Abstract
Hypertension is a powerful risk factor for cardiovascular mortality and morbidity, including heart failure with both preserved and reduced ejection fraction. Hypertensive heart disease (HHD) defines the complex and diverse perturbations of cardiac structure and function occurring secondary to hypertension. Left ventricular hypertrophy (LVH) is one of the most recognized features of HHD and is an established risk factor for adverse CV outcomes in hypertension. Beyond LVH, LV geometry provides additional information regarding the cardiac response to hypertension. Imaging studies from larger cohorts of hypertensive patients reveal wide variability in the prevalence of LVH and LV geometric patterns, with the prevalence of concentric LVH similar to that of eccentric LVH. Hypertension is also associated with concomitant impairments in LV diastolic and systolic function. It remains uncertain why patients develop different patterns of LVH, although demographics and clinical comorbidities appear to influence that response.
Keywords: Hypertension, Ventricular Remodeling, Echocardiography
INTRODUCTION
Hypertension is a major public health concern and one of the most important modifiable cardiovascular (CV) risk factors, responsible for up to half of all cardiovascular deaths1. It is also a powerful risk factor for incident heart failure (HF) with both preserved and reduced ejection fraction2, conditions that are increasing in prevalence in parallel with the aging population.3 Most importantly, treating hypertension can effectively prevent its associated complications, even in the elderly.4, 5
Hypertensive heart disease (HHD) defines the complex and diverse perturbations of cardiac structure and function occurring secondary to hypertension. It is frequently characterized by left ventricle hypertrophy (LVH), left atrial enlargement (LAE), and left ventricular (LV) systolic and diastolic dysfunction which are themselves potent risk factors for heart failure and atrial arrhythmias.6 LVH, in particular, is a hallmark of HHD. 7 The pathogenesis underlying LVH is likely multifactorial.8 In the face of abnormal loading conditions, particularly chronically elevated afterload, LVH allows for normalization of LV wall stress and preservation of LV mechanical function9. Despite its presumptive adaptive nature, LVH correlates with the overall CV risk of the hypertensive patient and is one of the most robust and validated prognostic markers in hypertension10-12.
Beyond LV mass alone, assessment of LV shape, or geometry, provides additional information regarding the cardiac response to hypertension. In a seminal paper published more than fifty years ago, Linzbach described specific ventricular morphologic adaptations to different hemodynamic stimuli and their functional correlates13. Based on these observations, currently the most commonly used schema for classifying LV geometry relates mass (hypertrophy) with the relative wall thickness (RWT), which describes the relationship between wall thickness and cavity size (concentricity)14. Using these 2 features, LV geometry can be classified as concentric LVH (increased mass and increased concentricity), eccentric LVH (increased mass and normal concentricity) and concentric remodeling (normal LV mass with an increased concentricity)15, 16.
HHD has classically been associated with concentric LVH, as increased LV wall thickness allows for normalization of LV wall stress in the face of elevated blood pressure17. It has been postulated that eventually, chronic increase in afterload result in LV dilatation (eccentric LVH) and reduced pump function, although several lines of preclinical and clinical evidence challenge this view of HHD progression18-20.
There is significant heterogeneity in the cardiac phenotype in hypertension, related to disease expression in addition to variability in duration, severity, effective treatment as well as the presence of associated comorbidities. As studies with small sample sizes may fail to adequately capture the spectrum of alterations in cardiac structure and function in hypertension, in the present review we focus on larger imaging studies from epidemiology and clinical trial cohorts of hypertensive patients. We review the observed perturbations in cardiac structure and function with special emphasis on LV geometric patterns and diastolic and systolic function.
LEFT VENTRICULAR STRUCTURE
Left Ventricular Hypertrophy
The prevalence of LVH in hypertension varies according to the characteristics of the population studied. In a hypertensive population with metabolic syndrome and chronic kidney disease, Iwashima et al.21 reported a prevalence of 71.5%, in contrast to 19.5% in a middle-aged cohort with uncomplicated hypertension.22 This variability is also potentiated by the different criteria used in different studies to calculate LVH23. Currently, the formula recommended by the American Echocardiography Society24 has gained wide acceptance, although some debate remains about the best indexation method25. LVH is associated with elevation in prognostically relevant cardiac biomarkers of myocardial injury (high sensitivity troponin) and wall stress (N-terminal B-type natriuretic peptide).26-28 Indeed, an extensive body of evidence supports the association of LVH with hypertension-related morbidity and mortality11, 29. Compared to hypertensive patients without LVH, Ganau et al. observed a 3-fold higher incidence of myocardial infarction or death in those with echocardiographically detected LVH16. Although the mechanisms linking LVH in hypertension to adverse clinical outcomes are not fully defined, LVH is a marker of the concomitant vascular disease associated with hypertension.30, 31 In addition, the process of cardiomyocyte hypertrophy underlying chamber-level hypertrophy is paralleled by myocardial microcirculation rarefaction, interstitial fibrosis, and increased myocyte apoptosis which together appear to predispose to myocardial dysfunction, ischemia and ventricular arrhythmias32.
