Abstract
Objectives
To compare obstructive sleep apnea (OSA) in World Trade Center (WTC) responders with aerodigestive disorders and snoring with non-WTC habitual snorers, and to distinguish features of OSA in a subset of responders with worsening of snoring after 9/11 from responders with previous habitual snoring.
Methods
Cross-sectional comparative study of 50 WTC Medical Monitoring and Treatment Program responders with aerodigestive disorders and snoring and 50 nonresponders with snoring. Responders with worsening of snoring after 9/11 were compared with previous habitual snorers.
Results
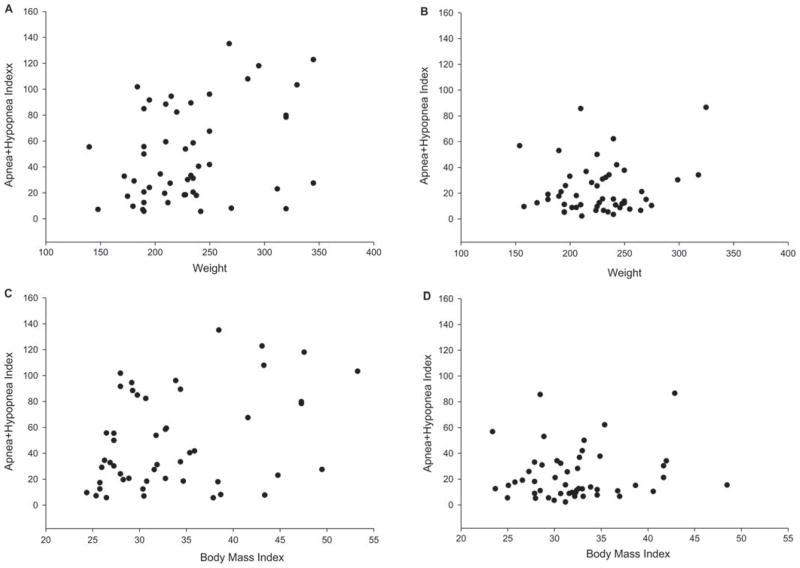
While there was a strong correlation between body mass index (BMI), weight, and Apnea + Hypopnea Index (r = 0.36, P = 0.001; r = 0.29, P = 0.044) in the nonresponders, no correlation between either BMI or weight and Apnea + Hypopnea Index was found in the responders. Responders with worsening of snoring after 9/11 had a significantly lower BMI than previous habitual snorers.
Conclusion
Mechanisms other than obesity are important in the pathogenesis of OSA in WTC responders with aerodigestive disorders.
After the World Trade Center (WTC) disaster on September 11, 2001, an estimated 40,000 individuals worked in rescue, recovery, and debris removal and were exposed to significant amounts of dust.1 A high prevalence of persistent aerodigestive symptoms [upper airway disease (UAD) and gastroesophageal reflux disease (GERD)] has been reported in participants of the World Trade Center Medical Monitoring and Treatment Program (WTCMMTP), as well as in firefighters exposed to the WTC disaster.2–4 These symptoms have persisted for years after the exposure. Since snoring and daytime symptoms of either sleepiness or disturbances in mood, concentration, and memory were commonly reported symptoms among these individuals, nocturnal polysomnography has frequently been performed in this population for evaluation of obstructive sleep apnea (OSA). OSA is characterized by episodes of complete or partial pharyngeal obstruction during sleep. Obesity and certain craniofacial features are notable predisposing factors for OSA. OSA occurs in obese patients during sleep as a result of increased fat deposition surrounding the upper airway resulting in a smaller airway lumen and increased collapsibility.5 Upper airway inflammation resulting in mucosal congestion could mimic these predisposing conditions and compromise upper airway patency during sleep. OSA has been described in patients with nasal congestion, seasonal allergic rhinitis, and after occupational exposure to guar gum dust, and is also associated with GERD.6–9 Previous studies of the relationship between WTC-related conditions and OSA reached differing conclusions on the association between GERD and/or chronic rhinosinusitis and increased risk for OSA.10,11
The aim of our study was twofold. Our first aim was to compare the characteristics of OSA in WTCMMTP responders with aerodigestive disorders, snoring, daytime symptoms, and complaints of sleep disturbance with a population of non-WTC habitual snorers with daytime symptoms referred to a comprehensive sleep disorders center (CSDC) to rule out OSA. The purpose of this comparison was to determine if, because of the exposure to WTC dust, this population could be distinguished from a population referred for habitual snoring and daytime symptoms. Our second aim was to gain insight into the pathogenesis of OSA in the WTCMMTP responders. We hypothesized that WTCMMTP responders with aerodigestive disorders and worsening of snoring after the WTC disaster would have unique features of OSA as a result of upper airway inflammation distinguishing them from a similar cohort with previous habitual snoring.
