Introduction
Adolescents engage in risky behaviors that can become habitual patterns for adulthood. Physicians are asked to address these behaviors confidentially to ensure the adolescents’ willingness to openly and honestly discuss these sensitive health topics.1 Although legal issues can make assuring confidentiality challenging for primary care providers to negotiate,2 a crucial first step is spending a portion of the visit without parents.3,4 Even though this policy has been promoted by the American Academy of Pediatrics and American Medical Association for 2 decades, only 40% of parents report that their adolescents had time alone with a clinician during their most recent preventive health visit.5 Interestingly, about two thirds of physicians self-report routinely spending time alone with their adolescent patients during annual visits.6 Given these discrepant reports, there is a need for more objective examinations of how often confidentiality is assured, how often adolescents are seen alone, and which physicians are more likely to do either of these. Respecting adolescent privacy and autonomy is a key component of patient-centered care. One marker of patient-centered care is motivational interviewing (MI). Therefore, we hypothesized that physicians who used MI techniques would be more likely to provide private and confidential care for their adolescent patients.
Methods
Data were obtained from baseline data from Teen CHAT, a randomized trial designed to enhance physician communication with overweight and obese adolescent patients.7 We identified primary care pediatrics and family medicine practices in 2 counties in North Carolina, which included rural, suburban, and urban settings. Forty pediatricians and 9 family practice physicians agreed to have their annual visit encounters with overweight adolescents audio recorded. Participants were recruited from all upcoming routine well-visit and chronic care appointments for patients 12 to 18 years old with a body mass index >85th percentile. These patients were sent introductory letters from the treating physician describing the study and included a phone number to call to opt out of participation. If the patient or parent did not decline participation, research staff called parents and adolescent to obtain verbal consent/assent and administer a baseline survey with the adolescent. Written consent/assent was then obtained from the parent and adolescent on the day of the encounter that was audio recorded. The recorded visits took place between December 2009 and September 2011.
Trained researchers coded all visits for (a) confidentiality assurance (ie, whether the physician provided an explicit assurance of confidentiality) and (b) whether the parent was asked to leave the examination room. We calculated total time of the visit and, thereof, total time when a parent was not present. Coders also rated MI techniques related to discussions about nutrition, weight, and physical activity using the Motivational Interviewing Treatment Integrity Code,8 which has previously been validated for convergent and discriminant validity.9 Any use of MI techniques was considered the use of “some MI.”
We calculated descriptive statistics by physician. We examined the association between confidentiality assurance (yes/no) and time spent alone (yes/no) using generalized estimating equations models to account for clustering within physicians fitting a logit link with a binomial distribution.10 For the subgroup of encounters where the physician spent time alone with the adolescent, we calculated the mean time spent alone and examined predictors of time spent alone using generalized estimating equations models assuming a normally distributed outcome. Differences between age-groups were calculated using the χ2.
Results
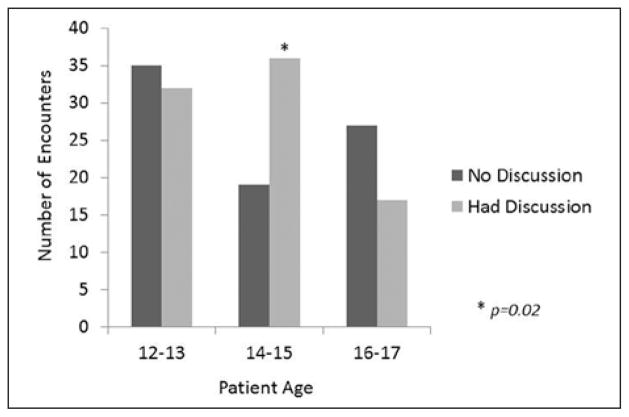
Demographics for patients and physicians are summarized in Table 1. The mean age of physicians was 41 years, and 65% were female. The mean age of patients was 14.2 years (SD = 1.63), 54% were female, 39% white, and 48% African American. Physicians spent an average of 21.8 minutes (SD = 9.1, range = 4.7–54.4 minutes) with adolescents; in half of these encounters (51%), they spent some time alone with the adolescent (mean time when they spent time any alone was 7.8 minutes, SD = 5.2, range = 0.6–27.5 minutes). Physicians provided an explicit statement of confidentiality in only 31% of encounters. Physicians used at least some MI techniques in 71% of encounters. In bivariate analysis, when physicians used MI techniques, they were also more likely to assure confidentiality (36% vs 19%, MI vs no MI, respectively, P = .03). When controlling for physician factors (gender, years since medical school, specialty) and patient factors (race, gender, maternal education level), physicians who provided confidentiality assurances were more likely to spend time alone with the adolescent (odds ratio = 8.1, 95% confidence interval = 3.3–19.7, P < .001), and pediatricians were more likely than family practitioners (odds ratio = 3.0, 95% confidence interval = 1.3–6.6, P = .008) to do so. Most (65%) physicians assured confidentiality with patients aged 14 to 15 years, more so than with younger adolescents aged 12 to 13 years (48%) or older adolescents aged 16 to 17 years (39%), P = .02 (see Figure 1).