Left Ventricle Geometry
There is wide variability in the prevalence of LV geometric patterns across the large epidemiology studies and clinical trials, likely related to the heterogeneity in the characteristics of the various hypertensive populations (Table 1). However, across studies, the prevalence of normal geometry was high. In only 4 epidemiologic studies was the prevalence of normal LV geometry less than 45%,21, 33-35and each of them had distinctive features that may explain the increased LV mass or concentricity. These included advanced age33, untreated blood pressure that was significantly elevated34, the presence of chronic kidney disease (CKD) or metabolic syndrome,21 and African American ethnicity35. Concordant with other literature reviews23, the prevalence of eccentric LVH was similar to, or higher than, the prevalence of concentric LVH in most of the cohorts we reviewed (Table 1). In aggregate these data emphasize the absence of a uniform LV geometric response to hypertension, likely reflecting the clinical and pathophysiological heterogeneity of hypertension. It remains uncertain why patients develop different patterns of LVH, but the duration and severity of hypertension along with demographic features, comorbidities, and genetic background are important determinants36, 20.
Table 1.
Cardiac geometry patterns prevalence in hypertension epidemiological studies and clinical trials.
| Demographics | LV structure | LV geometry | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Studies | Age, y | Male gender, % | White, % | BMI, Kg/m2 | EDD, mm | LVMi, g/m2 | LVH, % | Normal, % | Concentric Remodeling, % | Concentric LVH, % | Eccentric LVH, % |
| Saba et al. * (N=966) |
53±13 | 47.7 | 100 | 29.0±6.7 | 52.9±5.7 | 124±27 | 9.9 | 68.1 | 22 | 3.6 | 6.3 |
| PAMELA Study * (N=944) |
59±10 | 53.6 | 100 | 27.4±4.6 | NA | NA | 19.5 | 69.9 | 10.5 | 6 | 13.6 |
| APROS Study † (N=1074) |
48±11 | 53 | 100 | 26.9±4.7 | NA | NA | 36.9 | NA | NA | 6.6 | 30.3 |
| Fesler et al. † (N=645) |
44±13 | 57.1 | 100 | 25.3±3.7 | NA | NA | 33 | 48 | 22 | 19 | 11 |
| Muiesan et al. ‡ (N=436) |
56±8 | 57.1 | 100 | 26.5±3.5 | NA | NA | 38.6 | 47.9 | 13.5 | 17.9 | 20.7 |
| Eguchi et al. † (N=400) |
68±9 | 38 | 0 (100% Asian) | 24.5±3.5 | NA | NA | 59.75 | 21.5 | 18.75 | 31.75 | 28 |
| St. Petersburg Study ‡ (N=734) |
51±3 | 35.2 | 100 | 29.0±5.0 | 50.1±4.3 | 130±32 | 63.7 | 29.6 | 6.4 | 32.4 | 31.3 |
| Glorioso et al. † (N=493) |
47±10 | 59.6 | 100 | 26.8[1.3] | 49±4.1 | 97{25] | 26.2 | 67.5 | 6.3 | 6.5 | 19.7 |
| HyperGEN Study * (N=1384) |
53±11 | 64 | 37 (AA-63%) | 31.8±6.8 | NA | NA | 27 | 70 | 3.5 | 4 | 23 |
| APROS- diadys Study† (N=2545) |
70±4 | 49 | 100 | 26±2.6 | NA | NA | 30 | 51.4 | 18.6 | 15.5 | 14.5 |
| Iwashima et al. † (N=1160) |
63±11 | 53 | 0 (100 Asian) | 24.2±3.4 | NA | NA | 58.3 | 21.4 | 20.4 | 17.9 | 40.3 |
| LOLIPOP Study ‡ (N=1074) |
NA | NA | 100 | NA | NA | NA | 26 | 61 | 13 | 6 | 20 |
| Adebayo et al. † (N=1020) |
58±13 | 56 | 0 (100% Africans) | 27.0±5.3 | NA | NA | 33.9 | 18.2 | 47.8 | 23.2 | 10.7 |
| LIFE Study § (N=937) |
NA | 82 | NA | 27.2±4.4 | NA | NA | 34.3 | 63.1 | 2.6 | 29.8 | 4.5 |
| SEAS Subtudy§ (N=1238) |
69±11 | 59 | NA | 27.2±4.5 | 50.4±6.3 | NA | 40.2 | 50 | 10 | 12.1 | 30 |
population-based cohort
hospital-based cohort
Primary care practice-based cohort
Clinical trial
AA, African American; EDD – end-diastolic diameter, LVMI – left ventricular mass index; LVH – left ventricular hypertrophy. Values in italics were estimated by the authors from primary data provided in the referenced manuscript.
Ethnicity appears to be an important modulator of the LV adaptation to hypertension. In a population-based African American cohort, Fox et al.37 described a high prevalence of LVH, with concentric remodeling (36%) and concentric LVH (29%) more prevalent than other patterns. Concordant results are provided from other studies in black populations35, 38. These findings contrast with those of the Cardiovascular Health Study which, although enrolling older white hypertensive patients, found a much lower prevalence of LVH and increased concentricity 39. In addition, Drazner et al.40 demonstrated that the prevalence of LVH was increased in black compared to white patients even after adjustment for age, gender, body composition, blood pressure and socioeconomic status. Importantly, although these studies support an independent association between black ethnicity and higher LV mass and concentricity, ethnicity by itself only explains a small proportion of the variance in LVH41 and environmental influences appear more relevant.
