Abstract
The purpose of this study was to compare the acetabular version between male and female pelvises. We hypothesized that female acetabula would demonstrate more retroversion because Pincer-type femoroacetabular impingement (FAI) is associated with acetabular retroversion, which is more commonly observed in females. 120 bony pelvic specimens were randomly collected. The version was measured at three different axial sections of each acetabuli: cranial, central, and caudal. Males demonstrated significantly less anteversion than females in every section. The global version (the average of all three measurements) was also significantly different between males and females (16°±7° and 19°±8° respectively, p<0.001). Of the 240 examined acetabuli, 21 demonstrated cranial retroversion (16 males & 5 females). The data showed no significant difference (p=0.353) between global version of African Americans (18°±9°) and Caucasians (17°±7°). The results of this study suggest that symptomatic FAI in the female population likely reflects a complex interplay of femoral and acetabular dysmorphology and cannot be explained by differences in acetabular version alone.
Keywords: femoroacetabular impingement, hip impingement, acetabular retroversion, pincer impingement, hip pain
Introduction
Femoroacetabular impingement (FAI) was first described as a cause of early osteoarthritis of the hip by Smith-Petersen in 1936 [1]. However, FAI has only recently become widely accepted as a primary disease process and as a significant cause of hip pain in younger patients [2] [3] [4] [5] [6] [7] [8]. Previous studies have associated FAI with both femoral and acetabular anatomic abnormalities as well as a complication of periacetabular osteotomies and malunited femoral neck fractures [9] [10]. Today, FAI has been associated with the development of early hip osteoarthritis [11] [12]. The repetitive collision of anatomic abnormalities of the proximal femur and/or acetabulum with dynamic hip motion results in damage to the labrum and chondral surfaces [13].
The pathoanatomy of FAI has been classified as either acetabular-sided (“pincer”), femoral-sided (“cam”) deformity, or combined (both cam and pincer abnormalities are present) [14] [15]. Camtype FAI is more prevalent in younger males and results from either a decreased femoral head-neck offset, a nonspherical femoral head or a decrease in the angle of the head and neck of the femur relative to the femoral condyles (femoral retrotorsion) [7] [15] [16] [14] [17]. Frequently a bump can be seen on frog-leg lateral radiographs at the head neck junction where the impingement takes place. This bump is often referred to as a "pistol grip" deformity. Pincer-type FAI has been reported to be more prevalent in active, middle-aged women and involves global retroversion, global overcoverage (protrusio acetabuli, coxa profunda), or focal overcoverage (cephalad acetabular retroversion) of the femoral head-neck junction by the anterior rim of the acetabulum [2] [8] [18] [19] [20].
Increased focal or global acetabular retroversion may predispose patients to mechanical impingement and help to explain clinical differences observed between the male and female population [21]. However, no studies to-date have quantified the differences in prevalence of relative and absolute acetabular retroversion (version <0°) between males and females. Therefore, the purpose of the present study was to define differences in acetabular version between genders. Based on a higher prevalence of pincer-type impingement in females, we hypothesize that females of both races will demonstrate more relative and absolute retroversion than males [15].
Materials and Methods
IRB approval was not required given no human subject information was gathered in this project. The Hamann-Todd Human Osteological Collection at the Cleveland Museum of Natural History has 2,967 skeletal specimens. This collection has previously been examined in multiple published orthopedic studies [22] [23] [24]. One hundred and twenty (sixty male and sixty female) randomly collected pelvic specimens (240 hips), including the corresponding sacrums, were inspected. Race and mean age were held constant between the two genders. The mean age within both categories was 32 years old (range: 14 to 60 years). The specimens were representative of the population of Cleveland, Ohio during the early 20th century.
The measurement techniques were adopted from Jamali et al [25]. Each pelvis and sacrum was rearticulated using rubber bands and a 5cm thick foam piece in place of the pubis symphysis (Fig. 1). The plane formed between the anterior superior iliac spines (ASIS) and the pubic symphysis was used to define the anatomic frontal plane of reference of the pelvis. During normal upright standing and walking, this plane is positioned vertically [26] [27]. To stabilize the pelvic specimens while taking measurements, the specimens were set on a flat table with the ASIS and the pubic symphysis rested against the table. Thus, the table defined the anatomic frontal plane.