METHODS
Study Population
This study is a cross-sectional comparative study of two populations. Fifty WTCMMTP responders with aerodigestive symptoms and sleep-related problems, snoring and daytime symptoms were referred from January 2007 to December 2008 to the CSDC for evaluation to rule out OSA. The non-WTC comparison population was 50 male patients between the ages of 30 and 60 years with habitual snoring and daytime symptoms referred to the CSDC between July 2007 and June 2008 to rule out OSA. This referral population is drawn from an area surrounding the sleep center, within central New Jersey. The study was approved by the institutional review board of University of Medicine and Dentistry of New Jersey (UMDNJ)–Robert Wood Johnson Medical School.
World Trade Center Responders
The WTCMMTP at UMDNJ-Environmental and Occupational Health Sciences Institute, Piscataway, NJ, sees WTC responders who were exposed to significant amounts of dust and debris that followed the WTC disaster on September 11, 2001. The study population included those WTC responders who had symptoms that included snoring, choking and gasping at night, chronic cough, and a diagnosis of chronic rhinosinusitis or GERD, and had potential sleep-related daytime complaints including disturbance in mood, concentration, or memory for evaluation to rule out OSA at the CSDC between the period of January 2007 and December 2008.
Selection of Comparison Group
A total of 990 sleep studies were performed in the CSDC during that period. The majority of this referral population comes from central New Jersey and lives in the area surrounding the sleep center. To control for the age group and sex of the WTC responders, sleep studies from men between the ages of 30 and 60 years referred during this period who were not WTC responders were then chosen (n = 334). Of these, 225 studies were diagnostic or split night studies, whereas the remaining were CPAP titration studies. Fifty of the 225 charts were randomly chosen on the basis of a computer-generated random number. If information regarding snoring duration or other significant data was missing, it was replaced by a study performed on the same day that had all the necessary information.
Questionnaires
Two self-administered questionnaires were used. Upon enrollment in the WTC registry, a snoring questionnaire was administered to all WTCMMTP responders during their initial screening evaluation. It assessed frequency of snoring in the year before 9/11 and in the month before the initial screening evaluation. An ascending score of 0 to 4 was given for increasing frequency of snoring. The second questionnaire was administered at the CSDC to both the responders and non-responders and obtained more detailed information about demographics, sleep characteristics and daytime symptoms. Demographic questions included questions regarding age, sex, present weight, weight 3 years before the study, medical history, and current medications. Sleep questions included duration of snoring, history of witnessed apneas, and history of waking up choking or gasping, and subjects were asked to rate the quality of sleep as either poor, fair, good, or excellent in addition to other relevant questions regarding the patient’s sleep history. Questions regarding daytime symptoms included an Epworth Sleepiness Scale (ESS). The ESS is a self-administered questionnaire that asks people to rate their usual chance of dozing off on a four-point scale (0–3) in eight different situations. It provides a measure of a person’s general level of daytime sleepiness. The total ESS score is the sum of eight-item scores and can range between 0 and 24. The higher the score, the higher the person’s level of daytime sleepiness. Questions were also administered to determine if subjects complained of disturbance in mood, concentration, or memory.
In addition, all responders, regardless of symptoms, received spirometry with and without bronchodilators at their first examination.
Snoring Questionnaire Administered to the WTC Responders at the Monitoring Program
Questions included frequency of snoring with a scale of 0 to 4 with 0 being either never or rarely, no more than few times in the year; 1: sometimes, a few nights per month; 2: at least once a week; 3: three to five nights a week; and 4: six to seven nights a week.
