Abstract
Summary
Though the etiology of multiple sclerosis remains unknown, the widely accepted explanation is that it has an autoimmune inflammatory background. In 2006 Paolo Zamboni renewed the somewhat forgotten vascular theory of the pathogenesis of multiple sclerosis, proposing the new entity of ‘chronic cerebrospinal venous insufficiency’.
As a result of this hypothesis, Zamboni suggested an endovascular treatment for multiple sclerosis involving venoplasty of the internal jugular vein and the azygos vein. Unfortunately, several teams have tried to replicate Zamboni’s results without success. In this review, we present a chronological description of the results of the studies conducted by Zamboni and the later attempts to replicate his work. The main conclusion is that, taking into account results that are currently available, we should remain cautious and routine use of this treatment in patients should not be advisable.
Keywords: Venoplasty, CCSVI, Multiple Sclerosis
The Theory of Chronic Cerebrospinal Venous Insufficiency in the Context of Pathogenesis of Multiple Sclerosis
Multiple sclerosis (MS) is a disease of unexplained etiology, with autoimmune background currently accepted as the most probable explanation [1].
In 2006, Italian vascular surgeon, Paolo Zamboni, proposed a hypothesis based on the analogy between perivascular histopathological lesions in venous insufficiency of lower limbs and cerebral venous pathologies in multiple sclerosis patients. The syndrome of lesions was named chronic cerebrospinal venous insufficiency (CCSVI). The disorder is associated with hindered outflow of blood from the brain as an effect of venous abnormalities, such as stenosis, or impaired venous valve function which may lead to local reversal of blood flow in cerebral and/or cervical veins. These disorders lead to the breakage of the brain/blood barrier, extravascular deposition iron and development of local inflammation and demyelinative lesions that are the cause of MS [2]. Cerebral blood outflow disorders may be confirmed by both non-invasive methods such as Doppler ultrasonography (USG) and magnetic resonance (MR) venography, as well as by direct invasive phlebography.
In 2009, at the Congress of the International Union of Phlebology, CCSVI has been categorized into the group of venous malformations [3].
The relationship between changes within the cerebral venous system and MS is not a new concept: as early as in 1863, German pathologist Georg Eduard von Rindfleisch reported the presence of occluded veins with thickened walls in the center of demyelinative lesions [4], while in approximately the same period, Jean-Martin Charcot defined MS as a primary inflammatory demyelinative disorder due to glial pathology with secondary vascular lesions [5].
In the 1930s, based on his animal studies, Tracy Jackson Putnam proposed a hypothesis that the occlusion of small veins may lead to the development of local inflammation within the brain and thus stimulate formation of demyelinating plaque [6].
In 1965, Danish neurologist Torben Fog provided a description of veins referred to as central or parent veins, which were the centers for the spread of demyelinative lesions [7]. Finally, in 1986, an Austrian researcher Franz Alfons Schelling has published the hypothesis of venous reflux as a possible factor involved in the pathogenesis of MS [8].
The first report by Zamboni, its title starting with words “The big idea”, was presented at the meeting of the Royal Medical Society in London on 1 July 2006. In this report, Zamboni demonstrated an analogy between venous insufficiency in lower limbs and potential disturbances of cerebral blood outflow, later referred to as chronic cerebrospinal venous insufficiency.
Zamboni’s theory provides for a number of obstacles that hinder the drainage of blood from the brain, mainly via internal jugular veins, vertebral veins and the azygos vein system. These disturbances reportedly lead to blood reflux within deep cerebral veins, with erythrocytes being transferred into the perivascular space leading to an increase in perivascular deposits of iron. As a result, adhesion molecules and leukocyte activation takes place, together with the development of local inflammation and fibrin sheath around the veins. These local inflammatory lesions reportedly lead to myelination disorders [9].
In their later studies, Zamboni et al. proposed ultrasonographic criteria of chronic cerebrospinal venous insufficiency in a transcranial examination as well as in the examination of extracranial segments of internal jugular veins and vertebral veins. CCSVI was diagnosed when at least two of five criteria listed were met [2,10] (Table 1).
