Abstract
Background:
Over 60% of patients with carpal tunnel syndrome present with symptoms and findings of nerve compression in both hands. Our goal was to compare patient-rated difficulties in performing activities of daily living in the early postoperative period between those undergoing bilateral carpal tunnel release and those undergoing unilateral carpal tunnel release.
Methods:
This prospective cohort study enrolled consecutive patients with bilateral carpal tunnel syndrome undergoing bilateral carpal tunnel release (n = 47) or unilateral carpal tunnel release (n = 41). Patient function and disease severity were measured by an abbreviated form of the Disabilities of the Arm, Shoulder and Hand questionnaire, QuickDASH, and the Boston Carpal Tunnel Questionnaire at baseline, at postoperative visit 1 at a mean time (and standard deviation) of 10 ± 3 days, and at postoperative visit 2 at a mean time (and standard deviation) of 30 ± 6 days. Patients rated their difficulty in completing fifteen activities of daily living each day for the first postoperative week. Patients reported the factors that influenced their choice of surgery.
Results:
There was no difference in baseline function or disease severity between the two groups with regard to QuickDASH and the Boston Carpal Tunnel Questionnaire. Patients in both groups improved after carpal tunnel release with no difference between groups either at postoperative visit 1 for QuickDASH (p = 0.97) and the Boston Carpal Tunnel Questionnaire (p = 0.86) or at postoperative visit 2 for QuickDASH (p = 0.43) and the Boston Carpal Tunnel Questionnaire (p = 0.34). Patients undergoing bilateral carpal tunnel release had more difficulty only during postoperative days 1 to 2 in opening jars (p = 0.03), cooking (p = 0.008), and doing household chores (p = 0.02). Patients in the two groups did not differ (p > 0.05) in their abilities to perform activities of daily living necessary for personal hygiene or independence on any day during the first seven days following surgery with regard to using the bathroom, bathing, dressing, or eating. Although the most common reason why patients chose bilateral carpal tunnel release was to avoid two surgical procedures (42%), the most common reason why patients chose unilateral carpal tunnel release was concern for self-care (36%).
Conclusions:
Patients with bilateral carpal tunnel syndrome can anticipate more severe functional impairment during the first few postoperative days with bilateral carpal tunnel release compared with unilateral carpal tunnel release, but limitations beyond postoperative day 2 or 3 are similar for bilateral and unilateral carpal tunnel release.
Level of Evidence:
Therapeutic Level II. See Instructions for Authors for a complete description of levels of evidence.
Carpal tunnel syndrome is the most common upper-extremity compressive neuropathy, with a prevalence of 3% to 5% in the general population1. Of the affected patients, 60% to 70% present with bilateral symptoms and the rest are likely to develop subsequent symptoms in the initially unaffected hand2,3. With more than 500,000 carpal tunnel releases performed in the United States annually4, the treatment of median nerve compression represents a substantial societal and economic burden5.
Despite the high prevalence of symptomatic bilateral median neuropathy, there is a paucity of literature to guide clinical decision-making regarding treatment. In the absence of definitive evidence, many physicians believe that patients are better served by staging the carpal tunnel release procedures. In a recent unpublished survey by the American Society for Surgery of the Hand, 166 (85%) of 195 practicing hand surgeons replied that they performed simultaneous bilateral carpal tunnel release less often or never in patients with symptomatic bilateral carpal tunnel syndrome compared with how often they staged unilateral releases6. To date, only one small study conducted by Wang et al. has described patient-rated difficulty in completing activities of daily living after simultaneous bilateral carpal tunnel release7. Despite these data, evidence that guides decision-making in the surgical treatment of bilateral carpal tunnel syndrome is lacking.
The primary aim of this study was to compare the postoperative difficulty in performing activities of daily living between patients undergoing unilateral or simultaneous bilateral carpal tunnel release. Our secondary aim was to determine why patients decided to undergo simultaneous bilateral carpal tunnel release. Our hypothesis was that simultaneous bilateral carpal tunnel release would lead to significantly more short-term impairment, causing bilateral surgery to be a less favorable option.
