Abstract
Background:
Prelacteal feeding is an underestimated problem in a developing country like India, where infant mortality rate is quite high. The present study tried to find out the factors determining prelacteal feeding in rural areas of north India.
Methods:
A crosssectional study was conducted among recently delivered women of rural Uttar Pradesh, India. Multistage random sampling was used for selecting villages. From them, 352 recently delivered women were selected as the subjects, following systematic random sampling. Chi-square test and logistic regression were used to find out the predictors for prelacteal feeding.
Results:
Overall, 40.1% of mothers gave prelacteal feeding to their newborn. Factors significantly associated with such practice, after simple logistic regression, were age, caste, socioeconomic status, and place of delivery. At multivariate level, age (odds ratio (OR) = 1.76, 95% confidence interval (CI) = 1.13-2.74), caste and place of delivery (OR = 2.23, 95% CI = 1.21-4.10) were found to determine prelacteal feeding significantly, indicating that young age, high caste, and home deliveries could affect the practice positively.
Conclusions:
The problem of prelacteal feeding is still prevalent in rural India. Age, caste, and place of delivery were associated with the problem. For ensuring neonatal health, the problem should be addressed with due gravity, with emphasis on exclusive breast feeding.
Keywords: Breast feeding, colostrum, infant feeding, prelacteal feeding, rural India
INTRODUCTION
Breast feeding is the primary step toward ensuring optimal health and development of the children. Colostrum, the early breast milk, plays a vital role in boosting immunity of a newborn. Apart from providing fat soluble vitamins, it also primes gastrointestinal tract.[1,2] Breast milk plays a protective role against a number of diseases including insulin-dependent diabetes mellitus, obesity, eczema, and childhood leukemias.[3] The bond it builds between the mother and the child paves way for the most precious relationship on the earth.
But, unfortunately, the habit of prelacteal feeding is common in our society due to different customs and misbelieves. It not only leads to discarding of colostrum, but might deny the success of breast feeding and paves way for infections.[4,5] With delay in initiation of breast feeding, a marked increase in neonatal mortality has been reported earlier from different parts of the world.[6]
To address the problem, the concept of baby friendly hospital initiative (BFHI) was launched globally in 1991 by UNICEF and WHO for promoting and supporting breast feeding.[7] In past 20 years, many hospitals have been designated from different countries including India. Still, available literatures from India depict a poor picture of widely practiced prelacteal feeding to the newborn in the country, in spite of its detrimental effect on health of the neonate. Researches from other parts of south-east Asia also reflect the same. The maternal perception of delayed arrival of milk, coupled with cultural customs, has made it a universal habit across the subcontinent.[8,9,10,11,12] In this background, the present study aimed to find out the extent of prelacteal feeding in rural area of Uttar Pradesh, a backward state in north India.
METHODS
This crosssectional study was conducted among recently delivered women (RDWs) of rural Lucknow from August 2009 to July 2010. Rural Lucknow, with a population of 1,326,873 (36% of the district), is having a literacy rate of 52.3% among the females.[13,14] Scheduled caste/tribes are the most populous section in the area. They, in general, form the bottom line in caste-based society and economically most challenged.
A RDW was defined as a postnatal woman, who had delivered a baby during the period from January 2009 to June 2010. Prelacteal feeding was defined as any food other than breast milk given to the newborn after birth before initiating breast feeding. Data were collected as a part of a larger study which addresses the whole spectrum of pregnancy, its outcome as well as newborn care. A total of 352 RDWs were covered from 32 villages.
Sampling technique
Multistage random sampling was used for selecting subcenters (SCs). In the first stage, out of nine community health centers (CHCs) in Lucknow, two were chosen randomly. From each of them, two primary health centers (PHCs) were selected in the second stage. From each PHC, four SCs were taken. From each of the SC, two villages were selected; one being SCvillage and other as non-SC villages. Thus, the study covered 32 villages.
From every village, list of RDWs was retrieved from accredited social health activists (ASHAs) and anganwadi workers, two baseline health workers at the rural community level. Systematic random sampling was followed to pick up the required number of beneficiaries.
The criterion for inclusion was a RDW present in the villages under study on the day of survey. The guests were excluded. Those who refused for interview were excluded.