Table 1.
Ultrasound criteria of the chronic cerebrospinal venous insufficiency (CCSVI).
| Chronic cerebrospinal venous insufficiency (CCSVI) criteria according to Zamboni [9]. |
|---|
| 1. Reflux constantly present in an outflow pathway (IJV and/or VV) with the head in any position. |
| 2. Reflux propagated upward to the DCVs. |
| 3. High resolution B-mode ultrasonography evidence of proximal IJV stenoses. |
| 4. Flow not CD detectable in the IJVs and/or VVs despite numerous deep inspirations. |
| 5. Negative ΔCSA in the IJV. |
IJV(s) – internal jugular vein(s); VV(s) – vertebral vein(s); DCVs – deep cerebral veins; CD – color Doppler; ΔCSA – change in the cross-sectional area.
Based on his hypothesis, Zamboni proposed a method for the treatment of CCSVI consisting in jugular and azygos vein angioplasty, nicknaming it a “liberation therapy” (Figures 1–3).
Figure 1.
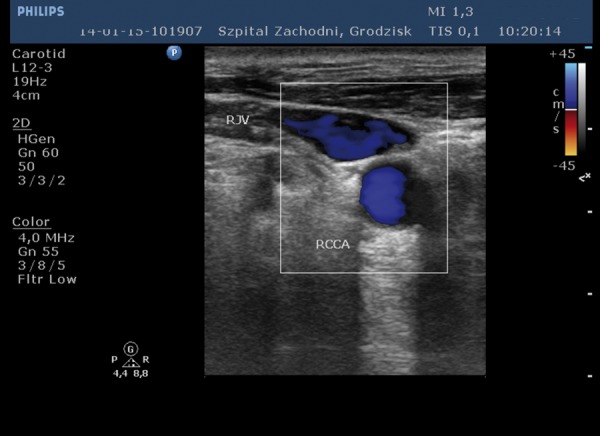
Internal jugular vein reflux.
Figure 3.
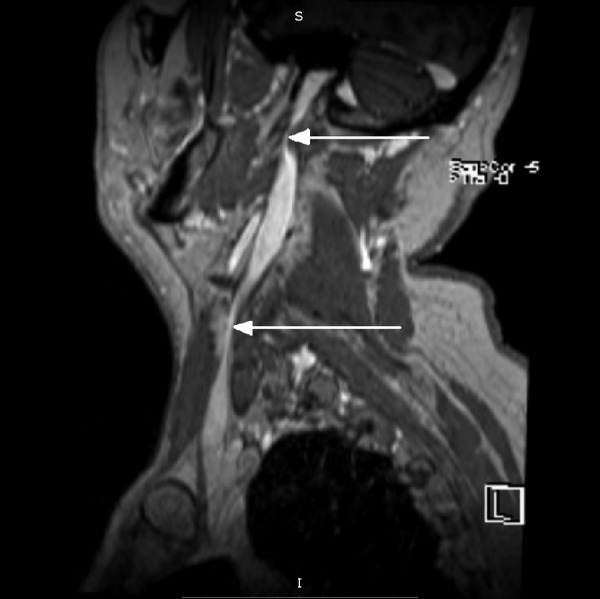
Segmental stenoses within the internal jugular veins.
Results of Studies Conducted to Date
The results of Zamboni’s studies suggested a strong correlation between chronic cerebrospinal insufficiency and MS. Lesions typical for CCSVI were observed in 100% of MS patients while no lesions were detected in individuals without MS (no coexistence of 2 criteria was detected in any subject in the control group) [2]. In later years, reports that partially confirmed Zamboni’s results were published, for example a study by R. Zivadinov et al. published in 2012, in which the criteria of venous insufficiency were met in 62.5% patients with MS and 25.5% of healthy volunteers [11].
However, contradictory results were obtained by the Bochum group of C. Krogias et al. in 2010. The researchers carried out US scans in MS patients to detect Zamboni’s criteria of chronic cerebrospinal venous insufficiency only in 20% of subjects [12].