Fig. 1.
Pelvis measurement techniques were adopted from Jamali et al [25].
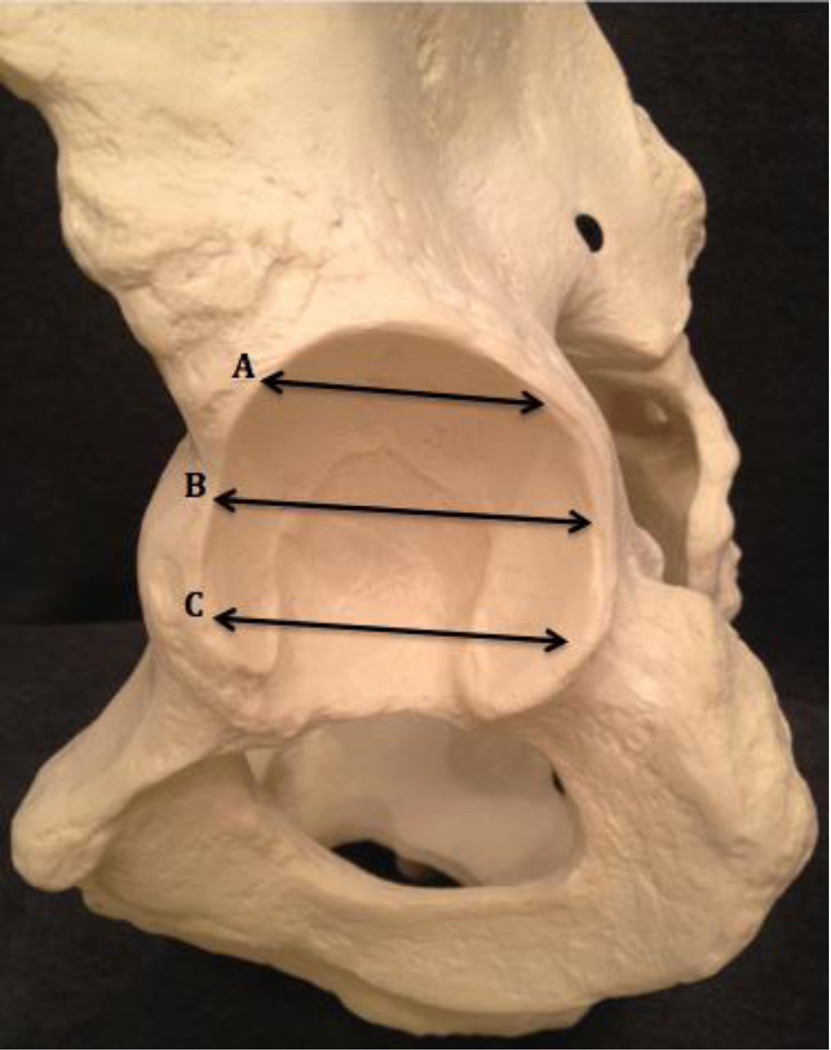
Acetabular version (AV) was measured using a goniometer at three separate axial sections as described by Jamali et al [25]: cranial (5mm distal to the acetabular roof), central (through the longitudinal center of the acetabulum), and caudal (5mm proximal from the most inferior edge of the acetabular cavity) (Fig. 2). Most focal rim impingement lesions are encountered anterosuperiorly, and therefore were represented by the cranial measurement location [28]. All calculations were rounded to the nearest whole number. The global version for each of the 240 acetabulum was calculated by taking the average of the three separate measurements (cranial, central, and caudal). These global version values were then averaged to come up with the overall mean global version.
Fig. 2.
(A) Cranial version: 5 mm distal to the acetabular roof. (B) Central version: through the longitudinal center of the acetabulum. (C) Caudal version: 5mm proximal to the most inferior edge of the acetabular cavity.
