Abstract
Background
Biospecimen collection from diverse populations can advance cancer disparities research, but is currently underrepresented.
Methods
We partnered with a community-based clinic serving Cantonese-speaking Chinese Americans to develop and revise an educational seminar on biospecimen collection. Through a randomized controlled trial (n = 395), the intervention seminar was compared with a control seminar (cancer prevention) on change in willingness to donate biospecimens.
Results
At baseline, many were willing to donate a biospecimen (saliva, urine, hair, toenails, blood, unused cancerous tissue) whether healthy or hypothetically had cancer. Also, many would donate because future generations would benefit, and few had concerns about donation. In logistic regression analyses, there was an intervention effect for willingness to donate: urine if had cancer [OR, 2.2; 95% confidence interval (CI), 1.3–3.7], toenails if healthy (OR, 2.1; 95% CI, 1.4–3.2) or had cancer (OR, 2.3; 95% CI, 2.0–2.7), hair if healthy (OR, 1.8; 95% CI, 1.3–2.5) or had cancer (OR, 2.8; 95% CI, 1.9–4.0), and unused cancerous tissue (OR, 1.8; 95% CI, 1.2–2.9). There was also an intervention effect for donating because future generations would benefit (OR, 2.0; 95% CI, 1.4–3.0), and this attitude was a strong independent predictor for willingness to donate all biospecimens, whether healthy or had cancer (OR, 2.9–4.2).
Conclusion
Cantonese-speaking Chinese American participants of an educational seminar on biospecimen collection showed greater increases in willingness to donate biospecimens and donating for the benefit of future generations, than participants who attended a control seminar.
Impact
Donating for the benefit of future generations is a theme that should be incorporated in messages that encourage biospecimen donation for Chinese Americans.
Introduction
Biospecimen collection will advance the development of personalized cancer therapeutics and prevention agents (1), and including diverse populations has the potential to advance cancer disparities research (2). Biospecimens are defined by the National Cancer Institute (Bethesda, MD) as “biologic materials from people such as tissue, blood, plasma, and urine.”(3) However, the most significant roadblock to such research is “the limited availability of carefully collected and controlled, high-quality human biospecimens annotated with essential clinical data and properly consented for broad investigational use.”(3) Implicit in this challenge is the need to collect biospecimens from diverse racial and ethnic minorities (4), specifically, African American, American Indian, Asian, Hispanic, and Native Hawaiian, and Pacific Islanders. Although some research has been conducted with Western European populations (5–7), little is known about the baseline knowledge, attitudes, and behaviors related to biospecimen collection among most racial/ethnic minority populations (8, 9). Furthermore, appropriate messages that might increase biospecimen donations have yet to be explored and developed. The purpose of this study was to evaluate the impact of an educational seminar on an Asian American community’s willingness to donate biospecimens in a randomized, controlled trial.
For this study, we chose to examine a subset of Chinese Americans, the largest Asian American population in the United States (10), due to this subset’s higher smoking prevalence rates, and thus higher cancer risk. All Chinese Americans are not alike. Chinese Americans typically speak: English, the preferred language for the most acculturated; Mandarin or Putonghua for the more highly educated from China or Taiwan; or Cantonese, for the earlier Chinese settlers who tend to cluster in the “Chinatowns” and reflect more blue-collar occupations (e. g., restaurants; ref. 11). Cantonese-speaking men may have a higher cancer risk because they have the highest smoking prevalence rate (21.7%) among Californian Chinese, compared with 7.2% for English-speaking and 14.1% for Mandarin-speaking men; this rate is higher than the general California population whose rate is 15.2% (12).
A culturally-tailored seminar may address traditional perspectives of Chinese Americans that may affect attitudes toward biospecimen donation. Lam and McCullough (13) describe how willingness to donate an organ was influenced by beliefs that associate an intact body with respect for ancestors or nature, yet willingness was modified by social distance to the potential recipient. Tison and colleagues (14) describe that traditional Chinese beliefs about blood draws affecting the life energy “qi” can affect donation preferences.
Our specific objective in developing an educational seminar about biospecimen collection was that it would enhance understanding and potential participation with the community. To evaluate the effectiveness of message content about biospecimen collection, participants were randomized to either an intervention group (biospecimen seminar) or an attention control group (general cancer education seminar). The selection of the control topic on general cancer education reflects education currently available to the general public.
Materials and Methods
Study setting
The study was conducted at the Chinatown Public Health Center (CPHC) in San Francisco, California. CPHC is a clinic within San Francisco’s Chinatown and a trusted community resource for over 40 years, serving a predominantly Cantonese-speaking clientele of almost 6,000. The CPHC health education team, led by Lei-Chun Fung, was a key partner in all aspects of this study, including design, recruitment, conduct, data collection, and analysis. All study activities were conducted in Cantonese.
Theoretical framework and content development for seminar
The theoretical framework for this study is the Health Behavior Framework (HBF; refs. 15, 16), which has been used extensively because of its applicability to less acculturated Asian American groups and its robustness to accommodate the variety of factors measured, including the individual’s cognitive and cultural influences on behavioral intention. The HBF is based on the premise that we can only influence multifaceted behaviors by using a multidimensional model derived from varying theoretical orientations. The HBF assumes that individual variables (knowledge, communication with provider, health beliefs, social norms and support, past health behaviors, barriers and supports, and cultural factors and beliefs) and provider and health care system factors (provider characteristics, health care setting, practice patterns, and structural factors) influence behavioral intentions, which then influence health behavior.
