Abstract
Malignant pleural effusions (MPEs) are the second leading cause of exudative pleural effusions after parapneumonic effusions. In the vast majority of cases, a MPE signifies incurable disease associated with high morbidity and mortality. Considerable advances have been made for the diagnosis of MPEs, through the development of improved methods in the specialized cytological and imaging studies. The cytological or histological confirmation of malignant cells is currently important in establishing a diagnosis. Furthermore, despite major advancements in cancer treatment for the past two decades, management of MPE remains palliative. This article presents a comprehensive review of the medical approaches for diagnosis and management of MPE.
Keywords: Diagnosis; Pleural Effusion, Malignant; Disease Management
Introduction
Malignant pleural effusions (MPEs), which are diagnosed by the identification of malignant cells in pleural fluid or on pleural biopsy, represent an advanced malignancy disease associated with high morbidity and mortality, precluding the possibility of a curative treatment approach. Although almost all types of cancers can cause an MPE, more than 75% of MPEs are due to metastases originating from tumors in the lung, breast and ovary, as well as from lymphomas. Metastatic adenocarcinoma is the most frequent histological finding. However, the primary tumor is not identified in approximately 10% of patients with MPEs1,2,3.
Despite major advances in cancer treatment in the past two decades, the median survival time following a diagnosis of MPE depends on the origin of the primary tumor, histological type and stage, and usually ranges from 4 to 12 months. In particular, lung cancer patients with MPE have the shortest survival time1,2,4,5. For this reason, the recently revised staging system for non-small cell lung cancer (NSCLC) upstaged the presence of MPE from T4 to M1a6. A small amount of pleural effusion sometimes presents in cancer patients in whom cytological or histological diagnosis for the effusion using thoracentesis is not feasible. Our recent study demonstrated that the presence of only a small amount of pleural effusion could confer poor prognosis in NSCLC patients7. This article presents a comprehensive review of the medical approaches to the diagnosis and management of MPE and an attempt to derive a treatment algorithm for the management of MPE based on a review of the recent literature.
Diagnosis of MPEs
The most common symptom reported by patients with MPE is dyspnea, which occurs in more than 50% of patients, followed by cough, weight loss, and chest pain. However, an MPE can initially be found incidentally on imaging studies in an asymptomatic patient8.
Recently, the diagnostic accuracy of MPEs has been improved by the development of new chest imaging modalities3,9. However, confirmation of malignant cells in the pleural fluid or in the pleural biopsy is required to establish a diagnosis of MPE.
1. Pleural fluid analysis
Diagnostic thoracentesis is usually the first diagnostic step in determining pleural effusion characteristics. Analysis of pleural fluid using thoracentesis may help establish the origin of MPE. Pleural fluid samples are routinely analyzed for total and differential cell counts, proteins, lactate dehydrogenase (LDH), glucose, and pH, as well as subjected to microbiological and cytological examinations. MPEs are almost always categorized as exudates using the Light's criteria2, including LDH and protein values. However, very few MPEs with other systemic disorders can be categorized as transudates10,11. The general pleural fluid characteristics suggestive of the probability of MPE and differential diagnosis are summarized in Table 1.
Table 1.