The plane perpendicular to the anatomical frontal plane was set as 0°. Thus, AV angles were defined as positive (absolute anteversion) if the acetabulum tilted outward or lateral to this plane and negative (absolute retroversion) if the acetabulum tilted inward or medial to this plane.
Data collected from a pilot study measuring AV of 50 skeletal specimens demonstrated a mean difference of 2°±6° in global acetabular version between genders. Based on information from this pilot study, a power analysis determined that a minimum of n=119 would be necessary to detect a statistically significant difference between groups with a power of 0.80 and a significance of p<0.05. Therefore, we chose a sample size of n=120 specimens for our study. Data are expressed as mean ± the standard deviation. Statistical comparisons were performed using one-way ANOVA tests and two-tailed t-test.
Results
The mean global AV of the population was found to be 17°±9°. The mean cranial AV (12°±9°) was significantly less than the mean central AV (20°±8°) (p<0.001), but no significant difference was found between the central and the caudal AV (21°±8°) (p=0.162). Furthermore, 8.75% (21/240) acetabuli were cranially retroverted (bilaterally in one pelvis and unilaterally in the other nineteen). However, none of the pelvi demonstrated absolute central or caudal retroversion. Of the 71 acetabuli that demonstrated central AV between 10° and 15°, 21 (29.57%) were cranially retroverted, and above 15° of central AV, only 1 acetabuli was cranially retroverted.
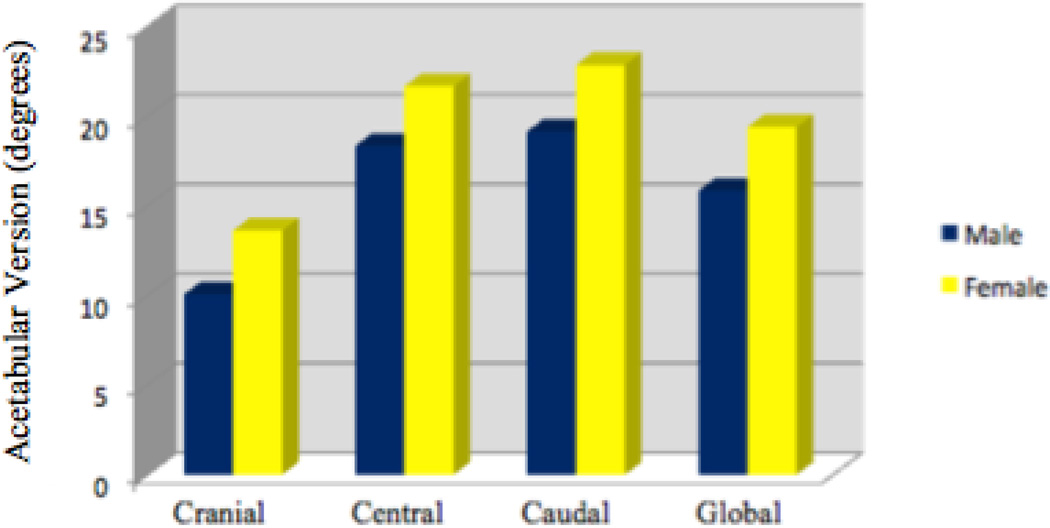
The global male version (16°±7°) and global female version (19°±8°) were significantly different (p<.001), with females demonstrating greater relative anteversion (Fig. 3). The data showed a significant difference (p=0.003) between the male cranial AV (10°±8°) and female cranial AV (14°±10°) (Table 1). There was also a significant difference (p=0.001) between male central AV (18°±7°) and female central AV (22°±8°). A significant difference (p<0.001) between male caudal AV (19°±7°) and female caudal AV (23°±8°) was also observed. Thus, females were significantly more anteverted in all measurements. Lastly, of all 21 acetabuli with absolute cranial retroversion, 16 (76.2%) were male and 5 (23.8%) were female.
Fig. 3.
Mean gender differences in acetabular version.
Table 1.