Gender also appears to influence the LV response to hypertension. Data from the Framingham Heart Study demonstrate that the LV geometric adaptation to isolated systolic hypertension differs by sex, with women more likely to develop concentric LVH and men eccentric LVH42. Consistently, the effect of age and metabolic syndrome on LV structure appears to differ by gender, a more pronounced impact on LV mass and concentricity in women than men34, 43,43. Estrogen cannot fully explain this as the association was observed before and after menopause43. Differences in neurohumoral changes may be implicated in this sex-specific LV response44-46.
Diabetes is a major CV risk factor that is increasingly prevalent and clearly associated with hypertension47, 48. In the HyperGEN population-based cohort, diabetes was associated with LVH and concentricity independent of age, sex, BMI, blood pressure, and antihypertensive medication49. Interestingly, in a hypertensive Asian cohort, Eguchi et al. observed that diabetes influenced LV geometry but not LVH independently of ambulatory BP33. Differences in the demographic and clinical features of the studied populations such as ethnicity, duration of hypertension and degree of insulin-resistance may explain some between-study discordance regarding the influence of diabetes on the LV structure among hypertensive patients50-52.
Obesity is also a very prevalent comorbidity in hypertensive patients53. However unlike diabetes, obesity appears associated with eccentric rather than concentric LVH54. The increased cardiac output associated with relative hypervolemia in obesity may partially explain this impact on LV geometry. These changes are reversible, as morbidly obese patients demonstrate significant improvement of LV geometry after bariatric surgery due both to reductions in LV mass and degree of concentricity55, 56. As discussed in a recent meta-analysis57, differences in demographic and clinical features, including ethnicity, severity of obesity, and coexistence of obstructive sleep apnea, along with differences in the echocardiographic criteria employed might explain some of the discordance in findings between studies on the impact of obesity on cardiac structure in hypertension.
Greater LV mass is associated with chronic kidney disease (CKD) 58, 59. The presence of LVH correlates with the severity of glomerular filtration rate impairment and proteinuria, and is highly predictive of CV morbidity and mortality60, 61. CKD is associated with a concentric pattern of hypertrophy 21, 62. One plausible mechanistic explanation of the increased prevalence of concentric geometry is the increased aortic stiffness often observed in CKD patients. The noncompliant arterial tree increases LV afterload by enhancing wave reflections toward LV, which had been linked with concentric hypertrophy in preclinical and clinical studies63, 64. The precise mechanisms underlying the development of LVH in CKD are still not clearly defined although several studies also point to an important role of insulin resistance, inflammation, oxidative stress, and abnormalities of calcium-phosphate homeostasis 65, 66.
LV geometry and prognosis
Several studies have evaluated the prognostic value of LV geometry beyond just the presence of LVH with mixed results. This question is particularly challenging, as LV concentricity and mass are interrelated measures. Some studies have observed incremental prognostic value of LV geometric pattern beyond that conveyed by LV mass alone15, 67, 68. In untreated hypertensive patients, Muiesan et al.69 demonstrated that not only changes in LV mass but also changes in LV geometry from baseline to follow-up after initiation of antihypertensive therapy had independent prognostic value. In a population of patients with atrial fibrillation and a high prevalence of hypertension (>70%), concentric LVH was found to be an independent prognostic marker for all-cause mortality70. However, several other studies failed to demonstrate additive prognostic value of LV geometry71, 72. Using data from the Framingham Heart Study, Krumholz et al.73 found little prognostic value of LV geometry when adjusted to LV mass. Further studies are needed to evaluate the incremental prognostic value of characterizing LV geometry in hypertension. Using data from the Framingham cohort participants free of prevalent CV disease, Velagaleti et al. observed that eccentric LVH preferentially increased the risk of HF with reduced ejection fraction, while concentric LVH was associated with the development of HF with preserved ejection fraction74. Although limited by the absence of adjustment for relevant potential confounders such as coronary artery disease and valvular heart disease, these results suggest LV geometry is a determinant of subsequent functional impairment and HF phenotype.
LV geometry – limitations of the current classification
One limitation of the classification scheme for LV geometry described above is the failure to distinguish eccentric hypertrophy with or without LV dilatation. LV volume is a robust and validated prognostic marker in a wide range of CV diseases including hypertension75. Khouri et al.76 and Bang et al.77, using cardiac MRI and echocardiography respectively, classified LV geometry into 4 groups using LV volume and mass. They demonstrated differences in clinical and hemodynamic profiles between patients with eccentric LVH subclassified into either dilated or normal LV volume categories77. This suggests that the inclusion of LV volume, in addition to LVH and LV concentricity, may further refine the identification of relevant sub-phenotypes within hypertension, although its prognostic value has not yet been defined.