Materials and Methods
This prospective, dual-cohort, patient-preference observational study was approved by our institutional review board and was registered with clinicaltrials.gov (protocol 201206073, NCT01961011). The study was performed in accordance with the STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) statement. Consecutive patients with the diagnosis of symptomatic bilateral carpal tunnel syndrome with indications for carpal tunnel release were recruited to participate. After giving written consent, participants underwent preoperative physical examination, including the administration of carpal tunnel provocative maneuvers (Tinel sign, Phalen sign, medial nerve compression test), two-point discrimination, and thenar muscle strength testing. Patient history was focused on findings similar to those noted in the validated Carpal Tunnel Symptoms Scale 6 questionnaire8. Patients were followed prospectively for a period of one month after surgery. To assess overall upper-extremity disability, we administered the validated shortened form of the Disabilities of the Arm, Shoulder and Hand questionnaire (QuickDASH)9-11. To quantify symptom severity of carpal tunnel syndrome and patient functional status, we administered the validated Boston Carpal Tunnel Questionnaire symptom severity and functional status scales12-15. Both cohorts completed all three validated questionnaires preoperatively (baseline), at their first postoperative visit (seven to ten days after surgery), and at their four-week postoperative visit. To better understand patient rationale for their choice of surgery and to better understand their overall postoperative experiences, we administered a secondary survey at the first postoperative visit. Patients also completed a daily log (see Appendix) rating their difficulties with activities of daily living during the first seven days after surgery.
Participants
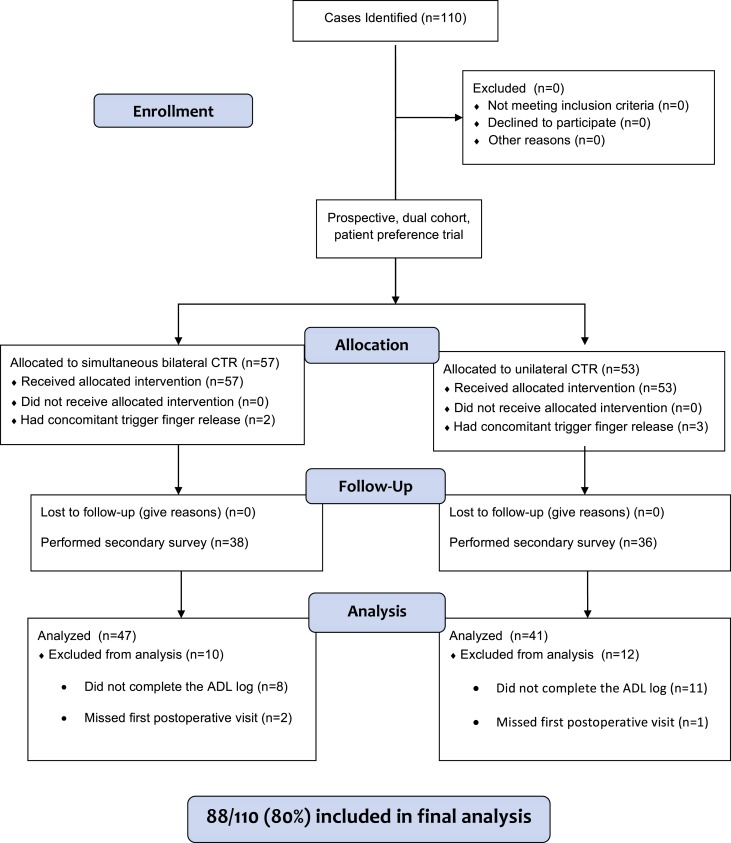
Consecutive patients with bilateral carpal tunnel syndrome were enrolled from July 2012 to April 2013 by one of five fellowship-trained hand surgeons (D.A.O., R.P.C., M.I.B., C.A.G, and R.H.G.) at a tertiary-care institution (Fig. 1). Inclusion criteria were (1) if the clinical examination led to a diagnosis of symptomatic idiopathic bilateral carpal tunnel syndrome, (2) if the patient had failed conservative treatment (which in all cases included a trial of splinting the wrist at night), (3) if the treating physician thought that carpal tunnel release was indicated in both hands, and (4) if the patient had help available at home during the early postoperative period. Patients with one trigger finger indicated for release at the same time as carpal tunnel release on one or both hands were included, but those who needed more than one trigger finger release on either hand or any other concurrent procedure were excluded. Eligible patients were enrolled into one of two groups. After discussion regarding both options, patients chose whether to undergo unilateral or bilateral carpal tunnel release. Consistent with the standard practice of the participating surgeons, therapeutic carpal tunnel injection was not performed on the contralateral hand in patients who chose unilateral carpal tunnel release. The bilateral group included those patients who chose simultaneous bilateral carpal tunnel release and the unilateral group included those who chose unilateral carpal tunnel release on the hand of their choice. Patients in the unilateral group were permitted to continue using a splint on the contralateral extremity not undergoing the surgical procedure during the study period. All surgical procedures were performed with use of a limited palmar incision open carpal tunnel release. Patients were excluded from data analysis if they did not complete their log of activities of daily living or if they missed their first postoperative appointment (n = 22 of 110 enrolled patients).