Tools of data collection
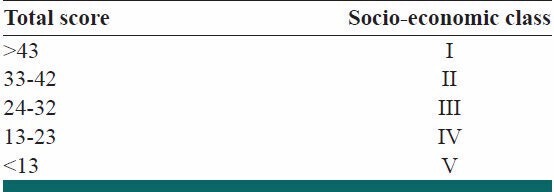
The study was conducted after getting clearance from the Institutional Ethical Committee of the university and permission from the superintendents of the concerned CHCs. Before interview, verbal consent was obtained from the RDWs. A structured interview schedule was used to collect required information. After pretesting, necessary modifications were done for bringing clarity. For calculating socioeconomic status (SES), modified Pareek's classification for rural area was used [Tables 1 and 2].[15] The main outcome variable was practice of prelacteal feeding. Among different independent variables, age, religion, caste, education, SES, family type, parity, and place of delivery were included.
Table 1.
Modified Pareek's socio-economic scale for rural area
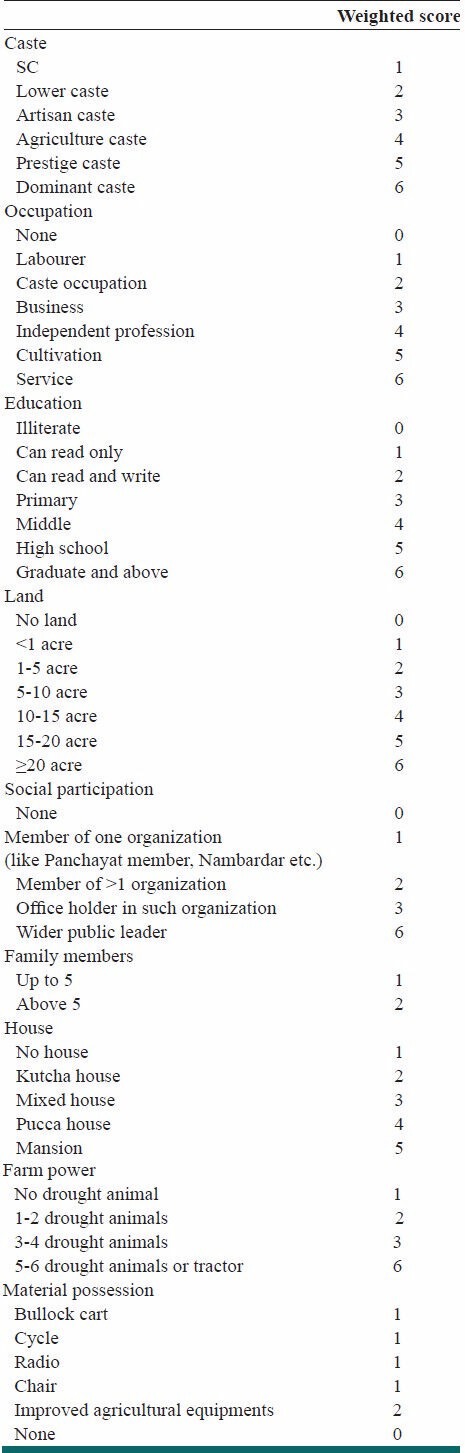
Table 2.
Socio-economic class
Statistical analysis
Data entry and analysis were done using Predictive Analytics Software for Windows software (Version 19.0; SPSS Inc, Chicago). Frequency and percentage for categorical variables were calculated. The Chi-square test was used to compare the RDWs who had given prelacteal feeding to their children and who had not. A P value of less than 0.05 was considered statistically significant. Simple and multiple logistic regressions were used to find out crude and adjusted odd's ratios (OR) and 95% confidence interval (CI) for factors associated with practice of giving prelacteal feed. Independent variables that were significant at univariate level were included in multivariate model for avoiding confounding. Backward logistic model, based on likelihood ratio, was used to find predictors for prelacteal feeding. The fit of final model was assessed using Hosmer-Lemeshow goodness-of-fit test.
RESULTS
More than half (54.5%) of the RDWs were above the age of 25 years. Most of them (91.2%) were Hindu and illiterate/educated till primary standard (63.6%). Considering SES, 25.9% belonged to class V. About 84.9% of the women had delivered at health facilities. Overall, 40.1% mothers gave prelacteal feeding to their children.
The comparison between the profiles of the mothers who had given prelacteal feeding to their children and who had not revealed significant difference in terms of age, caste, SES, and place of delivery. The influence of religion, parity, education, or family type was not prominent. (applying Chi-square, table not given)
On simple logistic regression, significant relation was found between practice of prelacteal feeding and age (OR = 1.68, 95% CI = 1.10-2.59), caste and SES (OR = 1.72, 95% CI = 1.03-2.86). Young RDWs, those belonging to higher castes or SES and who had home deliveries were found to be more likely to adopt the practice of prelacteal feeding for their children. No interaction was seen with other sociodemographic factors such as religion, parity, education, or family type of the RDWs. Overall, women who delivered at home were found to have two-fold increased risk for prelacteal feeding (OR = 2.02, 95% CI = 1.12-3.64) [Table 3].
