Abstract
Problems in intimate relationships frequently occur among individuals with posttraumatic stress disorder (PTSD). This study includes examination of whether deficits in the intimacy process occur among couples affected by PTSD, and whether gender differences exist in the association between PTSD symptom severity and intimate behaviors. Heterosexual community couples in which at least 1 partner was experiencing elevated symptoms of PTSD were video-recorded while discussing positive and negative aspects of their relationship. Each partner's intimacy behaviors (i.e., self-disclosure and support provision) were coded. Results of an actor-partner interdependence model indicate that husbands, but not wives, with greater PTSD symptom severity provided less support (i.e., expressions of understanding, validation, and caring) to their partners during discussions of negative aspects of their relationship. This finding supports prior literature while increasing generalizability beyond samples of male combat veterans and addressing a possible confound of prior research that has exclusively relied on self-reported intimacy. In addition, wives' PTSD symptom severity was associated with husbands engaging in more self-disclosure when discussing negative aspects of their relationship, which may have represented husbands' expression of more negative thoughts and feelings in this context. Overall, women appeared to be resilient against the potential negative impact of PTSD symptoms on their ability to continue providing intimacy behaviors to their partners.
Keywords: intimacy, PTSD, observational coding, self-disclosure, support
Marital relationships are associated with positive outcomes for both mental and physical health (Kiecolt-Glaser & Newton, 2001). Care and support from a loved one are important predictors of recovery from psychopathology (Pierce, Sarason, & Sarason, 1996). However, psychopathology may disrupt intimacy, damaging the relationships that are needed most (Kiecolt-Glaser & Newton, 2001). As one example, posttraumatic stress disorder (PTSD) is implicated in marital problems such as low marital and sexual satisfaction, elevated divorce rates, and partner violence (Monson, Taft, & Fredman, 2009). The central role of marital relationships in PTSD risk and recovery has become increasingly clear, and, subsequently, the impact of PTSD on intimacy has accumulated interest in recent years (Monson et al., 2009).
PTSD likely influences poor marital outcomes through disrupted communication and bonding (Solomon, Dekel, & Zerach, 2008), central aspects of intimacy. Intimacy is often defined by feelings of mutual understanding, trust, affection, and ability to share with one's partner (Prager, 1995; Reis & Shaver, 1988) and is composed of self-disclosure (i.e., sharing personal thoughts and feelings) and support provision (i.e., providing responses that convey understanding, validation, or caring; Cordova & Scott, 2001; Prager, 1995; Reis & Shaver, 1988). Partners can reciprocally reinforce self-disclosure through supportive behavior (Cordova & Scott, 2001).
Although not developed specifically for understanding the impact of PTSD on relationships, the Vulnerability-Stress-Adaptation (VSA; Karney & Bradbury, 1995) model suggests that the enduring individual changes that can follow the experience of trauma, as well as transient stressors that frequently arise among couples adapting to the impact of trauma, can influence marital outcomes. As such, changes in intimacy related to individuals' symptoms of PTSD can limit couples' ability to adapt to the way PTSD impacts their relationship, decreasing overall marital satisfaction and stability. In addition, the Couple Adaptation to Traumatic Stress (CATS; Goff & Smith, 2005) model highlights how each partner's predisposing factors and posttrauma functioning can disrupt couples' intimacy. Both models emphasize that persistent and transient factors interact across partners, thus, necessitating a couple-level perspective for understanding the impact of PTSD on intimacy and associated marital outcomes.
Consistent with these models, recent research reveals that PTSD symptoms disrupt relationships in terms of individuals' difficulties with self-disclosure, expressing affection, and decreased sexual satisfaction (Henry et al., 2011; Monson et al., 2009). Particular features of PTSD (e.g., diminished interest in pleasurable activities, difficulty experiencing positive emotions, feeling detached, poor emotion skills; Monson, Price, Rodriquez, Ripley, & Warner, 2004) may impair engagement in the intimacy process. According to the VSA and CATS models, individuals' symptoms of PTSD may also affect their partners' provision of intimacy. Indeed, male combat veterans' PTSD symptoms are associated with negative communication patterns (e.g., negative escalation, invalidation, negative interpretations, withdrawal) with their wives (Allen, Rhoades, Stanley, & Markman, 2010). Prior studies have primarily focused on samples of male combat veterans, despite PTSD occurring 2–3 times more often among women than men and combat-related trauma representing a relatively small portion of the types of trauma that result in PTSD (National Comorbidity Survey, 2005). Therefore, we do not yet understand the nature of relationship difficulties, such as with intimacy, in the civilian population with PTSD.