LV DIASTOLIC FUNCTION IN HYPERTENSION
There is extensive evidence demonstrating an association between hypertension and diastolic dysfunction in community-based populations78, 79. Similarly, the prevalence of diastolic dysfunction is high in hypertensive cohorts.80-83 Importantly, these noninvasive measures of diastolic performance are prognostic of incident HF and CV death78, 79, 82. The occurrence of diastolic dysfunction appears to occur in parallel with the structural changes characterizing hypertension. The presence of LVH is associated with both concomitant impaired relaxation and elevated LV filling pressure. 80, 84, 85. In contrast, concentric remodeling, while associated with impaired LV relaxation, does not appear to be a predictor elevated filling pressure. 86
Left atrial size is a barometer of chronic LV filling pressure and LAE has demonstrated prognostic value in several CV diseases87,90, 91. In hypertension, LAE correlates with blood pressure values, LVH and other echocardiographic measures of diastolic function88. The overall prevalence of LAE in hypertension patients is difficult to estimate because of the diversity of echocardiographic criteria and the clinical heterogeneity of patients. Cuspidi et al. recently analyzed 15 studies that reported LAE in hypertensive patients and estimated a pooled prevalence of 32%89. Although few studies have assessed the prognostic value of LAE specifically in hypertensive cohorts, LAE has been consistently and robustly associated with CV events in studies across the spectrum of CV disease87, 90.
LV SYSTOLIC FUNCTION IN HYPERTENSION
Among asymptomatic subjects with hypertension and no overt HF, the prevalence of LV systolic dysfunction defined by an LV ejection fraction (LVEF) <50% is approximately 3.6%,91 and identified patients at a 9-fold higher risk of developing HF 92. However, the LV structural changes associated with hypertension can also be associated with abnormalities in LV systolic function despite preserved LVEF. For example, midwall fractional shortening (FSmw) is a measure of LV radial deformation that appears less load-dependent than LVEF. In hypertension, FSmw is reduced despite preserved LVEF and this reduction is associated with greater LVH. Importantly, reduced FSmw is also associated with worse prognosis93, 94. Using novel echocardiography-based myocardial deformation imaging to assess cardiac mechanics, some groups have observed impairment in LV deformation in a variable proportion of hypertensive patients95-97. Although the association between systolic function and LV geometry is still debatable86, 98, the negative correlation between LVM and systolic function is quite consistent across studies91, 95, 99. These studies challenge the common perception of systolic abnormalities as a late change in the natural history of hypertension, although the clinical correlates and prognostic significance of these more subtle abnormalities is systolic function remain to be determined.
RV CHANGES IN HYPERTENSION
A meta-analysis of echocardiography studies of hypertensive subjects demonstrate that on average 25% have concomitant RV hypertrophy (range: 25-80%) and its severity correlates with the prevalence and magnitude of LVH100. Patients enrolled in these studies were unlikely to have pulmonary hypertension to explain these findings101, 102. Therefore, while the relationship between right and left ventricular structure is commonly framed in anatomic or hydraulic terms, these findings suggest that systemic diseases such as arterial hypertension can influence the RV through neurohumoral activation. Among the several putative pathophysiological mechanisms, increased sympathetic tone and abnormal activation of reninangiotensin-aldosterone system deserve particular attention and have been supported by several preclinical studies 103, 104. Using echocardiography-based deformation imaging, Tadic et al.105 observed worse RV and right atrial mechanics in hypertensive patients with inadequate BP control. In addition, these changes in the right-sided chambers correlate with aerobic exercise performance. Further studies are needed to examine the impact of treatment on RV function and to determine the prognostic value of these perturbations in RV structure and function in hypertension.
IMPACT OF ANTIHIPERTENSIVE TREATMENT ON CARDIAC STRUCTURE AND FUNCTION
Antihypertensive therapy has been associated with significant reduction in LV mass in several studies.69, 81, 106, 107 Interestingly, the magnitude of reduction in LV mass was found to correlate only modestly with the extent of BP decline81. Muiesan et al.69 also observed an impact of antihypertensive treatment on LV geometry, with a normalization of LV geometry occurring in 9% of the 436 subjects and associated with a better prognosis. In hypertensive patients treated with losartan or atenolol, Wachtell et al.108 reported a conversion of concentric to eccentric LVH in 34% of subjects, whereas only 3% of patients with eccentric LVH transitioned to concentric LVH.
Several groups have also noted an improvement of diastolic function in response to antihypertensive therapy109-111. However, two randomized clinical echocardiography sub-studies with larger sample sizes and longer duration of follow-up demonstrated no impact of antihypertensive therapy on diastolic function, despite adequate blood pressure control and significant regression of LV mass81, 106. This dissociation between structural and functional improvement may be related to the multifactorial pathogenesis of diastolic dysfunction. Alternatively, this dissociation could represent a preferential dependence of hypertension-induced diastolic dysfunction on the extracellular matrix composition as opposed to cardiomyocyte hypertrophy, which is the principal determinant LV mass81.
