Abstract
OBJECTIVE:
The goal of the present study was to compare the prognoses of patients with non-ST-elevation acute coronary syndromes who were treated with invasive or conservative treatment strategies.
METHODS:
We performed a meta-analysis of studies of patients with non-ST-elevation acute coronary syndromes to assess the benefits of an invasive strategy vs. a conservative strategy for short- and long-term survival. We searched PubMed for studies published from 1990 to November 2012 that investigated the effects of an invasive vs. conservative strategy in patients with non-ST-elevation acute coronary syndromes. The following search terms were used: “non-ST-elevation myocardial infarction”, “unstable angina”, “acute coronary syndromes”, “invasive strategy”, and “conservative strategy”. The primary endpoints were all-cause mortality at 30 days and 1 year.
RESULTS:
Seven published studies were included in the present meta-analysis. The pooled analyses show that an invasive strategy decreased the risk of death (risk ratio [0.839] [95% confidence interval {0.648-1.086}; I2, 86.46%] compared to a conservative strategy over a 30-day-period. Furthermore, invasive treatment also decreased patient mortality (risk ratio [0.276] [95% confidence interval {0.259-0.294}; I2, 94.58%]) compared to a conservative strategy for one year.
CONCLUSION:
In non-ST-elevation acute coronary syndromes, an invasive strategy is comparable to a conservative strategy for decreasing short- and long-term mortality rates.
Keywords: Non-ST-elevation Acute Coronary Syndrome, Invasive Strategy, Conservative Strategy, Meta-analysis, Mortality
INTRODUCTION
Non-ST-elevation acute coronary syndrome (NSTE-ACS) includes non-ST-elevation myocardial infarction (NSTEMI) and unstable angina (UA), which accounted for more than two thirds of all cases of acute coronary syndrome (ACS) in the United States in 2009 (1). Furthermore, cardiovascular disease, including NSTE-ACS, still remains the leading cause of mortality worldwide (2). NSTE-ACS represents an increasingly frequent cause of hospital admission, as it is the most frequent presentation of coronary instability in patients with prior cardiac events or coronary revascularizations (3). Compared with ST-elevation myocardial infarction (STEMI), NSTE-ACS is usually associated with a partial or transient coronary obstruction that results in a temporary reduction in coronary blood flow, and microemboli have also been implicated in the pathophysiology of NSTE-ACS (4). Recognizing the difference between NSTE-ACS and STEMI is critical when developing therapeutic strategies for NSTE-ACS. For instance, thrombolytic management is not indicated in NSTE-ACS management (5). Experimental data from randomized clinical trials have clearly demonstrated the efficacy of conservative or invasive approaches in the above mentioned patients (6-8). In clinical practice, physicians caring for NSTE-ACS patients are faced with immediate decisions about substantially different therapeutic strategies that may significantly affect short- and long-term outcomes (9).
An increasing number of studies havedemonstrated that an invasive treatment strategy rather than a conservative approach improves the outcomes of NSTE-ACS patients (6-8,10-16). However, some studies have shown that a conservative strategy provides the same benefit as an invasive strategy for NSTE-ACS patients, and clearly shown that the efficacy of invasive treatment was not definite (17,18).
According to the 2012 American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines (19), medical therapy remains a cornerstone in managing patients with NSTE-ACS, and we found that in the above mentioned studies that demonstrated the benefit of an invasive strategy, the administration of antithrombotics (antiplatelets or oral anticoagulants) statins was the primary step prior to interventional therapy. However, in the conservative treatment group, the NSTE-ACS patients also received interventional therapy during the index hospitalization when medical therapy failed or if substantial residual ischemia was documented in some of the randomized control trials (RCTs) (6,8,9,18,20,21).
It is necessary to clearly distinguish between the different efficacies for invasive and conservative strategies for NSTE-ACS patients. Therefore, we performed the present meta-analysis to analyze the benefits between invasive and conservative strategies for NSTE-ACS patients.
METHODS
We followed the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) guidelines (22) for randomized clinical trials and the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines (23) for observational cohort studies in the present meta-analysis.
Study search strategy
Accessing the PubMed database, we conducted a literature search for research papers published from 1990 to November 2012. The following search terms and keywords were used: “non-ST-elevation myocardial infarction”, “unstable angina”, “acute coronary syndromes”, “invasive strategy”, and “conservative strategy”. In addition, we also manually checked the reference list of each article. The main focus of the study was RCTs and observational cohort studies (OCS). We excluded those research papers with the following keywords: “review”, “review literature”, “review of reported cases”, “review, academic”, “review, multicase”, “review, tutorial”, “case reports”, “congresses”, “interview”, “overall”, “comment”, “letter”, “practice guideline”, “scientific integrity review”, “news”, “newspaper article”, and “address”. The search was limited by the search words of “>19 years”, “Publication Date from 1990/01/01 to 2012/11/01”, “English”, and “Human”.
