Abstract
Introduction
Chronic mesenteric ischemia (CMI) is a challenging problem, with revascularization the mainstay of treatment. Management of CMI is especially challenging in the patient with superior mesenteric artery (SMA) and celiac artery (CA) occlusions.
Report
We report a case series of four patients with chronic mesenteric ischemia who were not candidates for CA or SMA revascularization who were successfully treated with inferior mesenteric artery (IMA) angioplasty and stent placement to improve collateral circulation and palliate symptoms.
Discussion
To our knowledge, this is the largest case series to date reporting the use of an IMA stent to improve collateral circulation in patients with CMI.
Keywords: Chronic mesenteric ischemia, Endovascular treatment, Percutaneous transluminal angioplasty, Stent, Celiac artery, Celiac trunk, Inferior mesenteric artery, Superior mesenteric artery, Vascular disease
INTRODUCTION
Chronic mesenteric ischemia (CMI) is a challenging problem with a significant economic impact and a catastrophic outcome if left untreated.1 This case series reports four patients with chronic mesenteric ischemia who were not candidates for CA or SMA revascularization but who were successfully treated with inferior mesenteric artery (IMA) angioplasty and stent placement to improve collateral circulation and palliate symptoms.
CASE SERIES
Patient number 1
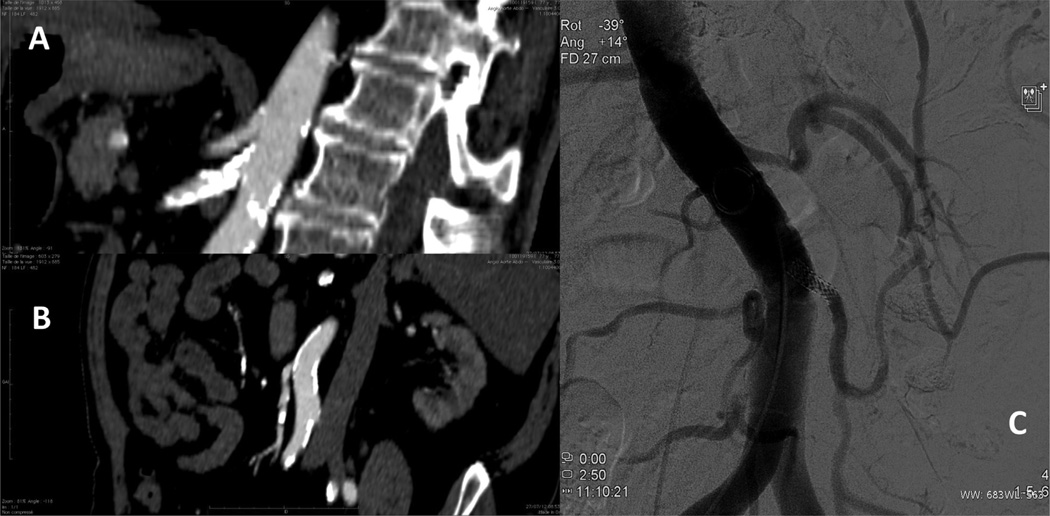
A 77-year-old male with hypertension, type II diabetes, ischemic cardiomyopathy, and tobacco abuse presented with a three week history of severe postprandial abdominal pain. A computed tomography (CT) scan revealed a high-grade stenosis of the first 3 cm of the superior mesenteric artery (SMA), which was also highly calcified. The celiac trunk was calcified along its entire course but appeared to be patent, without significant stenosis (Fig. 1A). The inferior mesenteric artery (IMA) had a tight stenosis at its origin but was otherwise patent, with a well-developed Riolan arcade (Fig. 1B). Because the entire length of the SMA was diseased and heavily calcified, and no stenosis could be identified along the celiac trunk, neither the SMA nor the celiac trunk was a target for intervention. As the Riolan arcade was well developed, IMA stenting was chosen. Angioplasty was performed via a left brachial puncture and a 6 × 18 mm stent (Herculink, Boston, MA, USA) placed. Two stenoses, one at the origin of the left colic and one at the origin of the superior rectal artery, were also dilated by balloon angioplasty (Fig. 1C). The postoperative course was uneventful and the abdominal pain resolved completely. Six months after the operation, the patient underwent a control angiogram that showed a patent stent without intrastent stenosis. One year after the procedure, a duplex ultrasound and a CT scan both showed a patent stent and the patient remains asymptomatic.
Figure 1.