Compared with men, women display somewhat higher rates of intimacy behaviors and emotion skills (e.g., Laurenceau, Barrett, & Rovine, 2005; Mirgain & Cordova, 2007; see Lippert & Prager, 2001, for an exception). This gender gap may widen when considering couples experiencing a stressor. The “tend-and-befriend” theory (Taylor et al., 2000) posits that women seek social support to protect their families and emotional health during times of stress, such as when they or their partners are experiencing PTSD symptoms. Indeed, compared with less stressful days, on more stressful days husbands report their wives provide more support, whereas wives report their husbands engage in more negative behaviors (Neff & Karney, 2005). Wives also provide more support than their husbands when discussing severe, but not less severe, marital problems (Neff & Karney, 2005). To date, no studies have directly tested for gender differences in the relation between PTSD symptoms and intimacy. However, men's provision of intimacy may be impacted more significantly by PTSD symptoms than women's due to women's strategies for responding to stress and their greater emotion skills.
We aimed to first confirm, using behavioral observation during partner discussions, that elevated PTSD symptoms are associated with providing less intimacy (i.e., self-disclosure and support provision). Prior studies have relied exclusively on self-report measures of intimacy, which may be biased by the emotion skill deficits in PTSD (Monson et al., 2004). Our second goal was to determine whether gender moderates the relation between PTSD and intimacy. We expected that, compared with women, men's PTSD symptoms would more severely impact their provision of intimacy. We additionally explored whether provision of intimacy may be negatively impacted by partners' PTSD symptoms and if this was especially the case for men.
Method
Participants
Married or cohabiting heterosexual couples (N = 64 couples, 128 individuals) were recruited from rural or semirural communities with advertisements targeting couples in which at least one partner had experienced a stressful life event. Couples were excluded if neither partner indicated probable PTSD (i.e., score >44 on the PTSD Checklist, Civilian Version; Weathers, Litz, Herman, Huska, & Keane, 1993; n = 122 couples), they were no longer interested (n = 8 couples), combined income exceeded $100,000 per year and/or either partner had more than 6 years post-high school education (n = 3 couples), or their relationship ended (n = 1 couple). We obtained written informed consent and Institutional Review Board approval.
The sample was predominantly White (85.9%; 1.6% White Hispanic or Latino, 2.3% Nonwhite Hispanic or Latino, 6.3% African American, and 3.9% multiracial) with an average age of 37.2 (SD = 12.6, range 18–64) years, an individual monthly income of $1,733.00 (SD = $1,529.00), and 14.31 (SD = 2.31) years of education. Few (17%) participants were students, and most (68.6%) were currently employed. The couples had been together for an average of 11 years and 11 months (SD = 11 years and 10 months, range 4 months to 45 years). Although some couples were unmarried (n = 17), they are referred to as husbands and wives for brevity.
Procedure
As part of a larger study of PTSD and relationship functioning, a graduate student administered a diagnostic interview for PTSD to participants. Couples also privately generated a list of the five most positive aspects or events and five most distressing aspects, events, or problems in their relationship (e.g., “We have the same sense of humor,” “We don't compromise”). Couples completed two 10-min video-recorded discussions: one regarding the positive topic and one regarding the negative topic that both partners rated most highly. Discussion order was counterbalanced with approximately 90 min between discussions.
Measures
PTSD symptoms
The Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) is the gold standard 30-item diagnostic interview for DSM–IV PTSD criteria. Symptoms are rated on a 5-point scale for frequency and intensity, then summed for total symptom severity (α = .94). Interrater reliability for 10% of interviews yielded an intraclass correlation of .92.