Fig. 1.
Clinical study design flow diagram. CTR = carpal tunnel release and ADL = activities of daily living.
Procedure
Patients underwent the anesthetic of their choice (local, regional, or general) after discussion with the anesthesiologist. After exsanguinating the arm and inflating the tourniquet, the surgeon made a longitudinal 2-cm incision over the proximal aspect of the palm, distal to the wrist crease, radial to the hook of the hamate. Skin and dermis were sharply divided. The subcutaneous fat was divided and was retracted ulnarly to protect the ulnar neurovascular bundle. Palmar fascia was identified and was divided adjacent to its ulnar border. The transverse carpal ligament was divided perpendicular to its fibers, 3 mm radial to the hook of the hamate to release the median nerve. The antebrachial fascia was released at the proximal border of the transverse carpal ligament. The nerve was inspected underneath the radial flap of the transected transverse carpal ligament. The surgical wound was irrigated with normal saline solution prior to closure of the skin with interrupted nylon sutures. For those patients undergoing bilateral surgery, this procedure was repeated on the opposite wrist. Soft bandages consisting of a non-adhering, petroleum-impregnated gauze, 4 × 4 gauze pad, a cotton undercast padding, and an elastic compressive dressing were then applied around the hand and wrist after injection of 0.5% bupivacaine into the skin and dermis.
During the first postoperative week, patients completed a log in which they recorded their ability to complete typical activities of daily living. Patients rated fifteen activities of daily living each day for seven days following surgery (see Appendix). To assist patients with the performance of hygiene-related activities after surgery, extra-large, latex-free, disposable gloves and disposable wipes were given to patients in both groups at the time of surgery. Patients were instructed to wear the gloves over the operative dressing to provide a protective barrier against fluid and to keep the dressings clean. The disposable wipes were provided to facilitate personal hygiene. Patients were instructed to avoid manual labor and lifting more than 5 kg (10 pounds) for one month after surgery. Other than these restrictions, patients were not given any other functional limitations, consistent with the protocol that we use in clinical practice. All enrolled patients in the unilateral and bilateral groups had a home assistant (typically a spouse or another immediate family member) to help with activities as needed. Patients were not required to use help if they felt able to perform their activities of daily living.
An interim data analysis was conducted after completion of the first postoperative assessment in eighteen patients (eleven in the unilateral group and seven in the bilateral group). On the basis of findings from that assessment, we administered an additional secondary survey to the remaining patients (thirty-eight in the bilateral group and thirty-six in the unilateral group). The new survey queried how patients were able to complete activities of daily living and assessed the factors that led patients to choose either bilateral simultaneous or unilateral surgery. In addition, patients were asked whether or not they would recommend bilateral carpal tunnel release to those patients who did not have help at home (see Appendix).
Data Analysis
Sample-size analysis determined that forty patients were needed in each cohort to provide 90% power to detect a minimal clinically important difference of 12 points in average QuickDASH scores between groups11. On the basis of the estimated mean minimal clinically important difference values (and standard deviation) of data on the Boston Carpal Tunnel Questionnaire and activities of daily living scales, this number of enrolled patients was sufficient for statistical analysis of both the Boston Carpal Tunnel Questionnaire and the activities of daily living scores. QuickDASH scores were calculated with use of the standard QuickDASH scoring algorithm to provide a score from 0 to 100 points (0 points indicate no disability and 100 points indicate maximum disability). The Boston Carpal Tunnel Questionnaire syndrome severity score and function severity score were calculated with use of each patient’s mean rating, producing a scale of 1 to 5 points (1 point indicates no symptoms and 5 points indicate maximum severity)12.
