Abstract
Spontaneous idiopathic splenic hematomas occur very rare. Hematomas of the spleen are usually associated with trauma, or infectious, neoplastic, or hematologic diseases. They present a diagnostic challenge as they can be easily confused with other more common entities. We report a case of atraumatic idiopathic splenic hematoma in a patient with no underlying systemic or local disease and discuss the approach to diagnosis and treatment.
INTRODUCTION
The spleen is the most vascular organ of the body, with a blood flow of ∼350 l/day. It can hold up to 1.5 l of blood in total, making it a reservoir of 30% of the total blood volume. Splenic hematomas with subsequent calcification or immediate rupture are most commonly the result of blunt abdominal trauma [1]. However, atraumatic hematomas of the spleen, which constitute 23% of cases, may result from a multitude of systemic diseases which may be infectious, hematologic, neoplastic or infiltrative in nature. 6.3% of atraumatic splenic hematomas are dubbed ‘idiopathic’ with no identifiable causative factor [2]. We present a case of chronic idiopathic spleen hematoma that was discovered incidentally, and treated electively with laparoscopic splenectomy, with no abnormal histological findings on pathologic examination of spleen.
CASE REPORT
A 24-year-old woman with negative medical and surgical history, complaining of epigastric discomfort and associated nausea and occasional vomiting underwent abdominal ultrasound evaluation for suspicion of gallstone disease. The ultrasound results, further confirmed by computed tomography (CT) scan (Fig. 1a–c), revealed a large 16 × 12 cm splenic cystic mass. She was referred to Poissy Hospital (Paris) for surgical management of the splenic cystic tumor. The decision was made to perform laparoscopic splenectomy, with high suspicion of splenic hydatid cyst. Preoperative laboratory workup including Complete Blood Count, parasitic serologies and chemistries were within normal limits. Pneumovax 23™ 23-valent pneumococcal polysaccharide vaccine was administered 2 weeks prior to the planned splenectomy. Under general anesthesia, with the patient in the right decubitus position in reverse flexion, the abdomen was prepped and draped in the usual manner. Pneumoperitoneum was induced through a left sub-costal Veress needle insertion. A 10 mm camera port was inserted in the umbilical area. A 12 mm trocar was inserted in the sub-costal anterior axillary line. Another 5 mm trocar was inserted in the left sub-xiphoid area and a 5 mm trocar was inserted in the sub-costal mid axillary line. Exploration of the abdomen revealed a large splenic mass occupying the left flank and the epigastrium, covered with patchy white membranes. The rest of the spleen was lying posterior and inferior to the tumor and no other abnormalities were detected. Using Echelon Endopath™, a white endostapler, the splenocolic ligament was dissected exposing the left gastroepicloic artery, which was clipped and cut. Then the splenic hilum was dissected after retracting the spleen cephalad. The splenic vasculature was of bundled type with one major splenic artery, which was identified superior to the splenic vein. Both were dissected, clipped and cut making sure to preserve the pancreatica magna artery. Then dissection was carried on along the greater curvature of the stomach, where the short gastric were also cut. In order to completely mobilize the spleen, the splenophrenic ligament was also cut. A small hole was punctured into the wall of the cyst, through which 1.1 l of chocolate-colored liquid was entirely contained and suctioned to be sent for cytology followed by extensive irrigation with cetrimide ensuring no contamination. A fragment of the wall was sent to frozen section and was histologically identified as organized calcified hematoma with negative cytology. The spleen and the remainder of the cystic tumor were removed through a small incision in the left lower quadrant. A Hemovac™ suctioning device was left in the surgical site. The postoperative period was uneventful. The patient received prophylactic antibiotic treatment with 1.2 g of Amoxicillin/Clavulanic acid (Augmentin™) IVDrip every 12 h for six doses and the drain was removed on the fifth postoperative day. The patient's platelet count on postoperative day 6 was 620 000/µl. Consequently, 75 mg of acetylsalicylic acid (Kardegic™) was started once daily. The patient was discharged on postoperative day 7.
Figure 1:
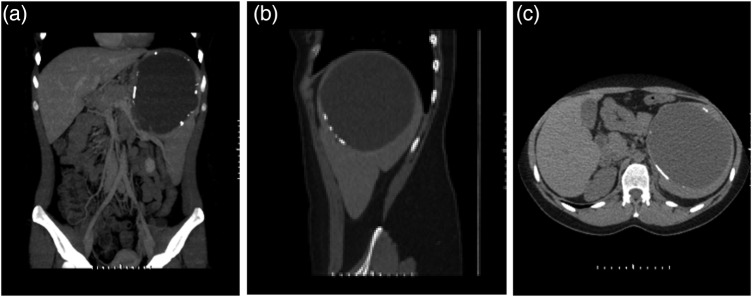
CT scan of the abdomen and pelvis without contrast, showing the 16 cm splenic cyst with partially calcified rim. (a) Coronal view, (b) saggital view, (c) cross-sectional view.