The differential diagnosis and characteristics of pleural fluid suggestive of malignant pleural effusion (MPE)2,3
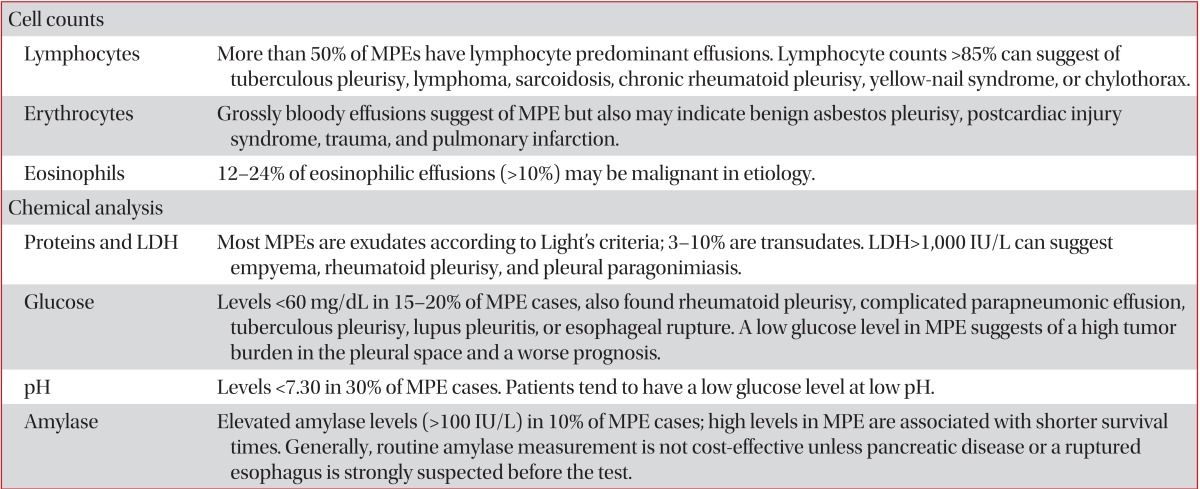
Adopted from Heffner and Klein3, with permission from Elsevier.
LDH, lactate dehydrogenase.
2. Tumor markers in pleural fluid
Many articles have suggested the possibility of diagnosing MPE when increased levels of tumor markers are found in the pleural fluid. To improve the diagnosis of MPE, a number of tumor markers have been evaluated intensively. However, the search for a highly accurate tumor marker in pleural fluid that reliably confirms MPE has been fruitless thus far12. Meta-analysis conducted for conventional tumor markers, such as carcinoembryonic antigen (CEA), carbohydrate antigens (CA) 15-3, CA 19-9, CA 125, and cytokeratin 19 fragments (CYFRA 21-1), reported pooled results on the diagnostic accuracy of each tumor marker in MPE (Table 2)12,13. These results illustrate several factors for consideration for tumor marker measurements in pleural fluid. First, measurement of pleural CEA is likely to be a useful diagnostic tool for confirming MPE and is useful for the differential diagnosis between malignant pleural mesothelioma and metastatic lung cancer. A high level of pleural CEA seems to rule out malignant mesothelioma. Second, CA 15-3, CA 19-9, and CYFRA 21-1 are highly specific but insufficiently sensitive to diagnose MPE, and the combination of two or more tumor markers appears to increase the diagnostic sensitivity. Therefore, the results of tumor marker assays should be interpreted in parallel with clinical findings and with the results of conventional tests12,13.
Table 2.
Pooled results of the diagnostic accuracies of each tumor marker in malignant pleural effusions based on meta-analysis12,13,15
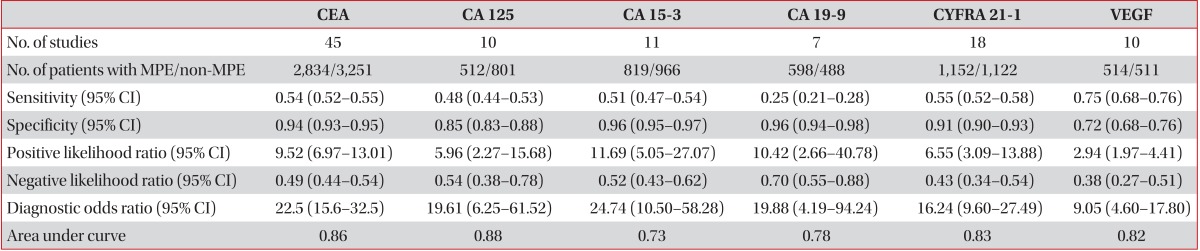
Adopted from Liang et al.12, with permission from BMJ Publishing Group Ltd.