Also in 2010, F. Doepp et al. at Berliner Charite published an article attempting to verify the results obtained by Zamboni. IN a group consisting of 56 MS patients and 20 control subjects, abnormal flow direction was detected only in one MS patient. Ten patients in the study group and 4 patients in the control group met none of the criteria of venous insufficiency [13].
In the same year, a Swedish group of P. Sundström et al. conducted a study in a group of 21 MS patients and 20 healthy volunteers using phase contrast MR angiography. No significant differences were detected in jugular vein outflows in both groups, and no jugular vein reflux was detected. Internal jugular vein stenosis was observed in 3 study group patients [14].
In October 2010, two other reports were published: one from the dutch group of M. P. Wattjes et al. and the other from the Lebanese group of B. Yamout et al. The first group carried out phase contrast MR venography with contrast administration, as well as flow measurements within the cerebral veins and the straight sinus using a 3T MR apparatus in 20 MS patients and 20 healthy volunteers. The results of these studies were analyzed by interventional radiologists unaware of subject’s disorders and having no morphological images of brain at their disposal. Cerebral and extracranial veins were assessed for stenosis/occlusion and collateral circulation. Anatomical vein anomalies were observed in 10 out of 20 MS patients as well as in 8 out of 20 healthy subjects. Collateral circulation was observed in in 6 MS patients as well as in 5 healthy subjects. No vascular lesions were observed in 10 study group subjects. No venous reflux was detected in any of the subjects [15].
The second group of B. Yamout et al. assessed the presence of extracranial vein stenoses by means of selective venography in 42 MS patients, detecting stenoses in 12 out of 13 patients with long history of MS and in 7 out of 29 patients with early MS. Only 3 out of 42 patients (all with long history of MS) had stenosis in both jugular veins. In the face of these results, the authors arrived at a conclusion that extracranial vein stenosis was not a probable cause of MS, while secondary venous disorders in the natural history of cerebral atrophies are possible [16].
In 2011, the group of C. Baracchini conducted a study in 50 patients with probable clinical diagnosis of MS and 50 control subjects. The study population also consisted of 60 patients with transient global amnesia and a control group selected to match the sex and age profile of these patients. Trans- and extracranial Doppler ultrasound scans were performed in all patients. Selective venography was also performed in patients with probable clinical diagnosis of MS who met the CCSVI criteria. No changes were observed in transcranial examinations of either of the patients with probable clinical diagnosis of MS. One or more lesions in extracranial vein ultrasound scans were observed in 26 (52%) patients in the study group and 35 (31.8%) patients in the control groups as well as in 41 (68.3%) patients with transient global amnesia. Eight patients in the study group met Zamboni’s criteria. Selective venography was performed in 7 of these patients (one patient had not agreed to undergo the examination), yielding unremarkable results. [17].
In the same year Ch. A. Mayer with a group of other German researchers performed a trial in 20 MS patients and 20 healthy volunteers. Stenosis of internal jugular vein was observed in 13 MS patients and 16 control group subjects; reduced cross-sectional area of jugular vein upon changing the position for the supine position to the sitting position was observed in all patients and considered to be physiological. No jugular vein blood flow upon deep inspiration was observed in only 1 control group subject. No abnormalities of this type were observed in the group of MS patients. Only 2 subjects in the control group met at least 2 ultrasonographic criteria of chronic cerebrospinal venous insufficiency. The criteria were not met by any MS patient [18].
In 2012, the American group of A.D. Baretto published the results of a study conducted in a group of 276 patients (including 206 MS patients). Zamboni’s criteria were met by 13 patients, including 8 patients with MS and 5 patients with disorders other than MS [19].
In 2013, the Naples group of R. Lancillo et al. conducted a study in a group of 171 MS patients and 41 healthy volunteers. The criteria of venous insufficiency were met by 76% of MS patients and 16% of control group subjects. The authors concluded that venous insufficiency was more common in MS patients, although it seemed to be more correlated with their age and poorly correlated with the natural history of MS [20].