Trauma history
The Traumatic Life Events Questionnaire has good test–retest reliability and content validity (Kubany et al., 2000), thus, it was used to help determine the primary trauma for the CAPS interview.
Marital satisfaction
The Dyadic Adjustment Scale (Spanier, 1976) is a 32-item self-report questionnaire measuring satisfaction within intimate relationships. Scores range from 1 to 151, and scores less than 97 indicate low marital satisfaction or distressed relationships (α = .93).
Intimacy behavior
We used two global behavioral coding systems to measure self-disclosure and support provision, the identified components of intimacy (Cordova & Scott, 2001; Prager, 1995; Reis & Shaver, 1988). For support provision, we used the Global Responsive Behaviors Coding Guide (Maisel, Gable, & Strachman, 2008) to code the degree (i.e., frequency and quality; 7-point Likert scale ranging from 1 [none] to 7 [a great deal]) of understanding (e.g., asking questions or indicating that one understands), validation (e.g., validating the partner's identity or emotions), and caring (e.g., conveying love or concern) displayed by each partner. Ratings of understanding, validation, and caring were averaged to yield a total support provision score (α = .54 for the positive discussion, and α = .73 for the negative discussion).
For self-disclosure, we translated the construct definition (i.e., statements of one's feelings, wishes, or beliefs that reveal something about that person) from the Rapid Marital Interaction Coding System (RMICS; Heyman & Vivian, 2000), a microanalytic coding system, into one global rating that was rated on a 7-point scale. We did not designate valence (i.e., positive or negative) of disclosures because both can result in the vulnerable state required for intimacy (Cordova & Scott, 2001) and it can be difficult to characterize valence due to the range of valence in one disclosure and the ambiguity of how the disclosure could impact the couple.
Separate teams of two coders coded self-disclosure and support provision. The self-disclosure team achieved very strong interrater reliability (husbands' intraclass correlation coefficient [ICC] = .96; wives' ICC = .97; based on 15 positive and 16 negative interactions or 24.2%). The support provision team achieved strong reliability for understanding (ICC for husbands = .80; ICC for wives = .79), validation (ICC for husbands = .82; ICC for wives = .87), and caring (ICC for husbands = .93; ICC for wives = .70; based on 16 positive and 16 negative interactions or 25.0%).
Data Analysis
Continuous PTSD scores were used because taxometric analyses indicate that PTSD is a dimensional disorder representing an extreme reaction to traumatic life events (e.g., Broman-Fulks et al., 2006). Continuous scores also improve statistical power, are more reliable, and yield a greater amount of clinically relevant information than categorical measures.
The actor-partner interdependence model (APIM; Kenny, Kashy, & Cook, 2006) was used to determine the effects of both one's own (actor) and one's partner's (partner) PTSD symptom severity on intimacy behaviors (i.e., self-disclosure and support provision) observed in couples' positive and negative discussions. Actor's and partner's PTSD symptom severity were centered, and gender was effect coded (women as −1, men as 1). We created interaction variables by multiplying the main effect (i.e., PTSD symptom severity) by the moderating effect (i.e., gender). We replicated all analyses with marital satisfaction as a main effect variable to determine whether the findings were specific to intimacy, rather than marital satisfaction. All APIM analyses were conducted using the proc MIXED procedure in SAS 9.2 (SAS Institute, 2002–2008). Data were treated as repeated within the dyad, and heterogeneous compound symmetry was used to allow the error to vary between husbands and wives (Kenny et al., 2006).