CONCLUSIONS
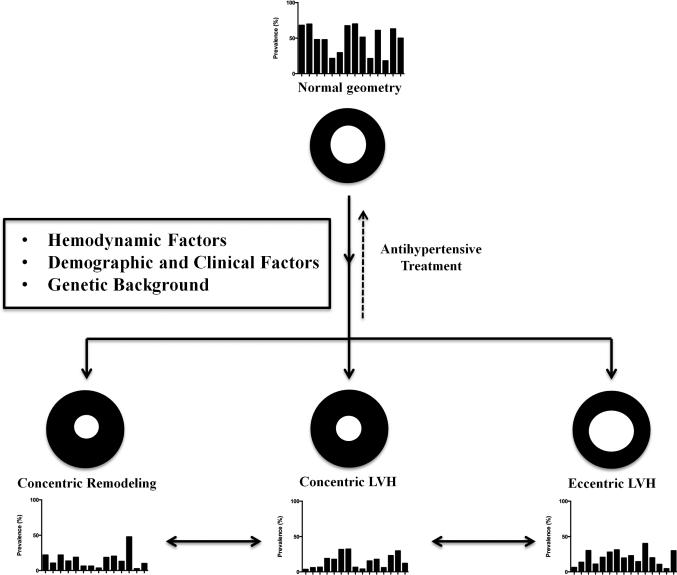
Patients with hypertension demonstrate diverse patterns of perturbation in cardiac structure and function (Figure 1). The prevalence of LVH varies considerably based on population characteristics including age, race, and co-morbidites. When present, LVH identifies patients at higher risk of CV events. Although classically associated with concentric hypertrophy, eccentric LVH is also common in hypertensive cohorts. HHD is also characterized by subclinical impairment in diastolic and systolic function. The determinants of the LV structural and functional response to hypertension – and its inter-individual variability – remain unclear, although patient characteristics including age, gender, race/ethnicity, and comorbidities likely contribute. Our current understanding of the underlying cellular and molecular mechanisms have been reviewed elsewhere32, 112, 113. Ultimately, a better understanding of the mechanisms and prognostic significance of these different cardiac phenotypes in hypertension may help improve our ability to individualize treatment and, ultimately, further reduce the morbidity and mortality caused by hypertension.
Figure 1.
Representation of different left ventricular geometric patterns and their interrelationship in hypertension. Bar graphs depict the prevalence of each LV geometric pattern in the reviewed epidemiological studies and clinical trials (Table 1; scale 0-100%). Arrows highlight the dynamic nature of cardiac structure, as illustrated by studies of the effect of antihypertensive treatment (see text for further discussion).
Acknowledgments
Funding Source:
The work for this manuscript was supported by Portuguese Foundation for Science and Technology grant HMSP-ICJ/0013/2012 (M.S.) and NHLBI grant 1K08HL116792-01A1 (A.M.S.).
Amil M. Shah declares that he work for this manuscript was partially supported by NHLBI grant 1K08HL116792-01A1. Dr. Shah is a recipient of a career development award (NHLBI grant 1K08HL116792-01A1) from NIH/NHLBI.
Footnotes
Conflict of Interest
Mário Santos declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
REFERENCES
- 1.Lawes CM, Vander Hoorn S, Rodgers A. Global burden of blood-pressure-related disease, 2001. Lancet. 2008;371:1513–1518. doi: 10.1016/S0140-6736(08)60655-8. [DOI] [PubMed] [Google Scholar]
- 2.Ho JE, Lyass A, Lee DS, Vasan RS, Kannel WB, Larson MG, Levy D. Predictors of new-onset heart failure: Differences in preserved versus reduced ejection fraction. Circ Heart Fail. 2013;6:279–286. doi: 10.1161/CIRCHEARTFAILURE.112.972828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Go AS, Mozaffarian D, Roger VL, Benjamin EJ, Berry JD, Borden WB, Bravata DM, Dai S, Ford ES, Fox CS, Franco S, Fullerton HJ, Gillespie C, Hailpern SM, Heit JA, Howard VJ, Huffman MD, Kissela BM, Kittner SJ, Lackland DT, Lichtman JH, Lisabeth LD, Magid D, Marcus GM, Marelli A, Matchar DB, McGuire DK, Mohler ER, Moy CS, Mussolino ME, Nichol G, Paynter NP, Schreiner PJ, Sorlie PD, Stein J, Turan TN, Virani SS, Wong ND, Woo D, Turner MB. Heart disease and stroke statistics--2013 update: A report from the american heart association. Circulation. 2013;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beckett NS, Peters R, Fletcher AE, Staessen JA, Liu L, Dumitrascu D, Stoyanovsky V, Antikainen RL, Nikitin Y, Anderson C, Belhani A, Forette F, Rajkumar C, Thijs L, Banya W, Bulpitt CJ. Treatment of hypertension in patients 80 years of age or older. N Engl J Med. 2008;358:1887–1898. doi: 10.1056/NEJMoa0801369. [DOI] [PubMed] [Google Scholar]
- 5.Briasoulis A, Agarwal V, Tousoulis D, Stefanadis C. Effects of antihypertensive treatment in patients over 65 years of age: A meta-analysis of randomised controlled studies. Heart. 2013 doi: 10.1136/heartjnl-2013-304111. [DOI] [PubMed] [Google Scholar]
- 6.Georgiopoulou VV, Kalogeropoulos AP, Raggi P, Butler J. Prevention, diagnosis, and treatment of hypertensive heart disease. Cardiol Clin. 2010;28:675–691. doi: 10.1016/j.ccl.2010.07.005. [DOI] [PubMed] [Google Scholar]
