Abstract
Several lines of evidence suggest that childhood maltreatment is associated with an increased risk for both psychotic disorders and subclinical psychotic-like experiences in the general population. Few studies, however, have sought to examine whether the strength of this relationship is comparable across patient and non-patient groups. The present study sought to compare the strength of the association between childhood maltreatment and self-reported psychotic symptoms in 447 healthy adult volunteers and 184 stable outpatients with schizophrenia or schizoaffective disorder. Strong positive correlations between childhood maltreatment and self-reported symptoms were observed in both groups. Although patients scored significantly higher than controls on both history of childhood maltreatment and self-reported symptoms, the strength of the relationship did not differ between groups. These data provide strong support for etiological continuity between subclinical psychotic symptoms and psychotic disorders.
Keywords: subclinical psychosis, psychotic disorders, childhood maltreatment
Childhood maltreatment is a major public health concern that has significant long-term consequences including an increased risk for poor physical health (Gilbert et al., 2009) and poor mental health outcomes (McLaughlin et al., 2010). The World Health Organization defines childhood maltreatment as all types of physical and/or emotional maltreatment and sexual abuse that results in actual or potential harm to the child and estimates that approximately one third of the general population experiences some form of maltreatment during childhood (Kessler et al., 2010). Several studies have demonstrated an association between childhood maltreatment and psychotic disorders and a recent review and meta-analysis of these studies (Varese et al., 2012) found that childhood adversity is substantially associated with an increased risk for psychosis with a population attributable risk of ~33%.
In recent years, considerable data have provided support for the existence of a continuous distribution of subclinical psychotic symptoms in the general population and several lines of evidence indicate that there is considerable etiological continuity between clinical and subclinical psychosis phenotypes (see Linscott & van Os, 2013 for a review). This continuity is particularly pronounced for the relation between psychosis and childhood maltreatment (van Os & Linscott, 2012) even when genetic vulnerability to psychosis is taken into account (Arseneault et al., 2011). These data suggest that the experience of maltreatment during childhood may create a biological (Read, Perry, Moskowitz, & Connolly, 2001) or psychological (Garety & Rigg, 2001) vulnerability for the development of psychotic symptoms along a continuum (Janssen et al., 2004).
In support of this continuum, Kelleher et al (2013) recently demonstrated a dose-response relationship between childhood trauma and psychotic experiences in a large prospective cohort of adolescents followed over a 12-month period. Specifically, they found that the odds of psychotic experiences increased in line with increasing levels of bullying and physical assault. These data are consistent with findings suggesting that patients with psychotic disorders often have a more severe history of childhood maltreatment than healthy individuals (Kessler et al., 2010). To date, however, only a single study that we are aware of has sought to directly examine whether this difference in severity of childhood maltreatment directly contributes to the severity of self-reported psychotic symptoms across both patient and healthy control groups. Heins and colleagues (2011) examined the relationship between severity of self-reported childhood maltreatment and severity of psychosis ranging from clinically significant psychotic symptoms to schizotypal symptoms across patients with psychotic disorders, their unaffected siblings and healthy controls. These authors found that self-reported histories of childhood abuse were associated with positive symptoms in a dose-response fashion across all three groups. However, the primary analyses in this study relied on a dichotomous measure of child abuse and thus, did not directly assess the strength of the relationship across the study groups. The aim of the present study was to examine whether the strength of the relation between childhood maltreatment and self-reported subclinical psychotic symptoms in healthy adult volunteers differs from the strength of the relation between childhood maltreatment and clinically significant psychotic symptoms in patients with schizophrenia or schizoaffective disorder.
METHOD
Participants
The present sample is comprised of 447 healthy adult volunteers (172 males, 275 females, Mage=41.06±17.06) and 184 stable outpatients with schizophrenia or schizoaffective disorder (127 males, 57 females, Mage=40.98±11.07). Healthy volunteers were recruited from the general population via word of mouth, newspaper and internet advertisements and posted flyers for an NIMH-funded study of subclinical psychosis (MH086756 to PD). Healthy participants were excluded from the study if they had an Axis I affective or psychotic disorder diagnosis, active or recent substance abuse or any disorder known to affect the brain. Approximately 6% of healthy participants screened for this project were excluded; most of whom met for a past affective disorder. Patient participants were recruited from the Zucker Hillside Hospital (ZHH), a division of the North Shore-Long Island Jewish Health System (NSLIJHS), for an NIMH-funded study on functional disability (MH079800 to AKM). Patient participants were excluded from the study if they had a psychiatric hospitalization within the preceding 6 months, met diagnostic criteria for current substance abuse (within the past month), or had a history of CNS trauma, neurological disorder or mental retardation. The patient sample used in the present study represents a subset of a larger sample and were selected based on the availability of data from the Community Assessment of Psychic Experiences (CAPE: Stefanis et al. 2002). The limited availability of CAPE data in the patient sample was due to the late addition of this measurement to an ongoing study of functional disability in psychotic disorder patients. All participants provided written informed consent to a protocol approved by the Institutional Review Board of the NSLIJHS. Specifically, patients provided consent for a study seeking to understand how genetic variability might contribute to differences in long-term prognosis while controls provided consent for a study seeking to understand how genetic variation migh contribute to the normal expression of psychiatric symptoms.