CEA: carcinoembryonic antigen; CA: carbohydrate antigens; VEGF: vascular endothelial growth factor; MPE: malignant pleural effusion; CI: confidence interval.
Recently, there has been growing interest in vascular endothelial growth factor (VEGF) as a diagnostic biomarker of MPE because of the high levels of VEGF present in MPE14. VEGF is thought to be the key mediator in the formation of MPE via increased vascular permeability and vascular leakage of fluid. A recent meta-analysis based on 1,025 patients in 10 studies concluded that VEGF might play a role in the diagnosis of MPE, while its diagnostic value is not satisfactory (Table 2)15. Mesothelin and fibulin-3 in pleural effusion have also been introduced as potential new biomarkers to detect pleural mesothelioma at an earlier stage16,17.
However, the clinical applicability of measuring these tumor markers in pleural fluid is limited because, even at high concentrations, further confirmatory cytohistologic diagnosis is necessary18.
3. Cytology and biopsy
Pleural fluid cytology has traditionally been the analytical method of choice for the detection of tumor cells in pleural fluid. Many studies have shown a large variation in the diagnostic sensitivity of pleural fluid cytological analysis, ranging from 40-87%2. In particular, a cytomorphologic distinction between reactive mesothelial cells, mesothelioma, and metastatic adenocarcinoma, as well as between lymphomas and reactive lymphocytosis, can often be difficult because of significant overlapping cytologic features. Therefore, other procedures, such as immunohistochemistry (IHC) using monoclonal antibodies against tumor markers and chromosomal analysis, complement cytology in the diagnosis of MPEs. IHC staining can be performed on conventional cytology specimens and cell blocks. There have been many reports on the application of different IHC markers in pleural effusion samples to diagnosis MPE and to identify the primary site of origin. However, while there is no agreement on the ideal combination of IHC markers, a diagnostic sensitivity of ~80% is desirable for inclusion18,19.
When cytology is negative and MPE is still suspected, a pleural biopsy might be indicated. There are benefits of undertaking pleural biopsy, which allows for histological analysis of the samples and also characterization of specific hormonal or mutation statuses. In an early prospective intrapatient comparison, the diagnostic yield of nonsurgical biopsy methods in MPEs was studied simultaneously in 208 patients20. The diagnostic yield was 62% using pleural fluid cytology, 44% using closed pleural biopsy, and 95% using medical thoracoscopy. Medical thoracoscopy exhibited significantly higher diagnostic sensitivity than did cytology combined with closed needle biopsies from effusions, which were positive in 74% of cases. The combined methods were diagnostic in 97% of the MPEs20.
Recently, image-guided and thoracoscopic biopsy techniques have improved the diagnostic yield, as compared with traditional closed pleural biopsy using Abram's or Cope needles. In a randomized study of patients with cytologically negative suspected MPEs, a blind Abram's pleural biopsy had a sensitivity of 47% for correctly diagnosing malignancy, in contrast to 87% sensitivity for computed tomography (CT)-guided cutting needle pleural biopsy21. The diagnostic advantage of CT-guided biopsy may be <5-mm pleural thickening and fewer adverse events.
Another option for obtaining pleural biopsy samples is to perform a medical or surgical thoracoscopy, both of which allow for direct visualization of the pleura.
4. Novel diagnostic tool
Recent progress in molecular biology has provided a framework to develop novel diagnostic tools for MPEs. Molecular biology techniques, such as analyses of DNA copy number, gene sequence, mRNA and miRNA expression, and DNA methylation status and protein expression studies on malignant and normal cells within pleural effusions, have identified novel molecular diagnostic biomarkers that demonstrate potential for complementing cytology in the diagnosis of MPEs. Several challenges need to be addressed prior to the incorporation of these molecular tests into routine clinical diagnosis, including validation of molecular diagnostic markers in well-designed prospective and comparative studies with analysis of cost-effectiveness19.
