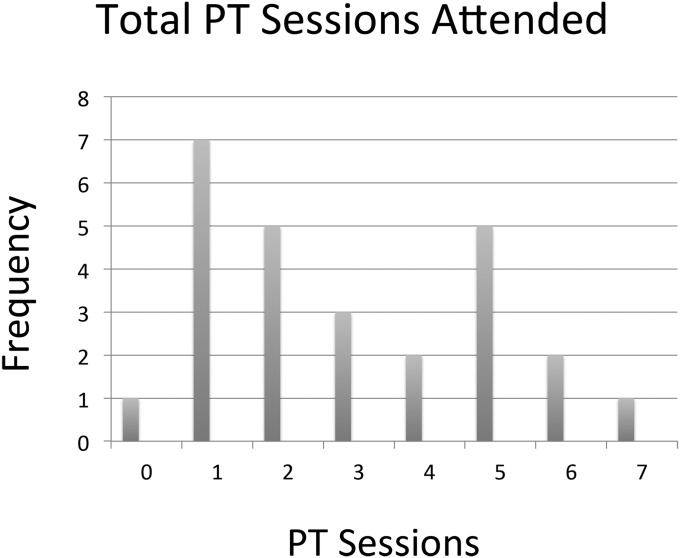
A total of 133 eligible patients were screened during the two-year period. Seventy-two of the patients decided not to participate in the study, and the remaining sixty-one were randomized to the PT or the no-PT group (Fig. 1). Of the thirty patients allocated to the PT group, twenty-six received treatment, three were excluded because of misdiagnosis or additional injury sustained during the treatment period but unrelated to the study, and one failed to attend any physical therapy sessions or follow-up visits but was included in the analysis in accordance with the intent-to-treat approach. The number of physical therapy sessions attended ranged from zero to seven (as one family requested an additional session), with a mean of three sessions (Fig. 2; see Appendix). Of the thirty-one patients allocated to the no-PT group, follow-up data were obtained for twenty-nine. Baseline characteristics were similar between the groups (Table I). Two patients with a Gartland type-I fracture had only a posterior fat pad sign at presentation; the remaining nineteen patients with a type-I fracture had an obvious fracture on initial radiographs. The extent of missing data (due primarily to patient loss to follow-up) did not differ appreciably between the groups (see Appendix). Approximately 50% of the patients in the PT group declined to schedule additional physical therapy sessions despite having not achieved the motion goals; the remainder continued therapy until discharged by our study therapists.
Fig. 1.
Flow diagram of the study.
Fig. 2.
Histogram showing attendance at therapy sessions for the entire PT group.
TABLE I.
Baseline Characteristics of the Groups
| Variable | PT Group, N = 27 | No-PT Group, N = 31 | P Value* |
| Age† (yr) | 6.04 ± 1.32 | 6.71 ± 1.68 | 0.093 |
| Sex‡ | 0.194 | ||
| M | 11 (41) | 19 (61) | |
| F | 16 (59) | 12 (39) | |
| Fracture treatment‡ | 0.861 | ||
| Surgery | 15 (56) | 19 (61) | |
| Cast only | 12 (44) | 12 (39) | |
| Gartland fracture type‡ | 0.798 | ||
| I | 11 (41) | 10 (32) | |
| II | 6 (22) | 8 (26) | |
| III | 10 (37) | 13 (42) | |
| Side of injury‡ | 0.524 | ||
| L | 17 (63) | 23 (74) | |
| R | 10 (37) | 8 (26) |
T test (for continuous variables) or chi-square test (for categorical variables).
The values are given as the mean and the standard deviation.
The values are given as the number of patients, with the percentage in parentheses.
ASK-p scores were significantly higher (better function) in the no-PT group at nine weeks, with an estimated difference between groups of 5.5 points (95% confidence interval [CI], 0.9 to 10.1 points; p = 0.02). At fifteen weeks, ASK-p scores were again significantly better in the no-PT group, with an estimated difference between groups of 6.1 points (95% CI, 1.5 to 10.8 points; p = 0.01). The differences between groups were no longer significant at twenty-seven weeks after injury (see Appendix). An exploratory analysis with use of linear regression did not show that patients with more visits had higher ASK-p scores; in fact, on average, they appeared to have lower scores. Thus, the intent-to-treat analysis appeared to be a reasonable approach.
