Abstract
Objective
Our objective was to assess the efficacy of Problem Solving Therapy for Primary Care (PST-PC) for preventing episodes of major depression and mitigating depressive symptoms in older black and white adults, as compared with an active control condition-- coaching in healthy dietary practices (“DIET”),
Methods
247 participants (90 blacks, 154 whites, 3 Asians) with subsyndromal depressive symptoms were recruited into a randomized, “indicated” depression prevention trial comparing effects of PST-PC and DIET on time to episodes of major depressive disorder (SCID/DSM-IV) and level of depressive symptoms (Beck Depression Inventory) over two years. Cumulative intervention time was similar in PST-PC or DIET, averaging 5.5- 6.0 hours in each arm.
Results
PST-PC and DIET did not differ significantly in time to major depressive episodes (HR = .87; p > .748). Participants in both arms experienced low incidence of such episodes (blacks: n=8, 9%; whites n=13, 8%), compared to published rates of one in four or five over one year in persons with subsyndromal symptoms receiving care as usual. Participants also showed a mean decrease of 4 points in depressive symptoms, sustained over two years. Despite greater burden of depression risk factors among blacks, no significant differences with whites were found in the primary outcome
Conclusion
Both PST-PC and DIET are potentially effective in protecting older black and white adults with subsyndromal depressive symptoms from developing episodes of major depression over two years. Absent a control for concurrent usual care, this conclusion is preliminary. If confirmed, both interventions hold promise as scalable, safe, non-stigmatizing interventions for delaying or preventing episodes of major depression in the nation’s increasingly diverse older population.
Introduction
Major depressive disorder is prevalent, with adequate treatment being difficult to access and only partially successful in averting years lived with disability [1]. In later life, particularly, major depressive disorder has public health importance due to its prevalence and associated disability, morbidity, health care costs, and mortality, especially in primary care outpatients and in racial/ethnic minorities [2]. MDD is also a risk factor for dementia [3]. The limitations of treatment underscore the need to develop public-health relevant approaches to prevent depression and its down-stream consequences in high-risk older adults.
Minority elderly demonstrate particular vulnerability to common mental illnesses. Older blacks, for example, endorse significantly greater depressive symptoms than whites [4] and bear a higher burden of risk for depression based in social and medical disadvantages [5]: more disability, greater health risks (e.g., obesity, smoking, substance use disorders), lower educational attainment, and lower likelihood of marriage compared to whites [6]. Blacks also have a higher incidence of dementia [7], and preventing depression may delay or prevent dementia [8]. In addition, inequalities in the rates of mental health services use and treatment of depression continue to grow [9], compounded by barriers of trust, stigma, and shortages of like-ethnic providers [10].
Mildly symptomatic individuals are at highest risk for developing episodes of major depression [11] [12] [13]. Bereavement, social isolation, sleep disturbance, disability, previous depression, and female gender are important risk factors for depression in older community resident adults [14]. Per the Institute of Medicine, focusing depression prevention on mildly symptomatic persons (“indicated” prevention) may have the greatest efficiency from a public health perspective, with a lower number needed to treat to prevent one incident case [14,15].
The dearth of randomized controlled prevention trials in older adults, however, raises the question of which interventions to use. Older patients, especially blacks, prefer psychosocial interventions to antidepressant medication for treatment of depression [16]. Moreover, antidepressant medications, while effective in severe depression, appear to show minimal benefit relative to placebo in mild depression [17], although the notion that mild depression does not respond to antidepressant medication is not settled [18].
Problem–solving therapy for primary care (PST-PC) is a brief intervention with antidepressant treatment efficacy, deliverable by non-mental health clinicians in primary care [19] [20]. It delays or prevents depression in older adults with macular degeneration [21] and following stroke [22]. The antidepressant and depression-preventing effects of PST-PC may be mediated by a seven-step approach to better problem solving (including behavioral activation), leading to improved self-efficacy and resilience, together with reduction in learned helplessness [23].
In designing this trial, we sought a culturally acceptable, active comparison intervention to control for non-specific effects of time and attention inherent in PST-PC. The choice of coaching in healthy dietary practices (“DIET”) grew out of field data collected from 1244 black participants in the Healthy Black Family Project at the University of Pittsburgh’s Graduate School of Public Health, in which many of the respondents with high levels of stress were either over-weight (45%) or obese (50%). Our Community Research Advisory Board endorsed the choice of DIET as an active control arm and as a culturally acceptable strategy consistent with clinical equipoise and one which would facilitate recruitment of black participants (many of whom were not receiving primary care services) more easily than treatment as usual or a no-intervention control.
Our primary study hypothesis was that PST-PC would reduce incident episodes of major depression by 50% over two years, relative to DIET. Our second hypothesis was that participants in PST-PC would report more and better sustained decline in depressive symptoms than in DIET.
Participants and Methods
Informed Consent, Screening, Assessment, and Enrollment
The protocol was overseen by a Data Safety Monitoring Board and reviewed and approved annually by the University of Pittsburgh’s Institutional Review Board.