Polysomnography and Definition of OSA
After obtaining body mass index (BMI) by measuring height and weight of the subjects, standard polysomnography was performed with three electroencephalography electrodes, electro-oculography, chin electromyography, pressure transducer to measure airflow through the nose, a thermistor for measurement of airflow through the mouth, pulse oximetry for measurement of oxygen saturation, piezoelectric respiratory signals for measurement of chest and abdominal movement, and anterior tibialis electromyography. Obstructive apneas were defined as cessation of airflow for at least 10 seconds and hypopneas were defined as at least 50% reduction in airflow with an associated 3% reduction in oxygen saturation with or without an arousal. All the apneas and hypopneas over the total duration of sleep are added up and an Apnea + Hypopnea Index (AHI) is obtained by dividing the total number of episodes by the total duration of sleep in hours. Sleep apnea was classified as “absent” if AHI was less than five episodes per hour of sleep, “mild” with an AHI of 5 to 15 episodes per hour of sleep, “moderate” with 15 to 30 episodes per hour of sleep, and “severe” if more than 30 episodes per hour of sleep. Rapid eye movement (REM) AHI was determined by dividing the total number of apneas and hypopneas during REM sleep by the total duration of REM sleep.
DATA ANALYSIS
Data obtained from the questionnaire administered at the CSDC and information from sleep studies including presence and severity of sleep-disordered breathing, AHI, REM and supine AHI were collected and compared between the WTCMMTP responders and nonresponders. The snoring questionnaire administered upon enrollment in the WTC registry, clinical history, and spirometry data from WTCMMTP responders were reviewed and snoring score, diagnosis of UADs, and the forced expiratory volume in the first second/forced vital capacity and forced expiratory flow (FEF)50/forced inspiratory flow (FIF)50 were recorded. To compare WTCMMTP responders with and without worsening of snoring symptoms, responders were divided into two groups based on the snoring questionnaire administered during the initial screening evaluation: responders with no or infrequent snoring (score of 0–2) before 9/11 and who developed habitual snoring (score > 3) after the exposure at the WTC (group 1) (n = 26) and those responders who had habitual snoring before the exposure (score of 3–5) (group 2) (n = 14). Ten patients were excluded from this analysis either because of an absence of information regarding snoring (n = 3) or because they had infrequent or no snoring (score < 2) that had either remained the same or improved (n = 7).
STATISTICAL ANALYSIS
Means and standard deviations or frequencies were calculated for each variable, as appropriate, for both WTCMMTP responders and for nonresponders. Two group t tests examined differences between groups for continuous variables while exact chi-square tests (permutation analyses) examined differences for categorical variables. To account for the possibility of confounding factors, analysis of covariance compared WTCMMTP responders versus nonresponders with respect to AHI, REM AHI, supine AHI, the ratio of supine AHI to AHI, sleep quality, ESS, and weight gain, adjusting for age, BMI, smoking status, and alcohol use; while additional comparisons of BMI between the two groups controlled for just age, smoking status, and alcohol use. The same unadjusted analyses as those discussed earlier compared WTCMMTP responders who were habitual snorers before the WTC disaster versus those who had worsening of snoring symptoms after the WTC disaster.
RESULTS
The demographics and clinical features of the WTCMMTP responders and nonresponders are shown in Table 1. Responders referred to the CSDC were men between the ages of 30 and 60 years and the majority were obese (BMI = 32.2 ± 5.2 kg/m2). Forty-six of the 50 patients were previously diagnosed with chronic rhinosinusitis, or pharyngitis with or without GERD, two patients had GERD alone, one patient had stridor and one had a diagnosis of reactive airways dysfunction syndrome at the time of referral. They had gained weight (4.5 ± 6.5 kg) in the previous 3 years, had snored for an average of about 11 years, and had mild daytime sleepiness (ESS = 9.8 ± 5.5). Ninety-six percent of the referred WTCMMTP responders were diagnosed with OSA on the basis of the sleep study and although approximately half of them had mild OSA (AHI of <15 events per hour of sleep), the group overall had a mean AHI of 22.7 ± 19.6 events per hour of sleep. Interestingly, although they had an average ESS of less than 10, more than half of them complained of poor sleep and neurocognitive symptoms including difficulty with memory, concentration, and mood.
TABLE 1.