Results
Descriptive statistics and correlations among study variables are presented in Table 1. Only one participant did not endorse at least one Criterion A trauma; consequently, she reported on PTSD symptoms in reference to her most stressful life event. CAPS scores for PTSD symptom severity had a nonnormal distribution (Shapiro-Wilk statistic = .96, p < .01) with a positive skew (skewness = .26, SE = 0.21). No transformation led to a normal distribution, so the original CAPS scores were used in all analyses. Reflecting the natural disparity in PTSD prevalence within the general population (National Comorbidity Survey, 2005), wives reported more severe PTSD symptoms than husbands, t(126) = 5.08, p < .01. Overall, the mean CAPS score was 36.11, which is high but below the generally accepted score for clinical significance (i.e., 45). This is expected since couples were typically recruited into the study because only one partner met screening criteria for PTSD. Among participants with more severe PTSD symptoms than their partners (i.e., partners who were the basis for recruiting the couple), the mean CAPS score was 52.83 (SD = 18.93), with no significant difference between husbands and wives (M = 57.13, SD = 22.36 and M = 51.51, SD = 17.80, respectively), t(62) = 1.34, ns. Sixteen (25.0%) husbands and 31 (48.4%) wives met DSM–IV diagnostic criteria for PTSD. The mean marital satisfaction score was 100.97 (SD = 19.44), suggesting that the average couple was not distressed (Eddy, Heyman, & Weiss, 1991), though great variability existed across couples (range 23–138). We found no gender differences in support provision or self-disclosure during either discussion.
Table 1.
Descriptive Statistics and Bivariate Correlations Among Study Variables
| Variable | M (SD) | Range | 1 | 2 | 3 | 4 | 5 | 6 | 7 |
|---|---|---|---|---|---|---|---|---|---|
| M (SD) | — | — | 46.16† (20.30) | — | 2.45 (1.58) | 3.53 (0.91) | 2.55 (1.53) | 2.89 (0.92) | 100.45 (20.19) |
| Range | — | — | 0–93 | — | 1.00–7.00 | 1.67–5.67 | 1.00–7.00 | 1.33–5.00 | 23.00–138.00 |
| 1. PTSD symptoms | 26.06† (24.32) | 0–102 | — | −.16 | .12 | −.03 | .16 | .00 | .23 |
| 2. Partners' PTSD symptoms | — | — | −.16 | — | .01 | .22 | −.12 | −.05 | −.38** |
| 3. Self-disclosure, positive discussion | 2.53 (1.60) | 1.00–7.00 | .32** | .02 | — | .30** | .34** | −.02 | .04 |
| 4. Support provision, positive discussion | 3.58 (0.85) | 2.00–6.33 | −.32** | .05 | −.02 | — | .21 | .29* | .15 |
| 5. Self-disclosure, negative discussion | 2.95 (1.64) | 1.00–7.00 | .06 | .38* | .28* | .09 | — | −.09 | −.01 |
| 6. Support provision, negative discussion | 3.08 (1.10) | 1.33–6.00 | −.44** | .18 | .01 | .53** | .23 | — | .36** |
| 7. Marital satisfaction | 101.45 (18.86) | 43.00–138.00 | −.21 | .20 | −.10 | .14 | .16 | .30* | — |
Note. Data for wives are above the diagonal; data for husbands are below the diagonal. Variables represent the actor unless specified. PTSD = posttraumatic stress disorder.
Significant gender difference, t(126) = 5.08.
p < .05.
p < .01.
As displayed in Table 1, among husbands but not wives, PTSD symptom severity was negatively correlated with support provision during the positive (r = −.32, p < .01) and negative (r = −.44, p < .01) discussions, as well as positively correlated with self-disclosure during the positive discussion (r = .32, p < .01). Partners' PTSD symptom severity was positively correlated with self-disclosure only during the negative discussions among husbands (r = .38, p < .01). Self-disclosure and support provision across both discussions were positively correlated among husbands (self disclosure r = .28, p < .05; support provision r = .53, p < .01) and wives (self disclosure r = .34, p < .01; support provision r = .29, p < .05). Self-disclosure and support provision were positively correlated during the positive discussions among wives (r = .30, p % .05) but not husbands. Marital satisfaction was positively correlated with support provision in negative discussions for husbands (r = .30, p < .01) and wives (r = .36, p < .01). For wives, partner's PTSD symptom severity was negatively correlated with marital satisfaction (r = −.38, p < .01). All other correlations among variables were nonsignificant.