Gender differences in mean AV ± SD
| Group | Cranial | Central | Caudal | Global |
|---|---|---|---|---|
| Males | 10°±8° | 18°±7° | 19°±7° | 16°±7° |
| Females | 14°±10° | 22°±8° | 23°±8° | 19°±8° |
| P value | 0.003 | 0.001 | 0<.001 | 0<.001 |
The data showed no significant difference (p=0.353) between African American AV (18°±9°) and Caucasian AV (17°±7°). Furthermore, when comparing African American males to Caucasian males none of the AV’s measured were significantly different. Similarly, when comparing African American females to Caucasian females, none of the AV’s measured were significantly different (Tables 2–3).
Table 2.
Race/Gender differences in mean AV ± SD
| Group | Cranial | Central | Caudal | Global |
|---|---|---|---|---|
| African American males | 11°±10° | 19°±8° | 19°±8° | 16°± 8° |
| Caucasian males | 10°±7° | 18°± 5° | 19°± 6° | 15°±6° |
| African American females | 14°±10° | 22°±8° | 23°±9° | 20°±8° |
| Caucasian females | 13°± 9° | 21°±8° | 23°± 7° | 19°±8° |
Table 3.
P values for differences between races
| Group | Cranial | Central | Caudal | Global |
|---|---|---|---|---|
| Males | 0.542 | 0.3 | 0.682 | 0.473 |
| Females | 0.736 | 0.3 | 0.669 | 0.528 |
Discussion
Increased focal or global acetabular retroversion may predispose patients to femoroacetabular impingement and help to explain clinical differences observed between the male and female population [21]. In the current study, we have defined significant differences in the global and focal acetabular version observed between different gender and race populations using a previously validated osteological collection in pre-arthritic patients [22] [23] [24]. In contrast to our hypothesis, males demonstrated significantly greater relative and absolute acetabular retroversion than females. No significant differences in African American and Caucasian populations were observed.
The repetitive collision of the proximal femur with a rim lesion during dynamic hip motion results in predictable damage to the labrum and chondral surfaces. With rim lesions, the labrum is primarily damaged and bone apposition occurs on the osseous rim adjacent to the labrum [29] [30]. The labrum itself becomes thinner until it is no longer distinguishable. The acetabular cartilage adjacent to the involved labrum undergoes degeneration, but in a rather thin strip. Rim lesions can also result in “contre-coup” chondral injury that is believed to result from flexion or rotation of the hip beyond engagement of the focal rim lesion, resulting in levering of the femoral head and abnormal shear forces on the posterior chondral surfaces. Correspondingly, Giori and Trousdale found primary osteoarthritis to be significantly more prevalent in patients with acetabular retroversion (20%) than in patients without retroversion (5%) [20].
Although past clinical studies have suggested that women generally suffer from pincer-type impingement more often than men, our studies suggest that this discrepancy is not due to a higher incidence of relative or absolute acetabular retroversion in women. Recognition of true acetabular retroversion is critical to guide surgical treatment. Unlike a focal rim impingement lesion seen with cephalad retroversion, true “global” acetabular retroversion is accompanied by posterior “undercoverage” and can even result in posterior instability or dislocation. Isolated open or arthroscopic management with an aggressive anterior rim decompression may fail to address the overall deformity and result in iatrogenic anterior and posterior wall deficiency. An “anteverting” periacetabular osteotomy to provide anteversion correction of the acetabulum and improve mechanics between the femoral head-neck junction and the acetabular rim may be more appropriate in this setting [31] [32].
We found the incidence of acetabular retroversion to be higher among men, which supports the thought that a higher prevalence of pincer-type FAI seen in women must be due to other contributing factors. Perhaps examining combined acetabular and femoral version rather than acetabular version in isolation may provide more information regarding potential risk factors for FAI. D’Lima et al examined the effects of acetabular and femoral orientation on hip range of motion and found that combined femoral and acetabular anteversion had an additive effect on hip flexion [33]. Thus, despite males demonstrating more acetabular retroversion, examination of the total hip (i.e. acetabular and femoral version) may show women to have more femoral retroversion contributing to higher rates of FAI.