Patient number 1 preoperative image, with a computed tomography angiogram revealing a high-grade stenosis of the first 3-cm of a heavily calcified superior mesenteric artery and a widely patent celiac artery (A). The inferior mesenteric artery had a tight stenosis at its origin but otherwise appeared patent, with a well-developed Riolan arcade (B). Completion angiogram shows stent in the inferior mesenteric artery (C).
Patient number 2
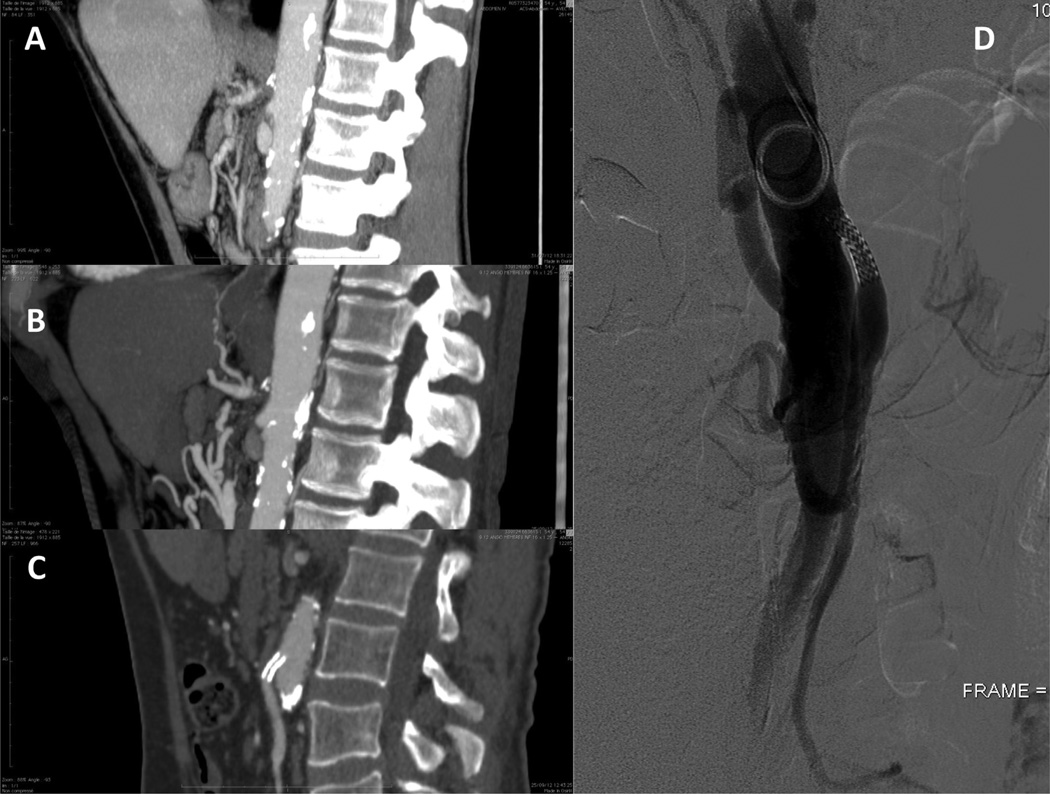
A 54-year-old male with ischemic cardiomyopathy, tobacco abuse, and previous stroke presented with postprandial abdominal pain and 40 pound weight loss over the previous 4 months. Esophagogastroduodenoscopy showed no identifiable abnormalities. CT scan showed a 4.5-cm segment of thrombosed SMA, a short occlusion of the celiac trunk, and a tight stenosis of the IMA consistent with chronic mesenteric ischemia (Fig. 2A, B).
Figure 2.
Patient number 2. A computed tomography scan showed a 4.5-cm segment of thrombosed superior mesenteric artery, and stenosis of the celiac trunk, consistent with chronic mesenteric ischemia (A). At the end of the case, angiography showed perfusion of the Riolan arcade and branches of the inferior mesenteric artery (B). Postoperative computed tomography scan and 6-month follow-up angiogram showing patent stent in the inferior mesenteric artery (C, D).
A 5 × 15 mm stent was placed (Herculink) via a percutaneous brachial approach. Control angiography showed perfusion of the Riolan arcade and branches of the IMA (Fig. 2C). Postoperatively, the abdominal pain resolved completely. At 6-month follow-up he had recovered his normal weight. A control angiogram and a duplex scan showed no intrastent stenosis (Fig. 2D). Seven months later, the stent was still patent but the patient presented with recurrent abdominal pain. An antegrade prosthetic bypass from the supra coeliac aorta to revascularize the celiac trunk, SMA, and IMA was performed. The patient recovered uneventfully.