In the APIM analyses, actors' PTSD symptom severity was associated with greater self-disclosure, b = .016, t(107) = 2.40, p < .05, during the positive discussions. There were no other significant relations for the positive discussions. During the negative discussions, actors' PTSD symptom severity was associated with providing less support, b = −.010, t(101) = −2.41, p < .05. In addition, partners' PTSD symptom severity was associated with providing more self-disclosure, b = .013, t(115) = 2.05, p < .05. There was an interaction between actors' PTSD symptom severity and gender such that husbands, but not wives, engaged in less support provision when they had greater PTSD symptom severity, b = −.009, t(118) = −2.47, p < .05 (Figure 1). There was also an interaction between partners' PTSD symptom severity and gender such that husbands, but not wives, were more likely to engage in self-disclosure when their partners had greater PTSD symptom severity, b = .019, t(116) = 3.06, p < .01 (Figure 1).
Figure 1.
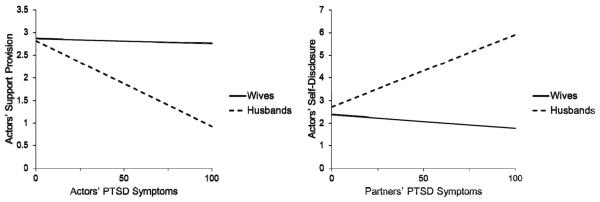
During negative discussions, gender moderates the relation between actors' posttraumatic stress disorder (PTSD) symptom severity and actors' support provision (left) and between partners' PTSD symptom severity and actors' self-disclosure (right).
Of note, we found no main effect of gender on the amount of self-disclosure or support provided during either discussion. Additionally, including actors' marital satisfaction as a covariate did not alter the pattern of results. Finally, the pattern of results remained unchanged when including only the subsample of couples in which at least one partner met either subthreshold or full diagnostic criteria for PTSD (n = 57 couples).
Discussion
Consistent with the VSA (Karney & Bradbury, 1995) and CATS (Goff & Smith, 2005) models, as well as prior research suggesting that intimacy is negatively impacted by PTSD (Monson et al., 2009), in this study greater PTSD symptom severity was associated with less support provision. Corroboration of existing research using observed intimacy behaviors helps negate the argument that prior findings may be confounded by a diminished ability to report on emotional processes among those with PTSD (Monson et al., 2004). In addition, corroboration among a community sample with diverse trauma histories increases confidence in the generalizability of the negative effect of PTSD symptoms on this aspect of the intimacy process.
We also found that gender played an important role in determining whether elevated PTSD symptoms are associated with the provision of fewer intimacy behaviors. In particular, husbands, but not wives, with greater PTSD symptom severity provided less support to their partners during discussions of negative aspects of their relationship. Past research has similarly suggested that male veterans report lower comfort with and expression of intimacy (Monson et al., 2009; Solomon et al., 2008) and male veterans with PTSD typically withdraw (i.e., provide less support) during important conversations (Galovski & Lyons, 2004). Our finding that women with more severe PTSD were not impaired in their ability to provide support is consistent with women's stronger emotional and interpersonal skills (Mirgain & Cordova, 2007) and their tendency to seek and provide support when under stress (Taylor et al., 2000), which may buffer against the negative impact of PTSD symptoms on their provision of intimacy. This finding was not replicated in the positive discussions, potentially indicating that gender differences emerge only when discussing predominantly negative and more stressful topics.
Contrary to expectations, PTSD symptom severity was associated with more self-disclosure during positive discussions, possibly indicating that some aspects of intimacy remain intact despite PTSD symptoms, and may even be heightened in the context of discussing positive aspects of one's relationship. It may also be that, in this context, partners with more severe PTSD symptoms felt more comfortable airing negative thoughts and emotions. Indeed, PTSD severity among male combat veterans and first responders is associated with disclosing more negative emotions and fewer positive emotions (Hoyt, Pasupathi, Smith, Yeater, & Tooley, 2010). Anecdotally, we observed that participants primarily focused on positive material (e.g., shared interests or supporting each other) during positive discussions, but some discussions still contained a substantial degree of negative material. Although negative disclosures can result in intimacy (Cordova & Scott, 2001), disclosures by one partner were not associated with greater support provision by the other partner so this may not have been the case. Instead, these disclosures may have been experienced by partners as complaints or general negativity.