DISCUSSION
Traumatic hemorrhage or rupture of a normal spleen is a common result of high velocity trauma. A pathologic splenic hematoma is less frequently encountered secondary to diseases affecting the reticuloendothelial system (Epstein–Barr virus infection, cytomegalovirus infection, hepatitis, malaria) or neoplasia (lymphoma, leukemia) [3]. Spontaneous hematoma formation with possible rupture of the normal spleen has been a subject of controversy since the first case reported by Atkinson (1874) [4]. Orloff and Peskin later identified criteria for the diagnosis of spontaneous spleen insult [3]. Guided by those criteria, we found no history of trauma or unusual effort which conceivably could have injured the patient's spleen; there was no evidence of systemic or local disease in organs other than the spleen. Moreover, there was no evidence of perisplenic adhesions or scarring that could have suggested trauma or previous rupture. Aside from the hematoma, the spleen was normal on both gross inspection and histological examination. Furthermore, coagulation studies were normal. The acute-phase and convalescent sera did not show any significant rise in viral antibody titers suggestive of recent infection with viral types associated with spleen involvement, such as Epstein–Barr virus, cytomegalovirus or hepatitis viruses.
CT scanning is considered to be superior to ultrasonography for characterizing splenic pathology [5]. It usually is performed in conjunction with the intravenous administration of contrast material to maximize density differences between the splenic parenchyma and hematomas. In this fashion, CT is the imaging modality of choice as it allows for the best evaluation of the spleen and surrounding tissue changes [6]. When a mass lesion is identified within the spleen on CT scan, ultrasound, or MRI and the radiological diagnosis is inconclusive, splenectomy may be necessary as a combined diagnostic and curative procedure [7]. In such cases, the conservative nonsurgical approach generally used in stable traumatic splenic injuries [8] is not adequate. In the past decade, laparoscopy has become the standard approach for elective splenectomy, even for patients such as ours, presenting with massive splenomegaly and hematoma [9]. Perioperative vaccination of patients undergoing splenectomy is crucial for protection against sepsis caused by encapsulated microorganisms including Streptococcus pneumonia, Hemophilus influenza and Nisseria meningitides. Vaccine administration should be carried out 2 weeks prior to elective cases and on average 2 weeks after unplanned splenectomies [10].
Therefore, idioapathic splenic hematomas are rare, and their diagnosis is challenging in the absence of a history of systemic disease or trauma or alarming signs such as hemorrhage or rupture on presentation. When thorough history taking and physical examination coupled with diagnostic imaging and laboratory work-up are inconclusive, a laparoscopic splenectomy is the ultimate diagnostic and curative approach.
REFERENCES
- 1.Tintinalli JE, Kelen GD, Stapczynski JS. Emergency Medicine: A Comprehensive Study Guide. 6th edn. New York: McGraw Hill; 2004. [Google Scholar]
- 2.Renzulli P, Hostettler A, Schoepfer AM, Gloor B, Candinas D. Systematic review of atraumatic splenic rupture. Br J Surg. 2009;96:1114–21. doi: 10.1002/bjs.6737. [DOI] [PubMed] [Google Scholar]
- 3.Orloff MJ, Peskin GW. Spontaneous rupture of the normal spleen; a surgical enigma. Int Abstr Surg. 1958;106:1–11. [PubMed] [Google Scholar]
- 4.Atkinson E. Death from idiopathic rupture of the spleen. BMJ. 1874;2:403–4. [Google Scholar]
- 5.Kendall JL, Faragher J, Hewitt GJ, Burcham G, Haukoos JS. Emergency department ultrasound is not a sensitive detector of solid organ injury. West J Emerg Med. 2009;10:1–5. [PMC free article] [PubMed] [Google Scholar]
- 6.Umlas SL, Cronan JJ. Splenic trauma: can CT grading systems enable prediction of successful nonsurgical treatment? Radiology. 1991;178:481–7. doi: 10.1148/radiology.178.2.1987612. [DOI] [PubMed] [Google Scholar]
- 7.Kraus MD, Fleming MD, Vonderheide RH. The spleen as a diagnostic specimen: a review of 10 years’ experience at two tertiary care institutions. Cancer. 2001;91:2001–9. doi: 10.1002/1097-0142(20010601)91:11<2001::aid-cncr1225>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 8.Resciniti A, Fink MP, Raptopoulos V, Davidoff A, Silva WE. Nonoperative treatment of adult splenic trauma: development of a computed tomographic scoring system that detects appropriate candidates for expectant management. J Trauma. 1988;28:828–31. [PubMed] [Google Scholar]
- 9.Rescorla FJ, West KW, Engum SA, Grosfeld JL. Laparoscopic splenic procedures in children: experience in 231 children. Ann Surg. 2007;246:683–7. doi: 10.1097/SLA.0b013e318155abb9. discussion 687–8. [DOI] [PubMed] [Google Scholar]
- 10.Shatz DV, Romero-Steiner S, Elie CM, Holder PF, Carlone GM. Antibody responses in postsplenectomy trauma patients receiving the 23-valent pneumococcal polysaccharide vaccine at 14 versus 28 days postoperatively. J Trauma. 2002;53:1037–42. doi: 10.1097/00005373-200212000-00001. [DOI] [PubMed] [Google Scholar]