Beginning in September, 2006, and extending over a period of 42 months, we enrolled a sample of 247 participants: 154 whites, 90 blacks, and 3 Asians (Table 1). To recruit participants with subsyndromal depressive symptoms, we screened individuals aged 50 and older, using the CES-D [24], requiring a score of 11 or greater and an absence of a major depressive episode during the previous year. We administered the Structured Clinical Interview for DSM-IV Disorders [25] to rule out current major depressive disorder. Participants were also required to have a Mini-Mental State Score [26] of 24 or higher, to exclude probable dementia An episode of alcohol or other substance use disorder within the past 12 months, a history of bipolar disorder, other psychotic disorder, or neurodegenerative disorder also were grounds for exclusion. Recruitment pathways to study participation differed for blacks and whites, largely reflecting the different settings in which help-seeking takes place (Table 2). For example, the major source of white participants was referrals from primary care practices, while for black participants the major source was community-based agencies, including black churches.
Table 1.
Sociodemographic and Clinical Characteristics of Participants in PST-PC and DIET
| PST-PC N=125 |
DIET N=122 |
|||||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | Test statistic | df | p | |
| Sociodemographics | ||||||||
| Age (years) | 65.8±10.9 | 65.4±11.0 | 247 | .28 | 245 | p>.778 | ||
| %Female | 86 | 69 | 90 | 74 | 247 | .52 | 1 | p>.470 |
| Race | 247 | |||||||
| %Asian Pacific | 2 | 2 | 1 | 1 | p>.541a | |||
| %Black | 42 | 34 | 48 | 39 | ||||
| %White | 81 | 65 | 73 | 60 | ||||
| Education (years) | 14.4±2.8 | 14.7±2.7 | 247 | −.78 | 245 | p>.436 | ||
| Marital Status | ||||||||
| %co-habitating/married | 58 | 46 | 56 | 46 | 247 | 1.68 | 3 | p>.640 |
| %divorced/separated | 21 | 17 | 27 | 22 | ||||
| %never married | 17 | 14 | 12 | 10 | ||||
| %widowed | 29 | 23 | 27 | 22 | ||||
| %Employed | 52 | 42 | 47 | 39 | 247 | .13 | 1 | p>.716 |
| Median Household Income | 50510.8±25786.5 | 45545.2±21598.7 | 243 | 1.62 | 241 | p>.105 | ||
| Health | ||||||||
| Cumulative Illness Rating Scale (CIRSG) | ||||||||
| Totalb | 7.7±3.6 | 8.0±4.2 | 245 | −.60 | 243 | p>.550 | ||
| Countc | 4.9±2.1 | 5.0±2.4 | 246 | −.48 | 244 | p>.628 | ||
| Heart + Vasculard | 2.0±1.5 | 1.9±1.5 | 246 | .60 | 244 | p>.549 | ||
| Body Mass Index (BMI) | ||||||||
| Total | 30.5±6.6 | 30.6±7.3 | 245 | −.07 | 243 | p>.942 | ||
| % ≥ 30 | 57 | 46 | 62 | 52 | 245 | .68 | 1 | p>.411 |
| Health Status Inventory (RAND12) | ||||||||
| Physical Health Component | 41.3±11.8 | 42.9±11.8 | 207 | −.95 | 205 | p>.342 | ||
| Mental Health Component | 42.4±9.8 | 43.7±9.0 | 207 | −1.04 | 205 | p>.297 | ||
| Cognitive Status | ||||||||
| Mini-Mental Status Examinatione | 28.1±1.7 | 28.4±1.5 | 246 | −1.38 | 244 | p>.170 | ||
| Mental Health | ||||||||
| Hamilton Rating Scale for Depression (17 Items)f | 11.6±4.0 | 10.8±3.5 | 246 | 1.68 | 244 | p>.094 | ||
| Center for Epidemiologic Studies Depression Scaleg | 21.9±8.3 | 20.4±7.5 | 246 | 1.48 | 244 | p>.141 | ||
| Beck Depression Inventoryh | 11.1±5.9 | 9.9±5.5 | 233 | 1.60 | 231 | p>.110 | ||
| Brief Symptom Inventory Anxiety | .5±.5 | .5±.5 | 235 | −.16 | 233 | p>.875 | ||
| % History of major depressive disorder | 41 | 33 | 42 | 34 | .02 | 1 | p>.892 | |
| % History of anxiety disorder | 27 | 22 | 25 | 20 | .00 | 1 | p>.954 | |
| %Current anxiety disorder | 27 | 22 | 33 | 27 | .72 | 1 | p>.395 | |
| Social Problem Solving Inventory (SPSI) | ||||||||
| SPSI Total | 99.8±13.7 | 103.1±13.0 | 214 | −1.82 | 212 | p>.070 | ||
| Positive Problem Orientation | 95.8±16.4 | 99.8±14.7 | 229 | −1.92 | 227 | p>.056 | ||
| Referral Source | ||||||||
| Kingsley Center, Healthy Black Family Project, Healthy Hearts and Souls, Giant Eagle Screening, Barbershop | 22 | 18 | 24 | 20 | 3.54 | 5 | p>.618 | |
| Mental Health Specialist | 5 | 4 | 5 | 4 | ||||
| Primary Care | 53 | 43 | 57 | 47 | ||||
| Research (research program or registry) | 13 | 11 | 12 | 10 | ||||
| Self-referred (media, brochure, presentation, peer educator) | 23 | 19 | 13 | 11 | ||||
| Word of Mouth | 7 | 6 | 10 | 8 |
Fisher Exact p-value reported
Possible scores range from to 0 to 52, with higher scores indicating more medical burden.
Possible scores range from to 0 to 13, with higher scores indicating more medical burden.
Possible scores range from to 0 to 8, with higher scores indicating more medical burden.
Possible scores range from to 0 to 30, with higher scores indicating more cognitive impairment.