Table 3.
Factors associated with prelacteal feeding by the mothers on simple and multiple logistic regressions
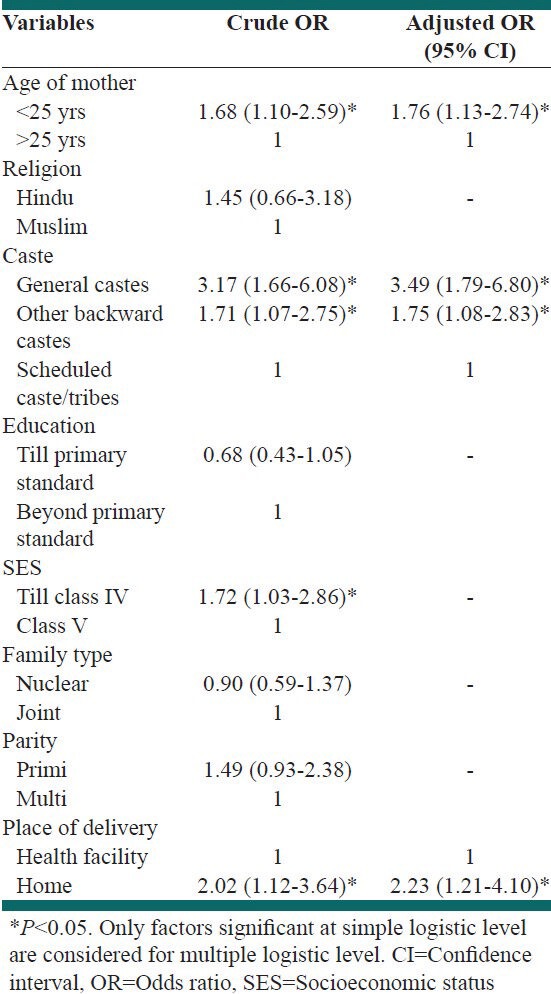
At multivariate level, age (OR = 1.76, 95% CI = 1.13-2.74), caste, and place of delivery (OR = 2.23, 95% CI = 1.21-4.10) were significant, indicating that young age, higher caste, and home deliveries could affect prelacteal feeding positively [Table 3]. The result of Hosmer-Lemeshow goodness-of-fit test was not significant (P = 0.646, df = 5). Overall, correct classification result indicated that 62.8% of the RDWs are predicted rightly about their behavior regarding prelacteal feeding.
DISCUSSION
The present descriptive study tried to find out the determinants for prelacteal feeding, a custom still widely practiced in rural India. The analysis points out that some sociodemographic factors exert important influences on the practice of prelacteal feeding.
The prevalence found was similar to some previous studies.[9,11,16,17,18,19] The magnitude is less in the study area than rural UP as well as rural India.[20,21] Considering the fact that 5 years of National Rural Health Mission have been passed with introduction of ASHA at village level, this difference might be counted as the success of the mission. ASHAs act as a bridge between health care delivery system and motivate the villagers to change their health-related practices. The impact of intervention into rural life with the aid of ASHA is substantial, acceptability being a vital issue. With proper strategy, this could succeed in bringing a long-term change in the newborn health at the village level. The current and potential role ASHA could play in breast feeding promotion need to be explored.
No apparent effect of religion, family type, education of mother, and parity was evident from the present study on the practice of prelacteal feeding. This is similar to a previous study which could not find any effect of parity or family type on the same.[9] Among other factors, caste has earlier been found to influence the practice. Similar to the present study, higher prevalence among other backward classes was also prominent from the national data.[21] It was a surprise to see that higher castes practice such habit more than scheduled caste/tribes, the lowest strata in social hierarchy. But, one thing still remains very common that is caste-wise disparity in access to knowledge and health practices.
The tendency of the young mothers for prelacteal feeding is another concern. Wide availability of infant formula over the counter as well as at the general market is the underpinning factor in this regard. With such alternate at hand, the thought that initial less secretion of breast milk is not enough for the newborn might have influenced their decision. Moreover, they are easily convinced by the elderly members of the society, often considered as the carrier for traditional practices. Modernization in breast feeding practices coupled with sociobehavioral factors may pose a challenge in implementing universal practice of “no prelacteal feeding”. The health care providers should focus on this vulnerable group in particular by health education and community involvement.