The content of the biospecimen educational materials and questionnaires was designed using the HBF framework to address: cognitive, cultural and contextual concerns, collection/storage of specimens, and research use of specimens. Content for the seminar included information from the National Cancer Institute’s Office of Bio-repositories and Biospecimen Research (3), and was refined after focus group input about usefulness and comprehension of material. The presentation was developed and translated for a sixth grade literacy level, reflective of many Chinese immigrants (17). The final seminar consisted of the following elements: (i) “background of cancer research”: how cancer is the leading cause of death in Asian Americans (18), research on cancer needs to compare different populations, including more Asian Americans, and different tissue samples (e.g., hair, saliva, blood, and urine) can be used for molecular analysis to improve understanding and action on cancer; (ii) “issues about community participation”: reasons or concerns for participation, where concerns were addressed with explanations (e.g., difficulty of individual feedback was addressed with example of a biospecimen blood drive that offered a phone number to get personal results); and (iii) “examples of community participation”: whether a person was sick or healthy with four scenarios: “healthy person in a research study,” “healthy person at a blood drive for research,” “healthy person at a bone marrow drive,” and “sick person donating at a hospital.”
The control seminar consisted of an existing “Cancer 101” seminar. The seminar topics included: what is cancer, common cancers by ethnic group, risk factors for common cancers, early warning signs of common cancers, cancer screenings (breast, cervical, prostate, colorectal), and general cancer risk reduction. The seminars on the two topics were conducted by two Cantonese-speaking female physicians, who were trained on the content by the CPHC team.
Focus groups and development of seminar and questionnaire materials
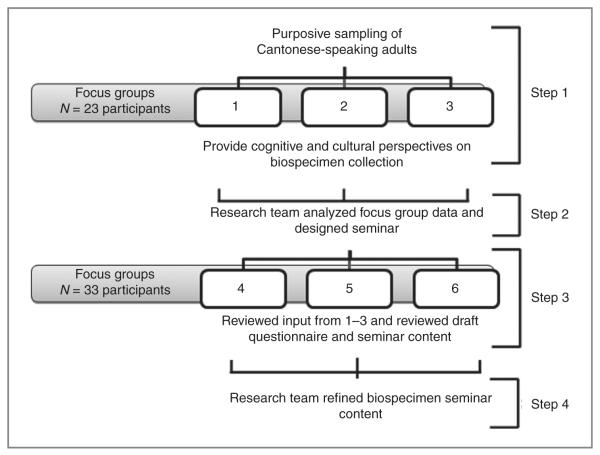
Figure 1 shows a diagram of the formative evaluation process. An experienced bilingual moderator from the CPHC conducted focus groups in Cantonese. Purposive sampling of Cantonese-speaking adults based on age (< or > 50 years old) and cancer status was done for an initial set of three focus groups (n = 23) to obtain cognitive and cultural perspectives related to biospecimen collection. The interview guide’s domains included terminology, cultural beliefs that promote or inhibit specimen donation, relationships with recipient/those requesting biospecimens, motivations for/benefits of donating, risks related to specimen use or personal information, and assessment of current educational materials. A draft questionnaire and biospecimen educational seminar was developed incorporating the focus group input. A second phase of three additional groups (n = 33) reviewed these draft materials, and revisions were subsequently made based on their feedback. Participants received a $30 gift card for participation in the focus groups.
Figure 1.
Diagram of formative evaluation process.
Younger participants and cancer survivors were more likely to say they might consider biospecimen donation than older participants, so we included age and cancer history in our questionnaires. Health clinics and well-known research institutions were considered the most trust-worthy sources for biospecimen collection and requests for donation; thus, our final biospecimen seminar case-based scenarios featured community settings or university studies. No Chinese terminology seemed appropriate for “biospecimens” but participants understood the term if specific types of tissues were described.
Participants reviewing the draft seminar found utility in understanding the process of informed consent. Blood donation was indeed what many participants first thought of about biospecimen donation, and participants appreciated learning that different types of tissues could be donated. Some participants noted that if research on the specimen revealed a “serious” health problem, individual donors should be alerted to the problem; thus, we modified a case scenario to have some health information given back to the participants. We inserted a case scenario involving bone marrow donation, an event familiar to Asian Americans, after participants made an analogy with biospecimen collection. Participants felt that the use of “qi” could be deemphasized given the variety of biospecimen types and wanted information about how quickly blood could be replenished, so potential donors would not be worried. Participants also felt that materials could emphasize healthy people as well as patients.
Recruitment for randomized trial
More than 700 Chinese Americans from the general community contacted CPHC about the study from a bilingual flyer distributed at CPHC health education outreach events. The flyer for the randomized trial stated that participants must be willing to be randomized to an educational seminar about cancer, whether “cancer research in the community” or “cancer screening and prevention.” Participants received a $25 gift card for participation in the randomized trial. Figure 2 illustrates the CONSORT flow diagram of the randomized trial in which we screened 511 Chinese American adults, randomized 400, and 395 were available for analysis. These participants were randomized to eight seminars (each lasting 1 hour) to compare the effects of the intervention seminar (biospecimen education) with a control seminar. A brief questionnaire was administered before and after the seminars.
Figure 2.