Management of MPEs
The presence of an MPE generally indicates that the malignancy cannot be cured by surgery. Because the prognosis of patients with MPEs is so poor, treatment is focused on palliation of symptoms rather than a cure. Therefore, the management options for MPEs should consider several factors such as symptoms and performance status of the patient, the primary tumor type and its response to systemic therapy, and expected survival, as well as the social and financial status of the patient. Options for management include observation, repeated therapeutic thoracentesis, indwelling pleural catheter (IPC), chemical pleurodesis, and shunt22. The ideal management would offer immediate and long-term relief of symptoms and have minimal side effects. It would involve a procedure that requires the least amount of time spent in the hospital and clinic, avoids repeat uncomfortable procedures, and has the least cost1. Therefore, the British Thoracic Society (BTS) guidelines recommended that if the patient is asymptomatic and the tumor type is known to be responsive to systemic chemotherapy, observation is recommended23.
1. Therapeutic thoracentesis
Thoracentesis is typically the first step in the management of newly diagnosed MPE. Although symptoms can improve after thoracentesis, almost all patients with MPE experience reaccumulation of fluid and recurrence of symptoms within 30 days. If the patient remains symptomatic despite large-volume thoracentesis, causes such as lymphangitic spread, pulmonary embolism, or malignant airway obstruction should be suspected and investigated appropriately3,24. The complications related to thoracentesis include vasovagal reactions, cough, chest pain, hemothorax or pneumothorax, and reexpansion pulmonary edema. In addition, repeated thoracentesis (RT) often leads to fluid loculation, which can make further thoracentesis or subsequent pleurodesis difficult. Therefore, repeated therapeutic thoracentesis should be performed in patients with slowly reaccumulating pleural effusion, low life expectancy (1-3 months), cancers that commonly respond to therapy with resolution of the associated effusions, and who cannot tolerate other more interventional procedures to control pleural fluid, such as pleurodesis3,23. To prevent reexpansion pulmonary edema, the amount of fluid removed by thoracentesis should be assessed by patient symptoms (cough, chest discomfort) and limited to 1.5 L on a single occasion23.
2. Indwelling pleural catheter
IPC is also known as a tunneled or small gauge catheter. Insertion of an IPC is an alternative method for controlling recurrent and symptomatic MPEs, including trapped lung. Several catheters have been developed for this purpose, and published studies employing them have reported encouraging results23. Generally, the IPC system is composed of a silicone catheter, allowing ambulatory pleural drainage into plastic vacuum bottles, with fenestrations on the distal margin and a one-way valve on the proximal margin25. Placement is simple and is generally performed on an outpatient basis with local anesthesia.
A recent unblinded randomized control study comparing IPC and talc slurry pleurodesis via chest tube demonstrated that there was no significant difference in relieving patient-reported dyspnea between the two methods26. However, while the IPC-treated group spent reduced time in the hospital, it was associated with an excess number of adverse events. In light of the limited life span of patients with MPE, IPCs show promise in requiring fewer hospital days, improving dyspnea, and decreasing the need for additional procedures25,26.
Long-term IPCs may lead to spontaneous pleurodesis in 40-58% of patients with IPC2,3,23,25. Therefore, sclerosants can be instilled through the catheter if spontaneous pleurodesis does not occur after several weeks of drainage. In addition, IPC placement and maintenance are safe and free of complications in the vast majority of patients. Complications include infections, clogging of the catheter, or other rare events, such as empyema or tumor spread along the catheter track25.
3. Pleurodesis
Pleurodesis is defined as the process of mechanical or chemically induced pleural inflammation to obliterate the area between the visceral and parietal pleura and prevent the accumulation of either air or liquid in the pleural space. The pleural mesothelial cell is the primary target for the sclerosant and plays a pivotal role in the entire pleurodesis process. Many different sclerosing agents share similar mechanisms of inducing pleural mesothelial cell-mediated biological responses. These mechanisms include diffuse inflammation with pleural coagulation/fibrinolysis imbalance, recruitment and proliferation of fibroblasts leading to collagen production, and release of several mediators (such as interleukin 8, transforming growth factor β, and basic fibroblast growth factor) that contribute to the required fibrotic state1,2,27.