In another study published in 2013, another group of Italian researchers led by M.A. Leone observed similar numbers of patients meeting at least two of Zamboni’s criteria in the study group of 68 MS patients and the control group of 68 healthy volunteers (30.9% and 33.8%, respectively). [21]
In August 2013, a study was published by Canadian group of researchers who examined 100 MS patients and 100 control group volunteers. Only one patient in the study group (and none of the control group subjects) met two ultrasonographic criteria required for the diagnosis of CCSVI [22].
The published study results are listed in Table 2.
Table 2.
Prevalence of CCSVI in multiple sclerosis patients vs. controls – selected studies.
| Authors | MS patients | Non-MS patients | Positive CCSVI criteria in MS patients [%] | Positive CCSVI criteria in non-MS patients[%] |
|---|---|---|---|---|
| Zamboni P. et al. [32] | 65 | 235 | 100% | 0% |
| Al-Omari M.H. et al. [33] | 25 | 25 | 84% | 0% |
| Doepp F. et al. [13] | 56 | 20 | 0% | 0% |
| Baracchini C. et al. [17] | 50 | 50 | 16% | 2% |
| Mayer C.A. et al. [18] | 20 | 20 | 0% | 5% |
| Zivadinov R. et al.[11] | 289 | 163 | 56.1% | 22.7% |
| Floris R. et al. [34] | 40 | 34 | 55% | 35% |
| Patti F. et al. [35] | 148 | 172 | 18.9% | 6.4% |
| Lanzillo R. et al. [36] | 146 | 38 | 76% | 16% |
| Leone M.A. et al. [37] | 68 | 68 | 30.9% | 33.8% |
| Van den Berg P.J. et al. [38] | 90 | 41 | 9% | 0% |
| Chambers B. et al. [39] | 70 | 70 | 0% | 1.4% |
| Barreto A.D. et al. [19] | 200 | 76 | 3.88% | 7.14% |
| Imperiale D. et al. [40] | 80 | 41 | 17.5% | 7.3% |
| Rodger I.W. et al. [41] | 99 | 100 | 1% | 0% |
| Brod S.A. et al. [42] | 206 | 70 | 3.88% | 7.14% |
| Comi G. et al. [43] | 1165 | 376 | 3.26% | 2.13% |
| Traboulsee A.L. et al. [44] | 79 | 43 | 44% | 45% |
| Tromba L. et al. [45] | 112 | 67 | 59.8% | 0% |
Reservations Regarding the Diagnostic Criteria of CCSVI
The diagnostic criteria of CCSVI as proposed by Zamboni are also subject to criticism.
-
Reflux (t>0.88 s) within the internal jugular veins and/or vertebral veins in supine and sitting positions.
Comment: The reflux time proposed by Zamboni originates from another study of internal jugular venous valve insufficiency ant its elongation is a manifestation of valve insufficiency. Direct translation of this value onto vertebral veins is not justified.
-
Reflux (t>0.5 s) within deep cerebral veins in Color Doppler scans.
Comment: The methodology is controversial – assessment through the new supracondylar window with no previous studies defining reference norms for this type of images. No spectral Doppler used – the obtained color Doppler scans may be misinterpreted, and therefore diagnosing reflux on this basis only is unauthorized. The reflux time (0.5 s) is taken directly from studies of venous insufficiency in lower limbs where it is used to assess valvular insufficiency following tourniquet loosening.
-
Stenosis (cross-sectional area of <0.3 cm2) in proximal internal jugular vein area in high resolution B-mode scan.
Comment: the value is taken from examinations of intensive care unit patients without consideration to the possible impact of artificial ventilation and possibility of hypovolemia – a dubious reference for healthy patients. Difficult choice of the vessel assessment site as the vessel may have a meandering course and physiological dilatations in upper and lower segments. Possibility of error: the mere pressure exerted by the examination probe may cause local increase in tissue pressure and lead to false positive results.
-
Lack of flow features in Doppler ultrasound scan of the internal jugular vein and/or vertebral vein despite numerous deep inspirations with head fully extended (0°) and bent (90°).