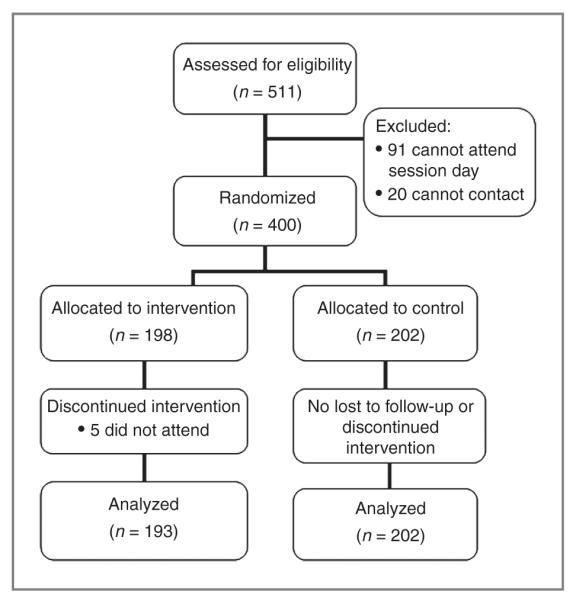
Randomized controlled trial of willingness to donate biospecimens among Chinese Americans.
Study approval and consent
The research protocol was approved by the University of California Davis Institutional Research Board (Sacramento, CA). Informed consent was obtained for each study participant.
Power calculation
A power calculation for the difference between study arms in pre-post change in willingness to donate a biospecimen was based on a Singapore study (mainly Chinese participants) examining willingness to donate blood for genetic research (19). In the study, 69.4% of participants who had heard of a genetic test (similar to our educational intervention on biospecimens) were willing to donate compared with 44.4% of participants who had not heard of a genetic test. Besides the effect size of 25%, we also included estimates of the proportion of participants who change from “willing” to “not willing,” as well as the increase in the proportion of control participants who are “willing.” Assuming that 5% of participants (in both study arms) change from “willing” at pretest to “unwilling” at post, a seminar size of 50, and an intraclass correlation coefficient of 0.04, a sample size of 178 in each study arm provided 80% power to detect the difference between a net change of 0% in the control group and 25% in the intervention group, at the 0.05 level, two-sided level. The targeted sample size of 400 allowed for an 11% attrition/no-show rate.
Measures
The first challenge we encountered in the focus groups was terminology. No Chinese word exists for the English term “biospecimens.” Thus, we chose to use specific examples of “biospecimens” as the following: saliva, blood (two vials specified because volume might be a concern), urine, hair, toenails, or other body part tissue (e.g., kidney).
Demographics included age, gender, marital status, and educational status. Acculturation measures included years lived in the United States and English proficiency (very well, well, so-so, not too well, not at all). Medical history included family and personal history of cancer.
The primary outcomes were change in willingness to donate biospecimens for two scenarios: whether a participant was healthy or hypothetically had cancer. The biospecimens included the five tissue types listed above, as well as any unused tissue already being collected.
Secondary outcomes examined reasons to donate or concerns about donation, some of which reflect culturally specific issues, either brought up in the focus groups or as described from a previous study (19). The four reasons to donate were: future generations will benefit, a person I know would benefit, I could be notified about abnormal results, and samples would already be collected as part of my medical care. The six concerns about donation were: losing my privacy, being asked to donate more specimens later, not knowing how my donation will be used, not getting medical information about my donation, upsetting the balance of “qi” in my body, and not maintaining the entire body (given by parents and ancestors). Participants were also asked about different requestors or beneficiaries for donation that would affect donation willingness.
Statistical analysis
First, we compared the study arms with respect to demographic characteristics using χ2tests. Then we assessed the difference between the study arms in the primary outcome, change from pre- to postseminar in the proportion of participants willing to donate a biospecimen, using generalized estimating equations (GEE) to account for clustering of participants attending the same seminar and within-person correlation over time; a bias-corrected sandwich estimator was used due to the small number of clusters. The study arms were similarly compared with respect to changes in reasons for and concerns about donation, and requestors or beneficiaries of donation affecting willingness to donate. Logistic regression GEE models were used to further assess the intervention effect and to determine associations of willingness to donate a biospecimen at pre- and post-seminar with the following sociodemographic factors: age, gender, marital status, education, years in the United States, family history of cancer, and personal history of cancer; the attitude that future generations will benefit was added in a separate model. Regression models were also conducted for reasons or concerns about donating. All analyses used SAS 9.3 statistical software.
Results
Demographics
Table 1 shows that the intervention and control groups differed only with the intervention group having a somewhat greater proportion of females. Otherwise, participants were mostly female, married, and younger than 65 years. Less than half had less than a high school education, over half reported speaking English “not too well” or “not at all,” and less than half reported living in the United States for 10 years or less. Few reported ever smoking cigarettes. Less than a third reported having a family history of cancer, whereas an eighth reported a personal history of cancer.
Table 1.