A two-tailed independent t test was used to compare the differences in the QuickDASH and the Boston Carpal Tunnel Questionnaire symptom and functional severity scores between the unilateral and bilateral groups. The difference between groups in each specific activity of daily living was analyzed for each of the seven postoperative days with use of the Mann-Whitney U test. Chi-square tests were used to determine if there was a difference in help needed to perform activities of daily living after surgery. We reported descriptive statistics on the results of the secondary survey.
Study data were collected and managed using REDCap (Research Electronic Data Capture) tools hosted in the Biostatistics Division of Washington University School of Medicine. REDCap is a secure, web-based application designed to support data capture for research studies16.
Source of Funding
There was no source of external funding for this study.
Results
A total of 110 patients with bilateral carpal tunnel syndrome were enrolled. No patient eligible for enrollment declined to participate. Of the 110 patients, fifty-three underwent unilateral carpal tunnel release and fifty-seven underwent bilateral carpal tunnel release. A concomitant trigger finger release was performed in three patients (6%) who underwent unilateral carpal tunnel release and in two patients (4%) who underwent bilateral carpal tunnel release. Twelve patients (23%) in the unilateral group and ten patients (18%) in the bilateral group did not complete their activities of daily living logs or did not achieve an appropriate duration of follow-up. A total of forty-seven patients in the bilateral group and forty-one patients in the unilateral group were included in our final analysis. Sex, baseline carpal tunnel severity, and baseline upper-extremity impairment were similar between the two groups (Table I).
TABLE I.
Demographic Characteristics and Baseline Severity
| Unilateral (N = 41) | Bilateral (N = 47) | Total | |
| Age* (yr) | 57 ± 11.9 | 52 ± 11.1 | 54.4 ± 11.7 |
| No. of female patients† | 32 (78%) | 32 (68%) | 64 (73%) |
| Baseline severity* (points) | |||
| QuickDASH | 48.5 ± 19.4 | 46.2 ± 18.3 | 47.3 ± 18.8 |
| Boston Carpal Tunnel Questionnaire symptom severity score | 3.2 ± 0.86 | 3.2 ± 0.71 | 3.2 ± 0.78 |
| Boston Carpal Tunnel Questionnaire function severity score | 2.7 ± 0.79 | 2.7 ± 0.78 | 2.7 ± 0.78 |
| Time to visit* (d) | |||
| First postoperative visit | 11 ± 3 | 10 ± 3 | 10 ± 3 |
| Second postoperative visit | 30 ± 6 | 30 ± 6 | 30 ± 6 |
| Occupation‡ | |||
| Desk job | 70% | 59% | 65% |
| Laborer | 30% | 41% | 35% |
The values are given as the mean and the standard deviation.
The values are given as the number, with the percentage in parentheses.
The values are given as the percentage of patients.
Complications
Postoperative complications were similar in both groups, with the most common complication being scar tenderness or pillar pain (pain along the thenar and hypothenar eminences) (33% in the unilateral group and 28% in the bilateral group). There were no hospital readmissions, infections, or wound complications. Three patients in the bilateral group had corticosteroid injections for postoperative trigger finger. One patient in the unilateral group had persistent symptoms in the involved hand that ultimately required revision carpal tunnel release. Although no patients in the bilateral group reported severe nocturnal symptoms or nighttime awakenings in the first month after surgery, nine patients (22%) in the unilateral group reported that they had had severe sleep disturbance due to symptoms from the hand that had not undergone surgery.
Patient-Rated Outcomes
There were no significant differences (p > 0.05) in the Boston Carpal Tunnel Questionnaire symptom severity scores, the Boston Carpal Tunnel Questionnaire functional severity scores, or the QuickDASH scores at either the first or second postoperative visit between patients undergoing bilateral carpal tunnel release and those undergoing unilateral carpal tunnel release (Table II). All three measures of disability and severity improved from baseline at each subsequent postoperative visit.
TABLE II.