Comparison of Demographics and Clinical Features Between the WTCMMTP and a Comparison Population of Men With Obstructive Sleep Apnea During the Same Referral Period
| Variable | WTCMMTP (n = 50) | Non-WTC (n = 50) | P |
|---|---|---|---|
| Age (yr) | 47.4 ± 7.31 | 45.3 ± 8.5 | 0.19 |
| Height (in) | 70.3 ± 3.3 | 70.1 ± 2.8 | 0.69 |
| Weight (kg) | 102.7 ± 16.3 | 104.7 ± 26.0 | 0.65 |
| Body mass index (kg/m2) | 32.2 ± 5.2 | 33.0 ± 7.9 | 0.57 |
| Weight gain (3 yr) (kg) | 4.5 ± 6.5 | 4.3 ± 10.4 | 0.90 |
| Snoring duration (yr) | 10.9 ± 8.0 | 13.7 ± 8.7 | 0.10 |
| Epworth Sleepiness Scale | 9.8 ± 5.5 | 10.1 ± 6.1 | 0.78 |
| Apnea + Hypopnea Index | 22.7 ± 19.6 | 43.4 ± 34.3 | 0.0004 |
| Apnea + Hypopnea Index | 0.05 | ||
| Absent | 4% | 8% | |
| Mild | 42% | 20% | |
| Moderate | 24% | 20% | |
| Severe | 30% | 52% | |
| REM Apnea + Hypopnea Index | 28.7 ± 25.6 | 43.7 ± 31.6 | 0.023 |
| Supine Apnea + Hypopnea Index | 36.0 ± 29.2 | 45.3 ± 38.3 | 0.19 |
| Witnessed apneas | 50% | 58% | 0.55 |
| Choking and gasping at night | 64% | 50% | 0.23 |
| Headaches | 68% | 62% | 0.68 |
| Difficulty with memory, concentration, and mood | 74% | 74% | 1.00 |
| Sleep quality | 0.12 | ||
| Poor | 52% | 34% | |
| Fair | 30% | 46% | |
| Good | 18% | 16% | |
| Excellent | 0% | 4% | |
| Smoker (regular) | 12% | 14% | 1.00 |
| Alcohol | 0.42 | ||
| None | 18% | 22% | |
| Occasionally | 56% | 42% | |
| At least once a week | 26% | 36% | |
| Chronic rhinosinusitis with or without GERD | 92% | ||
| GERD alone | 6% |
± values are means ± 1 SD.
GERD, gastroesophageal reflux disease; REM, rapid eye movement sleep; WTCMMTP, World Trade Center Medical Monitoring and Treatment Program.
In comparison with the nonresponder population of habitual snorers referred to the CSDC for a diagnostic evaluation for OSA, no significant differences were noted in mean BMI, snoring duration, weight gain in the previous 3 years, alcohol consumption, or smoking frequency. Ninety-two percent of this population was found to have OSA. Nevertheless, the mean AHI and REM-related AHI were significantly higher in this group as than in the WTCMMTP responders (mean AHI = 43.4 ± 34.3 vs 22.7 ± 19.6; P < 0.0004; REM AHI = 43.7 ± 31.6 vs 28.7 ± 25.6; P < 0.02). Although 82% of the nonresponder population had moderate to severe OSA, only 54% of the WTCMMTP responders had moderate to severe OSA (P < 0.05). The severity of sleep-disordered breathing remained significantly higher in the comparison population than in the WTCMMTP responders after adjusting for age, BMI, smoking status, and alcohol use (Table 2). Sleep quality was significantly poorer in the WTCMMTP responders as than in the comparison population despite having a significantly lower AHI (Table 2).
TABLE 2.
Indices of Sleep-Disordered Breathing, Sleep Quality, and Epworth Sleepiness Scale, Unadjusted and Adjusted for Age, Body Mass Index, Smoking Status, and Alcohol Use
| Variable | Unadjusted Means
|
P* | Adjusted Means
|
P | ||
|---|---|---|---|---|---|---|
| WTCMMTP | Control | WTCMMTP | Control | |||
| AHI | 22.7 (14.8, 30.5) | 43.4 (35.5, 51.2) | 0.0004 | 27.2 (17.0, 37.4) | 48.5 (38.7, 58.3) | 0.0002 |
| REM AHI (n = 81) | 28.7 (20.1, 37.4) | 43.7 (34.5, 53.0) | 0.021 | 33.7 (21.9, 45.4) | 51.4 (39.7, 63.2) | 0.0068 |
| Supine AHI (n = 90) | 36.0 (25.3, 46.7) | 45.3 (35.6, 55.1) | 0.20 | 41.1 (28.0, 54.3) | 51.1 (38.8, 63.5) | 0.17 |
| Supine AHI/AHI (n = 90) | 1.91 (1.45, 2.38) | 1.45 (1.02, 1.88) | 0.15 | 1.87 (1.25, 2.49) | 1.37 (0.79, 1.95) | 0.14 |
| Sleep quality | 1.66 (1.44, 1.88) | 1.90 (1.68, 2.12) | 0.13 | 1.40 (1.10, 1.69) | 1.72 (1.43, 2.00) | 0.046 |
| ESS | 9.8 (8.2, 11.4) | 10.1 (8.5, 11.7) | 0.78 | 11.4 (9.2, 13.5) | 11.1 (9.0, 13.2) | 0.81 |
Mean values with range in parenthesis; unless otherwise noted, n = 100. Values in bold are significant values.