Demographics of Chinese American participants in a randomized controlled trial
| ntervention % (n = 193) |
Control % (n = 202) |
Total % (n = 395) |
P | |
|---|---|---|---|---|
| Age >65 y | 34 | 31 | 33 | 0.36 |
| Female | 86 | 77 | 81 | 0.02 |
| Married/partner | 80 | 82 | 81 | 0.63 |
| Education | ||||
| <High school | 48 | 43 | 45 | 0.25 |
| HS graduate | 43 | 42 | 43 | — |
| Some college/graduate | 9 | 15 | 12 | — |
| English fluency | ||||
| Very/pretty well | 5 | 8 | 7 | 0.27 |
| So-so | 41 | 37 | 39 | — |
| Not too well/not at all | 54 | 55 | 55 | — |
| Years lived in the United States | ||||
| ≤10 y | 46 | 45 | 45 | 0.25 |
| >10 y | 54 | 55 | 55 | — |
| Ever smoke cigarettes | 8 | 6 | 7 | 0.84 |
| Family history of cancer | 31 | 28 | 29 | 0.55 |
| Personal history of cancer | 11 | 14 | 12 | 0.37 |
NOTE: Bold P values reflect a statistical significance of P < 0.05.
Baseline willingness and attitudes
At baseline, Table 2 shows that many in both groups would be willing to donate a biospecimen (saliva, urine, hair, toenails, or blood), whether they were healthy or had cancer. At the extremes, almost three quarters were willing to donate saliva and about half or less were willing to donate blood. Most participants at baseline also stated that if they had cancer, they would be willing to donate unused tissue.
Table 2.
Change in willingness to donate and reasons or concerns about donation among Chinese American participants in a randomized controlled trial
| Intervention % (n = 193) |
Control % (n = 202) |
Delta delta: intervention versus control (n = 395) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Delta | P | Pre | Post | Delta | P | P | ||
| If healthy, would donate: | ||||||||||
| Saliva | 73 | 85 | 12 | <0.001 | 74 | 81 | 6 | 0.008 | 5 | 0.05 |
| Urine | 62 | 77 | 15 | <0.001 | 68 | 73 | 5 | 0.12 | 10 | 0.03 |
| Blood (2 vials) | 40 | 49 | 9 | 0.07 | 39 | 42 | 2 | 0.18 | 6 | 0.22 |
| Toenails | 43 | 56 | 13 | <0.001 | 49 | 44 | −4 | 0.10 | 18 | <0.001 |
| Hair | 55 | 67 | 12 | <0.001 | 58 | 58 | 0 | 0.88 | 13 | <0.001 |
| If have cancer, would donate: | ||||||||||
| Saliva | 71 | 85 | 15 | <0.001 | 73 | 81 | 8 | 0.005 | 7 | 0.03 |
| Urine | 63 | 79 | 17 | <0.001 | 72 | 73 | 1 | 0.64 | 16 | <0.001 |
| Blood (2 vials) | 51 | 54 | 3 | 0.45 | 51 | 50 | −1 | 0.71 | 4 | 0.40 |
| Toenails | 44 | 59 | 15 | <0.001 | 53 | 49 | −5 | <0.001 | 20 | <0.001 |
| Hair | 52 | 72 | 20 | <0.001 | 64 | 61 | −3 | 0.04 | 23 | <0.001 |
| If have cancer, donate unused tissue |
76 | 86 | 10 | <0.001 | 82 | 82 | 0 | 0.77 | 10 | <0.001 |
| Reasons for willingness to donate | ||||||||||
| Future generations will benefit |
74 | 88 | 15 | <0.001 | 77 | 81 | 4 | 0.10 | 10 | 0.002 |
| A person I know would benefit |
48 | 56 | 8 | 0.001 | 42 | 47 | 5 | 0.29 | 3 | 0.62 |
| I could be notified about abnormal results |
26 | 27 | 1 | 0.74 | 34 | 25 | −9 | 0.001 | 10 | 0.01 |
| Samples would already be collected as part of my medical care |
18 | 22 | 4 | 0.30 | 23 | 20 | −3 | 0.61 | 8 | 0.33 |
| Concerns about donating for cancer research | ||||||||||
| Losing my privacy | 35 | 34 | −1 | 0.91 | 34 | 39 | 4 | 0.06 | −5 | 0.36 |
|
Being asked to donate more later |
25 | 25 | 0 | 1 | 25 | 23 | −2 | 0.62 | 2 | 0.77 |
| Not knowing how my donation will be used |
25 | 21 | −4 | 0.58 | 33 | 31 | −2 | 0.69 | −2 | 0.84 |
| Not getting medical information about my donation |
16 | 11 | −5 | 0.02 | 18 | 17 | 0 | 0.90 | −4 | 0.35 |
| Upsetting the balance of “qi” in my body |
10 | 12 | 2 | 0.59 | 9 | 8 | −1 | 0.75 | 3 | 0.53 |
| Not maintaining the entire body, which our parents and ancestors gave to us |
7 | 6 | −1 | 0.77 | 12 | 11 | 0 | 0.80 | 0 | 0.99 |
NOTE: Bold P values reflect a statistical significance of P < 0.05.
The majority of participants would donate because future generations will benefit. Less than half stated they would donate because a person they know would benefit. Less compelling reasons were being notified about abnormal results (<1/3), and donating if samples were already collected as part of their medical care (~1/5).
The majority of participants did not have significant concerns about donating for cancer research. “Losing my privacy,” “not knowing how my donation will be used,” and “being asked to donate more later” ranged only from a quarter to over a third of participants. Even less were concerned about “not getting medical information about the donation,” “upsetting the balance of “qi” in the body,” and “not maintaining the entire body.”