Study Selection
Eligible patients had experienced NSTE-ACS (i.e., NSTEMI or UA) that was treated with invasive or conservative treatment during the admission. The NSTE-ACS diagnosis was based on the American College of Cardiology Foundation/American Heart Association (ACCF/AHA) Guidelines 2012 for NSTE-ACS (19). In our present meta-analysis, the invasive group contained patients who underwent cardiac catheterization, diagnostic angiography, coronary artery bypass graft (CABG) surgery, and intra-aortic balloon pump (IABP) performed during the index hospitalization with or without revascularization; the conservative group contained patients who did not undergo catheterization, angiography, CABG, or IABP during the index hospitalization. Conservative therapy consists of vigorous anti-ischemic therapy with nitrates, statins, β-blockers, and (sometimes) calcium channel blockers, as well as antithrombotic therapy with aspirin, clopidogrel, or ticagrelor, and low molecular weight heparin (LMWH) while the patients are in the hospital. In ACS patients, antithrombotics can effectively inhibit thrombus formation and coagulation, and stains can play important roles in stabilizing plaque, inhibiting vascular endothelial inflammation, improving endothelial function, and reducing cholesterol levels. The main endpoints were death from all causes at 30 days and 1 year. Patients who received both conservative and interventional therapy in the hospital were excluded.
We originally planned to perform the meta-analysis in two parts: RCTs and OCS analyzed in two separate meta-analyses; however, there was only one RCT included in the present work (17). For this reason, we retrospectively analyzed all included studies at two different time points (30 days and 1 year) by meta-analysis.
Data Extraction
In addition to information about the study design, characteristics, and sample size, we extracted the following data from the research papers: the actual number of survivors and non-survivors and corresponding cohort sizes. The main outcome variables were 30-day and 1-year survival rates.
Statistical Analysis
We performed the meta-analysis using Comprehensive Meta-analysis software, version 2.2.064 (Biostat, Englewood, NJ, USA). Risk ratios (RR) and 95% confidence intervals (95% CI) were calculated for each study and pooled with a random effects model because the heterogeneity of all meta-analyses could not be ignored, as indicated by an I2 statistics above 50% and a p<0.10. Heterogeneity among studies was formally assessed by the Q and I2 statistics. Publication bias was assessed by calculating the fail-safe number (Nfs) (24) according to the formula Nfs.05 = (ΣZ/1.645)2-N. A fail-safe number indicates the number of non-significant, unpublished studies that would need to be added to a meta-analysis to reduce the overall statistically significant results to non-significance. If the number is large relative to the number of observed studies, the summary conclusions are fairly reliable. All analyses were performed using the SPSS 17.0 software package (SPSS, Inc., Chicago, IL, USA), and p-values<0.05 were considered to be statistically significant.
RESULTS
Seven studies were included in the meta-analysis; one study was an RCT, and the other six were OCS; the total number of patients in all seven studies was 61,652 (11-17) (Figure 1) (Table 1).
Figure 1.
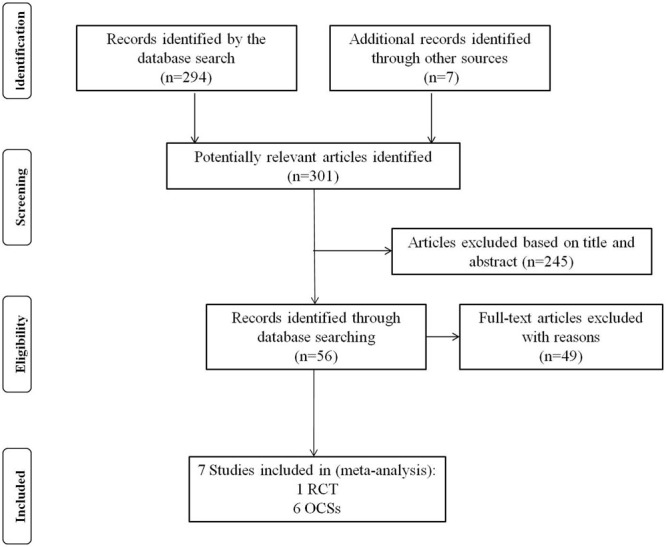
Study selection process for the studies included in the Meta-Analysis (based on the PRIMA guidelines).