P for effect of WTCMMTP vs control from the analysis of covariance model.
AHI, Apnea + Hypopnea Index; ESS, Epworth Sleepiness Score; REM, rapid eye movement sleep; WTCMMTP, World Trade Center Medical Monitoring and Treatment Program.
When correlating BMI and weight to AHI within nonresponders and WTCMMTP responders, we found the correlations were positive and significant in the nonresponder group. The correlations of BMI and weight with AHI were 0.36 (P = 0.0096) and 0.29 (P = 0.044), respectively (Fig. 1, panels A and C). For WTCMMTP responders, no correlation was found between either BMI or weight to AHI (r = 0.09, P = 0.52; r = 0.15; P = 0.29, respectively) (Fig. 1, panels B and D). These findings suggest that factors aside from BMI/weight may be associated with OSA in the WTC group. We hypothesized that WTC responders with OSA may have a distinct pathogenic mechanism related to their exposure. To examine this hypothesis more carefully, we defined a subgroup of WTCMMTP responders with infrequent or no snoring (score of <2) before 9/11, but worsening of snoring frequency after 9/11 (score of >3) (n = 26). They were compared with those who before 9/11 were habitual snorers (score of >3; n = 14) (Table 3). We found that the WTCMMTP responders who noted significant worsening of their snoring after 9/11 had a significantly lower BMI than in responders who were previously habitual snorers. They also reported a significantly shorter duration of snoring in their sleep questionnaire. Although WTCMMTP responders with an increase in snoring frequency after 9/11 had a significantly lower mean BMI, the severity of sleep-disordered breathing was no different from previously habitual snorers. Similarly, no significant differences were found in sleep quality, night time symptoms, ESS, or neurocognitive symptoms. Using the FEF50/FIF50 measurement as an index of dynamic upper airway obstruction, we found that both groups of WTCMMTP responders had a mean value greater than 1, suggestive of dynamic upper airway obstruction.
FIGURE 1.
Panels A and B show the correlation between weight and apnea + hypopnea index in the control and World Trade Center Medical Monitoring and Treatment Program (WTCMMTP) population. A significant and positive correlation (r = 0.29, P = 0.044) was found only in the control population (panel A). Panels C and D show the correlation between body mass index and apnea + hypopnea index in the control and WTCMMTP population. Again a significant and positive correlation (r = 0.36, P = 0.0096) was found only in the control population (panel C).
TABLE 3.