Difference in Symptom Severity at Follow-up*
| Unilateral* | Bilateral* | P Value | |
| First postoperative visit (ten days) | |||
| QuickDASH | 40.8 ± 19.0 | 40.9 ± 22.0 | 0.97 |
| Boston Carpal Tunnel Questionnaire symptom severity score | 2.1 ± 0.6 | 2.1 ± 0.8 | 0.86 |
| Boston Carpal Tunnel Questionnaire function severity score | 2.5 ± 0.8 | 2.4 ± 0.9 | 0.86 |
| Second postoperative visit (thirty days) | |||
| QuickDASH | 25.8 ± 18.2 | 22.6 ± 15.8 | 0.40 |
| Boston Carpal Tunnel Questionnaire symptom Severity Score | 2.0 ± 0.7 | 1.8 ± 0.7 | 0.35 |
| Boston Carpal Tunnel Questionnaire function severity score | 1.9 ± 0.8 | 1.7 ± 0.7 | 0.20 |
The values are given as the mean score and the standard deviation, in points.
Difficulty in Performing Activities of Daily Living
When comparing the activities of daily living necessary for personal hygiene and independence (see Appendix), there were no significant differences (p > 0.05) in patient-rated difficulties during any of the seven days following surgery. There were also no significant differences (p > 0.05) in other tasks such as using the computer, carrying groceries, shopping, writing, holding a book, holding a phone, and buttoning (see Appendix). Patients undergoing bilateral carpal tunnel release noted significantly more difficulty in the first two postoperative days for cooking (p = 0.001 for postoperative day 1 and p = 0.008 for postoperative day 2), doing household chores (p = 0.03 for postoperative day 1 and p = 0.02 for postoperative day 2), and opening jars (p = 0.006 for postoperative day 1 and p = 0.03 for postoperative day 2) (see Appendix). For all three tasks, there were no significant differences (p > 0.05) during postoperative days 3 to 7. Line graphs and statistical values are presented for all activities of daily living in the Appendix.
Secondary Survey
Data were collected for thirty-six patients (88%) in the unilateral carpal tunnel release group and thirty-eight patients (81%) in the bilateral carpal tunnel release group after the first postoperative visit. In response to the secondary survey, patients most commonly cited the desire to avoid two surgeries followed by the desire for immediate symptomatic relief in both hands as the reasons why they chose bilateral carpal tunnel release (Table III). The most important factors influencing a patient’s selection of unilateral carpal tunnel release related to the concern about independent self-care following surgery.
TABLE III.
Factors Leading Patients to Choose Bilateral Versus Unilateral Carpal Tunnel Release
| Biggest Factor | No. of Patients |
| Bilateral carpal tunnel release (n = 38) | |
| Could not miss work for an extended period | 4 (11%) |
| Wanted immediate relief from severe symptoms | 10 (26%) |
| Did not want two surgeries | 16 (42%) |
| Felt they could accomplish activities of daily living on their own | 1 (3%) |
| Felt they had adequate help at home | 6 (16%) |
| Other | 1 (3%) |
| Unilateral carpal tunnel release (n = 36) | |
| Felt that symptoms were not severe in the opposite hand | 8 (22%) |
| Did not want to be burden some on family | 2 (6%) |
| Worried about practically caring for self | 13 (36%) |
| Worried about needing help with personal hygiene | 12 (33%) |
| Other | 1 (3%) |
Of those who underwent bilateral carpal tunnel release, twenty-four patients (63%) would not recommend bilateral carpal tunnel release if help at home was not available. Patients also reported that the availability of help at home (71%) and latex-free gloves and plastic bags for protection of their dressings (63%) were helpful in performing activities of daily living (Table IV). During the first postoperative week following surgery, there was higher frequency in the utilization of help with regard to hygiene-related activities for patients undergoing bilateral carpal tunnel release (45%) compared with patients undergoing unilateral carpal tunnel release (22%) and with regard to non-hygiene-related activities for patients undergoing bilateral carpal tunnel release (79%) compared with patients undergoing unilateral carpal tunnel release (56%) (Table V).
TABLE IV.
Patient Observations About Their Postoperative Experiences After Undergoing Carpal Tunnel Release
| Observations | No. of Patients (N = 38) |
| Factors allowing patients to perform their activities of daily living | |
| Extra-large latex-free gloves or plastic bags | 24 (63%) |
| Help at home | 27 (71%) |
| Disposable wipes | 16 (42%) |
| Other | 3 (8%) |
| Patients recommending bilateral carpal tunnel release to patients without help at home | |
| Yes | 14 (37%) |
| No | 24 (63%) |
TABLE V.