Diagnostic Assessments
Healthy participants were initially administered the Structured Clinical Interview for the DSM-IV, Non-Patient edition (SCID-I/NP) (First, Spitzer, Gibbon, & Williams, 2002a) by Ph.D. or Master’s level psychometricians, to rule out a past or present affective or psychotic disorder. Information obtained from the SCID was compiled into a narrative case summary and presented to two senior ZHH faculty. Absence of pathology was determined by consensus after the presentation of the narrative case summary and discussion of any relevant symptomatology. Patient participants were administered the Structured Clinical Interview for the DSM-IV Axis I Disorders, Patient edition (SCID-I/P) (First, Spitzer, Gibbon, & Williams, 2002b) by by Ph.D. or Master’s level psychometricians. Information obtained from the SCID was supplemented by a review of medical records and interviews with family informants, whenever possible, and compiled into a narrative case summary. Diagnoses were then determined by a consensus among a minimum of three senior ZHH faculty, after a thorough review of the SCID and the corroborating information comprising the narrative case summary..
Assessment of Childhood maltreatment
To assess the history of childhood maltreatment we utilized the 28-item Childhood Maltreatment Questionnaire (CTQ) (Bernstein et al., 2003). The CTQ is a 5-point Likert-type self-report questionnaire that measures several dimensions of abuse and neglect during childhood including physical, emotional and sexual abuse as well as emotional and physical neglect. Summing across all of these dimensions provides a total score that represents the severity of overall maltreatment experienced by an individual during childhood.
Assessment of subclinical and clinical psychopathology
All participants were assessed using the Community Assessment of Psychic Experiences (CAPE) (Stefanis et al., 2006). The CAPE is a 42-item, self-report questionnaire that measures three dimensions of subclinical psychopathology including positive, negative and depressive symptoms. The CAPE provides scores on each of the three dimensions as well as a total score representing the overall severity of subclinical symptoms. Although the CAPE also includes a distress subscale, those scores were not utilized in the present study.
Patient participants were also assessed using standard clinician-administered rating scales to assess symptom severity during the week preceding the interview. These scales included the Brief Psychiatric Rating Scale (BPRS) (Overall & Gorham, 1962), the Scale for the Assessment of Negative Symptoms (SANS) (Andreasen, 1982) and the 17-item Hamilton Rating Scale for Depression (HRSD-17) (Hamilton, 1960). These assessments, which were completed the same day as the CAPE, were used to validate the self-report data derived from the CAPE in the patient sample. Doctoral or Master’s level psychometricians administered all clinician-administered scales. Interrater reliability on all measures, assessed annually using gold standard videotaped interviews, was high (all Kappa’s > .80).
Statistical Analysis
Patients and healthy volunteers were initially compared on demographic variables including age, sex and race using t-tests or chi square where appropriate. Next, groups were compared on the severity of symptoms in each of the 3 domains assessed by the CAPE as well as the individual CAPE subscales. Finally, groups were compared on the severity of history of childhood maltreatment across all domains measured by the CTQ as well as on the total CTQ score.
Because there are few data validating the use of the CAPE in psychotic patients, we initially sought to examine the validity of self-reported symptoms as measured by the CAPE. This was achieved by examining the relationships between scores on each of the subscales derived from the CAPE (positive, negative and depressive symptoms) and standard clinician-administered rating scales which assess the same symptom constructs. Specifically, the negative symptom subscale of the CAPE was compared to the total score derived from the SANS, the depressive symptom subscale was compared to the total score on the HRSD-17 and the positive symptom subscale was compared to the positive symptom subscale derived from the BPRS (Nicholson et al. 1995).