Furthermore, superphysiologic motion (i.e. excessive hip flexion) may also play a role in causing pincer FAI in women. Many middle-aged women suffering from pincer-type impingement often engage in activities that require extreme ranges of motion such as yoga. These activities may result in increased dynamic capsular laxity in female patients allowing for superphysiologic motion and dynamic impingement despite appropriate acetabular anteversion [34] [35]. Another possible mechanism may be an increased pelvic rotation (flexion) in women possibly due to weaker abdominal muscles.
In addition to acetabular retroversion, other pathoanatomic mechanisms of pincer impingement could be contributing to this observed gender difference. Coxa profunda, protrusio acetabuli, femoral retroversion, coxa vara, and os acetabuli are other distinct anatomic parameters that need to be investigated further for possible differences between males and females [36] [37] [38] [39] [40]. Primary protrusio acetabuli has shown to have a bilateral manifestation with a female dominance [29].
Acknowledgments
The research study did have some limitations worth noting. One limitation of this study was that we examined a random population of pelvic specimens, not particularly those identified to have FAI. In this regard, we examined a more “normal” population and not one known to have dysmorphology resulting in pathologic impingement. In addition, we have examined acetabular version in isolation. FAI results from a complex interplay of dynamic and static mechanical factors, including cam lesions, rim lesions, femoral and acetabular version, neck-shaft angle and acetabular dysplasia. We have treated these variables as independent, but they may in fact have co-variable relationships that predispose to mechanical impingement. For example, cam lesions with significant femoral retroversion are at a considerably greater risk for mechanical impingement with internal rotation compared to those lesions in the setting of increased femoral anteversion. Furthermore, relative or absolute acetabular retroversion may predispose to the most typical type of FAI seen anteriorly and anterosuperiorly. In contrast, focal or global retroversion of the acetabulum may have ameliorating effects on impingement related to superolateral or posterior cam lesions. Also, pelvic rotation and lordosis can be highly variable between patients and certainly influences the functional acetabular version. We acknowledge this limitation as we have examined these specimens in a “standardized” position. Lastly, since our population only consisted of pelvises from Caucasians and African Americans, the results of this study may not be relevant to other races.
This study has demonstrates that the higher incidence of pincer-type FAI commonly reported in women cannot be solely explained by a higher incidence of acetabular retroversion in women. Although acetabular retroversion has been shown to play a significant role in the development of pincer-type FAI, this study revealed that male acetabulum are statistically significantly more retroverted than female acetabulum. Thus, the higher incidence of pincer-type FAI observed in females must be explained by some other factor or mechanism in women that predisposes them to this pathology. Further research must be done in order to uncover the underlying differences in male and female hip joint anatomy and biomechanics causing women to be more prone to developing pincer-type FAI.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Smith-Petersen MN. The classic: Treatment of malum coxae senilis, old slipped upper femoral epiphysis, intrapelvic protrusion of the acetabulum, and coxa plana by means of acetabuloplasty. 1936. Clin Orthop Relat Res. 2009;467(3):608. doi: 10.1007/s11999-008-0670-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dandachli W, Islam SU, Liu M, et al. Three-dimensional CT analysis to determine acetabular retroversion and the implications for the management of femoro-acetabular impingement. J Bone Joint Surg Br. 2009;91(8):1031. doi: 10.1302/0301-620X.91B8.22389. [DOI] [PubMed] [Google Scholar]