This latter interpretation of the quality of self-disclosures may extend to our finding that, during the negative discussions, husbands were more likely to engage in self-disclosure when their wives had more severe PTSD symptoms. Although it is possible that husbands of women with more severe PTSD were putting forth extra effort to build intimacy with their partners, it is also possible that these husbands experienced more distress and were especially motivated to state their needs more frequently or strongly because of the burden associated with caring for a spouse experiencing psychopathology (Zarit, Todd, & Zarit, 1986). Because husbands' increased self-disclosure was not met with a commensurate increase in supportive behaviors, the bigger picture for couples affected by PTSD is one in which the intimacy process is disrupted. As emphasized by the VSA and CATS models, we would not have discovered this effect if we had not used a couple-level conceptualization and analytical process.
Several findings suggest that intimacy may be a more salient construct for couples affected by PTSD than is marital satisfaction. First, couples in this sample did not generally characterize their relationships as distressed, despite the presence of elevated PTSD symptoms in at least one partner. Second, although wives reported lower marital satisfaction when their husbands had greater PTSD symptom severity, this association did not emerge for husbands or for individuals in relation to their own PTSD symptom severity. Finally, marital satisfaction did not explain the associations between PTSD, intimacy, and gender. Future studies should build on our understanding of intimacy in this population above and beyond marital satisfaction.
The present study is the first to demonstrate the role of gender in the provision of intimacy among couples in which at least one partner is experiencing symptoms of PTSD. By studying community couples in which women experienced more PTSD symptoms than men (thus representative of the general population; National Comorbidity Survey, 2005), this study permits conclusions that extend to nonmilitary trauma and women with PTSD. The sample of couples willing to participate in this type of study may also represent couples most willing to engage in couples therapy for PTSD. Finally, the study benefited from methodological strengths including objective observation of intimacy and inclusion of both positive and negative discussions, which allowed for observation of how the valence of a topic might be important.
Certain limitations should also be noted. First, we cannot assume directional affects due to the cross-sectional nature of the study and the likely bidirectional relation between PTSD and intimacy behaviors. We interpret the likely direction of effects in line with prevailing theory and research, but the relative strength of effects in each direction is not currently known. Second, although there are certain benefits to using a community sample and a dimensional PTSD symptom score (and the pattern of results held when limiting the sample to those with full and subthreshold PTSD), it may be important to replicate the study using categorical PTSD diagnoses and a clinical population to determine how well the results generalize to clinical populations. Third, although considered a preferred methodology (Gottman, 1979), the external validity of laboratory discussions may be confounded. For example, men with more severe PTSD symptoms may be especially unlikely to engage in supportive behaviors due to privacy or impression management concerns. Finally, the global coding system does not capture the reciprocal process of self-disclosure and support provision (Cordova & Scott, 2001). Research using a microanalytic coding system could examine the pattern of self-disclosure and support provision to illuminate unique effects of the process and alternative functions of self-disclosures.
Results of this study suggest that therapy for couples affected by PTSD should address intimacy-related issues. Couples therapists may find that treatment is most effective when helping partners with PTSD, especially husbands, to provide support, even when discussing difficult relationship issues. It may also be especially important to continue to foster emotional closeness in couples therapy (e.g., Christensen, Jacobson, & Babcock, 1995; Johnson, 2002), in contrast to traditional couples therapy approaches that emphasize improving communication and problem solving skills to address disagreements (Jacobson & Margolin, 1979). It is hoped that such work could reverse the cycle in which PTSD may limit intimacy within a relationship, in turn diminishing the most important source of support for one's recovery (Pierce et al., 1996).
Acknowledgments
Amy D. Marshall is supported by the National Institutes of Health's Building Interdisciplinary Research Careers in Women's Health (BIRCWH) program (1 K12 HD055882). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. We thank Fiona Barwick, Charlene Chester, Kelly Parker-Guilbert, Lauren Sippel, Lauren Szkodny, and numerous undergraduate research assistants for their helpful contributions to participant recruitment, data collection, and data coding.