Numerous sclerosing agents have been studied in regard to management of MPEs, including talc, tetracycline/doxycycline/minocycline, Corynebacterium parvum extract, chemotherapeutic agents, such as bleomycin, cisplatin, doxorubicin, etoposide, and mitomycin, and biologic agents, such as interleukin-2 and interferon2,3,28,29,30. Recent studies suggest that silver nitrate31 and iodopovidone32 should be considered as reasonable alternative to other commonly used pleurodesis agents. Another study showed that Staphylococcus aureus superantigen, which is a powerful T-cell stimulant, might be an attractive alternative to existing palliative modalities for NSCLC patients with MPE who are not candidates for systemic chemotherapy33. However, the results of many studies have demonstrated diverse success rates with pleurodesis and no survival benefit. In addition, due to extensive practice variation and lack of adequately large comparative trials of different agents, the ideal agent choice remains controversial. To date, talc has the best rate of success with pleurodesis and is the preferred agent according to the BTS guidelines23, a recent review28, and Cochrance systematic review30.
The most common complications of chemical pleurodesis are fever and pain. Other rare complications include empyema and local site infection, arrhythmias, cardiac arrest, myocardial infarction, and hypotension. Acute respiratory distress syndrome (ARDS), acute pneumonitis, respiratory failure, and treatment-related mortality have also been reported after talc pleurodesis. ARDS occurs in up to 9% of talc pleurodesis cases1,2,3,23,30. In a recent multicenter, prospective study of 558 patients with MPE, none of the patients who received large-particle talc pleurodesis developed ARDS34. The development of ARDS is believed to be due to the small particle size of some talc preparations, which allows for systemic absorption and results in diffuse capillary leakage in the lung itself1. Therefore, experts now recommend the use of talc calibrated to a mean particle size of less than 20 µm with no particles less than 10 µm3.
Generally, pleurodesis should be restricted to patients who have respiratory symptoms caused by effusion, life expectancy longer than 2-3 months, MPE that is nonresponsive to systemic chemotherapy, and lung expansion to the chest wall after therapeutic thoracentesis2,3. A pleural agent can be instilled at the bedside via an intrapleural chest catheter (thoracostomy) or using thoracoscopic techniques, including video-assisted thoracoscopic surgery.
The BTS guidelines recommended the following pleurodesis procedure23: 1) small-bore (10-14 F) intercostal catheters should be the initial choice for effusion drainage and pleurodesis, 2) lidocaine (3 mg/kg; maximum 250 mg) should be administered intrapleurally immediately prior to sclerosant administration, 3) premedication should be considered to alleviate anxiety and pain associated with pleurodesis, 4) patient rotation is not necessary after intrapleural instillation of the sclerosant, 5) the intercostal tube should be clamped for 1 hour after sclerosant administration, and 6) in the absence of excessive fluid drainage (> 250 mL/ day), the intercostal tube should be removed within 24-48 hours of sclerosant administration.
4. Cost considerations
A relative cost-effectiveness analysis of MPE treatment modalities was recently reported, comparing RT, tunneled pleural catheter (TPC), bedside pleurodesis (BP), and thoracoscopic pleurodesis35. The results of the analysis showed that TPC is the preferred treatment for patients with MPE and limited survival. BP is the most cost-effective treatment for patients with more prolonged expected survival.
5. New therapeutic approach
Numerous new therapeutic modalities, such as intrapleural chemotherapy and gene therapy, and the use of a subcutaneous implantable pleural port have been investigated in comparison to the present standard treatment1.