Patient Utilization of Help During Early Postoperative Activities of Daily Living
| Patient Utilization of Help | Unilateral* (N = 36) | Bilateral* (N = 38) |
| With personal hygiene† | ||
| Yes | 8 (22%) | 17 (45%) |
| No | 28 (78%) | 21 (55%) |
| With activities of daily living other than personal hygiene‡ | ||
| Yes | 20 (56%) | 30 (79%) |
| No | 16 (44%) | 8 (21%) |
The values are given as the number of patients, with the percentage in parentheses.
The Fisher exact test determined that p = 0.04.
The Fisher exact test determined that p = 0.03.
Discussion
This study was designed to determine the impact of simultaneous bilateral or unilateral carpal tunnel release on the level of patient-reported difficulties with activities of daily living in patients with bilateral carpal tunnel syndrome. Our data show that patients with bilateral carpal tunnel release have difficulties with specific activities of daily living in the first two days following bilateral carpal tunnel release, but by postoperative day 3, their self-reported activities of daily living performance is equivalent to that of patients with unilateral carpal tunnel release. In addition, patients in both groups experienced a similar decrease in upper-extremity disability (as measured by the QuickDASH) and in carpal tunnel-related disability (as measured by the Boston Carpal Tunnel Questionnaire) at ten days and one month after surgery.
Few studies have investigated patient function after simultaneous bilateral carpal tunnel release. Weber and Boyer performed a retrospective study in which patients undergoing simultaneous bilateral carpal tunnel release or sequential unilateral carpal tunnel release were asked at two to three years after surgery to recall their difficulties with activities of daily living in the early postoperative period17. Although levels of function were similar in the two groups, those who had undergone simultaneous carpal tunnel release were less willing to endorse the procedure than those who had had staged operative procedures. Fehringer et al. reviewed outcomes after simultaneous and staged endoscopic bilateral carpal tunnel release and found that there was no difference in overall patient satisfaction between groups18. However, the simultaneous carpal tunnel release group returned to full-duty work more quickly than did the staged carpal tunnel release group. Although these two prior retrospective investigations indicate that simultaneous bilateral carpal tunnel release may lead to similar levels of patient satisfaction when compared with staged bilateral carpal tunnel release, concerns regarding both patient selection and patient recall of postoperative function limit the generalizability of the findings.
In a prospective study, Wang et al. reported on a series of twenty patients undergoing simultaneous bilateral carpal tunnel release in which patient-rated difficulties were assessed in performing fifteen different activities of daily living during the first postoperative week7. The authors reported that patients were highly satisfied with carpal tunnel release and, on average, returned to work within three weeks after surgery. In our study, patients with simultaneous bilateral carpal tunnel release had a degree of patient-rated difficulty in completing activities of daily living that was comparable with that reported by Wang et al.7. However, we noted several substantial differences. Patients in our bilateral group found that activities associated with heavier lifting and gripping were more difficult to perform during the first two postoperative days (see Appendix). For other activities, including those needed for independence (bathing, using the bathroom, performing personal hygiene, eating, dressing, and driving), patients in both groups reported similar levels of difficulty in performing the measured activities at any time point during the follow-up interval.
There are several potential explanations for the similarity in early results in the two groups. Patients with unilateral carpal tunnel release may be impaired by symptoms in the untreated hand, which are exacerbated by the increased use of this hand postoperatively. Wintman et al. showed previously that postoperative satisfaction is greater in patients who had preoperative night symptoms and activity-induced paresthesia, compared with those patients with wrist, hand, or forearm pain; constant numbness; hand weakness; hand clumsiness; or difficulty with work-related tasks19. Thus, with continued symptoms in the hand yet to undergo surgery, patients may still experience disrupted sleep and functional difficulty associated with persistent nerve compression. In this study, we did not perform corticosteroid injection in the contralateral carpal tunnel while performing unilateral carpal tunnel release. In our practice, this type of injection has been mostly reserved for diagnostic purposes, although it may offer a useful adjunct if staging carpal tunnel releases.