Comment: no flow in internal jugular veins is not necessarily tantamount to occlusion. Sometimes, unilateral lack of blood flow may be observed in supine position in completely healthy subjects. In vertical position, significant reduction in blood flow, and even no flow is observed in healthy subjects. No flow in vertebral veins is also sometimes encountered in supine position in healthy subjects. The obtained results are also largely dependent on the apparatus settings – improper settings may lead to false positive results.
-
Reduced cross-sectional area of internal jugular vein when changing patient’s position from the supine to the sitting position.
Comment: Reduced cross-sectional area of internal jugular vein when changing patient’s position from the supine to the sitting position is a physiologically normal phenomenon. Similarly as in 3 – the mere pressure from the probe may lead to false positive results [23].
No unambiguous confirmation could also be provided for other elements of Zamboni’s theory, such as absence of anatomical narrowings or other obstacles for venous outflow, such as membranes, inverted valves or incomplete septa within internal jugular veins. In angiographic examinations consisting of classical phlebography, phase contrast MR venography and phase contrast as well as contrast-enhanced venography, the incidence of these lesions in MS patients was not significantly different from the control group [14–17,22].
Currently, there are serious doubts regarding the appropriateness of the CCSVI diagnostic criteria. Some studies making use of Zamboni’s criteria could not confirm his results.
Also the cerebrospinal fluid levels of iron compounds which, according to Zamboni’s theory, were to promote the development of MS by being deposited in the perivascular space were not significantly different between diagnosed MS patients and patients not suffering from MS [24].
Controversies Regarding CCSVI Treatment
The treatment method, referred to as liberation therapy, also remains controversial. It consists of angioplasty of internal jugular veins and, less commonly, azygos veins, as well as implantation of stents within internal jugular veins at some sites. Following first reports on the efficacy of this method, particularly with respect to the relapsing-remitting disease [25], other reports were published suggesting lack of positive effects of angioplasty procedures [26,27] and discrepancies between treatment results as measured by the assessment of clinical status (Expanded Disability Status Scale, EDSS) and the extent of MRI lesions and the results of subjective quality of life assessment (MSQoL) [28]. Single reports of complications related to angioplasty procedures [29] and stent implantation [30] were also published. In 2011, CIRSE published a comment in which the routine use of this method is not recommended [31].
Conclusions
Although the relationship between the disturbances in cerebral venous outflow and certain neurological disorders (not only MS) remains an open issue that requires further studies, direct relationship with chronic cerebrospinal venous insufficiency diagnosed using Zamboni’s criteria remains controversial, as is the treatment method he also proposed. Due to medial publicity, numerous sites started to employ the “liberation therapy”, sometimes under pressure from patients and MS patient associations. However, in light of studies published to date and of the positions of scientific societies, widespread use of this method should be postponed until more convincing evidence is available regarding its efficacy.
Figure 2.
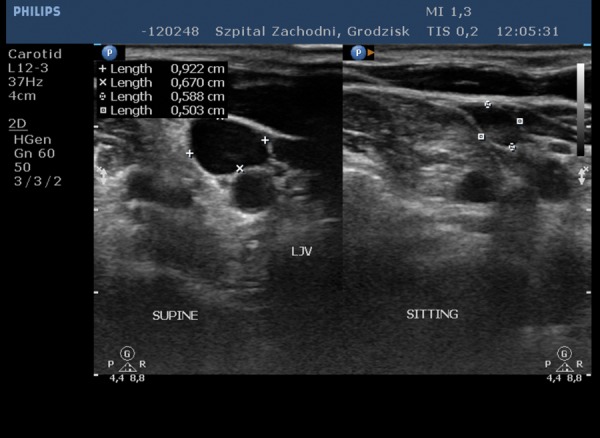
Reduced cross-sectional area of internal jugular vein when changing subject’s position from the supine to the sitting position.