The primary analysis sought to assess whether the overall severity of childhood maltreatment, which has been strongly associated with psychotic disorders, would show a similar relationship to the overall severity of subclinical psychotic symptoms in adults with no psychiatric illness. To this end, we examined the correlations between CTQ total score and CAPE total score in the patients and healthy volunteers separately. We then compared the slopes of the resulting regression lines produced by the two groups using a univariate analysis of covariance (ANCOVA). This analysis examined the interaction between patient/control status and the CTQ total score on the overall CAPE score. All analyses were conducted using SPSS version 11.5.
RESULTS
Comparison of demographic characteristics revealed significant differences in the distributions of males and females (χ2=48.77, p<.001) as well as the distribution of racial groups (χ2=38.67, p<.001) between patients and healthy volunteers. Specifically, the group of healthy volunteers had significantly more females and fewer minorities than the patient group. These data are shown in Table 1.
Table 1.
Characteristics of patients with schizophrenia or schizoaffective disorder and healthy volunteers included in the current study.
| Patients (N=184) |
Controls (N=447) |
Statistic | p value | |
|---|---|---|---|---|
| Mean Age (SD) | 40.98(11.07) | 41.06(17.06) | t=0.07 | 0.95 |
| Percent Female | 30.98 | 61.52 | χ2=48.77 | <.001 |
|
Race White Black Other |
80 68 36 |
311 81 55 |
χ2=38.67 | <.001 |
|
Mean CAPE (SD) Positive Negative Depressive Total |
29.90(8.19) 23.59 (6.83) 13.55(3.96) 67.05(16.02) |
23.46(3.13) 18.62(4.04) 11.44(1.97) 53.52 (7.88) |
U=19,531 U=22,816 U=28,560 U=19,311 |
<.001 <.001 <.001 <.001 |
|
Mean CTQ (SD) Emotional Abuse Physical Abuse Sexual Abuse Emotional Neglect Physical Neglect Total |
11.4(5.56) 8.95 (4.77) 8.40 (5.50) 11.43(5.50) 10.67(3.04) 50.91 (17.49) |
7.27 (3.57) 6.18(2.21) 5.66(2.15) 8.04 (3.87) 9.37(1.42) 36.52 (9.88) |
U=22,413 U=25,328 U=28,977 U=25,580 U=31,117 U=18,293 |
<.001 <.001 <.001 <.001 <.001 <.001 |
| Mean HRSD | 11.59(7.65) | n/a | n/a | n/a |
| Mean SANS (SD) | 29.01 (12.54) | n/a | n/a | n/a |
| Mean BPRS Positive | 5.77 (2.86) | n/a | n/a | n/a |
Consistent with several prior reports, examination of the scores obtained for both the CAPE (Van Os, Linscott, Myin-Germeys, Delespaul, & Krabbendam, 2009) and CTQ (Baker & Maiorino, 2010) revealed that the data were not normally distributed. Thus, comparisons between patients and healthy volunteers were carried out using a Mann-Whitney U test. These comparisons revealed significant differences across all subscale scores and total scores on the CTQ as well as the CAPE. In all cases, the patient scores were significantly higher than the scores of the healthy volunteers. These data are also shown in Table 1.
Analyses aimed at examining the validity of self-reported symptoms as measured by the CAPE subscales in the patient sample by comparing them to scores obtained on standard clinician-administered rating scales demonstrated strong validity for the CAPE in the present sample. Specifically, we found that the CAPE negative symptom subscale significantly correlated to total SANS score (rho=.21, p<.01), the CAPE depressive symptom subscale correlated to the HRSD-17 score (rho=.63, p<.001) and the CAPE positive symptom subscale correlated to the psychotic symptom subscale derived from the BPRS (rho=.46, p<.001). The average scores obtained on each measure are shown in Table 1. The correlation matrix showing the relations among all subscales derived from the assessments are shown in Table 2. Consistent with what has long been known about the relation between depression, negative symptoms and more general measures of psychopathology (Whiteford et al., 1987), the correlations among the various subscales shown in Table 2 are not domain specific.
Table 2.