We provided extra-large, latex-free, disposable gloves and disposable wipes to patients in both groups. Most patients found these to be important assistive tools for performing personal hygiene-related activities in the first week following surgery (Table V). These care-related adjuncts may have mitigated the potential additional impairment associated with presence of bulky soft bandages on both hands after bilateral carpal tunnel release. Finally, most patients in both groups needed help at home during the initial postoperative period. For patients in the bilateral carpal tunnel release cohort, personal assistance appeared to be an especially important factor, as the majority of these patients stated that they needed help with both hygiene and non-hygiene-related activities (Table V). Furthermore, most patients undergoing bilateral carpal tunnel release would not recommend bilateral carpal tunnel release to patients who did not have help at home (Table V). Nonetheless, one-third of patients still recommended bilateral release to patients who did not have help at home. Patients in the bilateral cohort showed a small and definable heightened level of early difficulty in performing activities of daily living with no demonstrable increased difficulty thereafter.
There were several limitations to our study. Owing to our prospective, dual-cohort, non-randomized study design, there may be patient-specific factors that predicted choice of simultaneous or consecutive bilateral carpal tunnel release. Patient employment status, age, availability of assistance at home, motivation to return to activity, symptom type, and comparative severity of symptoms in each patient’s hands are factors that may not have been evenly distributed between the groups, as the study was not randomized. We did not record the amount of time that anesthesia effects persisted in the hands or upper extremities of study patients after administration of a local or regional anesthetic at the time of surgery. Therefore, we were unable to determine if there was a difference in total anesthesia time between groups and if this difference could have affected function, especially in the first day or two after surgery. Through use of a postoperative survey, we asked patients to comment on their reasons for choosing unilateral or bilateral carpal tunnel release after they had already undergone surgery; it is possible that their responses may have been affected by recall bias. Finally, although patients in both groups demonstrated similar rates of difficulty with activities of daily living during the first postoperative week, there were significant differences in the percentages of patients with regard to assistance with hygiene-related activities of daily living (p = 0.04) between the bilateral carpal tunnel release cohort (45%) and the unilateral carpal tunnel release cohort (22%) and with regard to assistance with non-hygiene-related activities of daily living (p = 0.03) between the bilateral carpal tunnel release cohort (79%) and the unilateral carpal tunnel release cohort (56%). It is possible that these disparities may have masked a difference in impairment level between the two cohorts that would have otherwise been observed had assistance not been available.
The results of this study have changed our practice in the treatment of patients with bilateral carpal tunnel syndrome. We now routinely offer and perform simultaneous bilateral carpal tunnel release in patients who have substantial bilateral symptoms.
Appendix
A form showing the Bilateral Carpal Tunnel Release Survey and figures showing the postoperative daily log of activities of daily living and line graphs of the patient-rated difficulty with using the bathroom, using the computer, cooking, dressing, bathing, eating, buttoning, carrying groceries, shopping, writing, driving, holding a book, holding the phone, doing household chores, and opening jars each day for seven days after surgery are available with the online version of this article as a data supplement at jbjs.org.
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Washington University School of Medicine, St. Louis, Missouri
A commentary by William P. Cooney, MD, is linked to the online version of this article at jbjs.org.
Disclaimer: The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Disclosure: None of the authors received payments or services, either directly or indirectly (i.e., via his or her institution), from a third party in support of any aspect of this work. One or more of the authors, or his or her institution, has had a financial relationship, in the thirty-six months prior to submission of this work, with an entity in the biomedical arena that could be perceived to influence or have the potential to influence what is written in this work. No author has had any other relationships, or has engaged in any other activities, that could be perceived to influence or have the potential to influence what is written in this work. The complete Disclosures of Potential Conflicts of Interest submitted by authors are always provided with the online version of the article.