Table 1.
Study Participant Characteristics.
| Number | Percentage | |
|---|---|---|
| Adolescents | ||
| Race | ||
| White | 65 | 39 |
| African American | 80 | 48 |
| Other | 20 | 12 |
| Missing | 1 | 1 |
| Gender | ||
| Female | 90 | 54 |
| Male | 76 | 46 |
| Maternal education | ||
| High school or less | 36 | 23 |
| Trade/some college | 30 | 19 |
| 4-year degree | 58 | 38 |
| Advanced degree | 30 | 19 |
| Physicians | ||
| Gender | ||
| Female | 32 | 65 |
| Male | 17 | 35 |
| Specialty | ||
| General pediatrics | 40 | 82 |
| Family medicine | 9 | 18 |
| Mean | Standard Deviation | Median | Minimum | Maximum | |
|---|---|---|---|---|---|
| Physician agea in years | 41.0 | 8.5 | 40.0 | 29.6 | 62.6 |
| Years since medical school | 11.8 | 8.7 | 10.0 | 0.0 | 33.0 |
Seven physicians did not provide age. All answered “years since medical school.”
Figure 1.
Number of adolescents receiving assurances of confidentiality by age.
Discussion
It has been almost 20 years since the American Medical Association published the Guidelines for Adolescent Preventive Services (GAPS) that recommended that, starting at age 11 or 12, a portion of routine well-visit should be conducted with the adolescent alone, with explicit assurances of confidentiality provided.3 Unfortunately, our study found that physicians often do not provide these 2 basic, yet crucial, components of adolescent preventive services.
The use of MI techniques was associated with greater odds of providing assurances of confidentiality, leading us to posit that supporting adolescent autonomy and confidentiality might be related skills. One critical element of MI is acceptance and “meeting patients where they are.” It is difficult for physicians to meet adolescents where they are if they are reluctant to be forthcoming with physicians. Acceptance also involves supporting patient autonomy and realizing that patients, not physicians, are the principal agents of change. Again, it is difficult for physicians to support adolescent autonomy when parents are present. This finding may indicate that enhanced training in MI may improve physician provision of adolescent confidential care.
Not surprisingly, those who provided explicit assurances of confidentiality were more likely to spend time alone with their adolescent patients than those who did not provide such assurances. If physicians incorporate a standard script for assuring confidentiality they likely will remember to speak with adolescents alone.
Pediatricians were more likely to provide confidentiality assurances than family physicians. Family physicians may provide care for the entire family, that is, not only for their adolescent patients but also for those adolescents’ parents. Family physicians may be less comfortable asking the parents, who are also their patients, to leave the room, or they may be so focused on the family as a cohesive unit and good communication within the family that they have not routinely integrated the need for adolescent independence into their daily practice. Other reasons may be that pediatricians see far more adolescents than family physicians and likely have more established and consistent routine well-visit paradigms and routines they follow, or may feel more comfortable addressing confidential topics with adolescents.