References
- Allen ES, Rhoades GK, Stanley SM, Markman HJ. Hitting home: Relationships between recent deployment, posttraumatic stress symptoms, and marital functioning for Army couples. Journal of Family Psychology. 2010;24:280–288. doi: 10.1037/a0019405. doi:10.1037/a0019405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. doi:10.1002/jts.2490080106. [DOI] [PubMed] [Google Scholar]
- Broman-Fulks JJ, Ruggiero KJ, Green BA, Kilpatrick DG, Danielson CK, Resnick HS, Saunders BE. Taxometric investigation of PTSD: Data from two nationally representative samples. Behavior Therapy. 2006;37:364–380. doi: 10.1016/j.beth.2006.02.006. doi:10.1016/j.beth.2006.02.006. [DOI] [PubMed] [Google Scholar]
- Christensen A, Jacobson NS, Babcock JC. Integrative behavioral couples therapy. In: Jacobson NS, Gurman AS, editors. Clinical handbook for couples therapy. Guilford Press; New York, NY: 1995. pp. 31–64. [Google Scholar]
- Cordova JV, Scott RL. Intimacy: A behavioral interpretation. The Behavior Analyst. 2001;24:75–86. doi: 10.1007/BF03392020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eddy JM, Heyman RE, Weiss RL. An empirical evaluation of the Dyadic Adjustment Scale: Exploring the differences between marital “satisfaction” and “adjustment”. Behavioral Assessment. 1991;13:199–220. [Google Scholar]
- Galovski T, Lyons JA. Psychological sequelae of combat violence: A review of the impact of PTSD on the veteran's family and possible interventions. Aggression and Violent Behavior. 2004;9:477–501. doi:10.1016/S1359-1789(03)00045-4. [Google Scholar]
- Goff BSN, Smith D. Systemic traumatic stress: The Couple Adaptation to Traumatic Stress Model. Journal of Marital and Family Therapy. 2005;31:145–157. doi: 10.1111/j.1752-0606.2005.tb01552.x. doi:10.1111/j.1752-0606.2005.tb01552.x. [DOI] [PubMed] [Google Scholar]
- Gottman JM. Marital interaction: Experimental investigations. Academic Press; New York, NY: 1979. [Google Scholar]
- Henry SB, Smith DB, Archuleta KL, Sanders-Hahs E, Nelson Goff BS, Reisbig AMJ, Scheer T. Trauma and couples: Mechanisms in dyadic functioning. Journal of Marital & Family Therapy. 2011;37:319–332. doi: 10.1111/j.1752-0606.2010.00203.x. doi:10.1111/j.1752-0606.2010.00203.x. [DOI] [PubMed] [Google Scholar]
- Heyman RE, Vivian D. Rapid marital interaction coding system manual. State University of New York at Stony Brook; 2000. Unpublished manuscript. [Google Scholar]
- Hoyt T, Pasupathi M, Smith BW, Yeater EA, Tooley E. Disclosure of emotional events in groups at risk for posttraumatic stress disorder. International Journal of Stress Management. 2010;17:78–95. doi: 10.1037/a0017453. [Google Scholar]
- Jacobson NS, Margolin G. Marital therapy: Strategies based on social learning and behavior exchange principles. Brunner/Mazel; New York, NY: 1979. [Google Scholar]
- Johnson SM. Emotionally focused couple therapy with trauma survivors: Strengthening attachment bonds. Guilford Press; New York, NY: 2002. [Google Scholar]
- Karney BR, Bradbury TN. Longitudinal course of marital quality and stability: A review of theory, methods, and research. Psychological Bulletin. 1995;118:3–34. doi: 10.1037/0033-2909.118.1.3. doi:10.1037/0033-2909.118.1.3. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. Guilford Press; New York, NY: 2006. [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. doi:10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Leisen MB, Kaplan AS, Watson SB, Haynes SN, Owens JA. Development and preliminary validation of a brief broad-spectrum measure of trauma exposure: The Traumatic Life Events Questionnaire. Psychological Assessment. 2000;12:210–224. doi: 10.1037//1040-3590.12.2.210. doi: 10.1037/1040-3590.12.2.210. [DOI] [PubMed] [Google Scholar]