References
- 1.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosén I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999July14;282(2):153-8 [DOI] [PubMed] [Google Scholar]
- 2.Bagatur AE, Zorer G. The carpal tunnel syndrome is a bilateral disorder. J Bone Joint Surg Br. 2001July;83(5):655-8 [DOI] [PubMed] [Google Scholar]
- 3.Padua L, Padua R, Nazzaro M, Tonali P. Incidence of bilateral symptoms in carpal tunnel syndrome. J Hand Surg Br. 1998October;23(5):603-6 [DOI] [PubMed] [Google Scholar]
- 4.Fajardo M, Kim SH, Szabo RM. Incidence of carpal tunnel release: trends and implications within the United States ambulatory care setting. J Hand Surg Am. 2012August;37(8):1599-605 Epub 2012 Jun 23 [DOI] [PubMed] [Google Scholar]
- 5.Foley M, Silverstein B, Polissar N. The economic burden of carpal tunnel syndrome: long-term earnings of CTS claimants in Washington State. Am J Ind Med. 2007March;50(3):155-72 [DOI] [PubMed] [Google Scholar]
- 6.Gelberman RH One question results. American Society for Surgery of the Hand. http://www.assh.org/Members/MCT/Pages/wmu-122812.aspx#survey. Accessed 2014 Jan 31.
- 7.Wang AA, Hutchinson DT, Vanderhooft JE. Bilateral simultaneous open carpal tunnel release: a prospective study of postoperative activities of daily living and patient satisfaction. J Hand Surg Am. 2003September;28(5):845-8 [DOI] [PubMed] [Google Scholar]
- 8.Atroshi I, Lyrén PE, Gummesson C. The 6-item CTS symptoms scale: a brief outcomes measure for carpal tunnel syndrome. Qual Life Res. 2009April;18(3):347-58 Epub 2009 Feb 20 [DOI] [PubMed] [Google Scholar]
- 9.Gummesson C, Ward MM, Atroshi I. The shortened disabilities of the arm, shoulder and hand questionnaire (QuickDASH): validity and reliability based on responses within the full-length DASH. BMC Musculoskelet Disord. 2006May18;7:44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Angst F, Schwyzer HK, Aeschlimann A, Simmen BR, Goldhahn J. Measures of adult shoulder function: Disabilities of the Arm, Shoulder, and Hand Questionnaire (DASH) and its short version (QuickDASH), Shoulder Pain and Disability Index (SPADI), American Shoulder and Elbow Surgeons (ASES) Society standardized shoulder assessment form, Constant (Murley) Score (CS), Simple Shoulder Test (SST), Oxford Shoulder Score (OSS), Shoulder Disability Questionnaire (SDQ), and Western Ontario Shoulder Instability Index (WOSI). Arthritis Care Res (Hoboken). 2011November;63Suppl 11:S174-88 [DOI] [PubMed] [Google Scholar]
- 11.Calfee RP, Adams AA. Clinical research and patient-rated outcome measures in hand surgery. J Hand Surg Am. 2012April;37(4):851-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Levine DW, Simmons BP, Koris MJ, Daltroy LH, Hohl GG, Fossel AH, Katz JN. A self-administered questionnaire for the assessment of severity of symptoms and functional status in carpal tunnel syndrome. J Bone Joint Surg Am. 1993November;75(11):1585-92 [DOI] [PubMed] [Google Scholar]
- 13.Sambandam SN, Priyanka P, Gul A, Ilango B. Critical analysis of outcome measures used in the assessment of carpal tunnel syndrome. Int Orthop. 2008August;32(4):497-504 Epub 2007 Mar 17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Storey PA, Fakis A, Hilliam R, Bradley MJ, Lindau T, Burke FD. Levine-Katz (Boston) Questionnaire analysis: means, medians or grouped totals? J Hand Surg Eur Vol. 2009December;34(6):810-2 [DOI] [PubMed] [Google Scholar]
- 15.Leite JC, Jerosch-Herold C, Song F. A systematic review of the psychometric properties of the Boston Carpal Tunnel Questionnaire. BMC Musculoskelet Disord. 2006October20;7:78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009April;42(2):377-81 Epub 2008 Sep 30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Weber RA, Boyer KM. Consecutive versus simultaneous bilateral carpal tunnel release. Ann Plast Surg. 2005January;54(1):15-9 [DOI] [PubMed] [Google Scholar]
- 18.Fehringer EV, Tiedeman JJ, Dobler K, McCarthy JA. Bilateral endoscopic carpal tunnel releases: Simultaneous versus staged operative intervention. Arthroscopy. 2002March;18(3):316-21 [DOI] [PubMed] [Google Scholar]
- 19.Wintman BI, Winters SC, Gelberman RH, Katz JN. Carpal tunnel release. Correlations with preoperative symptomatology. Clin Orthop Relat Res. 1996May;(326):135-45 [PubMed] [Google Scholar]