Correlations among CAPE subscales and clinician administered rating scales in stable outpatients with schizophrenia and schizoaffective disorder (N=184).
| SANS | CAPE Negative |
HRSD-17 | CAPE Depression |
BPRS Positive Subscale |
CAPE Positive |
||
|---|---|---|---|---|---|---|---|
| SANS | rho p |
0.21 <.01 |
0.32 <.001 |
0.07 NS |
0.22 <.01 |
0.04 NS |
|
| CAPE Negative | rho p |
0.60 <.001 |
0.79 <.001 |
0.16 0.03 |
0.54 <.001 |
||
| HRSD-17 | rho p |
0.63 <.001 |
0.35 <.001 |
0.45 <.001 |
|||
| CAPE Depression | rho p |
0.13 NS |
0.54 <.001 |
||||
|
BPRS Positive Subscale |
rho p |
0.46 <.001 |
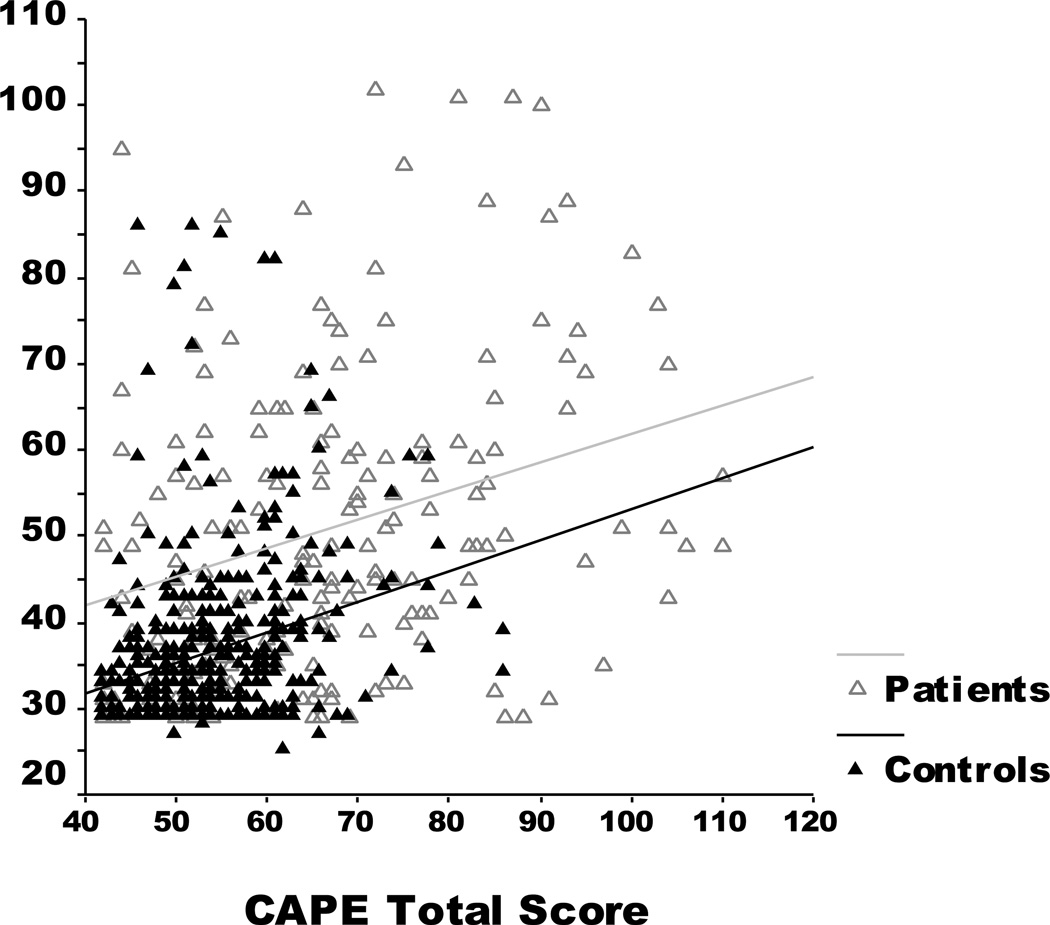
The primary analysis aimed at assessing whether the relation between overall severity of childhood maltreatment and overall severity of psychotic symptoms was similar across patient and healthy volunteers revealed strong positive correlations between the CTQ total score and CAPE total score in both patients (rho=.321, p<.001) and healthy participants (rho=.374, p<.001) and no significant difference in the slopes of the regression lines (F(1,627)=0.58, p=.45). These data are shown Figure 1. Because the patient and healthy volunteer samples differed substantially on both the distribution of males and females and racial make-up, we re-examined these relations in males and females separately and in our 3 racial groups (Black, White and Other minorities) separately. In each case, however, the relation between CTQ and CAPE scores remained significant (all rho’s >.40 and all p’s <.001). Moreover, in all cases, the slopes of the regression lines did not significantly differ (with p values ranging from .20 to .82).