There were no differences within or between groups with respect to the activities of daily living score or return to sports at any time point, as both of these outcomes had very little variability. Nearly all participants scored “0” for activities of daily living, meaning that they had no difficulties performing the five general tasks; and all reported “yes” for return to sports, indicating that they had returned to sports by nine weeks after injury. More of the girls were in the PT group and more of the boys were in the no-PT group; however, the ASK-p score and total motion did not differ significantly according to sex.
Anxiety at nine weeks was associated with lower ASK-p scores (worse function) in the PT group and with higher ASK-p scores (better function) in the no-PT group at both nine and fifteen weeks after injury. At nine weeks after injury, a one-unit increase in anxiety in the PT group was associated with a mean drop of 3.7 points (95% CI, −6.3 to −1.0 points; p = 0.01) in the ASK-p score. At fifteen weeks, a one-unit increase in anxiety at nine weeks in the PT group was associated with a mean drop of 3.1 points (95% CI, −5.6 to −0.6 points; p = 0.02) in the ASK-p score (Table II; see Appendix).
TABLE II.
Effect of Interaction Between PT Treatment and Anxiety Level
| ASK-p Score at 9 Weeks |
ASK-p Score at 15 Weeks |
|||
| Parameter | Estimate (95% CI) | P Value | Estimate (95% CI) | P Value |
| Intercept | 89.9 (86.7, 92.9) | <0.001 | 92.5 (89.5, 95.6) | <0.001 |
| Effect of anxiety at nine weeks | 0.4 (−1.0, 1.8) | 0.58 | 0.7 (−0.6, 2.1) | 0.28 |
| Effect of PT treatment | −2.7 (−7.5, 2.1) | 0.28 | −3.4 (−8.2, 1.4) | 0.17 |
| Effect of anxiety × treatment | −3.7 (−6.3, −1.0) | 0.01 | −3.1 (−5.6, −0.6) | 0.02 |
Whether the elbow underwent immediate immobilization (for a nondisplaced or minimally displaced fracture) or closed reduction and pinning followed by immobilization (for a displaced fracture) had no effect on return of function or motion in either treatment group. For those fractures treated with only casting, the mean time (and standard deviation) from injury to treatment was 4.7 ± 2 days, and the overall duration of immobilization was 24.3 ± 4 days. For those fractures treated operatively, the mean time from injury to surgery was 0.8 ± 0.6 day, and the overall duration of immobilization was 24.2 ± 3.9 days. The difference in overall duration of immobilization in the PT group compared with the no-PT group was not significant (95% CI, 1.86 to 3.07 days; p = 0.31).
At nine weeks, range of motion (total arc of elbow flexion-extension and of pronation-supination) in the injured arm was significantly lower than that in the normal arm (p < 0.001). Although range of motion in the injured arm improved between nine and fifteen weeks, it remained significantly lower than that in the normal arm at fifteen weeks (p < 0.001). Range of motion in the injured arm did not differ significantly between treatment groups at either of these time points (Tables III and IV). There were no differences in return of function or motion according to fracture type (Gartland I, II, or III) or treatment (casting or closed reduction and pinning followed by casting). No adverse events related to the treatments occurred in either group.
TABLE III.
Total Arc of Flexion-Extension Elbow Motion
| Week | Arm | PT Group* | No-PT Group* | P Value |
| 9 | Injured | 120.1 ± 17.8 | 126.3 ± 19.9 | 0.30 |
| Uninjured | 145.9 ± 10.4 | 149.0 ± 10.6 | ||
| 15 | Injured | 135.6 ± 10.5 | 137.9 ± 10.7 | 0.56 |
| Uninjured | 145.8 ± 7.1 | 149.3 ± 7.7 |
The values, in degrees, are given as the mean and the standard deviation.
TABLE IV.
Total Arc of Pronation-Supination Elbow Motion
| Week | Arm | PT Group* | No-PT Group* | P Value |
| 9 | Injured | 172.8 ± 10.8 | 168.4 ± 16.3 | 0.30 |
| Uninjured | 174.5 ± 8.3 | 173.7 ± 8.8 | ||
| 15 | Injured | 174.1 ± 7.9 | 169.1 ± 11.5 | 0.17 |
| Uninjured | 175.2 ± 6.7 | 174.8 ± 8.7 |
The values, in degrees, are given as the mean and the standard deviation.