Table 1.
Characteristics of the included NSTE-ACS studies.
| Sources | Study Design | Number of Deaths/Patients who Underwent Invasive Treatment for 30 days | Number of Deaths/Patients who Underwent Conservative Treatment for 30 days | Number of Deaths/Patients who Underwent Invasive Treatment for 1 year | Number of Deaths/Patients who Underwent Conservative Treatment for 1 year |
| OCS | |||||
| Leslie et al., (11) 2003*△ | Retrospective | 100/4535 | 97/3362 | 181/4535 | 309/3362 |
| Timm et al., (12) 2007△ | Prospective | 101/945 | 227/815 | ||
| Cindy et al., (13) 2008△ | Prospective | 55/1382 | 82/754 | ||
| Rogério et al., (14) 2009*△ | Prospective | 1/386 | 13/334 | 16/386 | 46/334 |
| Kouraki et al., (15) 2011△ | Prospective | 98/1215 | 185/771 | ||
| Joakim et al., (16) 2011△ | Prospective | 814/28112 | 2381/18343 | ||
| RCTs | |||||
| William et al., (17) 1998*△ | RCT | 33/442 | 7/256 | 52/442 | 24/256 |
NSTE-ACS: non-ST-elevation acute coronary syndrome; RCT: randomized controlled trials. * Included in the meta-analysis of all-cause mortality within 30 days for patients with NSTE-ACS. △ The seven studies included in the meta-analysis of all-cause mortality within 1 year for NSTE-ACS patients.
There were three studies in the first meta-analysis (11,14,17); we used all-cause mortality at 30 days as the primary endpoint, and 9,315 patients were included in the systematic review. After the data were analyzed, we found that an invasive strategy was associated with a statistically significant 15.6% decreased mortality (RR, 0.839 [95% CI, 0.648-1.086]) compared to conservative strategy during the 30 days after hospital discharge (Figure 2). In this meta-analysis, we used a random-effects model to consider the effect of heterogeneity among the studies (Q = 14.77, p = 0.001, I2 = 86.46%). The calculation for the Nfs.05 is 20.97, which suggests that there need to be 21 studies with a negative conclusion to reverse the conclusion. The conclusion from this meta-analysis is convincing, with little risk of publication bias.
Figure 2.
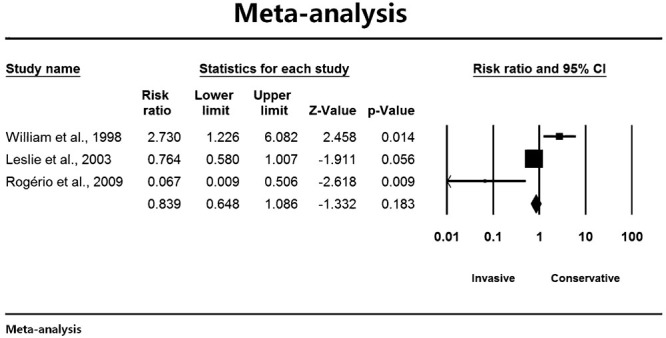
Primary analysis of the OCS in NSTE-ACS within 30 days.
In the next systematic review, the seven studies were included in the meta-analysis. We compared the mortality of patients treated with an invasive strategy and a conservative strategy for one year after hospital discharge. Of the 37,017 patients with NSTE-ACS who received invasive treatments and were discharged, there were 1,317 patients who died within one year. However, 24,635 patients received conservative treatment and were discharged and 3,254 patients died within one year. After the data were pooled, we found that invasive therapy significantly reduced mortality by 73.1% within one year after discharge (RR, 0.276 [95% CI, 0.259-0.294]) compared to conservative therapy (Figure 3). In the second meta-analysis, we also used a random-effects model to consider the effect of heterogeneity among the studies (Q = 110.7, p<0.001, I2 = 94.58%). The sensitivity analysis reveals that 2,505 negative studies have been missed to reverse the statistical significance (Nfs.05 = 2505). The conclusion from the second meta-analysis is convincing, and the publication bias could be neglected.
Figure 3.
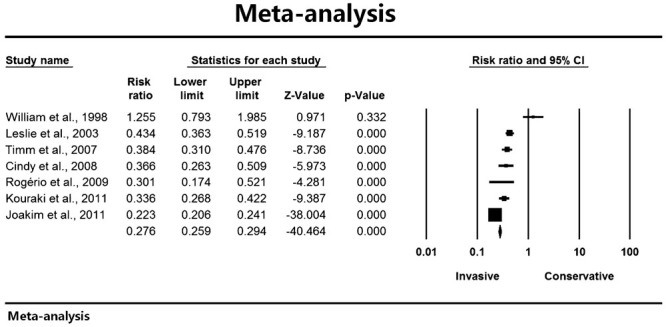
Primary analysis of the NSTE-ACS OCS within 1 year.