Figure 1.
Relation between a history of childhood trauma as measured by the 28-item Childhood Trauma Questionnaire (CTQ) and subclinical/clinical psychotic symptoms as measured by the Community Assessment of Psychic Experiences (CAPE). For both patients and healthy volunteers, the correlation between the CTQ and CAPE were significant (patients: n=184; rho=.32, p<.001; healthy volunteers: n=447; rho=.37, p<.001) and the slopes of the regression lines were not significantly different (F(1,627)=0.58, p=.48)
The primary analysis was followed up with post hoc correlation analyses aimed at more closely examining the relations among the CAPE subscale scores and the CTQ subscale scores. Although, fewer associations were observed for the patient group relative to the group of healthy volunteers, overall, the results of these analyses indicated remarkably consistent patterns of associations across both groups. The strongest and most consistent relationships were among the CAPE subscale scores and severity of childhood emotional abuse with all p values <.001 in both patients and healthy volunteers. These results are shown in Tables 3 and 4, respectively.
Table 3.
Correlations among CTQ subscales and CAPE subscales for patients with schizophrenia and schizoaffective disorder (N=184).
| Patients with SZ or SAD | ||||||||
|---|---|---|---|---|---|---|---|---|
| Physical Abuse |
Sexual Abuse |
Emotional Neglect |
Physical Neglect |
CAPE Positive Symptoms |
CAPE Negative Symptoms |
CAPE Depressive Symptoms |
||
| Emotional Abuse |
rho p |
0.58 <.001 |
0.47 <001 |
0.52 <.001 |
0.25 <.001 |
0.32 <.001 |
0.31 <.001 |
0.37 <.001 |
| Physical Abuse |
rho p |
0.47 <001 |
0.31 <.001 |
0.33 <.001 |
0.26 <.001 |
0.06 NS |
0.07 NS |
|
| Sexual Abuse |
rho p |
0.24 <01 |
0.21 <01 |
0.25 <.001 |
0.13 NS |
0.23 <.01 |
||
| Emotional Neglect |
rho p |
0.18 0.02 |
0.08 NS |
0.16 0.03 |
0.15 0.04 |
|||
| Physical Neglect |
rho p |
0.15 0.04 |
0.08 NS |
0.13 NS |
||||
| CAPE Positive Symptoms |
rho p |
0.54 <.001 |
0.54 <.001 |
|||||
| CAPE Negative Symptoms |
rho p |
0.79 <.001 |
||||||
Table 4.
Correlations among CTQ subscales and CAPE subscales for healthy volunteers (N=447).
| Healthy Volunteers | ||||||||
|---|---|---|---|---|---|---|---|---|
| Physical Abuse |
Sexual Abuse |
Emotional Neglect |
Physical Neglect |
CAPE Positive Symptoms |
CAPE Negative Symptoms |
CAPE Depressive Symptoms |
||
| Emotional Abuse |
rho p |
0.50 <.001 |
0.25 <001 |
0.50 <.001 |
0.21 <.001 |
0.31 <.001 |
0.29 <.001 |
0.30 <.001 |
| Physical Abuse |
rho p |
0.24 <001 |
0.38 <.001 |
0.19 <.001 |
0.26 <.001 |
0.18 <.001 |
0.17 <.001 |
|
| Sexual Abuse |
rho p |
0.18 <.001 |
0.15 <01 |
0.05 NS |
0.12 0.01 |
0.18 <.001 |
||
| Emotional Neglect |
rho p |
0.15 <01 |
0.26 <.001 |
0.31 <.001 |
0.30 <.001 |
|||
| Physical Neglect |
rho p |
0.04 NS |
0.11 0.02 |
0.05 NS |
||||
| CAPE Positive Symptoms |
rho p |
0.56 <.001 |
0.47 <.001 |
|||||
| CAPE Negative Symptoms |
rho p |
0.67 <.001 |
||||||
DISCUSSION
The present data provide strong support for a relation between childhood maltreatment and subclinical psychotic symptoms in healthy adult volunteers. Moreover, these results suggest that the nature of this relationship does not differ from the relationship between a history of childhood maltreatment and clinical levels of psychotic symptoms in patients diagnosed with schizophrenia or schizoaffective disorder. Specifically, we found that while patients with schizophrenia or schizoaffective disorder reported significantly higher levels of childhood maltreatment and psychotic symptoms than the healthy volunteers, the relationship between childhood maltreatment and subclinical symptoms seen in the healthy sample was not significantly different from the relationship between childhood maltreatment and clinical levels of psychotic symptoms seen in the patient sample. This finding was consistent when males and females, and racial groups were examined separately.