References
- 1.Frohman EM, Racke MK, Raine CS. Multiple sclerosis – the plaque and its pathogenesis. N Engl J Med. 2006;354:942–55. doi: 10.1056/NEJMra052130. [DOI] [PubMed] [Google Scholar]
- 2.Zamboni P, Menegatti E, Galeotti R, et al. The value of cerebral Doppler venous haemodynamics in the assessment of multiple sclerosis. J Neurol Sci. 2009;282(1–2):21–27. doi: 10.1016/j.jns.2008.11.027. [DOI] [PubMed] [Google Scholar]
- 3.Medicover Hospital What is CCSVI? [accessed 10.01.2014]. http://www.medicover.com/hospital/298,What-is-CCSVI.htm.
- 4.Lassmann H. Multiple sclerosis pathology: evolution of pathogenetic concepts. Brain Pathology. 2005;15(3):217–22. doi: 10.1111/j.1750-3639.2005.tb00523.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Compston A, McAlpine D. McAlpine’s multiple sclerosis. 4th ed. Philadelphia: Churchill-Livingstone Elsevier; 2006. pp. 24–37. [Google Scholar]
- 6.Putnam TJ. Studies in multiple sclerosis: ‘encephalitis’ and sclerotic plaques produced by venular obstruction. Arch Neurol Psychiatry. 1935;33:929–40. [Google Scholar]
- 7.Fog T. The topography of plaques in multiple sclerosis with special reference to cerebral plaques. Acta Neurol Scand Suppl. 1965;15:1–161. [PubMed] [Google Scholar]
- 8.Schelling F. Damaging venous reflux into the skull or spine: relevance to multiple sclerosis. Med Hypotheses. 1986;21:141–48. doi: 10.1016/0306-9877(86)90003-4. [DOI] [PubMed] [Google Scholar]
- 9.Zamboni P. The big idea: iron-dependent inflammation in venous disease and proposed parallels in multiple sclerosis. J R Soc Med. 2006;99:589–93. doi: 10.1258/jrsm.99.11.589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zamboni P, Menegatti E, Bartolomei I, et al. Intracranial venous haemodynamics in multiple sclerosis. Curr Neurovasc Res. 2007;4:252–58. doi: 10.2174/156720207782446298. [DOI] [PubMed] [Google Scholar]
- 11.Zivadinov R, Marr K, Cutter G, et al. Prevalence, sensitivity, and specificity of chronic cerebrospinal venous insufficiency in MS. Eur J Vasc Endovasc Surg. 2012;43(1):116–22. doi: 10.1212/WNL.0b013e318212a901. [DOI] [PubMed] [Google Scholar]
- 12.Krogias C, Schröder A, Wiendi H, et al. ‘Chronic cerebrospinal venous insufficiency’ and multiple sclerosis: critical analysis and first observation in an unselected cohort of MS patients. Nervenarzt. 2010;81:740–46. doi: 10.1007/s00115-010-2972-1. [DOI] [PubMed] [Google Scholar]
- 13.Doepp F, Paul F, Valdueza JM, et al. Cerebrocervical venous congestion in patients with multiple sclerosis. Ann Neurol. 2010;68:173–83. doi: 10.1002/ana.22085. [DOI] [PubMed] [Google Scholar]
- 14.Sundström P, Wahlin A, Ambarki K, et al. Venous and cerebrospinal fluid flow in multiple sclerosis: a case-control study. Ann Neurol. 2010;68:255–59. doi: 10.1002/ana.22132. [DOI] [PubMed] [Google Scholar]
- 15.Wattjes MP, Van Oosten BW, De Graaf WL, et al. No association of abnormal cranial venous drainage with multiple sclerosis: a magnetic resonance venography and flow-quantification study. J Neurol Neurosurg Psychiatry. 2011;82:429–35. doi: 10.1136/jnnp.2010.223479. [DOI] [PubMed] [Google Scholar]
- 16.Yamout B, Herlopian A, Issa Z, et al. Extracranial venous stenosis is an unlikely cause of multiple sclerosis. Mult Scler. 2010;16:1341–48. doi: 10.1177/1352458510385268. [DOI] [PubMed] [Google Scholar]
- 17.Baracchini C, Perini P, Calabrese M, et al. No evidence of chronic cerebrospinal venous insufficiency at multiple sclerosis onset. Ann Neurol. 2011;69(1):90–99. doi: 10.1002/ana.22228. [DOI] [PubMed] [Google Scholar]