- 3.Beck M, Leunig M, Parvizi J, et al. Anterior femoroacetabular impingement: part II. Midterm results of surgical treatment. Clin Orthop Relat Res. 2004;(418):67. [PubMed] [Google Scholar]
- 4.Ganz R, Parvizi J, Beck M, et al. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 5.Murphy S, Tannast M, Kim YJ, et al. Debridement of the adult hip for femoroacetabular impingement: indications and preliminary clinical results. Clin Orthop Relat Res. 2004;(429):178. doi: 10.1097/01.blo.0000150307.75238.b9. [DOI] [PubMed] [Google Scholar]
- 6.Tanzer M, Noiseux N. Osseous abnormalities and early osteoarthritis: the role of hip impingement. Clin Orthop Relat Res. 2004;(429):170. [PubMed] [Google Scholar]
- 7.Siebenrock KA, Wahab KH, Werlen S, et al. Abnormal extension of the femoral head epiphysis as a cause of cam impingement. Clin Orthop Relat Res. 2004;(418):54. doi: 10.1097/00003086-200401000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Kim WY, Hutchinson CE, Andrew JG, et al. The relationship between acetabular retroversion and osteoarthritis of the hip. J Bone Joint Surg Br. 2006;88(6):727. doi: 10.1302/0301-620X.88B6.17430. [DOI] [PubMed] [Google Scholar]
- 9.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;(363):93. [PubMed] [Google Scholar]
- 10.Eijer H, Myers SR, Ganz R. Anterior femoroacetabular impingement after femoral neck fractures. J Orthop Trauma. 2001;15(7):475. doi: 10.1097/00005131-200109000-00003. [DOI] [PubMed] [Google Scholar]
- 11.Gosvig KK, Jacobsen S, Sonne-Holm S, et al. Prevalence of malformations of the hip joint and their relationship to sex, groin pain, and risk of osteoarthritis: a population-based survey. J Bone Joint Surg Am. 92(5):1162. doi: 10.2106/JBJS.H.01674. [DOI] [PubMed] [Google Scholar]
- 12.Bardakos NV, Villar RN. Predictors of progression of osteoarthritis in femoroacetabular impingement: a radiological study with a minimum of ten years follow-up. J Bone Joint Surg Br. 2009;91(2):162. doi: 10.1302/0301-620X.91B2.21137. [DOI] [PubMed] [Google Scholar]
- 13.Parmar R, Parvizi J. The multifaceted etiology of acetabular labral tears. Surg Technol Int. 20:321. [PubMed] [Google Scholar]
- 14.Ganz R, Leunig M, Leunig-Ganz K, et al. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264. doi: 10.1007/s11999-007-0060-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pfirrmann CW, Mengiardi B, Dora C, et al. Cam and pincer femoroacetabular impingement: characteristic MR arthrographic findings in 50 patients. Radiology. 2006;240(3):778. doi: 10.1148/radiol.2403050767. [DOI] [PubMed] [Google Scholar]
- 16.Ganz R, Leunig M, Ganz KL, et al. Reflections on the Cause of Osteoarthritis of the Hip. The Orthopaedic Journal at Harvard Medical School. 2007;9:76. [Google Scholar]
- 17.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;(213):20. [PubMed] [Google Scholar]
- 18.Reynolds D, Lucas J, Klaue K. Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br. 1999;81(2):281. doi: 10.1302/0301-620x.81b2.8291. [DOI] [PubMed] [Google Scholar]
- 19.Banks KP, Grayson DE. Acetabular retroversion as a rare cause of chronic hip pain: recognition of the "figure-eight" sign. Skeletal Radiol. 2007;36(Suppl 1):S108. doi: 10.1007/s00256-006-0150-0. [DOI] [PubMed] [Google Scholar]
- 20.Giori NJ, Trousdale RT. Acetabular retroversion is associated with osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):263. doi: 10.1097/01.blo.0000093014.90435.64. [DOI] [PubMed] [Google Scholar]
- 21.Maruyama M, Feinberg JR, Capello WN, et al. The Frank Stinchfield Award: Morphologic features of the acetabulum and femur: anteversion angle and implant positioning. Clin Orthop Relat Res. 2001;(393):52. [PubMed] [Google Scholar]