Possible scores range from to 0 to 52, with higher scores indicating more depressive symptoms.
Possible scores range from to 0 to 60, with higher scores indicating more depressive symptoms.
Possible scores range from to 0 to 63, with higher scores indicating more depressive symptoms.
Possible scores range from to 0 to 4, with higher scores indicating more anxiety symptoms.
Table 2.
Sociodemographic and Clinical Characteristics of Black and White Participants
| Whites N=154 |
Blacks N=90 |
|||||||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | N | statistic | df | p | |
| Sociodemographics | ||||||||
| Age (years) | 65.5±11.7 | 65.8±9.7 | 244 | .24 | 242 | p>.813 | ||
| %Female | 104 | 68 | 70 | 78 | 244 | 2.44 | 1 | p>.118 |
| Education (years) | 15.2±2.8 | 13.3±2.2 | 244 | −5.56 | 242 | p<.001 | ||
| Marital Status | 244 | 21.74 | 3 | p<.001 | ||||
| %co-habitating/married | 88 | 57 | 25 | 28 | ||||
| %divorced/separated | 22 | 14 | 25 | 28 | ||||
| %never married | 12 | 8 | 16 | 18 | ||||
| %widowed | 32 | 21 | 24 | 27 | ||||
| %Employed | 71 | 46 | 27 | 30 | 244 | 5.48 | 4 | p<.019 |
| Median Household Income | 58,272.8±23, 210.1 | 31,003.1±13,137.0 | 240 | −10.16 | 238 | p<.001 | ||
| Health | ||||||||
| Cumulative Illness Rating Scale (CIRSG) | ||||||||
| Totalb | 7.4±3.8 | 8.4±4.0 | 242 | 1.89 | 240 | p>.059 | ||
| Countc | 4.8±2.2 | 5.2±2.2 | 243 | 1.60 | 241 | p>.109 | ||
| Heart + Vasculard | 1.8±1.5 | 2.1±1.5 | 243 | 1.34 | 241 | p>.181 | ||
| Body Mass Index (BMI) | ||||||||
| Total | 29.1±6.4 | 33.0±7.0 | 242 | 4.34 | 240 | p<.001 | ||
| % ≥ 30 | 60 | 39 | 57 | 63 | 242 | 11.95 | 1 | p<.001 |
| Health Status Inventory (RAND12) | ||||||||
| Physical Health Component | 43.9±11.3 | 38.8±12.0 | 204 | −3.00 | 202 | p<.004 | ||
| Mental Health Component | 42.9±9.2 | 43.3±9.9 | 204 | .27 | 202 | p>.788 | ||
| Cognitive Status | ||||||||
| Mini-Mental Status Examinatione | 28.7±1.3 | 27.4±1.8 | 243 | −6.61 | 241 | p<.001 | ||
| Mental Health | ||||||||
| Hamilton Rating Scale for Depression (17 Items)f | 10.9±3.7 | 11.7±3.8 | 243 | 1.64 | 241 | p>.101 | ||
| Center for Epidemiologic Studies Depression Scaleg | 21.1±8.0 | 21.3±7.9 | 243 | .19 | 241 | p>.851 | ||
| Beck Depression Inventoryh | 10.6±5.3 | 10.4±6.4 | 230 | −.22 | 228 | p>.829 | ||
| Brief Symptom Inventory Anxiety | .5±.5 | .5±.5 | 232 | −.41 | 230 | p>.684 | ||
| % History of major depressive disorder | 54 | 35 | 28 | 31 | 244 | .24 | 1 | p>.623 |
| % History of anxiety disorder | 30 | 19 | 22 | 24 | 244 | .56 | 1 | p>.452 |
| %Current anxiety disorder | 45 | 29 | 14 | 16 | 244 | 5.06 | 1 | p<.025 |
| Social Problem Solving Inventory (SPSI) | ||||||||
| SPSI Total | 100.3±13.4 | 103.7±13.4 | 212 | 1.80 | 210 | p>.073 | ||
| Positive Problem Orientation | 95.9±15.2 | 100.9±16.1 | 227 | 2.38 | 225 | p<.018 | ||
| Referral Source | 244 | 89.62 | 5 | p<.001 | ||||
| Kingsley Center, Healthy Black Family Project, Healthy Hearts and Souls, Giant Eagle Screening, Barbershop | 4 | 3 | 42 | 47 | ||||
| Mental Health Specialist | 7 | 5 | 3 | 3 | ||||
| Primary Care | 95 | 62 | 15 | 17 | ||||
| Research (research program or registry) | 19 | 12 | 6 | 7 | ||||
| Self-referred (media, brochure, presentation, peer educator) | 22 | 14 | 14 | 16 | ||||
| Word of Mouth | 7 | 5 | 10 | 11 |
Fisher Exact p-value reported
Possible scores range from to 0 to 52, with higher scores indicating more medical burden.
Possible scores range from to 0 to 13, with higher scores indicating more medical burden.
Possible scores range from to 0 to 8, with higher scores indicating more medical burden.
Possible scores range from to 0 to 30, with higher scores indicating more cognitive impairment.
Possible scores range from to 0 to 52, with higher scores indicating more depressive symptoms.
Possible scores range from to 0 to 60, with higher scores indicating more depressive symptoms.
Possible scores range from to 0 to 63, with higher scores indicating more depressive symptoms.
Possible scores range from to 0 to 4, with higher scores indicating more anxiety symptoms.