Differences Between Patients With No Change in Previous Frequent Snoring Symptoms and Those Whose Snoring Frequency Increased After World Trade Center Exposure
| Variable | Frequent Snoring Before (n = 14) | Increase in Frequency After (n = 26) | P |
|---|---|---|---|
| Age (yr) | 46.6 ± 7.1 | 47.0 ± 7.8 | 0.87 |
| Height (in) | 69.2 ± 4.1 | 70.7 ± 3.2 | 0.24 |
| Weight (kg) | 108.1 ± 17.0 | 100.9 ± 17.6 | 0.21 |
| Body mass index (kg/m2) | 35.2 ± 6.2 | 31.2 ± 4.7 | 0.047 |
| Weight gain (3 yr) (kg) | 6.8 ± 6.6 | 3.4 ± 7.0 | 0.15 |
| Snoring duration (yr) | 15.1 ± 9.3 | 8.3 ± 6.1 | 0.024 |
| Epworth Sleepiness Scale | 7.6 ± 5.3 | 10.6 ± 5.4 | 0.11 |
| Apnea + Hypopnea Index | 28.3 ± 25.2 | 21.6 ± 18.0 | 0.39 |
| REM Apnea + Hypopnea Index | 29.5 ± 37.2 | 29.6 ± 21.2 | 0.99 |
| Supine Apnea + Hypopnea Index | 40.3 ± 33.0 | 34.4 ± 28.3 | 0.62 |
| FEF50/FIF50 | 1.10 ± 0.54 | 1.11 ± 0.74 | 0.97 |
| FEV1/FVC | 0.77 ± 0.11 | 0.79 ± 0.06 | 0.81 |
| Witnessed apneas | 50.0% | 61.5% | 0.52 |
| Choking and gasping at night | 71.4% | 53.9% | 0.33 |
| Headaches | 64.3% | 65.4% | 1.00 |
| Difficulty with memory, concentration, and mood | 64.3% | 80.8% | 0.45 |
| Sleep-disordered breathing | 0.89 | ||
| Absent | 0% | 3.9% | |
| Mild | 50.0% | 46.2% | |
| Moderate | 14.3% | 23.1% | |
| Severe | 35.7% | 26.9% | |
| Sleep quality | 0.095 | ||
| Poor | 28.6% | 65.4% | |
| Fair | 42.9% | 19.2% | |
| Good | 28.6% | 15.4% | |
| Smoker (regular) | 0% | 11.5% | 0.30 |
| Alcohol | 0.80 | ||
| None | 21.4% | 11.5% | |
| Occasionally | 57.1% | 61.5% | |
| At least once a week | 21.4% | 26.9% |
± values are mean ± 1 SD.
FEF, forced expiratory flow; FEV1, forced expiratory volume in the first second; FIF, forced inspiratory flow; FVC, forced vital capacity; REM, rapid eye movement sleep.
DISCUSSION
Main Findings
We found a high prevalence of OSA in our sample of WTCMMTP responders. In contrast to a general population, we found no association between BMI or weight and AHI in this population. A subset of WTCMMTP responders who had developed habitual snoring after 9/11 had a significantly lower BMI than WTCMMTP responders who were habitual snorers before 9/11, despite having the same severity of OSA, indicating that obesity alone did not play a prominent role in their development of OSA. We believe that new onset upper airway inflammation should be considered a significant contributing factor in the pathogenesis of OSA in these individuals. That upper airway inflammation may play an important role in the pathogenesis of OSA in this population is also supported by the fact that symptoms of GERD and chronic rhinosinusitis were associated with an odds ratio of 2.7 and 2.21 of high risk for OSA in this population in a study by Webber et al.10 Chronic rhinosinusitis causes nasal mucosal congestion, increased nasal resistance, and flow limitation leading to conditions that are favorable to downstream pharyngeal collapse resulting in symptoms of habitual snoring, excessive daytime sleepiness, and increased likelihood of moderate to severe sleep-disordered breathing.9 Artificial nasal obstruction has been associated with a statistically significant increase in number of episodes of apnea and in apnea duration and treatment of nasal obstruction has resulted in reduction in the AHI and in the level of continuous positive airway pressure (CPAP) required in correcting OSA.12,13 The mechanism by which GERD might affect the development of OSA is less clear. Acid reflux into the upper airway could potentially lead to mucosal injury, edema, and airway obstruction.14
To understand the mechanism of OSA in the WTC responders, we examined the relationship of dynamic upper airway obstruction to the severity of OSA. Although the mean FEF50/FIF50 was greater than 1 in the WTCMMTP responders we found no association between the FEF50/FIF50 and AHI (data not shown) in either subgroup of WTCMMTP responders. These findings are consistent with previous studies that have shown that dynamic upper airway obstruction is not always associated with OSA.15,16
Comparison to Previous Studies
Our findings are significantly different from a recent publication by de la Hoz et al.11 Those authors found that OSA was associated with BMI and male sex in their sample of 100 WTCMMTP responders. It is likely that we did not find an association between BMI or weight and AHI, because we included only responders with aerodigestive disorders, whereas they included a broad sample of patients. The additional diagnoses likely diluted any effect of UAD on OSA pathogenesis and because WTCMMTP responders in general are middle-aged overweight men, the association between BMI and OSA was strengthened. De la Hoz et al also did not find an association between OSA and UAD. Nevertheless, these authors did not distinguish habitual snorers from those who had worsening of snoring after 9/11, allowing individuals with pre-existing OSA to potentially mask this association. Our study findings support the results of Webber et al10 who on the basis of questionnaire data found that in 11,701 responders, 16.9% of those not previously at high risk for OSA qualified as high risk for OSA after 9/11. Although, on the basis of a much smaller sample, confirmation of OSA with sleep studies in our study strengthens the case for WTC-induced sleep-disordered breathing.