Our findings indicating significantly higher levels of childhood maltreatment in the patient sample relative to the healthy volunteers, is consistent with several prior reports (Agid et al., 1999; Morgan & Fisher, 2007; Nettelbladt, Svensson, & Serin, 1996; Bendall, Jackson, Hulbert, & McGorry, 2008). Moreover, our findings are consistent with reports linking a history of childhood maltreatment to both clinical levels of psychotic symptoms in patients with schizophrenia and schizoaffective disorder (Kessler et al., 2010) and in patients with bipolar disorder (Etain et al., 2013). To our knowledge, however, this is the first report that directly compared the similarities between these relations.
Although examination of the relations between the different types of childhood maltreatment and subclinical/clinical psychotic symptoms was strikingly similar across both groups, the most notable consistency was seen for the relation between a history of childhood emotional abuse and all domains measured by the CAPE. This finding is consistent with a recent meta-analysis indicating that although all types of childhood maltreatment increased the risk for psychosis, emotional abuse was among the strongest predictor (OR=3.4) (Kessler et al., 2010). It should be noted, however, that all of the subscales derived from the CTQ were significantly positively correlated in both the patient and healthy samples. Moreover, the subscales derived from the CAPE were also significantly positively correlated in both the patient and healthy samples. This is consistent with prior data indicating strong relationships between positive, negative and depressive symptoms in both patient and healthy samples (Wigman et al., 2012). This overlap makes it difficult to draw conclusions regarding the relationship between specific forms of childhood maltreatment and specific types of subclinical/clinical psychotic symptoms.
Several limitations of the present study should be noted. The present study and all studies reporting on the effects of childhood maltreatment relied on the retrospective assessment of childhood experience. Although it could be argued that adults overreport childhood maltreatment, several studies have demonstrated that adults may under-report such experiences (Williams, 1994; Shaffer, Huston, & Egeland, 2008). Moreover, although several studies have used the CAPE for the assessment of psychotic symptoms in patient samples (Wigman et al., 2012, Varghese et al., 2011; Yung et al., 2007) and as a community screening instrument to identify at-risk individuals (Brenner et al., 2007), its use in a patient population has not been well validated. In the present study, however, we demonstrated that the subscales derived from the CAPE correlated well with standard clinician-administered rating scales that assessed the same symptom constructs.
In summary, the present data provide strong support for the continuity of the relation between childhood maltreatment and severity of subclinical psychotic symptoms observed in the general population and the severity of psychotic symptoms observed in patients with schizophrenia and schizoaffective disorder. Elucidating the mechanisms that underlie this relationship may provide insight into the pathophysiology of risk and resilience to psychotic disorders.
Acknowledgements
Role of Funding Source
Funding for this study was provided by NIMH grants MH086756 to PD; and MH079800 to AKM. The NIMH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Funding/Support: This work was supported in part by grants from the National Institute of Mental Health to Dr. DeRosse (MH086756) and Dr. Malhotra (MH079800), the NSLIJ Research Institute General Clinical Research Center (M01 RR018535), Advanced Center for Intervention and Services Research (P30 MH090590) and a Center for Intervention Development and Applied Research (P50 MH080173).
Dr. Malhotra has served as consultant or speaker for Bristol-Myers Squibb, Astra Zeneca, Vanda Pharmaceuticals and Clinical Data, Inc, and has received research support from Pfizer, Janssen Pharmaceuticals, Bristol-Myers Squibb, and Eli Lilly.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Declaration of Interests: None
Contributors
Author PD designed the study. Author BK managed the literature searches and Authors PD and GN conducted all analyses. Author AKM provided one of the study samples and assisted in the review of the manuscript. All authors contributed to and have approved the final manuscript.
Disclosures
Drs. DeRosse and Nitzburg and Mr. Kompancaril report no competing interests.