In contrast to other studies which saw high prevalence of prelacteal feed among poor section, the present study found that the extent of prelacteal feeding increases with better socioeconomic condition.[20,21] However, after controlling for other variables, the effect was not significant. A study from Jammu and Kashmir supports this view.[10] It may happen that well to do families have easy access to traditional alternates which indirectly influences their choice of prelacteal feeding. Whatever might be the underlying cause, RDWs should be sensitized about the benefits of colostrum feeding as well as drawbacks of prelacteal feeding to the newborn.
It is evident from our study that education has an important role in deciding the behavior of the RDW with regard to prelacteal feeding, though not significant. The pattern is in sharp contrast to previous finding that usually puts education as a factor for reducing such feeding.[11,21,22] In fact, this is a practice governed not only by education but interplay of several other factors. This may be the reason for apparent association between literacy and prelacteal feeding. However, a study from Honduras also found the same tendency among literate mothers.[5]
Higher rate of prelacteal feeding was also seen among mothers who delivered at home. The finding is supported by previous studies.[17,20,21,22] This group of mothers could be considered as those who, in general, lack not only touch with health workers as well as knowledge of newborn care. Less awareness coupled with negligence might have rendered these RDWs more vulnerable to ill care of the children.
Overall, the results indicate that age of the mother, caste, and place of delivery can influence the practice of giving prelacteal feeding to the newborn. They provide epidemiological evidence which can be utilized to find out high-risk groups for such feeding in rural settings. Keeping our commitment toward ensuring universal practice of breast feeding, this has vital implication for policy makers. Misconception prevailing in the society should also be dealt with utmost importance. The role of health workers in this regard needs to be emphasized. Earlier studies have proved that advices given by health worker for not feeding something prelacteal has substantial effect on maternal behavior.[23,24]
The present study has few limitations. The reasons for giving prelacteal feed and foods preferred were not collected. Collected data being recall-based, bias is also not an unexpected loophole here. Third, women who experience delayed arrival of milk for biological cause are more prone to give prelacteal feed.[5] This variable was not considered in the study. In spite of these methodological drawbacks, our study allows us to generate a model for predicting the behavior of the mother regarding prelacteal feeding. As data were collected by a single author, consistent technique and interpretation of the answers are the advantages of this study. Adequate sample size, systematic way of selecting representative sample, and community-based approach are some of the other strengths. The existence of limited such efforts to determine sociodemographic factors responsible for prelacteal feeding is another credit to this study. Future longitudinal studies addressing the same would be useful in this regard.
CONCLUSIONS
It can be said that the problem of prelacteal feeding is still prevalent in rural northern India. It is fact that traditional practices like prelacteal feeding will take time to be changed. The introduction of BFHI might have boosted the acceptance of exclusive breast feeding, but a long way is yet to be covered. The use of participatory health promotion techniques, such as women's groups, may prove successful at reducing this harmful practice. Message for changing behavior should be based on an understanding of traditional believes, if we want to convert it in practice. Presence of exclusive breast feeding support group in community would be another way. Religious leaders might be involved to promote the concept of feeding colostum and not anything prelacteal. Every effort should be made through community-based strategies and supportive intervention to discourage the use of pre-lacteal feeds and promote breastfeeding practices.