Randomization
A project statistician randomly assigned participants to either PST-PC or DIET, using permuted-block randomization stratified by the presence/absence of a history of major depression (since a past history is a strong risk factor for future episodes) and by site of recruitment --primary care, community agencies, specialty mental health—given the different sociodemographic characteristics of participants (including race) recruited from each type of site, as well as the possibility that recruitment site could influence rates of occurrence of major depressive episodes. Random assignment was communicated by the statistician to the project co-coordinator but concealed from independent evaluators. There were no instances of the blind being broken.
Interventions
Both interventions - PST-PC and DIET - had similar numbers of sessions (6–8 sessions) and semi-annual boosters (30–45 minutes at 3, 9, and 15 months). Both interventions were provided by interventionists trained in our NIMH-sponsored center for depression prevention and treatment in older adults. Both interventions included homework assignments and monitoring of adherence, and focused on concerns identified by each participant.
The experimental group received manualized PST-PC. To teach the model, the first session lasted an hour and the subsequent sessions lasted 30 minutes each (total time 4.55±1.46 hours in PST-PC and 3.92±2.19 hours in DIET).
Participants in DIET received coaching in healthy eating practices. Using a manualized educational intervention, interventionists reviewed general nutrition guidelines, including the US Department of Agriculture Food Pyramid, helped with preparing weekly menus and grocery lists, saving food coupons, and reviewed food intake since last visit. Topics discussed included access to healthy food, cost of food, meal preparation, culturally specific and acceptable foods, and specific topics raised by participants.
Interventionists were six white social workers and mental health nurses. The same interventionists delivered both PST-PC and DIET, to avoid confounding intervention with clinician effects. To ensure fidelity of intervention delivery, we used group supervision and one-on-one feedback using evaluations of randomly selected 20% of audiotapes of PST-PC and DIET sessions. PST-PC adherence ratings assessing quality were completed by the intervention supervisor, using two sessions for each case —an early session (1–3) and a later session (4–8). Following a batch of ratings, corrective feedback was provided. A majority (n=41/56,73%) of sessions of both PST-PC and DIET was rated as adherent. A treatment fidelity scale was also developed to document the absence of intervention contamination effects. Using this scale, ratings were completed on seven consecutive minutes of the session starting five minutes into the session. Sessions were rated independently by two raters for the presence of PST-PC elements and DIET elements. Based upon blind ratings, we found the two interventions to be highly discriminable (κ=.91), even though delivered by the same interventionists. Interventions were delivered primarily face to face in settings requested by the participants themselves: primary care offices, community agencies, and participant homes. About 9% (n=173/1884) of sessions were delivered over the telephone.
Outcomes
The primary outcome was incident episodes of major depression, per the SCID/DSM-IV section for mood disorders, [25] administered by independent evaluators blind to randomized intervention assignment at baseline (T1), at the end of intervention (T2), and every three months (T3 –T9) subsequently until 24 months. Also assessed at the same time points were levels of depressive symptoms (Beck Depression Inventory: BDI) [27] and health-related quality of life (SF 12) [28]. Other domains of assessment encompassed coexisting medical illness per total score on the Cumulative Illness Rating Scale for Geriatrics [29], problem solving skills (Social Problem Solving Inventory) [30], and anxiety (Brief Symptom Inventory: BSI) [31]. (Outcomes other than depression will be reported in a separate communication.)
Data analysis
Outcomes analyses were conducted blind to study arm by study statisticians operating independently of the investigators. All analyses were performed using the intent-to-treat principle so that comparisons were made according to the assigned intervention groups. All data were examined for normality prior to analyses and transformations were used where necessary. Baseline demographic and clinical differences between participants randomly assigned to PST-PC and DIET (Table 1) and between black and white participants (Table 2) were tested using t-tests for continuous variables and chi-square with continuity-correction for categorical. To display the comparison of the effects of PST-PC and DIET on incidence of major depressive episodes, Kaplan-Meier curves were employed. Formal inferences between groups were made using log-rank tests if the expected numbers of events in both arms were ≥ 5 or using Fisher’s exact tests otherwise. Multivariate Cox proportional hazard models were used to explore strongest predictors of major depressive disorder.
To compare depression levels (BDI), we first tested whether or not baseline differences were present between intervention groups. In cases where no differences were apparent, we then employed a mixed models approach to compare the trajectories of the variables over time between the groups. If there was a significant baseline difference between groups, we used the baseline value as a covariate in the fitted models. To characterize and compare the trajectories between PST-PC and DIET, we used mixed models examining intervention, time, time-squared, and the potential interactions among intervention and the time variables. In analyses involving race, we included race and the interactions among race and other variables. We documented reasons for missing data and handled missing data using mixed-model analyses. Formal tests were conducted to determine whether the missingness of data was at random.
To examine effects of Social Problem Solving Inventory (SPSI) on depressive symptoms, we conducted exploratory analyses and included the SPSI scores as time-varying covariate in the whole group longitudinal model. To examine the possibility of bidirectional relationship of SPSI scores and depressive symptoms, we also examined SPSI scores as outcome using same model of treatment, time and treatment*time effects but include BDI as time-varying covariate.
Results
PST-PC and DIET participants did not differ in sociodemographic, health, cognitive, mental health and recruitment pathways (Table 1). Primary care referrals provided the main source of enrollment, followed by recruitment in community based agencies and by self-referral in response to print and on-air advertisements.