REFERENCES
- Agid O, Shapira B, Zislin J, Ritsner M, Hanin B, Murad H, Lerer B. Environment and vulnerability to major psychiatric illness: a case control study of early parental loss in major depression, bipolar disorder and schizophrenia. Mol Psychiatry. 1999;4(2):163–172. doi: 10.1038/sj.mp.4000473. [DOI] [PubMed] [Google Scholar]
- Andreasen NC. Negative symptoms in schizophrenia: definition and reliability. Arch Gen Psychiatry. 1982;39(7):784. doi: 10.1001/archpsyc.1982.04290070020005. [DOI] [PubMed] [Google Scholar]
- Arseneault L, Cannon M, Fisher HL, Polanczyk G, Moffitt TE, Caspi A. Childhood trauma and children’s emerging psychotic symptoms: a genetically sensitive longitudinal cohort study. Am J Psychiatry. 2011;168(1):65. doi: 10.1176/appi.ajp.2010.10040567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker AJ, Maiorino E. Assessments of emotional abuse and neglect with the CTQ: Issues and estimates. Child Youth Serv Rev. 2010;32(5):740–748. [Google Scholar]
- Bendall S, Jackson HJ, Hulbert CA, McGorry PD. Childhood trauma and psychotic disorders: a systematic, critical review of the evidence. Schizophr Bull. 2008;34(3):568–579. doi: 10.1093/schbul/sbm121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Zule W. Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abuse Negl. 2003;27(2):169–190. doi: 10.1016/s0145-2134(02)00541-0. [DOI] [PubMed] [Google Scholar]
- Brenner K, Schmitz N, Pawliuk N, Fathalli F, Joober R, Ciampi A, King S. Validation of the English and French versions of the Community Assessment of Psychic Experiences (CAPE) with a Montreal community sample. Schizophr Res. 2007;95(1):86–95. doi: 10.1016/j.schres.2007.06.017. [DOI] [PubMed] [Google Scholar]
- Etain B, Aas M, Andreassen AO, Lorentzen S, Dieset I, Gard S, Kahn JP, Bellivier F, Leboyer M, Melle I, Henry C. Childhood trauma is associated with severe clinical characteristics of bipolar disorders. J Clin Psychiatry. 2013;74(10):991–998. doi: 10.4088/JCP.13m08353. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV axis I disorders, research version, non-patient edition. New York: Biometrics Research, New York State Psychiatric Institute; 2002a. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV-TR axis I disorders, research version, patient edition. New York: Biometrics Research, New York State Psychiatric Institute; 2002b. [Google Scholar]
- Garety PA, Rigg A. Early psychosis in the inner city: a survey to inform service planning. Soc Psychiatry Psychiatr Epidemiol. 2001;36(11):537–544. doi: 10.1007/s001270170004. [DOI] [PubMed] [Google Scholar]
- Gilbert R, Widom C, Browne K, Fergusson D, Webb E, Janson S. Burden and consequences of child maltreatment in high-income countries. Lancet. 2009;373(9657):68–81. doi: 10.1016/S0140-6736(08)61706-7. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatr. 1960;23(1):56. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heins M, Simons C, Lataster T, Pfeifer S, Versmissen D, Lardinois M, Myin-Germeys I. Childhood trauma and psychosis: a case-control and case-sibling comparison across different levels of genetic liability, psychopathology, and type of trauma. Am J Psychiatry. 2011;168(12):1286–1294. doi: 10.1176/appi.ajp.2011.10101531. [DOI] [PubMed] [Google Scholar]
- Janssen I, Krabbendam L, Bak M, Hanssen M, Vollebergh W, Graaf RD, Os JV. Childhood abuse as a risk factor for psychotic experiences. Acta Psychiatr Scand. 2004;109(1):38–45. doi: 10.1046/j.0001-690x.2003.00217.x. [DOI] [PubMed] [Google Scholar]
- Kelleher I, Keeley H, Corcoran P, Ramsay H, Wasserman C, Carli V, Cannon M. Childhood trauma and psychosis in a prospective cohort study: cause, effect, and directionality. Am J Psychiatry. 2013 doi: 10.1176/appi.ajp.2012.12091169. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Williams DR. Childhood adversities and adult psychopathology in the WHO World Mental Health Surveys. Br J Psychiatry. 2010;197(5):378–385. doi: 10.1192/bjp.bp.110.080499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linscott RJ, Van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. 2012;1(1):1–17. doi: 10.1017/S0033291712001626. [DOI] [PubMed] [Google Scholar]