Our study revealed a very high prevalence of OSA in both the referred population from the monitoring program and in our comparison population. This may have been because our study population was middle-aged men with a mean BMI greater than 30 and had aerodigestive symptoms, all factors that significantly increase the risk for OSA. The similarly high rate of OSA in our comparison population was also consistent with their demographic characteristics; that is, being middle-aged men with a high prevalence of obesity. The majority of the non-WTC responders had moderate to severe OSA, suggesting that referrals to our sleep center are largely snorers who have the characteristic clinical features of OSA.
Our study also found that both WTCMMTP responders and nonresponders had a similar degree of weight gain in the previous 3 years arguing against the hypothesis that the development of OSA is related to disabling psychological and physical comorbidities in this population. Sleep quality was worse in WTCMMTP responders, despite a lower AHI, suggesting other contributing factors to poor sleep quality in this population. Significant mental illness has persisted in 9/11 workers many years after exposure. An analysis performed on 10,132 workers indicated that 11.1% suffered from posttraumatic stress disorder (PTSD) and 5% suffered from depression. PTSD among WTC responders is reported to be higher than the US general population and comparable to returning Afghanistan war veterans.17 Poor sleep quality in our sample of responders may indeed be a marker of PTSD. The presence of PTSD independently increased the odds of high risk for OSA in this population but the mechanism is poorly understood.10
In summary, our study shows that in a sample of WTCMMTP responders with aerodigestive disorders who have sleep-related complaints, there is a high prevalence of OSA. The lack of association between BMI, or weight, and AHI is indicative of pathogenic mechanisms other than obesity in the development of OSA. This is further substantiated by the significantly lower BMI in WTCMMTP responders with increased frequency of snoring post 9/11. Poor sleep quality despite a significantly lower AHI indicates the presence of other factors such as PTSD in these individuals.
Limitations to the Study
A study of cross-sectional design can generate important hypotheses about the cause of OSA among WTC responders, but cannot make stronger statements about causality.
FEF50/FIF50 was not available for the comparison group and finally the members of the comparison group were from the general population in the area surrounding the sleep center and could potentially have had WTC-related exposures but were not part of the WTCMMTP.
These findings warrant a larger study to substantiate our results, and perhaps consideration of controlled trials to test the hypothesis of upper airway inflammation.
Learning Objectives.
Demonstrate familiarity with the types of persistent symptoms previously reported in World Trade Center (WTC) responders, including upper airway disease, gastroesophageal reflux disease, and obstructive sleep apnea (OSA).
Summarize the new findings, including differences in the factors associated with OSA and snoring in WTC responders versus nonresponder controls.
Discuss the implications for the pathogenesis of OSA in WTC responders.
Acknowledgments
Research was supported by Centers for Disease Control and Prevention and National Institute of Occupational Safety and Health (World Trade Center Medical Monitoring and Treatment Program grant UOH0088239) and Center Grant, NIEHS P30ES005022.
Footnotes
The JOEM Editorial Board and planners have no financial interest related to this research.