Summary
MPEs usually present in disseminated and advanced stages of malignancy. Prompt diagnosis using a minimally invasive test is important, because the median survival after diagnosis is only 4-9 months. Considerable advances have been made in the diagnosis of MPEs through the development of improved methods for specialized cytologic and imaging studies. In the future, rapidly performed and minimally invasive diagnostic tests will enable clinicians to provide the most effective therapies for patients with MPEs in a timely fashion.
However, all management approaches remain palliative, and relief of dyspnea remains the primary objective. An algorithm based on various guidelines1,2,23,24 for the management of MPEs is shown in Figure 136. It is important to consider the patient's overall prognosis, symptoms, functional status, and social and financial situation when selecting the modality of choice. It is advisable to select the modality that is most cost-effective, least invasive, and most likely to lead to fewer hospitalization days.
Figure 1.
Algorithm for the management of malignant pleural effusion36. Adopted from Nam and Ryu36, with permission from The Korean Association of Internal Medicine.
Acknowledgements
This study was supported by INHA UNIVERSITY Research Grant.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Thomas JM, Musani AI. Malignant pleural effusions: a review. Clin Chest Med. 2013;34:459–471. doi: 10.1016/j.ccm.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 2.Light RW. Pleural diseases. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2013. [Google Scholar]
- 3.Heffner JE, Klein JS. Recent advances in the diagnosis and management of malignant pleural effusions. Mayo Clin Proc. 2008;83:235–250. doi: 10.4065/83.2.235. [DOI] [PubMed] [Google Scholar]
- 4.Heffner JE, Nietert PJ, Barbieri C. Pleural fluid pH as a predictor of survival for patients with malignant pleural effusions. Chest. 2000;117:79–86. doi: 10.1378/chest.117.1.79. [DOI] [PubMed] [Google Scholar]
- 5.Bielsa S, Salud A, Martinez M, Esquerda A, Martin A, Rodriguez-Panadero F, et al. Prognostic significance of pleural fluid data in patients with malignant effusion. Eur J Intern Med. 2008;19:334–339. doi: 10.1016/j.ejim.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 6.Goldstraw P, Crowley J, Chansky K, Giroux DJ, Groome PA, Rami-Porta R, et al. The IASLC Lung Cancer Staging Project: proposals for the revision of the TNM stage groupings in the forthcoming (seventh) edition of the TNM Classification of malignant tumours. J Thorac Oncol. 2007;2:706–714. doi: 10.1097/JTO.0b013e31812f3c1a. [DOI] [PubMed] [Google Scholar]
- 7.Ryu JS, Ryu HJ, Lee SN, Memon A, Lee SK, Nam HS, et al. Prognostic impact of minimal pleural effusion in non-small-cell lung cancer. J Clin Oncol. 2014;32:960–967. doi: 10.1200/JCO.2013.50.5453. [DOI] [PubMed] [Google Scholar]
- 8.Chernow B, Sahn SA. Carcinomatous involvement of the pleura: an analysis of 96 patients. Am J Med. 1977;63:695–702. doi: 10.1016/0002-9343(77)90154-1. [DOI] [PubMed] [Google Scholar]
- 9.Alkhawaldeh K, Biersack HJ, Henke A, Ezziddin S. Impact of dual-time-point F-18 FDG PET/CT in the assessment of pleural effusion in patients with non-small-cell lung cancer. Clin Nucl Med. 2011;36:423–428. doi: 10.1097/RLU.0b013e3182173823. [DOI] [PubMed] [Google Scholar]