Participant descriptive data (Table 2)
Blacks differed significantly from whites in having: fewer years of formal education, greater likelihood of living alone, less likelihood of being employed, lower household income, greater rate of obesity, lower physical health–related quality of life, lower scores on cognitive screening measures, and lower rate of current anxiety disorder. Despite the greater burden of social and medical disadvantages, black participants did not differ from whites on pre-interventions measures of emotional distress (CES-D), depression (BDI), or anxiety (BSI); and proportion with past history of major depressive disorder. Black and white participants were similar on the Social Problem Solving Inventory (a self-report measure of problem-solving style) [30], with the one exception of a higher positive problem orientation (a measure of active coping and resilience) among black participants. More whites than blacks had a current anxiety disorder, despite lower social and medical burden in whites.
Survival analysis of time to episodes of major depressive disorder
PST-PC and DIET did not differ significantly in time to major depressive episodes (HR=.87, p>.748). Moreover, we observed similar incidence in black participants (8/90; 9% [95%CI 4.–17%]) and in whites (13/154; 8% [95%CI: 5–14%]), and similar incidence as well as by recruitment site (mental health specialty (7/67, 10% [95%CI: 4–19%], community agencies (5/62, 8% [95%CI: 3–18%] and primary care practices (9/111, 10%[95%CI:4–15%]). Multivariate Cox proportional hazard models identified the two strongest predictors of incident episodes: greater cumulative medical comorbidity (total CIRS-G scores, HR = 1.18; 95% CI: 1.07–1.31); and greater severity of depressive symptoms (Beck Depression Inventory, HR = 1.17; 95% CI: 1.09–1.25). Every one unit increase in total CIRS-G increased hazard of an event by 18%; and a unit increase on the BDI increased hazard by 17%.
The overall drop-out rate was 24% (59/247), not differing by study arms or race. Thus, similar percentages of blacks (n=62,69%) and whites (n=102, 66%) completed the study, experienced the onset of major depressive episodes (n=8,9%, n=13, 8%), died during the trial (n=2, 2%, n=3, 2%; no suicides), or dropped out related to loss of interest or respondent burden, participant relocation or additional diagnosis (n=18, 20%, n=36, 23%). We observed no differences in age, race, or baseline severity of depressive symptoms between participants who completed the trial and those who did not. However, a higher percentage of women did complete the trial than men (144/176, 82%, versus n=44/71, 62%; chi squared = 9.90, p < .001). PST-PC and DIET had comparable percentages of men and women participants randomly assigned to each arm.
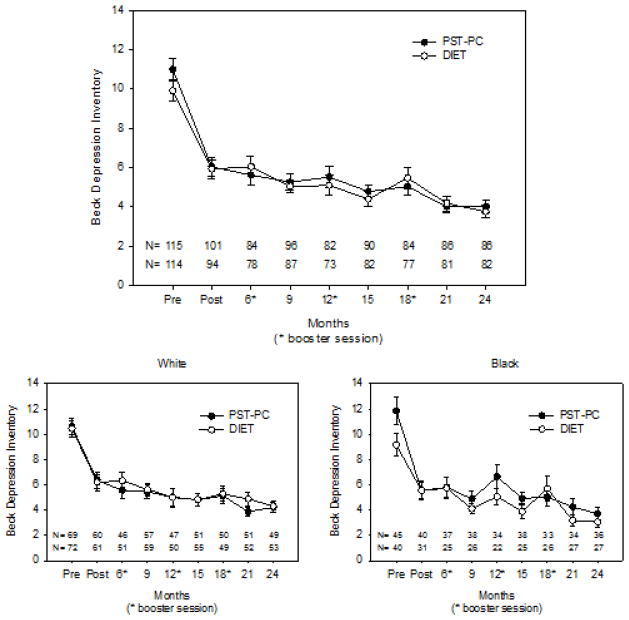
Symptom burden (Figure)
Figure 1. Trajectories of Beck Depression Inventory Scores in PST-PC and DIET.
Participants in both PST-PC and DIET demonstrated similar improvement in depressive symptoms (BDI). Improvements were sustained over two years. There was a significant quadratic and linear time effects (F(1,1356)=75.91, p<.001 and F(1,1356)=159.57, p<.001 respectively), but no significant intervention or intervention by time effects (F(1,1356)=2.49, p>.114 and F(1,1356)=.46, p>0.496). When examining race as moderator, we observed baseline difference in blacks between interventions; thus, we ran the model co-varying for baseline score. We detected significant time effect (F(1,1115)=26.78, p<.001) for post-intervention through 2 years, but no significant race, race*intervention or race*time effects.
Participants in both arms experienced on average a 4 point drop in depressive symptoms (BDI), with improvements sustained over two years of follow up. Black and white participants demonstrated similar patterns of responses to PST-PC and DIET on measures of depressive symptoms.
Both interventions were associated with similar and sustained improvements on total scores of the Social Problem Solving Inventory, a composite measure of self-reported positive problem solving orientation (active coping), negative problem orientation (avoidant coping, impulsivity, and rational problem solving [30,32] from pre to post treatment. SPSI score was a significant covariate in our longitudinal model of Beck depressive symptom (BDI) scores. An increase (improvement) in SPSI score was associated with a decrease in depressive symptoms (beta = −.030 ± .003, t(799)=−9.80, p<.001). Conversely, when examining SPSI scores as outcome using the same model of treatment, time and treatment*time effects, and including BDI as covariate, we found a bidirectional relationship such that depressive symptom scores were also a significant time-varying covariate of SPSI. A decrease in depression symptoms was associated with an increase (improvement) in SPSI Score (beta=−.654 ± .062, t(799)=−10.56, p< .001).