Participants were most likely to report (not shown) that they would consider donating if asked by their family (69%), followed by their doctor (60%), their friend (38%), a government health agency (33%), a Chinese community group (31%), and a university study (27%); only 10% would not consider donating blood or tissue. Participants were also most likely to consider donating if they thought that an immediate family member would benefit (85%), followed by a close relative (49%), a friend (39%), a distant relative (33%), a Chinese person (30%), and a stranger (22%).
Comparing intervention and control proportions before and after the seminar
Comparing before and after the educational seminar (Table 2), there was an intervention effect for saliva, urine, toenails, and hair, whether healthy or having cancer (except for saliva if healthy). The intervention group did increase their willingness to donate blood if they were healthy, but this was only a trend (P = 0.07) and did not differ from the change in the control group.
There was an intervention effect for two reasons to donate: future generations will benefit and being notified of abnormal results. However, the latter was due to a significant decrease in the control group proportion. There was no intervention effect for concerns about donation, or for different requestors or beneficiaries for donation affecting willingness.
Intervention effect for willingness to donate and attitudes
After adjusting for demographic and personal history factors, Table 3 shows that the intervention effect remained statistically significant for roughly doubling the willingness to donate for the following biospecimens: urine if they had cancer, toenails if they were healthy or had cancer, hair if healthy or had cancer, and unused cancerous tissue. With the adjusted analyses, there was now only a trend for willingness to donate saliva (healthy or if cancer) or urine if healthy. Again, willingness to donate blood did not have an intervention effect after adjustment.
Table 3.
Multiple logistic regression comparing change for willingness to donate and reasons or concerns about donation among Chinese American participants in a randomized controlled trial
| Factor | Intervention pre-post (n = 193) OR (95% CI) |
Control pre-post (n = 202) OR (95% CI) |
Intervention pre-post versus control pre-post (n = 395) OR (95% CI) |
P |
|---|---|---|---|---|
| If healthy, willing to donate | ||||
| Saliva | 2.2 (1.9–2.5) | 1.5 (1.1–2.2) | 1.4 (1.0–2.1) | 0.07 |
| Urine | 2.1 (1.6–2.8) | 1.3 (1.0–1.9) | 1.6 (1.0–2.4) | 0.05 |
| Blood | 1.5 (1.0–2.3) | 1.2 (0.9–1.4) | 1.3 (0.8–2.1) | 0.30 |
| Toenails | 1.8 (1.3–2.5) | 0.8 (0.7–1.1) | 2.1 (1.4–3.2) | <0.001 |
| Hair | 1.7 (1.4–2.1) | 1.0 (0.7–1.3) | 1.8 (1.3–2.5) | <0.001 |
| If have cancer, willing to donate | ||||
| Saliva | 2.5 (2.0–3.3) | 1.7 (1.2–2.4) | 1.5 (1.0–2.3) | 0.06 |
| Urine | 2.4 (1.5–3.9) | 1.1 (0.9–1.3) | 2.2 (1.3–3.7) | 0.002 |
| Blood | 1.1 (0.8–1.6) | 1.0 (0.7–1.3) | 1.2 (0.7–1.8) | 0.49 |
| Toenails | 1.9 (1.7–2.2) | 0.8 (0.8–0.9) | 2.3 (2.0–2.7) | <0.001 |
| Hair | 2.5 (1.8–3.4) | 0.9 (0.8–1.1) | 2.8 (1.9–4.0) | <0.001 |
| If have cancer, willing to donate unused tissue | 2.0 (1.4–2.8) | 1.1 (0.8–1.5) | 1.8 (1.2–2.9) | 0.01 |
| Reasons for willingness to donate | ||||
| Future generations will benefit | 2.8 (2.3–3.6) | 1.4 (1.0–1.9) | 2.0 (1.4–3.0) | <0.001 |
| A person I know would benefit | 1.4 (1.2–1.8) | 1.3 (0.8–2.0) | 1.1 (0.7–1.9) | 0.60 |
| I could be notified about abnormal results | 1.1 (0.8–1.4) | 0.6 (0.5–0.8) | 1.7 (1.2–2.3) | 0.003 |
| Samples would already be collected as part of my medical care |
1.2 (0.7–2.2) | 0.8 (0.3–1.9) | 1.5 (0.6–4.3) | 0.40 |
| Concerns about donating for cancer research | ||||
| Losing my privacy | 1.0 (0.7–1.5) | 1.3 (1.0–1.6) | 0.8 (0.5–1.3) | 0.35 |
| Being asked to donate more later | 1.0 (0.5–2.1) | 0.9 (0.5–1.5) | 1.1 (0.4–2.8) | 0.81 |
| Not knowing how my donation will be used | 0.8 (0.4–1.9) | 0.9 (0.6–1.5) | 0.9 (0.4–2.4) | 0.86 |
| Not getting medical information about my donation | 0.7 (0.5–1.1) | 1.0 (0.6–1.9) | 0.7 (0.3–1.5) | 0.34 |
| Upsetting the balance of “qi” in my body | 1.3 (0.6–2.6) | 0.9 (0.4–1.8) | 1.4 (0.5–3.9) | 0.50 |
| Not maintaining the entire body, which our parents and ancestors gave to us |
0.9 (0.5–1.7) | 0.9 (0.6–1.4) | 1.0 (0.5–2.0) | 0.92 |
NOTE: Adjusted for age, sex, marital status, education, years in the United States, family history of cancer, and personal history of cancer.