- 7.Mancia G, Fagard R, Narkiewicz K, Redon J, Zanchetti A, Bohm M, Christiaens T, Cifkova R, De Backer G, Dominiczak A, Galderisi M, Grobbee DE, Jaarsma T, Kirchhof P, Kjeldsen SE, Laurent S, Manolis AJ, Nilsson PM, Ruilope LM, Schmieder RE, Sirnes PA, Sleight P, Viigimaa M, Waeber B, Zannad F, Burnier M, Ambrosioni E, Caufield M, Coca A, Olsen MH, Tsioufis C, van de Borne P, Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Ferrari R, Hasdai D, Hoes AW, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Clement DL, Gillebert TC, Rosei EA, Anker SD, Bauersachs J, Hitij JB, Caulfield M, De Buyzere M, De Geest S, Derumeaux GA, Erdine S, Farsang C, Funck-Brentano C, Gerc V, Germano G, Gielen S, Haller H, Jordan J, Kahan T, Komajda M, Lovic D, Mahrholdt H, Ostergren J, Parati G, Perk J, Polonia J, Popescu BA, Reiner Z, Ryden L, Sirenko Y, Stanton A, Struijker-Boudier H, Vlachopoulos C, Volpe M, Wood DA. 2013 esh/esc guidelines for the management of arterial hypertension: The task force for the management of arterial hypertension of the european society of hypertension (esh) and of the european society of cardiology (esc). Eur Heart J. 2013;34:2159–2219. doi: 10.1093/eurheartj/eht151. [DOI] [PubMed] [Google Scholar]
- 8.Cacciapuoti F. Molecular mechanisms of left ventricular hypertrophy (lvh) in systemic hypertension (sh)-possible therapeutic perspectives. J Am Soc Hypertens. 2011;5:449–455. doi: 10.1016/j.jash.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 9.Frohlich ED, Apstein C, Chobanian AV, Devereux RB, Dustan HP, Dzau V, Fauad-Tarazi F, Horan MJ, Marcus M, Massie B, et al. The heart in hypertension. N Engl J Med. 1992;327:998–1008. doi: 10.1056/NEJM199210013271406. [DOI] [PubMed] [Google Scholar]
- 10.Gosse P, Cremer A, Vircoulon M, Coulon P, Jan E, Papaioannou G, Yeim S. Prognostic value of the extent of left ventricular hypertrophy and its evolution in the hypertensive patient. J Hypertens. 2012;30:2403–2409. doi: 10.1097/HJH.0b013e3283593029. [DOI] [PubMed] [Google Scholar]
- 11.Levy D, Garrison RJ, Savage DD, Kannel WB, Castelli WP. Prognostic implications of echocardiographically determined left ventricular mass in the framingham heart study. N Engl J Med. 1990;322:1561–1566. doi: 10.1056/NEJM199005313222203. [DOI] [PubMed] [Google Scholar]
- 12.Schillaci G, Verdecchia P, Porcellati C, Cuccurullo O, Cosco C, Perticone F. Continuous relation between left ventricular mass and cardiovascular risk in essential hypertension. Hypertension. 2000;35:580–586. doi: 10.1161/01.hyp.35.2.580. [DOI] [PubMed] [Google Scholar]
- 13.Linzbach AJ. Heart failure from the point of view of quantitative anatomy. Am J Cardiol. 1960;5:370–382. doi: 10.1016/0002-9149(60)90084-9. [DOI] [PubMed] [Google Scholar]
- 14.Devereux RB, Roman MJ. Left ventricular hypertrophy in hypertension: Stimuli, patterns, and consequences. Hypertens Res. 1999;22:1–9. doi: 10.1291/hypres.22.1. [DOI] [PubMed] [Google Scholar]
- 15.Koren MJ, Devereux RB, Casale PN, Savage DD, Laragh JH. Relation of left ventricular mass and geometry to morbidity and mortality in uncomplicated essential hypertension. Ann Intern Med. 1991;114:345–352. doi: 10.7326/0003-4819-114-5-345. [DOI] [PubMed] [Google Scholar]
- 16.Ganau A, Devereux RB, Roman MJ, de Simone G, Pickering TG, Saba PS, Vargiu P, Simongini I, Laragh JH. Patterns of left ventricular hypertrophy and geometric remodeling in essential hypertension. J Am Coll Cardiol. 1992;19:1550–1558. doi: 10.1016/0735-1097(92)90617-v. [DOI] [PubMed] [Google Scholar]
- 17.Grossman W, Jones D, McLaurin LP. Wall stress and patterns of hypertrophy in the human left ventricle. J Clin Invest. 1975;56:56–64. doi: 10.1172/JCI108079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Frey N, Olson EN. Cardiac hypertrophy: The good, the bad, and the ugly. Annu Rev Physiol. 2003;65:45–79. doi: 10.1146/annurev.physiol.65.092101.142243. [DOI] [PubMed] [Google Scholar]
- 19.Hill JA, Olson EN. Cardiac plasticity. N Engl J Med. 2008;358:1370–1380. doi: 10.1056/NEJMra072139. [DOI] [PubMed] [Google Scholar]
- 20**.Drazner MH. The progression of hypertensive heart disease. Circulation. 2011;123:327–334. doi: 10.1161/CIRCULATIONAHA.108.845792. [A review of the major pathophysiologic mechanisms underlying hypertensive heart disease and an informative discussion of the diverse pathways that it can take in the progression to heart failure.] [DOI] [PubMed] [Google Scholar]
- 21.Iwashima Y, Horio T, Kamide K, Tokudome T, Yoshihara F, Nakamura S, Ogihara T, Rakugi H, Kawano Y. Additive interaction of metabolic syndrome and chronic kidney disease on cardiac hypertrophy, and risk of cardiovascular disease in hypertension. Am J Hypertens. 2010;23:290–298. doi: 10.1038/ajh.2009.253. [DOI] [PubMed] [Google Scholar]