- 18.Mayer CA, Pfeilschifter W, Lorenz MW, et al. The perfect crime? CCSVI not leaving a trace in MS. J Neurol Neurosurg Psychiatry. 2011;82(4):436–40. doi: 10.1136/jnnp.2010.231613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barreto AD, Brod SA, Bui TT, et al. Chronic cerebrospinal venous insufficiency: case-control neurosonography results. Ann Neurol. 2013;73(6):721–28. doi: 10.1002/ana.23839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lanzillo R, Mancini M, Liuzzi R, et al. Chronic cerebrospinal venous insufficiency in multiple sclerosis: a highly prevalent age-dependent phenomenon. BMC Neurol. 2013;13:20. doi: 10.1186/1471-2377-13-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Leone MA, Raymkulova O, Naldi P, et al. Chronic cerebrospinal venous insufficiency is not associated with multiple sclerosis and its severity: a blind-verified study. PLoS One. 2013;8(2):e56031. doi: 10.1371/journal.pone.0056031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rodger IW, Dilar D, Dwyer J, et al. Evidence against the involvement of chronic cerebrospinal venous abnormalities in multiple sclerosis. A case-control study. PLoS One. 2013;8(8):e72495. doi: 10.1371/journal.pone.0072495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Baracchini C, Valdueza JM, Del Sette M, et al. CCSVI and MS: a statement from the European Society of neurosonology and cerebral hemodynamics. J Neurol. 2012;259:2585–89. doi: 10.1007/s00415-012-6541-3. [DOI] [PubMed] [Google Scholar]
- 24.Worthington V, Killestein J, Eikelenboom MJ, et al. Normal CSF ferritin levels in MS suggest against etiologic role of chronic venous insufficiency. Neurology. 2010;75:1617–22. doi: 10.1212/WNL.0b013e3181fb449e. [DOI] [PubMed] [Google Scholar]
- 25.Salvi F, Bartolomei I, Buccellato E, et al. Venous angioplasty in multiple sclerosis: neurological outcome at two years in a cohort of relapsing-remitting patients. Funct Neurol. 2012;27(1):55–59. [PMC free article] [PubMed] [Google Scholar]
- 26.Alroughani R, Lamdhade S, Thussu A, et al. Endovascular treatment of chronic cerebrospinal venous insufficiency in multiple sclerosis: a retrospective study. Int J Neurosci. 2013;123(5):324–28. doi: 10.3109/00207454.2012.759569. [DOI] [PubMed] [Google Scholar]
- 27.Ghezzi A, Annovazzi P, Cocco E, et al. Endovascular treatment of CCSVI in patients with multiple sclerosis: clinical outcome of 462 cases. Neurol Sci. 2013;34(9):1633–37. doi: 10.1007/s10072-013-1300-5. [DOI] [PubMed] [Google Scholar]
- 28.Zagaglia S, Balestrini S, Perticaroli E, et al. Percutaneous transluminal angioplasty for chronic cerebrospinal venous insufficiency in multiple sclerosis: dichotomy between subjective and objective outcome scores. Neurol Sci. 2013;34(12):2205–10. doi: 10.1007/s10072-013-1450-5. [DOI] [PubMed] [Google Scholar]
- 29.Thapar A, Lane TR, Pandey V, et al. Internal jugular thrombosis post venoplasty for chronic cerebrospinal venous insufficiency. Phlebology. 2011;26(6):254–56. doi: 10.1258/phleb.2011.011052. [DOI] [PubMed] [Google Scholar]
- 30.Dolezal O, Horakova D, Gdovinova Z, et al. Serious complication of percutaneous angioplasty with stent implantation in so called “chronic cerebrospinal venous insufficiency” in multiple sclerosis patient. Prague Med Rep. 2012;113(4):289–93. doi: 10.14712/23362936.2015.12. [DOI] [PubMed] [Google Scholar]