- Laurenceau JP, Barrett LF, Rovine MJ. The interpersonal process model of intimacy in marriage: A daily-diary and multilevel modeling approach. Journal of Family Psychology. 2005;19:314–323. doi: 10.1037/0893-3200.19.2.314. doi: 10.1037/0893-3200.19.2.314. [DOI] [PubMed] [Google Scholar]
- Lippert T, Prager KJ. Daily experiences of intimacy: A study of couples. Personal Relationships. 2001;8:283–298. doi:10.1111/j.1475-6811.2001.tb00041.x. [Google Scholar]
- Maisel NC, Gable SL, Strachman A. Responsive behaviors in good times and bad. Personal Relationships. 2008;15:317–338. doi: 10.1111/j.1475-6811.2008.00201.x. [Google Scholar]
- Mirgain SA, Cordova JV. Emotion skills and marital health: The association between observed and self-reported emotion skills, intimacy, and marital satisfaction. Journal of Social & Clinical Psychology. 2007;26:983–1009. doi:10.1521/jscp.2007.26.9.983. [Google Scholar]
- Monson CM, Price JL, Rodriguez BF, Ripley MP, Warner RA. Emotional deficits in military-related PTSD: An investigation of content and process disturbances. Journal of Traumatic Stress. 2004;17:275–279. doi: 10.1023/B:JOTS.0000029271.58494.05. doi:10.1023/B:JOTS.0000029271.58494.05. [DOI] [PubMed] [Google Scholar]
- Monson CM, Taft CT, Fredman SJ. Military-related PTSD and intimate relationships: From description to theory-driven research and intervention development. Clinical Psychology Review. 2009;29:707–714. doi: 10.1016/j.cpr.2009.09.002. doi:10.1016/j.cpr.2009.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Comorbidity Survey NCS-R appendix tables: Table 1. Lifetime prevalence of DSM–IV/WMH-CIDI disorders by sex and cohort. 2005 Accessed from http://www.hcp.med.harvard.edu/ncs/publications.php.
- Neff LA, Karney BR. Gender differences in social support: A question of skill or responsiveness? Journal of Personality and Social Psychology. 2005;88:79–90. doi: 10.1037/0022-3514.88.1.79. doi:10.1037/0022-3514.88.1.79. [DOI] [PubMed] [Google Scholar]
- Pierce GR, Sarason BR, Sarason IG. Handbook of social support and the family. Plenum Press; New York, NY: 1996. [Google Scholar]
- Prager KJ. The psychology of intimacy. Guilford Press; New York, NY: 1995. [Google Scholar]
- Reis HT, Shaver P. Intimacy as an interpersonal process. In: Duck S, Hay DF, Hobfoll SE, Ickes W, Montgomery BM, editors. Handbook of personal relationships: Theory, research, and interventions. Wiley; Oxford, England: 1988. pp. 367–389. [Google Scholar]
- Solomon Z, Dekel R, Zerach G. The relationships between posttraumatic stress symptom clusters and marital intimacy among war veterans. Journal of Family Psychology. 2008;22:659–666. doi: 10.1037/a0013596. doi:10.1037/a0013596. [DOI] [PubMed] [Google Scholar]
- Spanier GB. Measuring dyadic adjustment: New scales for assessing the quality of marriage and similar dyads. Journal of Marriage and Family. 1976;38:15–28. doi:10.2307/350547. [Google Scholar]
- Taylor SE, Klein L, Lewis B, Gruenewald T, Gurung R, Upde-graff J. Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review. 2000;107:411–429. doi: 10.1037/0033-295x.107.3.411. doi: 10.1037/0033-295X.107.3.411. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility. Paper presented at the meeting of the International Society for Traumatic Stress Studies; San Antonio, TX. Oct, 1993. [Google Scholar]
- Zarit SH, Todd PA, Zarit JM. Subjective burden of husbands and wives as caregivers: A longitudinal study. The Gerontologist. 1986;26:260–266. doi: 10.1093/geront/26.3.260. doi:10.1093/geront/26.3.260. [DOI] [PubMed] [Google Scholar]