- 22.Mancia G, Carugo S, Grassi G, Lanzarotti A, Schiavina R, Cesana G, Sega R. Prevalence of left ventricular hypertrophy in hypertensive patients without and with blood pressure control: Data from the pamela population. Pressioni arteriose monitorate e loro associazioni. Hypertension. 2002;39:744–749. doi: 10.1161/hy0302.104669. [DOI] [PubMed] [Google Scholar]
- 23.Cuspidi C, Sala C, Negri F, Mancia G, Morganti A. Prevalence of left-ventricular hypertrophy in hypertension: An updated review of echocardiographic studies. J Hum Hypertens. 2012;26:343–349. doi: 10.1038/jhh.2011.104. [DOI] [PubMed] [Google Scholar]
- 24.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Recommendations for chamber quantification: A report from the american society of echocardiography's guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the european association of echocardiography, a branch of the european society of cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 25.Armstrong AC, Gidding S, Gjesdal O, Wu C, Bluemke DA, Lima JA. Lv mass assessed by echocardiography and cmr, cardiovascular outcomes, and medical practice. JACC Cardiovasc Imaging. 2012;5:837–848. doi: 10.1016/j.jcmg.2012.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ojji DB, Opie LH, Lecour S, Lacerda L, Adeyemi OM, Sliwa K. The effect of left ventricular remodelling on soluble st2 in a cohort of hypertensive subjects. J Hum Hypertens. 2014 doi: 10.1038/jhh.2013.130. [DOI] [PubMed] [Google Scholar]
- 27.Sinning C, Keller T, Zeller T, Ojeda F, Schluter M, Schnabel R, Lubos E, Bickel C, Lackner KJ, Diemert P, Munzel T, Blankenberg S, Wild PS. Association of high-sensitivity assayed troponin i with cardiovascular phenotypes in the general population: The population-based gutenberg health study. Clin Res Cardiol. 2013 doi: 10.1007/s00392-013-0640-8. [DOI] [PubMed] [Google Scholar]
- 28.Rienstra M, Yin X, Larson MG, Fontes JD, Magnani JW, McManus DD, McCabe EL, Coglianese EE, Amponsah M, Ho JE, Januzzi JL, Jr., Wollert KC, Fradley MG, Vasan RS, Ellinor PT, Wang TJ, Benjamin EJ. Relation between soluble st2, growth differentiation factor-15, and high-sensitivity troponin i and incident atrial fibrillation. Am Heart J. 2014;167:109–115. e102. doi: 10.1016/j.ahj.2013.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.de Simone G, Gottdiener JS, Chinali M, Maurer MS. Left ventricular mass predicts heart failure not related to previous myocardial infarction: The cardiovascular health study. Eur Heart J. 2008;29:741–747. doi: 10.1093/eurheartj/ehm605. [DOI] [PubMed] [Google Scholar]
- 30.Cuspidi C, Ambrosioni E, Mancia G, Pessina AC, Trimarco B, Zanchetti A. Role of echocardiography and carotid ultrasonography in stratifying risk in patients with essential hypertension: The assessment of prognostic risk observational survey. J Hypertens. 2002;20:1307–1314. doi: 10.1097/00004872-200207000-00017. [DOI] [PubMed] [Google Scholar]
- 31.Andrikou E, Tsioufis C, Thomopoulos C, Andrikou I, Kasiakogias A, Leontsinis I, Kordalis A, Katsimichas T, Tousoulis D, Stefanadis C. Left ventricular mass index as a predictor of new-onset microalbuminuria in hypertensive subjects: A prospective study. Am J Hypertens. 2012;25:1195–1201. doi: 10.1038/ajh.2012.109. [DOI] [PubMed] [Google Scholar]
- 32**.Frohlich ED, Gonzalez A, Diez J. Hypertensive left ventricular hypertrophy risk: Beyond adaptive cardiomyocytic hypertrophy. J Hypertens. 2011;29:17–26. doi: 10.1097/HJH.0b013e328340d787. [A comprehensive review of the pathophysiological mechanisms underlying hypertensive heart disease.] [DOI] [PubMed] [Google Scholar]
- 33.Eguchi K, Kario K, Hoshide S, Ishikawa J, Morinari M, Shimada K. Type 2 diabetes is associated with left ventricular concentric remodeling in hypertensive patients. Am J Hypertens. 2005;18:23–29. doi: 10.1016/j.amjhyper.2004.08.024. [DOI] [PubMed] [Google Scholar]
- 34.Conrady AO, Rudomanov OG, Zaharov DV, Krutikov AN, Vahrameeva NV, Yakovleva OI, Alexeeva NP, Shlyakhto EV. Prevalence and determinants of left ventricular hypertrophy and remodelling patterns in hypertensive patients: The st. Petersburg study. Blood Press. 2004;13:101–109. doi: 10.1080/08037050410031855. [DOI] [PubMed] [Google Scholar]