Bold P values reflect a statistical significance of P < 0.05.
The intervention effect remained statistically significant for the attitudes that future generations would benefit and being notified about abnormal results (Table 3). As before, the latter result was due to a decrease in the control group, rather than an increase in the intervention group. Again, there was no intervention effect for the concerns about donating.
Other factors were significantly associated with the outcome of willingness to donate (not shown). People who were less educated were less likely to be willing to donate saliva, urine, blood, toenails, and hair. People with a family history of cancer were more likely to be willing to donate blood, toenails, or hair, and to consider donating because future generations would benefit, and less likely to be concerned about upsetting the balance of qi. Older people (>65) were more likely to be willing to donate saliva and urine and less likely to be willing to donate blood; they were less likely to be concerned about losing privacy or not knowing how their donation would be used, and more likely to be concerned about upsetting the balance of qi and not maintaining the entire body.
“Future generations will benefit” associated with willingness to donate
After adjusting for demographic, personal history factors, and trial group, Table 4 shows that the attitude that “future generations will benefit” is a strong independent predictor (nearly 3–4 times the odds) of willingness to donate all biospecimens, whether a participant was healthy or had cancer. This effect was seen even with blood (which did not have an intervention effect). Adding this attitude variable produced little attenuation of the intervention effects, with only one no longer being statistically significant [unused cancer tissue: OR 1.6; 95% confidence interval (CI), 0.9–2.6).
Table 4.
Multiple logistic regression of association between “future generations will benefit” attitude with willingness to donate biospecimens
| OR (95% CI) | P | |
|---|---|---|
| If healthy, willing to donate | ||
| Saliva | 3.54 (2.21–5.67) | <0.001 |
| Urine | 3.19 (2.01–5.07) | <0.001 |
| Blood | 2.98 (1.75–5.09) | <0.001 |
| Toenails | 2.85 (1.64–4.96) | <0.001 |
| Hair | 3.60 (2.20–5.88) | <0.001 |
| If have cancer, willing to donate | ||
| Saliva | 3.70 (1.95–7.03) | <0.001 |
| Urine | 3.63 (2.36–5.60) | <0.001 |
| Blood | 2.92 (1.69–5.02) | <0.001 |
| Toenails | 3.10 (2.01–4.78) | <0.001 |
| Hair | 3.47 (1.74–6.92) | <0.001 |
| If have cancer, willing to donate unused tissue |
4.18 (2.18–8.01) | <0.001 |
NOTE: Adjusted for age, sex, marital status, education, years in the United States, family history of cancer, personal history of cancer, and trial group.
Bold P values reflect a statistical significance of P < 0.05.
Discussion
To the best of our knowledge, our study is the first randomized, controlled trial focused on developing and evaluating the impact of an educational seminar on biospecimen collection, compared with an attention control seminar, among Cantonese-speaking Chinese Americans in a community setting. Our findings indicate that Cantonese-speaking Chinese Americans are highly receptive to education and participation in biospecimen collection, and behavioral intent may be enhanced with a culturally-tailored educational seminar. These findings are particularly interesting because our study population had a low acculturation and socioeconomic background. Many of our participants were women, but they are still at risk for cancer due to second-hand smoke exposure, as Cantonese-speaking men have high rates of smoking.
Our results demonstrate that there is an existing high degree of willingness to donate biospecimens among Cantonese-speaking Chinese Americans, whether healthy or with cancer. However, the type of biospecimen matters with the least invasive (saliva, urine) being more favorable than those that might involve embarrassment (toenails, hair) or are most invasive (blood). Still, even with blood it was surprising that at baseline the lowest percentage willing to donate was 40% if healthy and even higher at 50% if with cancer. This high degree of willingness might be attributed to the fact that community physicians and a trusted community clinic was delivering both the intervention and control messages. Our findings are consistent with others who have also determined that an educational plan should meet specific community needs, and that credentialed scientists and trusted institutions enhance the likelihood of acceptance (20). Future studies might investigate the difference if another entity outside of the community delivered the message.
Our biospecimen educational seminar made an impact on increasing willingness to donate for almost all biospecimens, whether a participant was healthy or had cancer, except for blood. Saliva and urine, only demonstrated a trend in the logistic regression analyses, but at baseline, the willingness to donate was already quite high. It is not clear about the reluctance to donate blood, especially because the concerns about donating were not significant. One possibility is that we did not ask about relevant concerns such as invasiveness, pain, inconvenience, or embarrassment with collection. We will investigate this qualitatively with participants about what might be changed for future biospecimen educational seminars.
The most compelling reason to donate for Chinese Americans was that future generations would benefit. Our study demonstrated an intervention effect in the regression analyses, and this attitude was strongly associated with willingness to donate biospecimens. This might be used as a key theme for future biospecimen educational seminars, and is culturally resonant with Chinese Americans who are considered more collectivist than individualist (21, 22). Although being notified about abnormal results was significant in the regression analyses between the groups, this change was mostly due to a negative change in the control group; further investigation is warranted. Interestingly, although the biospecimen educational seminar did focus on addressing concerns about donating, there was no intervention effect. This may be due to a low baseline prevalence of concerns about donating, and this might also be attributed to the trust with the message delivered by community physicians and the trusted community clinic. Older participants were more likely to report concerns of traditional perspectives (qi balance, not maintaining entire body), but they represented only a third of the sample.