Age of the patient also played a role in confidentiality assurances, with both younger and older teenagers being less likely to receive such assurances than 14- and 15-year-olds. It may be that physicians were either less comfortable having such conversations with 12- and 13-year-olds, or perhaps they did not think that such conversations were necessary with these younger patients as they were not emotionally mature enough, despite the recommendations that these conversations begin at the 11- or 12-year visit. Older adolescents were also less likely than the 14- and 15-year-olds to receive confidentiality assurances. Physicians may think it is unnecessary to provide such assurances if they have done so at previous visits, but it is unclear whether adolescents will remember such assurances if they are not provided routinely. Furthermore, the older adolescents become, the more topics might be relevant and need assurances of confidentiality (eg, adolescent might have become sexually active at age 17 but when confidentiality was assured at 15, it was not relevant to adolescent).
A limitation of this study is the small number of family physicians enrolled, which may limit generalizability. Also, all adolescent patients recruited to the study were either overweight or obese, although it is unlikely that physicians would systematically treat their overweight differently regarding confidential and private health care. These limitations do not detract from the strengths of the study, particularly given that we did not depend on self-report of the physicians, patients, or parents.
Despite expert recommendations regarding the need for providing adolescents confidential care, this is often not a part of routine care. We are encouraged by the finding that the use of MI techniques with adolescents is associated with greater odds of providing elements of confidential care, and the provision of such care may be enhanced by educational programs that enhance the use of MI by physicians.
Acknowledgments
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the National Heart, Lung, and Blood Institute (R01HL092403).
Footnotes
Reprints and permissions: sagepub.com/journalsPermissions.nav
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- 1.Ford CA, Millstein S, Halpern-Felsher B, Irwin CE., Jr Inluence of confidentiality assurances on adolescents’ willingness to disclose information and seek future health care. A radomized controlled trial. JAMA. 1997;278:1029–1034. [PubMed] [Google Scholar]
- 2.Berlan ED, Bravender T. Confidentiality, consent, and caring for the adolescent patient. Curr Opin Pediatr. 2009;21:450–456. doi: 10.1097/MOP.0b013e32832ce009. [DOI] [PubMed] [Google Scholar]
- 3.American Medical Association Department of Adolescent Health. . Guidelines for Adolescent Preventive Services (GAPS) Chicago, IL: American Medical Association; 1993. [Google Scholar]
- 4.Hagan J, Shaw J, Duncan P. Bright Futures: Guidelines for Health Supervision of Infants, Children, and Adolescents. 3. Elk Grove Village, IL: American Academy of Pediatrics; 2008. [Google Scholar]
- 5.Edman JC, Adams SH, Park MJ, Irwin CE., Jr Who gets confidential care? Disparities in a national sample of adolescents. J Adolesc Health. 2010;46:393–395. doi: 10.1016/j.jadohealth.2009.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Bravender T, Price CN, English A. Primary care providers’ willingness to see unaccompanied adolescents. J Adolesc Health. 2004;34:30–36. doi: 10.1016/s1054-139x(03)00205-2. [DOI] [PubMed] [Google Scholar]
- 7.Bravender T, Tulsky JA, Farrell D, et al. Teen CHAT: development and utilization of a web-based intervention to improve physician communication with adolescents about healthy weight. Patient Educ Couns. doi: 10.1016/j.pec.2013.08.017. published online September 9, 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alexander SC, Cox ME, Boling Turer CL, et al. Do the five A’s work when physicians counsel about weight loss? Fam Med. 2011;43:179–184. [PMC free article] [PubMed] [Google Scholar]
- 9.Moyers TB, Martin T, Manuel JK, Hendrickson SM, Miller WR. Assessing competence in the use of motivational interviewing. J Subst Abuse Treat. 2005;28:19–26. doi: 10.1016/j.jsat.2004.11.001. [DOI] [PubMed] [Google Scholar]
- 10.Diggle P, Heagerty P, Liang K, Zeger S. Analysis of Longitudinal Data. New York, NY: Oxford University Press; 2002. [Google Scholar]