Discussion
Both PST-PC and DIET are potentially effective in protecting older black and white adults over two years from the persistence of depressive symptoms (average of 4-point drop in Beck depression scores) and from the concomitant risk posed by persistent subsyndromal depressive symptoms for incident episodes of major depression. However, in the absence of a concurrent, usual-care control, this conclusion should be regarded as preliminary. Compared with previously published rates of incident major depression in persons with subsyndromal symptoms receiving usual care (1 in four to five over one year) (24–27), the apparent protective effect against major depression is noteworthy. We made a pragmatic decision not to control for care as usual (in effect a control for time’s passage, since treatment as usual is often no treatment at all) for several reasons, namely many black participants lacked primary care services, our community advisory board warned that it could be a barrier to participation, and other studies of treatment as usual, including our own, [33] have observed that subsyndromal depressive symptoms tend to persist under conditions of usual care, not improving, and putting individuals at risk for major depressive disorder and deteriorating quality of life.[33–37] For example, in our study of suicide prevention in primary care elderly {PROSPECT [34]}, older adults with subsyndromal symptoms, under conditions of usual care, had greater than a 5-fold increased risk of conversion of major depressive disorder within one year, compared to those without such symptoms.[33,35] Similarly, in a Dutch study of 170 older primary care patients aged 75 and older with subthreshold symptoms of depression and anxiety, a stepped-care intervention (which included problem solving therapy) reduced the incidence of depressive and anxiety disorders by 50% over one year relative to care as usual (24% versus 12%).[36] A similar result was reported in the MANAS trial (25% versus 12.3%) in a mixed-aged sample of primary care patients in Goa, India.[37] Our data showed an incidence of major depression of 21/247 or 9% over two years and 13/247 (5%) over one year, similar to the Dutch and Indian observations. This observation contrasts with published rates of major depressive disorder episodes over two years was one in four to five (20–25%), based upon the studies cited above, in which participants were recruited mainly in primary care settings.
A separate but related observation is that our sample was recruited from both primary care clinic and community sites (in order to oversample black participants). Because incidence rates may differ according to locus of recruitment, we stratified the randomization to PST-PC or DIET by locus of recruitment. We did not, however, detect different occurrence rates as a function of primary-care, community-based, or mental health specialty recruitment. Moreover, our community-referred participants were mostly black, and black participants carried a higher burden of risk for major depression than did white participants (table 2).
Contrary to our study hypothesis, we observed in both PST-PC and DIET comparable and sustained reductions in depressive symptoms over time. DIET provided more than a control for face-to-face contact. It was by design an active control intervention in its own right, coaching participants to address the challenges of implementing healthy dietary practices, with homework assignments. Participants in DIET reported both improvements in depressive symptoms and in problem-solving skills. DIET’s active-coping component, as well as social contact, may have protected against depression. Participants were helped to tackle a problem associated with managing health issues. With the higher positive problem solving orientation of black participants, DIET fit culturally with life experience of having to problem solve/cope even in the absence of many resources. DIET also did not pose the issues of safety, stigma, and financial burden associated with long term antidepressant pharmacotherapy.
In our longitudinal modeling of covariation between Beck depression scores and scores on the Social Problem Solving Inventory, we observed that increasing (improving) scores on the SPSI predicted lower depression scores; and vice versa, that falling depression scores predicted increasing (improving) scores on the SPSI. This suggests the possibility of a bidirectional effect (that is, better problem solving leads to improvement in depression, and improvement in depression leads to better problem solving). However, this inference should be seen as preliminary, since SPSI scores and BDI scores are very likely to have shared variance based upon their intrinsic definitions and constructs.
The current study breaks new ground in indicated depression prevention research with an active control condition for the effects of attention, face to face time, and support, two years of follow-up, and an adequate number of black participants to explore effects of race on patterns of incident depression, trajectory of symptoms, and changes in health-related quality of life over two years. Most studies of depression prevention have not used an active comparator, have followed patients for shorter periods of time (generally one year), and have not had sufficient racial or ethnic diversity in their study groups to examine variability related to socio-cultural characteristics. Both interventions were found to be acceptable to blacks and whites, with comparably low rates of non-adherence and dropout over two years.
Recruitment and retention of black participants was facilitated by partnerships with community champions for the study, the non-use of antidepressant medication, low respondent burden, and conduct of the study in community settings (including participant homes), rather than in a medical setting. Life-style interventions like DIET may be more culturally appropriate and acceptable in minority communities, regardless of income. These are important strategic considerations for reaching underserved individuals at risk, given that cultural beliefs and stigma contribute to low utilization of mental health care in minority older individuals. At a time on increasing shortages of mental health professionals dedicated to working with older adults (36), it is plausible that PST-PC and DIET may be amenable to delivery by like-ethnic lay health counselors (peer supporters), increasing their scalability in impoverished areas and utility to Federally qualified community health centers or other primary care settings where nurses or health educators could fill this role. Thus, the current results may be particularly pertinent to the integration of primary care and behavioral health services, especially for older patients whose increasing medical comorbidity places them at high risk for major depressive disorders.