DISCUSSION
NSTE-ACS is responsible for approximately 1 million admissions to U.S. hospitals and twice as many to European hospitals each year and is associated with an in-hospital mortality rate of approximately 5% (25). Worldwide, more than 4 million people each year are estimated to have a NSTEMI, and long-term mortality is higher in patients with NSTE-ACS than in those with ST-elevation acute coronary syndrome (STE-ACS) (26,27). In 2012, the ACCF/AHA published an update to their 2011 guidelines for the management of patients with NSTE-ACS (19,28). According to the new guidelines, selecting either invasive or conservative strategy is one of the most important decisions that must be made in managing NSTE-ACS patients. The ACC/AHA guidelines continue to support an early invasive strategy in patients with high-risk NSTE-ACS without serious comorbidities or contraindications to angiography; in contrast, an early conservative approach should be selected for low-risk patients.
The results of our present study were consistent with the new 2012 guidelines, and the two systematic meta-analyses showed that compared to a conservative strategy, an invasive strategy is associated with reduced short- and long-term mortality in patients with NSTE-ACS after hospital discharge.
Meta-analyses are statistical tools for pooling existing evidence; therefore, we considered the strength of the evidence from all seven studies (11-17). We searched and analyzed those articles addressing the treatment strategies for NSTE-ACS. Furthermore, we studied the details of the related studies according to the 2012 guidelines (19); these studies include well-known studies such as the FRISC II (Fragmin and Fast Revascularization During Instability in Coronary Artery Disease II) (4), the RITA 3 (Randomized Intervention Trial of Unstable Angina 3) trial (8), TACTICS-TIMI 18 (Treat angina with Aggrastat and Determine Cost of Therapy with an Invasive or Conservative Strategy-Thrombolysis in Myocardial Infarction 18) trial (7), ICTUS (Invasive vs Conservative Treatment in Unstable Coronary Syndromes) trial (29), TIMI IIIB (Thrombolysis in Myocardial Infarction IIIB) (30), MATE (Medicine vs Angiography in Thrombolytic Exclusion) (31), and VINO (Value of First Day Angiography/Angioplasty In Evolving Non-ST Segment Elevation Myocardial Infarction) (32). Based on the above mentioned studies, we found that an invasive strategy could improve the short- or long-term survival rates of NSTE-ACS patients compared to a conservative strategy. In addition, a related meta-analysis demonstrated that an invasive strategy had comparable benefits in men and high-risk women for reducing the composite end point of death, MI, or re-hospitalization with NSTE-ACS (33).
In our present work, we did not distinguish between gender, age, risk factors, and complications for the two strategies; however, we focused on the all-cause mortality at 30 days and 1 year after hospital discharge. At the same time, we strictly limited the definition of the invasive and conservative strategies. The invasive group contained patients who underwent cardiac catheterization during the index hospitalization with or without revascularization; in contrast, patients who did not receive catheterization in the hospital were included in the conservative group. Catheterization included angiography and percutaneous coronary intervention; moreover, patients who underwent CABG surgery and IABP in the hospital were included in the invasive group. Our purpose was to assess whether a particular strategy decreased all-cause mortality in NSTE-ACS patients. Boden et al. (17) demonstrated that some NSTE-ACS patients in the conservative group also received interventional therapy, but we analyzed the total details of the study and regrouped the patients into the conservative or invasive management groups; then, we retrospectively analyzed the data and eliminated the interference from the two therapies with one another. Although the William et al. study was a RCT, we included it in the present work after addressing the interfering factors. Thus, seven studies were included in our meta-analysis.
While analyzing our data, we assessed other reviews that compared the effectiveness of both strategies in NSTE-ACS patients. These reviews include Núñez et al. (9), Boden (34,35), Neumann et al. (36), Choudhry et al. (37), O′Donoghue et al. (33), Hoenig et al. (38,39), Navarese et al. (40), and Damman P et al. (41) Based on these reviews, we found that over the past 10 years, there is still controversy regarding invasive versus conservative strategy in NSTE-ACS patients. Compared with a conservative strategy for NSTE-ACS patients, some studies reported that an invasive therapy provided comparable benefits and reduced the rates of fatal or nonfatal re-infarction and hospital readmission but not all-cause mortality (9,33,35,37). However, other studies found that an invasive strategy was not related to improvements in long-term survival and reduced the rate of revascularization compared with conservative management (34,36,40,41).