References
- 1.Herbert R, Moline J, Skloot G, et al. The World Trade Center disaster and the health of workers: five-year assessment of a unique medical screening program. Environ Health Perspect. 2006;114:1853–1858. doi: 10.1289/ehp.9592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.de la Hoz RE, Shohet MR, Chasan R, et al. Occupational toxicant inhalation injury: the World Trade Center (WTC) experience. Int Arch Occup Environ Health. 2008;81:479–485. doi: 10.1007/s00420-007-0240-x. [DOI] [PubMed] [Google Scholar]
- 3.Moline JM, Herbert R, Levin S, et al. WTC medical monitoring and treatment program: comprehensive health care response in aftermath of disaster. Mt Sinai J Med. 2008;75:67–75. doi: 10.1002/msj.20022. [DOI] [PubMed] [Google Scholar]
- 4.Webber MP, Gustave J, Lee R, et al. Trends in respiratory symptoms of firefighters exposed to the world trade center disaster: 2001–2005. Environ Health Perspect. 2009;117:975–980. doi: 10.1289/ehp.0800291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shelton KE, Woodson H, Gay S, Suratt PM. Pharyngeal fat in obstructive sleep apnea. Am Rev Respir Dis. 1993;148:462–466. doi: 10.1164/ajrccm/148.2.462. [DOI] [PubMed] [Google Scholar]
- 6.Valipour A, Makker HK, Hardy R, Emegbo S, Toma T, Spiro SG. Symptomatic gastroesophageal reflux in subjects with a breathing sleep disorder. Chest. 2002;121:1748–1753. doi: 10.1378/chest.121.6.1748. [DOI] [PubMed] [Google Scholar]
- 7.Leznoff A, Haight JS, Hoffstein V. Reversible obstructive sleep apnea caused by occupational exposure to guar gum dust. Am Rev Respir Dis. 1986;133:935–936. [PubMed] [Google Scholar]
- 8.McNicholas WT, Tarlo S, Cole P, et al. Obstructive apneas during sleep in patients with seasonal allergic rhinitis. Am Rev Respir Dis. 1982;126:625–628. doi: 10.1164/arrd.1982.126.4.625. [DOI] [PubMed] [Google Scholar]
- 9.Young T, Finn L, Kim H. Nasal obstruction as a risk factor for sleep-disordered breathing. The University of Wisconsin Sleep and Respiratory Research Group. J Allergy Clin Immunol. 1997;99:S757–S762. doi: 10.1016/s0091-6749(97)70124-6. [DOI] [PubMed] [Google Scholar]
- 10.Webber MP, Lee R, Soo J, et al. Prevalence and incidence of high risk for obstructive sleep apnea in World Trade Center–exposed rescue/recovery workers. Sleep Breath. 2010:1–12. doi: 10.1007/s11325-010-0379-7. [DOI] [PubMed] [Google Scholar]
- 11.de la Hoz RE, Aurora RN, Landsbergis P, Bienenfeld LA, Afilaka AA, Herbert R. Snoring and obstructive sleep apnea among former World Trade Center rescue workers and volunteers. J Occup Environ Med. 2010;52:29–32. doi: 10.1097/JOM.0b013e3181c2bb18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dayal VS, Phillipson EA. Nasal surgery in the management of sleep apnea. Ann Otol Rhinol Laryngol. 1985;94(pt 1):550–554. doi: 10.1177/000348948509400605. [DOI] [PubMed] [Google Scholar]
- 13.Friedman M, Tanyeri H, Lim JW, Landsberg R, Vaidyanathan K, Caldarelli D. Effect of improved nasal breathing on obstructive sleep apnea. Otolaryngol Head Neck Surg. 2000;122:71–74. doi: 10.1016/S0194-5998(00)70147-1. [DOI] [PubMed] [Google Scholar]
- 14.Jecker P, Orloff LA, Mann WJ. Extraesophageal reflux and upper aerodigestive tract diseases. ORL J Otorhinolaryngol Relat Spec. 2005;67:185–191. doi: 10.1159/000086662. [DOI] [PubMed] [Google Scholar]
- 15.Herer B, Roche N, Carton M, Roig C, Poujol V, Huchon G. Value of clinical, functional, and oximetric data for the prediction of obstructive sleep apnea in obese patients. Chest. 1999;116:1537–1544. doi: 10.1378/chest.116.6.1537. [DOI] [PubMed] [Google Scholar]
- 16.Krieger J, Weitzenblum E, Vandevenne A, Stierle JL, Kurtz D. Flow-volume curve abnormalities and obstructive sleep apnea syndrome. Chest. 1985;87:163–167. doi: 10.1378/chest.87.2.163. [DOI] [PubMed] [Google Scholar]
- 17.Stellman JM, Smith RP, Katz CL, et al. Enduring mental health morbidity and social function impairment in world trade center rescue, recovery, and cleanup workers: the psychological dimension of an environmental health disaster. Environ Health Perspect. 2008;116:1248–1253. doi: 10.1289/ehp.11164. [DOI] [PMC free article] [PubMed] [Google Scholar]