- 10.Ashchi M, Golish J, Eng P, O'Donovan P. Transudative malignant pleural effusions: prevalence and mechanisms. South Med J. 1998;91:23–26. doi: 10.1097/00007611-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 11.Ryu JS, Ryu ST, Kim YS, Cho JH, Lee HL. What is the clinical significance of transudative malignant pleural effusion? Korean J Intern Med. 2003;18:230–233. doi: 10.3904/kjim.2003.18.4.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liang QL, Shi HZ, Qin XJ, Liang XD, Jiang J, Yang HB. Diagnostic accuracy of tumour markers for malignant pleural effusion: a meta-analysis. Thorax. 2008;63:35–41. doi: 10.1136/thx.2007.077958. [DOI] [PubMed] [Google Scholar]
- 13.Shi HZ, Liang QL, Jiang J, Qin XJ, Yang HB. Diagnostic value of carcinoembryonic antigen in malignant pleural effusion: a meta-analysis. Respirology. 2008;13:518–527. doi: 10.1111/j.1440-1843.2008.01291.x. [DOI] [PubMed] [Google Scholar]
- 14.Ishimoto O, Saijo Y, Narumi K, Kimura Y, Ebina M, Matsubara N, et al. High level of vascular endothelial growth factor in hemorrhagic pleural effusion of cancer. Oncology. 2002;63:70–75. doi: 10.1159/000065723. [DOI] [PubMed] [Google Scholar]
- 15.Shen YC, Liu MQ, Wan C, Chen L, Wang T, Wen FQ. Diagnostic accuracy of vascular endothelial growth factor for malignant pleural effusion: a meta-analysis. Exp Ther Med. 2012;3:1072–1076. doi: 10.3892/etm.2012.514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Davies HE, Sadler RS, Bielsa S, Maskell NA, Rahman NM, Davies RJ, et al. Clinical impact and reliability of pleural fluid mesothelin in undiagnosed pleural effusions. Am J Respir Crit Care Med. 2009;180:437–444. doi: 10.1164/rccm.200811-1729OC. [DOI] [PubMed] [Google Scholar]
- 17.Pass HI, Levin SM, Harbut MR, Melamed J, Chiriboga L, Donington J, et al. Fibulin-3 as a blood and effusion biomarker for pleural mesothelioma. N Engl J Med. 2012;367:1417–1427. doi: 10.1056/NEJMoa1115050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Porcel JM. Pleural fluid biomarkers: beyond the Light criteria. Clin Chest Med. 2013;34:27–37. doi: 10.1016/j.ccm.2012.11.002. [DOI] [PubMed] [Google Scholar]
- 19.Sriram KB, Relan V, Clarke BE, Duhig EE, Yang IA, Bowman RV, et al. Diagnostic molecular biomarkers for malignant pleural effusions. Future Oncol. 2011;7:737–752. doi: 10.2217/fon.11.45. [DOI] [PubMed] [Google Scholar]
- 20.Loddenkemper R. Thoracoscopy: state of the art. Eur Respir J. 1998;11:213–221. doi: 10.1183/09031936.98.11010213. [DOI] [PubMed] [Google Scholar]
- 21.Maskell NA, Gleeson FV, Davies RJ. Standard pleural biopsy versus CT-guided cutting-needle biopsy for diagnosis of malignant disease in pleural effusions: a randomised controlled trial. Lancet. 2003;361:1326–1330. doi: 10.1016/s0140-6736(03)13079-6. [DOI] [PubMed] [Google Scholar]
- 22.Musani AI. Treatment options for malignant pleural effusion. Curr Opin Pulm Med. 2009;15:380–387. doi: 10.1097/MCP.0b013e32832c6a8a. [DOI] [PubMed] [Google Scholar]
- 23.Roberts ME, Neville E, Berrisford RG, Antunes G, Ali NJ BTS Pleural Disease Guideline Group. Management of a malignant pleural effusion: British Thoracic Society Pleural Disease Guideline 2010. Thorax. 2010;65(Suppl 2):ii32–ii40. doi: 10.1136/thx.2010.136994. [DOI] [PubMed] [Google Scholar]