Acknowledgments
Supported by P60 MD000207; P30 MH090333; UL1RR024153, UL1TR000005, the UPMC Endowment in Geriatric Psychiatry, and the Commonwealth of Pennsylvania
Footnotes
Clinical Trials.gov ID: NCT00326677
Contributor Information
Charles F. Reynolds, III, Email: ReynoldsCF@upmc.edu, University of Pittsburgh, School of Medicine, Psychiatry, 3811 O’Hara Street, BT 758, Pittsburgh, Pennsylvania, 15213
Stephen B. Thomas, University of Maryland - Center for Health Equity, Maryland
Jennifer Q. Morse, Western Psychiatric Institute & Clinic - Psychiatry, 3811 O’Hara St. Personality Studies, Pittsburgh, Pennsylvania 15213.
Stewart J. Anderson, University of Pittsburgh Graduate School of Public Health - Department of Biostatistics, Pittsburgh, Pennsylvania
Steven Albert, University of Pittsburgh - Behavioral & Community Health Science, Pittsburgh, Pennsylvania 15261.
Mary Amanda Dew, University of Pittsburgh - Psychiatry, 3811 O’Hara Street, Pittsburgh, Pennsylvania 15213
Amy Begley, Western Psychiatric Institute & Clinic - Psychiatry, 3811 O’Hara St. Personality Studies, Pittsburgh, Pennsylvania 15213.
Jordan F. Karp, University of Pittsburgh School of Medicine - Psychiatry, Western Psychiatric Institute and Clinic 3811 O’Hara Street, Pittsburgh, Pennsylvania 15213
Ariel Gildengers, University of Pittsburgh School of Medicine - Dept of Psychiatry, 3811 O’Hara Street, Pittsburgh, Pennsylvania 15213
Meryl A. Butters, University of Pittsburgh Medical Center - Geriatric Psychiatry, 3811 O’Hara St. Rm. E-462 WPIC, Pittsburgh 15213.
Jacqueline A. Stack, University of Pittsburgh - Psychiatry, Pittsburgh, Pennsylvania
John Kasckow, VA Pittsburgh Health Care System - Behavioral Health, 7180 Highland Dr, Pittsburgh, Pennsylvania 15206. University of Pittsburgh Medical Center - Western Psychiatric Institute and Clinics, 3811 O’Hara St, Pittsburgh, Pennsylvania 15213.
Mark D. Miller, University of Pittsburgh, Shcool of Medicine - Psychiatry, Pittsburgh, Pennsylvania
Sandra C. Quinn, University of Maryland - Center for Health Equity, Maryland
References
- 1.Cuijpers P, Beekman ATF, Reynolds CF., III Preventing Depression: A Global Priority. Jama-Journal of the American Medical Association. 2012;307:1033–1034. doi: 10.1001/jama.2012.271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Reynolds CF, III, Cuijpers P, Patel V, et al. Early Intervention to Reduce the Global Health and Economic Burden of Major Depression in Older Adults. In: Fielding JE, Brownson RC, Green LW, editors. Annual Review of Public Health. Palo Alto, CA: Annual Reviews; 2012. [Google Scholar]
- 3.Diniz B, Butters MA, Albert SM, Dew MA, Reynolds CF., III Late-life depression and risk of vascular dementia and Alzheimer’s disease: a systematic review and meta-analysis of population-based cohort studies. British Journal of Psychiatry. 2013;202(5):329–335. doi: 10.1192/bjp.bp.112.118307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jang Y, Borenstein AR, Chiriboga DA, et al. Depressive symptoms among African American and white older adults. J Gerontol B Psychol Sci Soc Sci. 2005;60:313–319. doi: 10.1093/geronb/60.6.p313. [DOI] [PubMed] [Google Scholar]
- 5.Sriwattanakomen R, McPherron J, Chatman J, et al. A comparison of the frequencies of risk factors for depression in older black and white participants in a study of indicated prevention. International Psychogeriatrics. 2010;22:1240–1247. doi: 10.1017/S1041610210001523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.DHHS. A Report of the Surgeon General. Rockville, MD: 2001. Mental Health: Culture, Race and Ethnicity: A Supplement to Mental Health. [PubMed] [Google Scholar]
- 7.Shadlen MF, Siscovick DS, Fitzpatrick AL, et al. Education, cognitive test scores, and black-white differences in dementia risk. Journal of American Geriatrics Society. 2006;54:898–905. doi: 10.1111/j.1532-5415.2006.00747.x. [DOI] [PubMed] [Google Scholar]
- 8.Barnes DE, Yaffe K. The projected effect of risk factor reduction on Alzheimer’s disease prevalence. Lancet Neurol. 2011;10:819–828. doi: 10.1016/S1474-4422(11)70072-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Williams DR. Race, stress, and mental health, in minority health in America: Findings and policy implications from commonwealth fund minority health survey. Baltimore: Johns Hopkins University Press; 2000. [Google Scholar]
- 10.Steffens DC, Artigues DL, Ornstein KA, et al. A review of racial differences in geriatric depression: implications for care and clinical research. Journal of the National Medical Association. 1997;89:731–736. [PMC free article] [PubMed] [Google Scholar]
- 11.Cuijpers P, de Graaf R, van Dorsselaer S. Minor depression: risk profiles, functional disability, health care use and risk of developing major depression. Journal of Affective Disorders. 2004;79:71–79. doi: 10.1016/S0165-0327(02)00348-8. [DOI] [PubMed] [Google Scholar]
- 12.Munoz RF, Ying YW, Bernal G, et al. Prevention of depression with primary care patients: a randomized controlled trial. American Journal of Community Psychology. 1995;23:199–222. doi: 10.1007/BF02506936. [DOI] [PubMed] [Google Scholar]