Furthermore, the above mentioned studies did not strictly distinguish between or define conservative and invasive strategies; for instance, the administration of antithrombotics was the primary step prior to interventional therapy in invasive strategy. However, in some RCTs, patients with NSTE-ACS in the conservative treatment group also received interventional therapy during the index hospitalization when medical therapy failed or if substantial residual ischemia was documented. Based on these facts, we defined the concept of conservative and invasive strategies strictly as described in our article and performed the meta-analysis based on these definitions.
Inspired by the above mentioned studies, we strictly redefined the conservative and invasive strategy and retrospectively analyzed seven studies. The NSTE-ACS patients who received interventional management in the hospital were included in the invasive group, whereas the other patients were placed in the conservative group. The main end-point events were 30-day and 1-year all-cause mortality. After performing two systematic meta-analyses, we found that invasive therapy improved the prognosis of patients with NSTE-ACS (compared with conservative therapy) and reduced the short- and long-term mortality.
We also noted that the results of the Boden et al. study (17) demonstrated that conservative therapies could play more beneficial roles in NSTE-ACS patients than did invasive strategies. What are the reasons for the opposite results? We analyzed their findings in detail and further studied its quotation from Ferry et al. (42) and found that the authors excluded 247 patients with high-risk ischemic complications (e.g., unstable angina after infarction, congestive heart failure that did not respond to medical therapy, cardiogenic shock, or symptomatic ventricular arrhythmia) during the first 48 hours after the onset of infarction. Moreover, the invasive theories, techniques and equipment were not then as well established as they are currently. With the development of modern percutaneous coronary intervention technology, invasive strategies show more benefit than conservative medical therapies in NSTE-ACS patients.
For patients with NSTE-ACS (NSTEMI/UA), an invasive strategy reduces short- and long-term all-cause mortality compared with a conservative strategy. An invasive strategy is preferable to a conservative strategy in treating NSTE-ACS. Of course, these results require validation in future RCTs.
ACKNOWLEDGMENTS
This study was supported by grants from the National Natural Science Foundation of China (81372023). The funders played no roles in the study design, data collection, analysis, decision to publish, or manuscript preparation. We thank all our colleagues who supported this work.
Footnotes
No potential conflict of interest was reported.
REFERENCES
- 1.Giugliano RP, Braunwald E. The Year in Non-ST-Segment Elevation Acute Coronary Syndrome. J Am Coll Cardiol. 2012;60(21):2127–39. doi: 10.1016/j.jacc.2012.08.972. [DOI] [PubMed] [Google Scholar]
- 2.Roger VL, Go AS, Lloyd-Jones DM, Benjamin EJ, Berry JD, Borden WB, et al. Executive summary: heart disease and stroke statistics – 2012 update: a report from the American Heart Association. Circulation. 2012;125(1):188–97. doi: 10.1161/CIR.0b013e3182456d46. [DOI] [PubMed] [Google Scholar]
- 3.Di Chiara A, Fresco C, Savonitto S, Greco C, Lucci D, Gonzini L, et al. Epidemiology of non-ST elevation acute coronary syndromes in the Italian cardiology network: the BLITZ-2 study. Eur Heart J. 2006;27(4):393–405. doi: 10.1093/eurheartj/ehi557. [DOI] [PubMed] [Google Scholar]
- 4.DeWood MA, Stifter WF, Simpson CS, Spores J, Eugster GS, Judge TP, et al. Coronary arteriographic findings soon after non-Q-wave myocardial infarction. N Engl J Med. 1986;315(7):417–23. doi: 10.1056/NEJM198608143150703. [DOI] [PubMed] [Google Scholar]
- 5.Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Jr, et al. 2011 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;123(18):e426–e579. doi: 10.1161/CIR.0b013e318212bb8b. [DOI] [PubMed] [Google Scholar]