- 22.Ganapathi A, McCarron JA, Chen X, et al. Predicting normal glenoid version from the pathologic scapula: A comparison of 4 methods in 2- and 3-dimensional models. J Shoulder Elbow Surg. doi: 10.1016/j.jse.2010.05.024. [DOI] [PubMed] [Google Scholar]
- 23.Codsi MJ, Bennetts C, Powell K, et al. Locations for screw fixation beyond the glenoid vault for fixation of glenoid implants into the scapula: an anatomic study. J Shoulder Elbow Surg. 2007;16(3 Suppl):S84. doi: 10.1016/j.jse.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 24.Smucker JD, Akhavan S, Furey C. Understanding bony safety zones in the posterior iliac crest: an anatomic study from the Hamann-Todd collection. Spine (Phila Pa 1976) 35(7):725. doi: 10.1097/BRS.0b013e3181d39091. [DOI] [PubMed] [Google Scholar]
- 25.Jamali AA, Mladenov K, Meyer DC, et al. Anteroposterior pelvic radiographs to assess acetabular retroversion: high validity of the"cross-over-sign". J Orthop Res. 2007;25(6):758. doi: 10.1002/jor.20380. [DOI] [PubMed] [Google Scholar]
- 26.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970;52(1):148. [PubMed] [Google Scholar]
- 27.Visser JD, Jonkers A, Hillen B. Hip joint measurements with computerized tomography. J Pediatr Orthop. 1982;2(2):143. doi: 10.1097/01241398-198202020-00005. [DOI] [PubMed] [Google Scholar]
- 28.Rylander L, Froelich JM, Novicoff W, et al. Femoroacetabular impingement and acetabular labral tears. Orthopedics. 33(5):342. doi: 10.3928/01477447-20100329-21. [DOI] [PubMed] [Google Scholar]
- 29.Leunig M, Nho SJ, Turchetto L, et al. Protrusio acetabuli: new insights and experience with joint preservation. Clin Orthop Relat Res. 2009;467(9):2241. doi: 10.1007/s11999-009-0853-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Dolan MM, Heyworth BE, Bedi A, et al. CT Reveals a High Incidence of Osseous Abnormalities in Hips with Labral Tears. Clin Orthop Relat Res. doi: 10.1007/s11999-010-1539-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nehme A, Trousdale R, Tannous Z, et al. Developmental dysplasia of the hip: is acetabular retroversion a crucial factor? Orthop Traumatol Surg Res. 2009;95(7):511. doi: 10.1016/j.otsr.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 32.Xie J, Naito M, Maeyama A. Evaluation of acetabular versions after a curved periacetabular osteotomy for dysplastic hips. Int Orthop. 34(4):473. doi: 10.1007/s00264-009-0785-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.D'Lima DD, Urquhart AG, Buehler KO, et al. The effect of the orientation of the acetabular and femoral components on the range of motion of the hip at different head-neck ratios. J Bone Joint Surg Am. 2000;82(3):315. doi: 10.2106/00004623-200003000-00003. [DOI] [PubMed] [Google Scholar]
- 34.Ranawat AS, McClincy M, Sekiya JK. Anterior dislocation of the hip after arthroscopy in a patient with capsular laxity of the hip. A case report. J Bone Joint Surg Am. 2009;91(1):192. doi: 10.2106/JBJS.G.01367. [DOI] [PubMed] [Google Scholar]
- 35.Tibor LM, Sekiya JK. Differential diagnosis of pain around the hip joint. Arthroscopy. 2008;24(12):1407. doi: 10.1016/j.arthro.2008.06.019. [DOI] [PubMed] [Google Scholar]
- 36.Ruelle M, Dubois JL. [The protrusive malformation and its arthrosic complication. I. Radiological and clinical symptoms. Etiopathogenesis.] Rev Rhum Mal Osteoartic. 1962;29:476. [PubMed] [Google Scholar]
- 37.Beck M, Kalhor M, Leunig M, et al. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012. doi: 10.1302/0301-620X.87B7.15203. [DOI] [PubMed] [Google Scholar]
- 38.Gilmour J. Adolescent deformities of the acetabulum: an investigation into the nature of protrusio acetabuli. Brit J Surg. 1939;26:670. [Google Scholar]
- 39.Amstutz HC, Wilson PD., Jr Dysgenesis of the proximal femur (coxa vara) and its surgical management. J Bone Joint Surg Am. 1962;44-A:1. [PubMed] [Google Scholar]
- 40.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991;73(3):423. doi: 10.1302/0301-620X.73B3.1670443. [DOI] [PubMed] [Google Scholar]