Further attention, especially outside of the community-based setting, might tie in informed consent more closely with health education. Our focus groups told us that learning about informed consent was useful, and the highest ranking concern from our trial was loss of privacy. Studies of other racial/ethnic groups report that addressing confidentiality and consent issues enhances the likelihood of biospecimen contributions (23). Three studies also underscore the importance of informed consent and community education: (i) Beskow and Dean (24) interviewed 40 participants who were diverse in race/ethnicity, education, age, and sex. They learned that understanding of an informed consent template led to a majority of potential donors being comfortable with various biorepository policies (e.g., indefinite biospecimen storage, providing medical record access, not receiving individual results), but lack of trust in researchers was associated with declining certain consent options. More effort is needed in understanding and tailoring information to the needs of different subgroups before the time of informed consent. (ii) Wong and colleagues (19) conducted a survey of Singaporeans (mostly Chinese), in which willingness to donate blood for genetic research depended on whether or not the participant had heard of genetic testing (69.4% “yes” vs. 44.4% “no”). In a multivariate analysis, willingness to donate was also significantly associated with belief in the benefits of genetic research, intention to participate in government studies, having no fear of pain, blood, injections, and needles, and nonconcern about the loss of confidentiality. Because only half the population had heard of genetic tests, the authors called for greater public education and dialogue with community members. (iii) Fong and colleagues (25) conducted a survey in which Native Hawaiians were more likely than non-Hawaiians to require informed consent for genetic research, not just for personally identified specimens, but those that were ethnically identified or even anonymous. The authors concluded that community preferences must be determined to alleviate concerns about harms inherent in genetic research.
Limitations
Limitations include potential contamination effects among participants in a close social network who might share seminar content within the 2-month period that the seminars were being conducted. Given the limited budget and community-based nature of this study, we were not able to conduct the control group seminars in a separate community such as in Los Angeles. However, given that individual assessment occurred immediately postseminar, we believe the potential contamination effects were minimal. There may be reasons and concerns for donating that we did not identify in our study, and participants may not be cognizant without having experienced donation before. Also, we recognize that intention does not automatically translate into behavior. Nevertheless, considering the very positive feedback, we are confident that had we offered opportunities to donate biospecimens for cancer research after the educational seminar for the intervention group, the response rate would be quite positive.
Conclusions
Cantonese-speaking Chinese American participants of an educational seminar on biospecimen collection showed significantly greater increases in willingness to donate biospecimens than participants who attended a control seminar. The theme of benefiting “future generations” resonated strongly with willingness to donate. This conclusion is buttressed by our randomized, controlled trial design with an attention control group.
Acknowledgments
The authors thank Drs. Zhi Huang and Mei-Wen Wu for presenting the seminar material to the Chinese community, Dr. Angela Sun for sharing the cancer education presentation used in the control arm, the CPHC’s Health Education Team (Carrie Tang, Dan Ping Li, Joanna Lin, Maria Seeto, and Lily Fang) for assistance with conducting the seminar, and the support of Medical Director Dr. Albert Yu and Associate Medical Director Dr. Yee-Bun Lui.
Grant Support This work was financially supported by the National Cancer Institute (grant U54 CA153499).
Footnotes
Disclosure of Potential Conflicts of Interest No potential conflicts of interest were disclosed.
Authors’ Contributions Conception and design: E.K. Tong, S.L. Stewart, D.A. Paterniti, J.H.T. Dang, M.S. Chen
Development of methodology: E.K. Tong, L.-C. Fung, S.L. Stewart, D.A. Paterniti, J.H.T. Dang, M.S. Chen
Acquisition of data (provided animals, acquired and managed patients, provided facilities, etc.): L.-C. Fung
Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): E.K. Tong, L.-C. Fung, S.L. Stewart, D.A. Paterniti, M.S. Chen
Writing, review, and/or revision of the manuscript: E.K. Tong, S.L. Stewart, D.A. Paterniti, J.H.T. Dang, M.S. Chen
Administrative, technical, or material support (i.e., reporting or organizing data, constructing databases): E.K. Tong, J.H.T. Dang Study supervision: M.S. Chen
References
- 1.Hewitt RE. Biobanking: the foundation of personalized medicine. Current Opinion in Oncology. 2010;23:112–9. doi: 10.1097/CCO.0b013e32834161b8. [DOI] [PubMed] [Google Scholar]
- 2.Moore HM, Compton CC, Lim MD, Vaught J, Christiansen KN, Alper J. Biospecimen research network symposium: advancing cancer research through biospecimen science. Cancer Res. 2009;69:6770–2. doi: 10.1158/0008-5472.CAN-09-1795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.National Cancer Institute’s Office of Biorepositories and Biospecimen Research [accessed 2009 Dec 1];About OBBR: Overview. Available from: http://biospecimens.cancer.gov/about/overview.asp.