Patient number 3
A 70-year-old male with hypertension, tobacco abuse, severe alcoholism, and cirrhosis presented with worsening abdominal pain for several weeks and 20 pound weight loss in the previous 2 months. A CT scan showed short occlusions of the celiac trunk and SMA, and a tight stenosis of the IMA. The SMA and celiac trunk were highly calcified and deemed unsuitable for safe endovascular treatment. The patient was turned down for open repair. A 6 × 20 mm IMA stent (Formula™ Cook Medical, Bloomington, IN, USA) stent was placed. At review 3 months after the procedure, the patient was asymptomatic and had recovered his normal weight. Six months after the procedure, a control angio-gram showed an intrastent stenosis. Intrastent angioplasty was performed. The patient remained asymptomatic 1 year after the procedure, with a duplex scan and a CT scan showing a widely patent IMA stent.
Patient number 4
This patient was a 48-year-old female with hypertension, tobacco abuse, hyperlipidemia, pulmonary embolism, deep vein thrombosis, factor II deficiency, activated protein C resistance, HIV, and hepatitis C. The past medical history included a saphenous vein aortomesenteric bypass for chronic mesenteric ischemia. Six months after this operation, an angioplasty of the bypass was performed for symptomatic stenosis, followed by stenting of the bypass 1 year later for continued symptoms. She presented 2 years later with occlusion of the bypass and recurrent pain. At this point she received a 6 × 20 mm IMA stent (Formula Cook Medical, Bloomington, IN, USA) with good angiographic result. Six months after the operation, she remained asymptomatic, with no intrastent restenosis on duplex scan and CT scan.
DISCUSSION
To our knowledge, this is the largest case series to date reporting the use of an IMA stent to improve collateral circulation in patients with CMI. This technique of IMA stenting has also been corroborated by a German group who reported technical success and excellent short term results in three patients.2
Surgical revascularization remains the gold standard for CMI. Inflow may be from the supraceliac/descending thoracic or ascending aorta (antegrade) or the infrarenal aorta or common iliac artery (retrograde). Outflow is most frequently to the CA and SMA, and rarely to the IMA. A recent case series of 98 patients with CMI reported a 92% 5-year symptom-free survival with two-vessel reconstruction (celiac, SMA); IMA reconstruction added morbidity to the surgery and was considered unnecessary.3 In spite of excellent outcomes using surgical bypass, many patients with CMI cannot tolerate an open procedure; therefore, these patients become candidates for endovascular revascularization. 4 For these reasons, the preferred strategy is to perform SMA and/or CA revascularization whenever possible. IMA stenting rather than CA/SMA revascularization is performed only in the setting of long or heavily calcified lesions of the SMA/CA.
The current surveillance plan includes duplex scan at 1 month, 3 months, and every 6 months, CT angiogram at 3 months and yearly thereafter, followed by angiogram at 6 months. We perform angiography in order to detect occult intrastent stenosis not seen on the CT angiogram. Patients are placed on double antiplatelet therapy for at least 6 months postoperatively.
Footnotes
CONFLICT OF INTEREST
None.
REFERENCES
- 1.Chandra A, Quinones-Baldrich WJ. Chronic mesenteric ischemia: how to select patients for invasive treatment. Semin Vasc Surg. 2010;23(1):21–28. doi: 10.1053/j.semvascsurg.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 2.Aschenbach R, Bergert H, Kerl M, Zangos S, Neumeister A, Schlosser A, et al. Stenting of stenotic mesenteric arteries for symptomatic chronic mesenteric ischemia. Vasa. 2012;41(6):425–431. doi: 10.1024/0301-1526/a000232. [DOI] [PubMed] [Google Scholar]
- 3.Park WM, Cherry KJ, Jr, Chua HK, Clark RC, Jenkins G, Harmsen WS, et al. Current results of open revascularization for chronic mesenteric ischemia: a standard for comparison. J Vasc Surg. 2002;35(5):853–859. doi: 10.1067/mva.2002.123753. [DOI] [PubMed] [Google Scholar]
- 4.Kasirajan K, O’Hara PJ, Gray BH, Hertzer NR, Clair DG, Greenberg RK, et al. Chronic mesenteric ischemia: open surgery versus percutaneous angioplasty and stenting. J Vasc Surg. 2001;33:63–71. doi: 10.1067/mva.2001.111808. [DOI] [PubMed] [Google Scholar]