- 13.Smit F, Ederveen A, Cuijpers P, et al. Opportunities for cost-effective prevention of late-life depression: An epidemiological approach. Archives of General Psychiatry. 2006;63:290–296. doi: 10.1001/archpsyc.63.3.290. [DOI] [PubMed] [Google Scholar]
- 14.Cole MG. Evidence-based review of risk factors for geriatric depression and brief preventive interventions. Psychiatric Clinics of North America. 2005;28:785–803. vii. doi: 10.1016/j.psc.2005.09.010. [DOI] [PubMed] [Google Scholar]
- 15.Schoevers RA, Smit F, Deeg DJH, et al. Prevention of late-life depression in primary care: Do we know where to begin? American Journal of Psychiatry. 2006;163:1611–1621. doi: 10.1176/ajp.2006.163.9.1611. [DOI] [PubMed] [Google Scholar]
- 16.Cooper-Patrick L, Gallo JJ, Gonzales JJ, et al. Race, gender, and partnership in the patient-physician relationship. Journal of the American Medical Association. 1999;282:583–589. doi: 10.1001/jama.282.6.583. [DOI] [PubMed] [Google Scholar]
- 17.Fournier JC, DeRubeis RJ, Hollon SD, et al. Antidepressant drug effects and depression severity: a patient-level meta-analysis. Journal of American Medical Association. 2010;303:47–53. doi: 10.1001/jama.2009.1943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stewart J, Deliyannides D, Hellerstein D, et al. Can people with nonsevere major depression benefit from antidepressant medication? J Clin Psychiatry. 2012;73:518–525. doi: 10.4088/JCP.10m06760. [DOI] [PubMed] [Google Scholar]
- 19.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: A randomized controlled trial. Journal of the American Medical Association. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- 20.Nezu AM, Nezu CM. Problem solving therapy. Journal of Psychotherapy Integration. 2001;11:187–205. [Google Scholar]
- 21.Rovner BW, Casten RJ, Hegel MT, et al. Preventing depression in age-related macular degeneration. Archives of General Psychiatry. 2007;64:886–892. doi: 10.1001/archpsyc.64.8.886. [DOI] [PubMed] [Google Scholar]
- 22.Robinson RG, Jorge RE, Moser DJ, et al. Escitalopram and problem-solving therapy for prevention of poststroke depression: Randomized controlled trial. Journal of the American Medical Association. 2008;299:2391–2400. doi: 10.1001/jama.299.20.2391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alexopoulos GS, Raue P, Arean PA. Problem-solving therapy versus supportive therapy in geriatric major depression with executive dysfunction. American Journal of Geriatric Psychiatry. 2003;11:46–52. [PubMed] [Google Scholar]
- 24.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- 25.First M, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II), Version 2.0. New York: New York State Psychiatric Institute; 1994. [Google Scholar]
- 26.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 27.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 28.Ware J. SF-36 Health Survey. Manual and Interpretation Guide 2. Boston: The Health Institute, New England Medical Center, Nimrod Press; 1997. [Google Scholar]
- 29.Miller MD, Paradis CF, Houck PR, et al. Rating chronic medical illness burden in geropsychiatric practice and research: Application of the Cumulative Illness Rating Scale. Psychiatry Research. 1992;41:237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- 30.D’Zurilla TJ, Nezu AM. Development and preliminary evaluation of the Social Problem-Solving Inventory. Psychological Assessment. 1990;2:156–163. [Google Scholar]
- 31.Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- 32.D’Zurilla TJ, Nezu AM. Problem-solving therapy: A positive approach to clinical intervention. Springer Publishing Company; 2007. [Google Scholar]
- 33.Lyness JM, Heo M, Datto CJ, et al. Outcomes of minor and subsyndromal depression among elderly patients in primary care settings. Annals of Internal Medicine. 2006;144:496–504. doi: 10.7326/0003-4819-144-7-200604040-00008. [DOI] [PubMed] [Google Scholar]
- 34.Bruce ML, Ten Have TR, Reynolds CF, et al. Reducing suicidal ideation and depressive symptoms in depressed older primary care patients: A randomized controlled trial. Journal of the American Medical Association. 2004;291:1081–1091. doi: 10.1001/jama.291.9.1081. [DOI] [PubMed] [Google Scholar]
- 35.Lyness JM, Yu Q, Tang W, et al. Risks for depression onset in primary care elderly patients: potential targets for preventive interventions. Am J Psychiatry. 2009;166:1375–1383. doi: 10.1176/appi.ajp.2009.08101489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.van’t Veer-Tazelaar PJ, van Marwijk HW, van Oppen P, et al. Stepped-care prevention of anxiety and depression in late life: a randomized controlled trial. Archives of General Psychiatry. 2009;66:297–304. doi: 10.1001/archgenpsychiatry.2008.555. [DOI] [PubMed] [Google Scholar]
- 37.Patel V, Weiss HA, Chowdhary N, et al. The effectiveness of a lay health worker intervention for depressive and anxiety disorders in primary care: the Manas cluster randomized controlled trial in Goa, India. The Lancet. 2010;376:2086–2095. doi: 10.1016/S0140-6736(10)61508-5. [DOI] [PMC free article] [PubMed] [Google Scholar]