- 6.Invasive compared with non-invasive treatment in unstable coronary-artery disease: FRISC II prospective randomised multicentre study. FRagmin and Fast Revascularisation during InStability in Coronary artery disease Investigators. Lancet. 1999;354(9180):708–15. [PubMed] [Google Scholar]
- 7.Cannon CP, Weintraub WS, Demopoulos LA, Vicari R, Frey MJ, Lakkis N, et al. Comparison of early invasive and conservative strategies in patients with unstable coronary syndromes treated with the glycoprotein IIb/IIIa inhibitor tirofiban. N Engl J Med. 2001;344(25):1879–87. doi: 10.1056/NEJM200106213442501. [DOI] [PubMed] [Google Scholar]
- 8.Fox KA, Poole-Wilson PA, Henderson RA, Clayton TC, Chamberlain DA, Shaw TR, et al. Interventional versus conservative treatment for patients with unstable angina or non-ST-elevation myocardial infarction: the British Heart Foundation RITA 3 randomised trial. Randomized Intervention Trial of unstable Angina. Lancet. 2002;360(9335):743–51. doi: 10.1016/s0140-6736(02)09894-x. [DOI] [PubMed] [Google Scholar]
- 9.Bach RG, Cannon CP, Weintraub WS, DiBattiste PM, Demopoulos LA, Anderson HV, et al. The effect of routine, early invasive management on outcome for elderly patients with non-ST-segment elevation acute coronary syndromes. Ann Intern Med. 2004;141(3):186–95. doi: 10.7326/0003-4819-141-3-200408030-00007. [DOI] [PubMed] [Google Scholar]
- 10.Diderholm E, Andrén B, Frostfeldt G, Genberg M, Jernberg T, Lagerqvist B, et al. ST depression in ECG at entry indicates severe coronary lesions and large benefits of an early invasive treatment strategy in unstable coronary artery disease; the FRISC II ECG substudy. The Fast Revascularisation during InStability in Coronary artery disease. Eur Heart J. 2002;23(1):41–9. doi: 10.1053/euhj.2001.2694. [DOI] [PubMed] [Google Scholar]
- 11.Cho L, Bhatt DL, Marso SP, Brennan D, Holmes DR, Jr, Califf RM, et al. An invasive strategy is associated with decreased mortality in patients with unstable angina and non-ST- elevation myocardial infarction: GUSTO IIb trial. Am J Med. 2003;114(2):106–11. doi: 10.1016/s0002-9343(02)01446-8. [DOI] [PubMed] [Google Scholar]
- 12.Bauer T, Koeth O, Jünger C, Heer T, Wienbergen H, Gitt A, et al. Effect of an invasive strategy on in-hospital outcome in elderly patients with non-ST-elevation myocardial infarction. Eur Heart J. 2007;28(23):2873–8. doi: 10.1093/eurheartj/ehm464. [DOI] [PubMed] [Google Scholar]
- 13.Lee CH, Tan M, Yan AT, Yan RT, Fitchett D, Grima EA, et al. Use of cardiac catheterization for non-ST-segment elevation acute coronary syndromes according to initial risk: reasons why physicians choose not to refer their patients. Arch Intern Med. 2008;168(3):291–6. doi: 10.1001/archinternmed.2007.78. [DOI] [PubMed] [Google Scholar]
- 14.Teixeira R, Lourenço C, Baptista R, Jorge E, António N, Monteiro S, et al. Invasive versus conservative strategy in non-ST elevation acute coronary syndromes: data from a single Portuguese center. Rev Port Cardiol. 2009;28(4):355–73. [PubMed] [Google Scholar]
- 15.Kleopatra K, Muth K, Zahn R, Bauer T, Koeth O, Jünger C, et al. Effect of an invasive strategy on in-hospital outcome and one-year mortality in women with non-ST-elevation myocardial infarction. Int J Cardiol. 2011;153(3):291–5. doi: 10.1016/j.ijcard.2010.08.050. [DOI] [PubMed] [Google Scholar]
- 16.Alfredsson J, Lindbäck J, Wallentin L, Swahn E. Similar outcome with an invasive strategy in men and women with non-ST-elevation acute coronary syndromes: from the Swedish Web-System for Enhancement and Development of Evidence-Based Care in Heart Disease Evaluated According to Recommended Therapies (SWEDEHEART) Eur Heart J. 2011;32(24):3128–36. doi: 10.1093/eurheartj/ehr349. [DOI] [PubMed] [Google Scholar]
- 17.Boden WE, O′Rourke RA, Crawford MH, Blaustein AS, Deedwania PC, Zoble RG, et al. Outcomes in patients with acute non-Q-wave myocardial infarction randomly assigned to an invasive as compared with a conservative management strategy. Veterans Affairs Non-Q-Wave Infarction Strategies in Hospital (VANQWISH) Trial Investigators. N Engl J Med. 1998;338(25):1785–92. doi: 10.1056/NEJM199806183382501. [DOI] [PubMed] [Google Scholar]