Discussion
The importance of early motion to prevent stiffness after operative treatment of elbow fractures in adults is a widely held view27. Immobilization after elbow trauma in children also risks producing prolonged stiffness. We demonstrated no benefit to a formal physical therapy program for pediatric patients after closed treatment of a supracondylar humeral fracture, regardless of the degree of displacement of the fracture or whether or not the fracture was treated surgically. Among patients five to twelve years of age with a supracondylar humeral fracture treated with casting or with closed reduction and pinning followed by casting, those who underwent physical therapy had delays in restoration of function compared with those receiving no post-casting physical therapy, as measured by the ASK-p within the first fifteen weeks after injury. Function was ultimately restored by twenty-seven weeks after initiation of treatment, whether a few simple instructions for return to activity were given at the time of cast removal or the patient attended a five-week guided physical therapy program after cast removal. Patients in the PT group who had greater anxiety at nine weeks had worse function at nine and fifteen weeks after injury compared with less anxious patients. The functional assessment scores in both groups were much more tightly grouped around a score of 90 than initially expected in our pre-study power analysis. However, our patient population did not include children with special needs or previously existing conditions that would lead to lower functional assessments.
Keppler et al.15 studied forty-three children with a displaced supracondylar humeral fracture treated with open reduction and internal fixation. Children were randomized to receive community-based physical therapy or no physical therapy. A short-term advantage in terms of greater motion in the therapy group compared with the no-therapy group was seen at twelve and eighteen weeks but was no longer present at one year after injury. The mean duration of casting in that study (thirty-five days) was approximately eleven days longer than that in the present study (twenty-four days). Such prolonged casting may have resulted in stiffness that benefited from short-term therapy. In our patients, prolonged casting was not necessary as adequate healing of these fractures typically occurred by three weeks. We found no difference in motion between the PT and no-PT groups at any time point, in contrast to the findings of Keppler et al. Moreover, we used a standardized physical therapy treatment and found that the level of function was not significantly better, and in fact was worse, in children who received physical therapy, regardless of the type of fracture or whether they underwent only casting or reduction and pinning followed by casting.
Spencer et al.28 described the return of elbow motion following a supracondylar humeral fracture in children, noting that recovery of motion took longer after a more severely displaced fracture. However, more severely displaced fractures were immobilized longer in their patients, and all fracture types had a mean duration of immobilization of more than twenty-seven days. We found no difference in return of function or motion regardless of the severity of the fracture or whether it was treated operatively or nonoperatively, suggesting that the time to normalization after these injuries when they are treated in a closed fashion may be more a function of the duration of immobilization than of the degree of initial displacement of the fracture.
There are several limitations to our study. Our aim of controlling for the physical therapy regime affected our sample population; only families who could commit to travel to our hospital during regular hours for physical therapy participated in the study, which essentially limited enrollment to families living locally. We assumed our physical therapy program to be the optimal alternative to no therapy, although we had no evidence on which to base this assumption other than the expert advice of our therapists. These therapists may have been unduly aggressive or unduly conservative in their work with the patients, leading to slower patient progress.
Function was assessed by means of a questionnaire answered by the patients rather than by performance of monitored tasks. True measures of performance might have been more sensitive in revealing differences between groups. The anxiety measurement that correlated with worse function was the self-assessment performed at nine weeks, after completion of the physical therapy program. This suggests the possibility that the physical therapy sessions and relatively low self-assessment of function produced anxiety in our patients, rather than the anxiety leading to worse results with physical therapy. Enrollment into the physical therapy arm of the study represented a sacrifice for families, as attending the sessions resulted in out-of-pocket expenses for transportation as well as an opportunity cost for patients and families, perhaps leading to anxiety among participating patients.
The dropout rate was high in both groups despite efforts to maintain enrollment. We reminded families to return for follow-up and attempted to schedule follow-up sessions as prescribed by our protocol. Finally, this study examined only one particular type of humeral fracture; however, the result may be generalizable to fractures of the lateral condyle in children, as Wang et al. found similar early return of motion without therapy in patients with supracondylar and lateral condyle fractures29.