ACKNOWLEDGMENTS
The work has been attributed to the Upgraded Department of Community Medicine and Public Health, CSM Medical University UP, Lucknow, India.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Stephensen CB. Vitamin A, infection, and immune function. Annu Rev Nutr. 2001;21:167–92. doi: 10.1146/annurev.nutr.21.1.167. [DOI] [PubMed] [Google Scholar]
- 2.Goldman AS. Modulation of the gastrointestinal tract of infants by human milk. Interfaces and interactions. An evolutionary perspective. J Nutr. 2000;130(Suppl 2S):426S–31S. doi: 10.1093/jn/130.2.426S. [DOI] [PubMed] [Google Scholar]
- 3.Meyers D. Breastfeeding and health outcomes. Breastfeed Med. 2009;4(Suppl 1):S13–5. doi: 10.1089/bfm.2009.0066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ludvigsson JF. Breastfeeding intentions, patterns, and determinants in infants visiting hospitals in La Paz, Bolivia. BMC Pediatr. 2003;3:5. doi: 10.1186/1471-2431-3-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Perez-Escamilla R, Segura-Millan S, Canahuati J, Allen H. Prelacteal feeds are negatively associated with breast feeding outcomes in Honduras. J Nutr. 1996;126:2765–73. doi: 10.1093/jn/126.11.2765. [DOI] [PubMed] [Google Scholar]
- 6.Edmond KM, Kirkwood BR, Amenga-Etego S, Owusu-Agyei S, Hurt LS. Effect of early infant feeding practices on infection-specific neonatal mortality: An investigation of the causal links with observational data from rural Ghana. Am J Clin Nutr. 2007;86:1126–31. doi: 10.1093/ajcn/86.4.1126. [DOI] [PubMed] [Google Scholar]
- 7.Saadeh R. Global overview of the WHO/UNICEF Baby-Friendly Hospital Initiative International Child Health. 1996;7:31–3. [Google Scholar]
- 8.Madhu K, Chowdary S, Masthi R. Breast feeding practices and newborn care in rural areas: A descriptive cross-sectional study. Indian J Community Med. 2009;34:243–6. doi: 10.4103/0970-0218.55292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kishore S, Garg BS. Practice of prelacteal feeding in a rural community. Indian J Public Health. 1999;43:144–7. [PubMed] [Google Scholar]
- 10.Raina SK, Mengi V, Singh G. Determinants of pre lacteal feeding among infants of RS Pura Block of Jammu and Kashmir. India J Fam Med Primary Care. 2012;1:27–9. doi: 10.4103/2249-4863.94446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Haque MJ, Rahman MM, Sarker SK, Ali MA, Fakir M, Rahman MM, et al. Infant feeding practice by the rural mothers of Dinajpur district. Dinajpur Med Col J. 2010;3:35–8. [Google Scholar]
- 12.Iqbal SMJ, Afzal MF, Azhar IH, Sultan MS. First feed in newborn: Are we following WHO recommendations? Annals. 2010;16:229–32. [Google Scholar]
- 13.Census of India. 2001. [Last accessed on 2012 July 13]. Available from: http://censusindia.gov.in/PopulationFinder/District_Master.aspx?state_code=09 .
- 14.Uttar Pradesh, Lucknow: Ministry of Health and Family Welfare, Government of India, Mumbai; Government of India and International Institute for Population Science. District Level Household and Facility Survey (DLHS) 3, 2007.08. District Fact Sheet. [Google Scholar]
- 15.New Delhi: NIHFW; 2003. National Institute of Health and Family Welfare. Survey instruments for collection of information from house hold developed by NIHFW for collaborative activity of the National consortium of public health. [Google Scholar]
- 16.Gupta A, Gupta YP. Breast Feeding Promoting Network of India; 2003. Status of infant and young child feeding in 49 districts of India: A national report of quantitative study. [Google Scholar]
- 17.Kumar D, Agarwal N, Swami HM. Socio demographic correlates of breast-feeding in urban slums of Chandigarh. Indian J Med Sci. 2006;60:461–6. [PubMed] [Google Scholar]
- 18.Wadde SK, Vedpathak VL, Yadav VB. Breast feeding practices in rural mothers of Maharashtra. Int J Recent Trends Sci Tech. 2011;1:115–9. [Google Scholar]
- 19.Chaudhary RN, Shah T, Raja S. Knowledge and practice of mothers regarding breast feeding: A hospital based study. Health Renaissance. 2011;9:194–200. [Google Scholar]
- 20.Mumbai: IIPS; International Institute for Population Sciences (IIPS) and Macro International. 2008. National Family Health Survey (NFHS-3), India, 2005-06: Uttar Pradesh. [Google Scholar]
- 21.Mumbai: IIPS; 2007. International Institute for Population Sciences (IIPS) and Macro International, National Family Health Survey (NFHS-3), 2005-06: India: Volume I. [Google Scholar]
- 22.Raval D, Jankar DV, Singh MP. A study of breast feeding practices among infants living in slums of Bhavnagar city, Gujarat, India. Healthline. 2011;2:78–83. [Google Scholar]
- 23.Akuse RM, Obinya EA. Why health care workers give prelacteal feeds. Eur J Clin Nutr. 2002;56:729–34. doi: 10.1038/sj.ejcn.1601385. [DOI] [PubMed] [Google Scholar]
- 24.Okolo SN, Adewunmi YB, Okonji MC. Current breastfeeding knowledge, attitude, and practices of mothers in five rural communities in the Savannah region of Nigeria. J Trop Pediatr. 1999;45:323–6. doi: 10.1093/tropej/45.6.323. [DOI] [PubMed] [Google Scholar]