- 18.Savonitto S, Cavallini C, Petronio AS, Murena E, Antonicelli R, Sacco A, et al. Early aggressive versus initially conservative treatment in elderly patients with non-ST-segment elevation acute coronary syndrome: a randomized controlled trial. JACC Cardiovasc Interv. 2012;5(9):906–16. doi: 10.1016/j.jcin.2012.06.008. [DOI] [PubMed] [Google Scholar]
- 19.2012 Writing Committee Members. Jneid H, Anderson JL, Wright RS, Adams CD, Bridges CR, et al. 2012 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non-ST-elevation myocardial infarction (updating the 2007 guideline and replacing the 2011 focused update): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2012;126(7):875–910. doi: 10.1161/CIR.0b013e318256f1e0. [DOI] [PubMed] [Google Scholar]
- 20.Lagerqvist B, Husted S, Kontny F, Ståhle E, Swahn E, Wallentin L, et al. 5-year outcomes in the FRISC-II randomised trial of an invasive versus a non-invasive strategy in non-ST-elevation acute coronary syndrome: a follow-up study. Lancet. 2006;368(9540):998–1004. doi: 10.1016/S0140-6736(06)69416-6. [DOI] [PubMed] [Google Scholar]
- 21.Núñez J, Sanchis J, Núñez E, Bodi V, Bertomeu-González V, Bosch M. Prognostic differences between routine invasive and conservative strategies for the management of high-risk, non-ST segment acute coronary syndromes: Experience from two consecutive periods in a single center. Eur J Intern Med. 2007;18(5):409–16. doi: 10.1016/j.ejim.2006.12.011. et al. [DOI] [PubMed] [Google Scholar]
- 22.Moher D, Liberati A, Tetzlaff J, Altman DG. PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2008;149(4):264–9. doi: 10.7326/0003-4819-151-4-200908180-00135. [DOI] [PubMed] [Google Scholar]
- 23.Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of Observational Studies in Epidemiology: A Proposal for Reporting. JAMA. 2000;283(15):2008–12. doi: 10.1001/jama.283.15.2008. [DOI] [PubMed] [Google Scholar]
- 24.Rosenthal R. The file drawer problem and tolerance for null results. Psychol Bull. 1979;86:638–41. [Google Scholar]
- 25.Peterson ED, Roe MT, Mulgund J, DeLong ER, Lytle BL, Brindis RG, et al. Association between hospital process performance and outcomes among patients with acute coronary syndromes. JAMA. 2006;295(16):1912–20. doi: 10.1001/jama.295.16.1912. [DOI] [PubMed] [Google Scholar]
- 26.White HD, Chew DP. Acute myocardial infarction. Lancet. 2008;372(9638):570–84. doi: 10.1016/S0140-6736(08)61237-4. [DOI] [PubMed] [Google Scholar]
- 27.Terkelsen CJ, Lassen JF, Nørgaard BL, Gerdes JC, Jensen T, Gøtzsche LB, et al. Mortality rates in patients with ST-elevation vs. non-ST-elevation acute myocardial infarction: observations from an unselected cohort. Eur Heart J. 2005;26(1):18–26. doi: 10.1093/eurheartj/ehi002. [DOI] [PubMed] [Google Scholar]
- 28.Wright RS, Anderson JL, Adams CD, Bridge CR, Casey DE, Jr, Ettinger SM, et al. 2011 ACCF/AHA focused update of the guideline for the management of patients with unstable angina/Non-ST-elevation myocardial infarction (updating the 2007 guideline): a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;123(18):2022–60. doi: 10.1161/CIR.0b013e31820f2f3e. [DOI] [PubMed] [Google Scholar]
- 29.de Winter RJ, Windhausen F, Cornel JH, Dunselman PH, Janus CL, Bendermacher PE, et al. Early invasive versus selectively invasive management for acute coronary syndromes. N Engl J Med. 2005;353(11):1095–104. doi: 10.1056/NEJMoa044259. [DOI] [PubMed] [Google Scholar]
- 30.Effects of tissue plasminogen activator and a comparison of early invasive and conservative strategies in unstable angina and non-Q-wave myocardial infarction. Results of the TIMI IIIB Trial. Thrombolysis in Myocardial Ischemia. Circulation. 1994;89(4):1545–56. doi: 10.1161/01.cir.89.4.1545. [DOI] [PubMed] [Google Scholar]