In summary, children undergoing closed treatment of a supracondylar humeral fracture limited to approximately three weeks of immobilization were not benefited by a short course of physical therapy in terms of either return of function or motion. Blount’s suspicion that “Physical therapy...is almost never necessary in the management of [such an] uncomplicated children’s fracture”16 is supported by the findings of this study. The study suggests that physical therapy after closed management of a supracondylar humeral fracture in children is of no clinical benefit.
Appendix
Tables showing the number of patients with missing data and the ASK-p scores at each time point as well as figures showing attendance at physical therapy sessions according to fracture type and ASK-p scores at nine and fifteen weeks according to anxiety at nine weeks are available with the online version of this article as a data supplement at jbjs.org.
Acknowledgments
Note: The authors thank Dr. Janet Eary, Research Director for the Department of Orthopaedics and Sports Medicine at Seattle Children’s Hospital, for her continued support and encouragement; Dr. Lynn Staheli, Professor Emeritus and long-time supporter of evidenced-based research to optimize pediatric orthopaedic care, for his ideas, enthusiasm, and support of this work; and Dr. Walter Greene for his historical assistance. The Seattle Children’s Core for Biomedical Statistics is supported by the Center for Clinical and Translational Research at Seattle Children’s Research Institute and grant UL1TR000423 from the National Center for Advancing Translational Sciences of the National Institutes of Health.
Footnotes
Investigation performed at Seattle Children’s Hospital, Seattle, Washington
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. None of the authors, or their institution(s), have had any financial relationship, in the thirty-six months prior to submission of this work, with any entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. Also, no author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Young P A short history of the chartered society of physiotherapy. Physiotherapy. 1969July;55(7):271-8 [PubMed] [Google Scholar]
- 2.States RA, Pappas E, Salem Y. Overground physical therapy gait training for chronic stroke patients with mobility deficits. Cochrane Database Syst Rev. 2009July8;(3):CD006075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Steultjens EM, Dekker J, Bouter LM, van Schaardenburg D, van Kuyk MA, van den Ende CH. Occupational therapy for rheumatoid arthritis: a systematic review. Arthritis Rheum. 2002December15;47(6):672-85 [DOI] [PubMed] [Google Scholar]
- 4.Takken T, Van Brussel M, Engelbert RH, Van Der Net J, Kuis W, Helders PJ. Exercise therapy in juvenile idiopathic arthritis: a Cochrane Review. Eur J Phys Rehabil Med. 2008September;44(3):287-97 [PubMed] [Google Scholar]
- 5.Dagfinrud H, Kvien TK, Hagen KB. Physiotherapy interventions for ankylosing spondylitis. Cochrane Database Syst Rev. 2008January23;(1):CD002822 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.McIlwaine PM, Wong LT, Peacock D, Davidson AG. Long-term comparative trial of conventional postural drainage and percussion versus positive expiratory pressure physiotherapy in the treatment of cystic fibrosis. J Pediatr. 1997October;131(4):570-4 [DOI] [PubMed] [Google Scholar]
- 7.Crotty M, Unroe K, Cameron ID, Miller M, Ramirez G, Couzner L. Rehabilitation interventions for improving physical and psychosocial functioning after hip fracture in older people. Cochrane Database Syst Rev. 2010January20;(1):CD007624 [DOI] [PubMed] [Google Scholar]
- 8.Handoll HG, Sherrington C, Mak JC. Interventions for improving mobility after hip fracture surgery in adults. Cochrane Database Syst Rev. 2011March16;(3):CD001704 [DOI] [PubMed] [Google Scholar]
- 9.Coppola SM, Collins SM. Is physical therapy more beneficial than unsupervised home exercise in treatment of post surgical knee disorders? A systematic review. Knee. 2009June;16(3):171-5 Epub 2008 Oct 11 [DOI] [PubMed] [Google Scholar]