- 24.Uzbeck MH, Almeida FA, Sarkiss MG, Morice RC, Jimenez CA, Eapen GA, et al. Management of malignant pleural effusions. Adv Ther. 2010;27:334–347. doi: 10.1007/S12325-010-0031-8. [DOI] [PubMed] [Google Scholar]
- 25.Myers R, Michaud G. Tunneled pleural catheters: an update for 2013. Clin Chest Med. 2013;34:73–80. doi: 10.1016/j.ccm.2012.12.003. [DOI] [PubMed] [Google Scholar]
- 26.Davies HE, Mishra EK, Kahan BC, Wrightson JM, Stanton AE, Guhan A, et al. Effect of an indwelling pleural catheter vs chest tube and talc pleurodesis for relieving dyspnea in patients with malignant pleural effusion: the TIME2 randomized controlled trial. JAMA. 2012;307:2383–2389. doi: 10.1001/jama.2012.5535. [DOI] [PubMed] [Google Scholar]
- 27.Rodriguez-Panadero F, Montes-Worboys A. Mechanisms of pleurodesis. Respiration. 2012;83:91–98. doi: 10.1159/000335419. [DOI] [PubMed] [Google Scholar]
- 28.Tan C, Sedrakyan A, Browne J, Swift S, Treasure T. The evidence on the effectiveness of management for malignant pleural effusion: a systematic review. Eur J Cardiothorac Surg. 2006;29:829–838. doi: 10.1016/j.ejcts.2005.12.025. [DOI] [PubMed] [Google Scholar]
- 29.Walker-Renard PB, Vaughan LM, Sahn SA. Chemical pleurodesis for malignant pleural effusions. Ann Intern Med. 1994;120:56–64. doi: 10.7326/0003-4819-120-1-199401010-00010. [DOI] [PubMed] [Google Scholar]
- 30.Shaw P, Agarwal R. Pleurodesis for malignant pleural effusions. Cochrane Database Syst Rev. 2004;(1):CD002916. doi: 10.1002/14651858.CD002916.pub2. [DOI] [PubMed] [Google Scholar]
- 31.Paschoalini Mda S, Vargas FS, Marchi E, Pereira JR, Jatene FB, Antonangelo L, et al. Prospective randomized trial of silver nitrate vs talc slurry in pleurodesis for symptomatic malignant pleural effusions. Chest. 2005;128:684–689. doi: 10.1378/chest.128.2.684. [DOI] [PubMed] [Google Scholar]
- 32.Mohsen TA, Zeid AA, Meshref M, Tawfeek N, Redmond K, Ananiadou OG, et al. Local iodine pleurodesis versus thoracoscopic talc insufflation in recurrent malignant pleural effusion: a prospective randomized control trial. Eur J Cardiothorac Surg. 2011;40:282–286. doi: 10.1016/j.ejcts.2010.09.005. [DOI] [PubMed] [Google Scholar]
- 33.Ren S, Terman DS, Bohach G, Silvers A, Hansen C, Colt H, et al. Intrapleural staphylococcal superantigen induces resolution of malignant pleural effusions and a survival benefit in non-small cell lung cancer. Chest. 2004;126:1529–1539. doi: 10.1378/chest.126.5.1529. [DOI] [PubMed] [Google Scholar]
- 34.Janssen JP, Collier G, Astoul P, Tassi GF, Noppen M, Rodriguez-Panadero F, et al. Safety of pleurodesis with talc poudrage in malignant pleural effusion: a prospective cohort study. Lancet. 2007;369:1535–1539. doi: 10.1016/S0140-6736(07)60708-9. [DOI] [PubMed] [Google Scholar]
- 35.Puri V, Pyrdeck TL, Crabtree TD, Kreisel D, Krupnick AS, Colditz GA, et al. Treatment of malignant pleural effusion: a cost-effectiveness analysis. Ann Thorac Surg. 2012;94:374–379. doi: 10.1016/j.athoracsur.2012.02.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nam HS, Ryu JS. Diagnosis and management of malignant pleural effusion. Korean J Med. 2011;81:167–173. [Google Scholar]