- 4.Scott EA, Schlumpf KS, Matthew SM, Mast AE, Busch MP, Gottschall JL. Biospecimen reporitories: are blood donors willing to participate? Transfusion. 2010;50:1943–50. doi: 10.1111/j.1537-2995.2010.02667.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pulley JM, Brace MM, Bernard GR, Masys DR. Attitudes and perceptions of patients towards methods of establishing a DNA biobank. Cell Tissue Bank. 2008;9:55–65. doi: 10.1007/s10561-007-9051-2. [DOI] [PubMed] [Google Scholar]
- 6.Kettis-Lindblad A, Ring L, Viberth E, Hansson MG. Genetic research and donation of tissue samples to biobanks. What do potential sample donors in the Swedish general public think? Eur J Public Health. 2006;16:433–40. doi: 10.1093/eurpub/cki198. [DOI] [PubMed] [Google Scholar]
- 7.Schwartz MD, Rothenberg K, Joseph L, Benkendorf J, Lerman C. Consent to the use of stored DNA for genetics research: a survey of attitudes in the Jewish population. Am J Med Genet. 2001;98:336–42. doi: 10.1002/1096-8628(20010201)98:4<336::aid-ajmg1100>3.0.co;2-7. [DOI] [PubMed] [Google Scholar]
- 8.James RD, Yu JH, Henrikson NB, Bowen DJ, Fullerton SM. Strategies and stakeholders: minority recruitment in cancer genetics research. Community Genetics. 2008;11:241–9. doi: 10.1159/000116878. [DOI] [PubMed] [Google Scholar]
- 9.Robinson JM, Trochim WMK. An examination of community members’, researchers’ and health professionals’ perceptions of barriers to minority participation in medical research: an application of concept mapping. Ethn Health. 2007;12:521–39. doi: 10.1080/13557850701616987. [DOI] [PubMed] [Google Scholar]
- 10.U.S. Census Bureau The Asian population. 2010 Available from: www.census.gov/prod/cen2010/briefs/c2010br-11.pdf.
- 11.Lai HM. Becoming Chinese American: A History of Communities and Institutions. Alta Mira Press; Walnut Creek, CA: 2004. [Google Scholar]
- 12.Carr K, Beers M, Kassebaum T, Chen MS. California Chinese American Tobacco Use Survey– 2004. California Department of Health Services; Sacramento, CA: 2005. [Google Scholar]
- 13.Lam WA, McCullough LB. Influence of religious and spiritual values on the willingness of Chinese-Americans to donate organs for transplantation. Clin Transplant. 2000;14:449–56. doi: 10.1034/j.1399-0012.2000.140502.x. [DOI] [PubMed] [Google Scholar]
- 14.Tison GH, Liu C, Ren F, Nelson K, Shan H. Influences of general and traditional Chinese beliefs on the decision to donate blood among employer-organized and volunteer donors in Beijing, China. Transfusion. 2007;47:1871–9. doi: 10.1111/j.1537-2995.2007.01410.x. [DOI] [PubMed] [Google Scholar]
- 15.Bastani R, Glenn BA, Taylor VM, Chen MS, Jr, Nguyen TT, Stewart SL, et al. Integrating theory into community interventions to reduce liver cancer disparities: the health behavior framework. Prev Med. 2010;50:63–7. doi: 10.1016/j.ypmed.2009.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maxwell AE, Bastani R, Chen MS, Jr, Nguyen TT, Stewart SL, Taylor VM. Constructing a theoretically based set of measures for liver cancer control research studies. Prev Med. 2010;50:68–73. doi: 10.1016/j.ypmed.2009.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.NICOS Chinese Health Coalition . Chinese Community Health Summit Final Report. San Francisco: 2004. [Google Scholar]
- 18.Chen MS., Jr. Cancer health disparities among Asian Americans: what we know and what we need to do. Cancer. 2005;104:2937–9. doi: 10.1002/cncr.21501. [DOI] [PubMed] [Google Scholar]
- 19.Wong ML, Chia KS, Yam WM, Teodoro GR, Lau KW. Willingness to donate blood samples for genetic research: a survey from a community in Singapore. Clin Genet. 2004;65:45–51. doi: 10.1111/j..2004.00192.x. [DOI] [PubMed] [Google Scholar]
- 20.Erwin DO, Moysich K, Kivinemi MT, Saad-Harfouche FG, Davis W, Clark-Hargrave N, et al. Community-based partnership to identify keys to biospecimen research participation. J Cancer Educ. 2013;28:43–51. doi: 10.1007/s13187-012-0421-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee L, Zane NE. Handbook of Asian American Psychology. Sage Publications; Thousand Oaks, CA: 1998. [Google Scholar]
- 22.McLaughlin L, Braun K. Asian and pacific islander cultural values: considerations for health care decision making. Health Soc Work. 1998;23:116–26. doi: 10.1093/hsw/23.2.116. [DOI] [PubMed] [Google Scholar]
- 23.Luque JS, Quinn GP, Montel-Ishino FA, Arevalo M, Bynum SA, Noel-Thomas S, et al. Tampa Bay Community Cancer Network Partners. Formative research on perceptions of biobanking: what community members think. J Cancer Edu. 2012;27:91–9. doi: 10.1007/s13187-011-0275-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Beskow LM, Dean E. Informed consent for biorepositories: assessing prospective participants’ understanding and opinions. Cancer Epidemiol Biomarkers Prev. 2008;17:1440–51. doi: 10.1158/1055-9965.EPI-08-0086. [DOI] [PubMed] [Google Scholar]
- 25.Fong M, Braun KL, Chang RM. Native Hawaiian preferences for informed consent and disclosure of results from genetic research. J Cancer Educ Spring. 2006;21:S47–52. doi: 10.1207/s15430154jce2101s_10. [DOI] [PubMed] [Google Scholar]