- 10.Oskarsson GV, Hjall A, Aaser P. Physiotherapy: an overestimated factor in after-treatment of fractures in the distal radius? Arch Orthop Trauma Surg. 1997;116(6-7):373-5 [DOI] [PubMed] [Google Scholar]
- 11.Maciel JS, Taylor NF, McIlveen C. A randomised clinical trial of activity-focussed physiotherapy on patients with distal radius fractures. Arch Orthop Trauma Surg. 2005October;125(8):515-20 Epub 2005 Oct 22 [DOI] [PubMed] [Google Scholar]
- 12.Handoll HH, Madhok R, Howe TE. Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev. 2006July19;(3):CD003324 [DOI] [PubMed] [Google Scholar]
- 13.Dias JJ, Wray CC, Jones JM, Gregg PJ. The value of early mobilisation in the treatment of Colles’ fractures. J Bone Joint Surg Br. 1987May;69(3):463-7 [DOI] [PubMed] [Google Scholar]
- 14.Souer JS, Buijze G, Ring D. A prospective randomized controlled trial comparing occupational therapy with independent exercises after volar plate fixation of a fracture of the distal part of the radius. J Bone Joint Surg Am. 2011October5;93(19):1761-6 [DOI] [PubMed] [Google Scholar]
- 15.Keppler P, Salem K, Schwarting B, Kinzl L. The effectiveness of physiotherapy after operative treatment of supracondylar humeral fractures in children. J Pediatr Orthop. 2005May-Jun;25(3):314-6 [DOI] [PubMed] [Google Scholar]
- 16.Blount W Fractures in children. Baltimore: Williams & Wilkins; 1955 [Google Scholar]
- 17.Young NL, Williams JI, Yoshida KK, Wright JG. Measurement properties of the activities scale for kids. J Clin Epidemiol. 2000February;53(2):125-37 [DOI] [PubMed] [Google Scholar]
- 18.Plint AC, Perry JJ, Correll R, Gaboury I, Lawton L. A randomized, controlled trial of removable splinting versus casting for wrist buckle fractures in children. Pediatrics. 2006March;117(3):691-7 [DOI] [PubMed] [Google Scholar]
- 19.Crandall M, Lammers C, Senders C, Savedra M, Braun JV. Initial validation of a numeric zero to ten scale to measure children’s state anxiety. Anesth Analg. 2007November;105(5):1250-3 [DOI] [PubMed] [Google Scholar]
- 20.Wilkins KE, Beaty JH, Chambers HG, Toniolo RM. Fractures and dislocations of the elbow region. In: Rockwood CA, Wilkins KE, Beaty JH, editors. Fractures in children. 4th ed Philadelphia: Lippincott-Raven; 1996. p 653-752 [Google Scholar]
- 21.Kasser JR, Beaty JH. Supracondylar fractures of the distal humerus. In: Beaty JH, Kasser JR, editors. Rockwood and Wilkins’ fractures in children. 6th ed Philadelphia: Lippincott Williams and Wilkins; 2006. p 551-5 [Google Scholar]
- 22.Plint AC, Gaboury I, Owen J, Young NL. Activities scale for kids: an analysis of normals. J Pediatr Orthop. 2003Nov-Dec;23(6):788-90 [PubMed] [Google Scholar]
- 23.Rubin DB Multiple imputation after 18+ years. J Am Stat Assoc. 1996June;91(434):473-89 [Google Scholar]
- 24.Schafer JL Multiple imputation: a primer. Stat Methods Med Res. 1999March;8(1):3-15 [DOI] [PubMed] [Google Scholar]
- 25.Gail MH Eligibility exclusions, losses to follow-up, removal of randomized patients, and uncounted events in cancer clinical trials. Cancer Treat Rep. 1985October;69(10):1107-13 [PubMed] [Google Scholar]
- 26.Peto R, Pike MC, Armitage P, Breslow NE, Cox DR, Howard SV, Mantel N, McPherson K, Peto J, Smith PG. Design and analysis of randomized clinical trials requiring prolonged observation of each patient. I. Introduction and design. Br J Cancer. 1976December;34(6):585-612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Helfet DL, Schmeling GJ. Bicondylar intraarticular fractures of the distal humerus in adults. Clin Orthop Relat Res. 1993July;292:26-36 [PubMed] [Google Scholar]
- 28.Spencer HT, Wong M, Fong YJ, Penman A, Silva M. Prospective longitudinal evaluation of elbow motion following pediatric supracondylar humeral fractures. J Bone Joint Surg Am. 2010April;92(4):904-10 [DOI] [PubMed] [Google Scholar]
- 29.Wang YL, Chang WN, Hsu CJ, Sun SF, Wang JL, Wong CY. The recovery of elbow range of motion after treatment of supracondylar and lateral condylar fractures of the distal humerus in children. J Orthop Trauma. 2009February;23(2):120-5 [DOI] [PubMed] [Google Scholar]