- 31.Reekers JA, Lee MJ, Belli AM, et al. Cardiovascular and interventional radiological society of Europe commentary on the treatment of chronic cerebrospinal venous insufficiency. Cardiovasc Intervent Radiol. 2011;34(1):1–2. doi: 10.1007/s00270-010-0050-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zamboni P, Galeotti R, Menegatti E, et al. Chronic cerebrospinal venous insufficiency in patients with multiple sclerosis. J. Neurol. Neurosurg. Psychiatr. 2009;80(4):392–99. doi: 10.1136/jnnp.2008.157164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Al-Omari MH, Rousan LA. Internal jugular vein morphology and hemodynamics in patients with multiple sclerosis. Int Angiol. 2010;29:115–20. [PubMed] [Google Scholar]
- 34.Floris R, Centonze D, Fabiano S, et al. Prevalence study of chronic cerebrospinal venous insufficiency in patients with multiple sclerosis: preliminary data. Radiol Med. 2012;117(5):855–64. doi: 10.1007/s11547-011-0767-5. [DOI] [PubMed] [Google Scholar]
- 35.Patti F, Nicoletti A, Leone C, et al. Multiple sclerosis and CCSVI: a population-based case control study. PLoS One. 2012;7(8):e41227. doi: 10.1371/journal.pone.0041227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lanzillo R, Mancini M, Liuzzi R, et al. Chronic cerebrospinal venous insufficiency in multiple sclerosis: a highly prevalent age-dependent phenomenon. BMC Neurol. 2013;13:20. doi: 10.1186/1471-2377-13-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Leone MA, Raymkulova O, Naldi P, et al. Chronic cerebrospinal venous insufficiency is not associated with multiple sclerosis and its severity: a blind-verified study. PLoS One. 2013;8(2):e56031. doi: 10.1371/journal.pone.0056031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Van den Berg PJ, Van den Berg GB, Westerhuis LW, et al. Occurrence of CCSVI in patients with MS and its relationship with iron metabolism and varicose veins. Eur J Neurol. 2013;20(3):519–26. doi: 10.1111/ene.12010. [DOI] [PubMed] [Google Scholar]
- 39.Chambers B, Chambers J, Cameron H, et al. Chronic cerebrospinal venous insufficiency is not more prevalent in patients with mild multiple sclerosis: a sonographer-blinded, case-control ultrasound study. Mult Scler. 2013;19(6):749–56. doi: 10.1177/1352458512459986. [DOI] [PubMed] [Google Scholar]
- 40.Imperiale D, Melis F, Giaccone C, et al. Chronic cerebrospinal venous insufficiency in multiple sclerosis: a sonographer-blinded case-control study. Clin Neurol Neurosurg. 2013;115(8):1394–98. doi: 10.1016/j.clineuro.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 41.Rodger IW, Dilar D, Dwyer J, et al. Evidence against the involvement of chronic cerebrospinal venous abnormalities in multiple sclerosis. A case-control study. PLoS One. 2013;8(8):e72495. doi: 10.1371/journal.pone.0072495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brod SA, Kramer LA, Cohen AM, et al. Chronic cerebrospinal venous insufficiency: masked multimodal imaging assessment. Mult Scler. 2013;19(11):1499–507. doi: 10.1177/1352458513494493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Comi G, Battaglia MA, Bertolotto A, et al. Observational case-control study of the prevalence of chronic cerebrospinal venous insufficiency in multiple sclerosis: results from the CoSMo study. Mult Scler. 2013;19(11):1508–17. doi: 10.1177/1352458513501231. [DOI] [PubMed] [Google Scholar]
- 44.Traboulsee AL, Knox KB, Machan L, et al. Prevalence of extracranial venous narrowing on catheter venography in people with multiple sclerosis, their siblings, and unrelated healthy controls: a blinded, case-control study. Lancet. 2013;383(9912):138–45. doi: 10.1016/S0140-6736(13)61747-X. [DOI] [PubMed] [Google Scholar]
- 45.Tromba L, Blasi S, Vestri A, et al. Prevalence of chronic cerebrospinal venous insufficiency in multiple sclerosis: a blinded sonographic evaluation. Phlebology. 2013 doi: 10.1177/0268355513512823. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]