- 31.McCullough PA, O′Neill WW, Graham M, Stomel RJ, Rogers F, David S, et al. A prospective randomized trial of triage angiography in acute coronary syndromes ineligible for thrombolytic therapy. Results of the medicine versus angiography in Thrombolytic Exclusion (MATE) trial. J Am Coll Cardiol. 1998;32(3):596–605. doi: 10.1016/s0735-1097(98)00284-8. [DOI] [PubMed] [Google Scholar]
- 32.Spacek R, Widimský P, Straka Z, Jiresová E, Dvorák J, Polásek R, et al. Value of first day angiography/angioplasty in evolving Non-ST segment elevation myocardial infarction: an open multicenter randomized trial. The VINO Study. Eur Heart J. 2002;23(3):230–8. doi: 10.1053/euhj.2001.2735. [DOI] [PubMed] [Google Scholar]
- 33.O′Donoghue M, Boden WE, Braunwald E, Cannon CP, Clayton TC, de Winter RJ, et al. Early invasive vs conservative treatment strategies in women and men with unstable angina and non-ST-segment elevation myocardial infarction: a meta-analysis. JAMA. 2008;300(1):71–80. doi: 10.1001/jama.300.1.71. [DOI] [PubMed] [Google Scholar]
- 34.Boden WE. Avoidance of routine revascularization in the management of patients with non-ST-segment elevation acute coronary syndromes. Am J Cardiol. 2000;86(12B):42M–47M. doi: 10.1016/s0002-9149(00)01480-6. [DOI] [PubMed] [Google Scholar]
- 35.Boden WE. “Routine invasive” versus “selective invasive” approaches to non-ST-segment elevation acute coronary syndromes management in the post-stent/platelet inhibition era. J Am Coll Cardiol. 2003;41(4 Suppl S):113S–122S. doi: 10.1016/s0735-1097(02)02963-7. [DOI] [PubMed] [Google Scholar]
- 36.Neumann FJ, Kastrati A, Pogatsa-Murray G, Mehilli J, Bollwein H, Bestehorn HP, et al. Evaluation of prolonged antithrombotic pretreatment (“cooling-off” strategy) before intervention in patients with unstable coronary syndromes: a randomized controlled trial. JAMA. 2003;290(12):1593–9. doi: 10.1001/jama.290.12.1593. [DOI] [PubMed] [Google Scholar]
- 37.Choudhry NK, Singh JM, Barolet A, Tomlinson GA, Detsky AS. How should patients with unstable angina and non-ST-segment elevation myocardial infarction be managed? A meta-analysis of randomized trials. Am J Med. 2005;118(5):465–74. doi: 10.1016/j.amjmed.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 38.Hoenig MR, Doust JA, Aroney CN, Scott IA. Early invasive versus conservative strategies for unstable angina & non-ST-elevation myocardial infarction in the stent era. Cochrane Database Syst Rev. 2006;3:CD004815. doi: 10.1002/14651858.CD004815.pub2. [DOI] [PubMed] [Google Scholar]
- 39.Hoenig MR, Aroney CN, Scott IA. Early invasive versus conservative strategies for unstable angina and non-ST-elevation myocardial infarction in the stent era. Cochrane Database Syst Rev. 2010;3:CD004815. doi: 10.1002/14651858.CD004815.pub3. [DOI] [PubMed] [Google Scholar]
- 40.Navarese EP, De Servi S, Gibson CM, Buffon A, Castriota F, Kubica J, et al. Early vs. delayed invasive strategy in patients with acute coronary syndromes without ST-segment elevation: a meta-analysis of randomized studies. QJM. 2011;104(3):193–200. doi: 10.1093/qjmed/hcq258. [DOI] [PubMed] [Google Scholar]
- 41.Damman P, van Geloven N, Wallentin L, Lagerqvist B, Fox KA, Clayton T, et al. Timing of angiography with a routine invasive strategy and long-term outcomes in non-ST-segment elevation acute coronary syndrome: a collaborative analysis of individual patient data from the FRISC II (Fragmin and Fast Revascularization During Instability in Coronary Artery Disease), ICTUS (Invasive Versus Conservative Treatment in Unstable Coronary Syndromes), and RITA-3 (Intervention Versus Conservative Treatment Strategy in Patients With Unstable Angina or Non-ST Elevation Myocardial Infarction) Trials. JACC Cardiovasc Interv. 2012;5(2):191–9. doi: 10.1016/j.jcin.2011.10.016. [DOI] [PubMed] [Google Scholar]
- 42.Ferry DR, O′Rourke RA, Blaustein AS, Crawford MH, Deedwania PC, Carson PE, et al. Design and baseline characteristics of the Veterans Affairs Non-Q-Wave Infarction Strategies In-Hospital (VANQWISH) trial. J Am Coll Cardiol. 1998;31(2):312–20. doi: 10.1016/s0735-1097(97)00486-5. [DOI] [PubMed] [Google Scholar]