- Morgan C, Fisher H. Environment and schizophrenia: environmental factors in schizophrenia: childhood trauma—a critical review. Schizophr Bull. 2007;33(1):3–10. doi: 10.1093/schbul/sbl053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLaughlin KA, Green JG, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication II: associations with persistence of DSM-IV disorders. Arch Gen Psychiatry. 2010;67(2):124. doi: 10.1001/archgenpsychiatry.2009.187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nettelbladt P, Svensson C, Serin U. Background factors in patients with schizoaffective disorder as compared with patients with diabetes and healthy individuals. Eur Arch Psychiatry Clin Neurosci. 1996;246(4):213–218. doi: 10.1007/BF02188956. [DOI] [PubMed] [Google Scholar]
- Overall JE, Gorham DR. The brief psychiatric rating scale. Psychol Rep. 1962;10(3):799–812. [Google Scholar]
- Read J, Perry BD, Moskowitz A, Connolly J. The contribution of early traumatic events to schizophrenia in some patients: a traumagenic neurodevelopmental model. Psychiatry. 2001;64(4):319–345. doi: 10.1521/psyc.64.4.319.18602. [DOI] [PubMed] [Google Scholar]
- Shaffer A, Huston L, Egeland B. Identification of child maltreatment using prospective and self-report methodologies: A comparison of maltreatment incidence and relation to later psychopathology. Child Abuse Negl. 2008;32(7):682–692. doi: 10.1016/j.chiabu.2007.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stefanis NC, Hanssen M, Smirnis NK, Avramopoulos DA, Evdokimidis IK, Stefanis CN, Van Os J. Evidence that three dimensions of psychosis have a distribution in the general population. Psychol Med. 2002;32(2):347–358. doi: 10.1017/s0033291701005141. [DOI] [PubMed] [Google Scholar]
- Van Os J, Hanssen M, Bijl RV, Ravelli A. Strauss (1969) revisited: a psychosis continuum in the general population? Schizophr Res. 2000;45(1):11–20. doi: 10.1016/s0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- Van Os J, Hanssen M, Bijl RV, Vollebergh W. Prevalence of psychotic disorder and community level of psychotic symptoms: an urban-rural comparison. Arch Gen Psychiatry. 2001;58(7):663. doi: 10.1001/archpsyc.58.7.663. [DOI] [PubMed] [Google Scholar]
- Van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179. doi: 10.1017/S0033291708003814. [DOI] [PubMed] [Google Scholar]
- Van Os J, Linscott RJ. Introduction: the extended psychosis phenotype— relationship with schizophrenia and with ultra high risk status for psychosis. Schizophr Bull. 2012;38(2):227–230. doi: 10.1093/schbul/sbr188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Bentall RP. Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophr Bull. 2012;38(4):661–671. doi: 10.1093/schbul/sbs050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varghese D, Scott J, Welham J, Bor W, Najman J, O'Callaghan M, McGrath J. Psychotic-like experiences in major depression and anxiety disorders: a population-based survey in young adults. Schizophr Bull. 2011;37(2):389–393. doi: 10.1093/schbul/sbp083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdoux H, Van Os J, Maurice-Tison S, Gay B, Salamon R, Bourgeois M. Is early adulthood a critical developmental stage for psychosis proneness? A survey of delusional ideation in normal subjects.Schizophr Res. 1998;29(3):247–254. doi: 10.1016/s0920-9964(97)00095-9. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Riney SJ, Csernansky JG. Distinguishing Depressive and Negative Symptoms in Chronic Schizophrenia. Psychopathology. 1987;20:234–236. doi: 10.1159/000284506. [DOI] [PubMed] [Google Scholar]
- Wigman JT, van Nierop M, Vollebergh WA, Lieb R, Beesdo-Baum K, Wittchen HU, van Os J. Evidence That Psychotic Symptoms Are Prevalent in Disorders of Anxiety and Depression, Impacting on Illness Onset, Risk, and Severity—Implications for Diagnosis and Ultra–High Risk Research. Schizophr Bull. 2012;38(2):247–257. doi: 10.1093/schbul/sbr196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams LM. Recall of childhood trauma: a prospective study of women's memories of child sexual abuse. J Consult Clin Psychol. 1994;62(6):1167. doi: 10.1037//0022-006x.62.6.1167. [DOI] [PubMed] [Google Scholar]
- Yung AR, Buckby JA, Cosgrave EM, Killackey EJ, Baker K, Cotton SM, McGorry PD. Association between psychotic experiences and depression in a clinical sample over 6 months. Schizophr Res. 2007;91(1):246–253. doi: 10.1016/j.schres.2006.11.026. [DOI] [PubMed] [Google Scholar]