- 35.Adebayo RA, Bamikole OJ, Balogun MO, Akintomide AO, Adeyeye VO, Bisiriyu LA, Mene-Afejuku TO, Ajayi EA, Abiodun OO. Echocardiographic assessment of left ventricular geometric patterns in hypertensive patients in nigeria. Clin Med Insights Cardiol. 2013;7:161–167. doi: 10.4137/CMC.S12727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Devereux RB, de Simone G, Ganau A, Roman MJ. Left ventricular hypertrophy and geometric remodeling in hypertension: Stimuli, functional consequences and prognostic implications. J Hypertens Suppl. 1994;12:S117–127. [PubMed] [Google Scholar]
- 37.Fox ER, Taylor J, Taylor H, Han H, Samdarshi T, Arnett D, Myerson M. Left ventricular geometric patterns in the jackson cohort of the atherosclerotic risk in communities (aric) study: Clinical correlates and influences on systolic and diastolic dysfunction. Am Heart J. 2007;153:238–244. doi: 10.1016/j.ahj.2006.09.013. [DOI] [PubMed] [Google Scholar]
- 38.Akintunde A, Akinwusi O, Opadijo G. Left ventricular hypertrophy, geometric patterns and clinical correlates among treated hypertensive nigerians. Pan Afr Med J. 2010;4:8. doi: 10.4314/pamj.v4i1.53602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gardin JM, McClelland R, Kitzman D, Lima JA, Bommer W, Klopfenstein HS, Wong ND, Smith VE, Gottdiener J. M-mode echocardiographic predictors of six- to seven-year incidence of coronary heart disease, stroke, congestive heart failure, and mortality in an elderly cohort (the cardiovascular health study). Am J Cardiol. 2001;87:1051–1057. doi: 10.1016/s0002-9149(01)01460-6. [DOI] [PubMed] [Google Scholar]
- 40.Drazner MH, Dries DL, Peshock RM, Cooper RS, Klassen C, Kazi F, Willett D, Victor RG. Left ventricular hypertrophy is more prevalent in blacks than whites in the general population: The dallas heart study. Hypertension. 2005;46:124–129. doi: 10.1161/01.HYP.0000169972.96201.8e. [DOI] [PubMed] [Google Scholar]
- 41.Kizer JR, Arnett DK, Bella JN, Paranicas M, Rao DC, Province MA, Oberman A, Kitzman DW, Hopkins PN, Liu JE, Devereux RB. Differences in left ventricular structure between black and white hypertensive adults: The hypertension genetic epidemiology network study. Hypertension. 2004;43:1182–1188. doi: 10.1161/01.HYP.0000128738.94190.9f. [DOI] [PubMed] [Google Scholar]
- 42.Krumholz HM, Larson M, Levy D. Sex differences in cardiac adaptation to isolated systolic hypertension. Am J Cardiol. 1993;72:310–313. doi: 10.1016/0002-9149(93)90678-6. [DOI] [PubMed] [Google Scholar]
- 43.Kuch B, Muscholl M, Luchner A, Doring A, Riegger GA, Schunkert H, Hense HW. Gender specific differences in left ventricular adaptation to obesity and hypertension. J Hum Hypertens. 1998;12:685–691. doi: 10.1038/sj.jhh.1000689. [DOI] [PubMed] [Google Scholar]
- 44.Vasan RS, Evans JC, Benjamin EJ, Levy D, Larson MG, Sundstrom J, Murabito JM, Sam F, Colucci WS, Wilson PW. Relations of serum aldosterone to cardiac structure: Gender-related differences in the framingham heart study. Hypertension. 2004;43:957–962. doi: 10.1161/01.HYP.0000124251.06056.8e. [DOI] [PubMed] [Google Scholar]
- 45.Saba MM, Ibrahim MM, Rizk HH. Gender and the relationship between resting heart rate and left ventricular geometry. J Hypertens. 2001;19:367–373. doi: 10.1097/00004872-200103000-00003. [DOI] [PubMed] [Google Scholar]
- 46.Muscholl MW, Schunkert H, Muders F, Elsner D, Kuch B, Hense HW, Riegger GA. Neurohormonal activity and left ventricular geometry in patients with essential arterial hypertension. Am Heart J. 1998;135:58–66. doi: 10.1016/s0002-8703(98)70343-6. [DOI] [PubMed] [Google Scholar]
- 47.Teuscher A, Egger M, Herman JB. Diabetes and hypertension. Blood pressure in clinical diabetic patients and a control population. Arch Intern Med. 1989;149:1942–1945. doi: 10.1001/archinte.149.9.1942. [DOI] [PubMed] [Google Scholar]
- 48.Colosia AD, Palencia R, Khan S. Prevalence of hypertension and obesity in patients with type 2 diabetes mellitus in observational studies: A systematic literature review. Diabetes Metab Syndr Obes. 2013;6:327–338. doi: 10.2147/DMSO.S51325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Palmieri V, Bella JN, Arnett DK, Liu JE, Oberman A, Schuck MY, Kitzman DW, Hopkins PN, Morgan D, Rao DC, Devereux RB. Effect of type 2 diabetes mellitus on left ventricular geometry and systolic function in hypertensive subjects: Hypertension genetic epidemiology network (hypergen) study. Circulation. 2001;103:102–107. doi: 10.1161/01.cir.103.1.102. [DOI] [PubMed] [Google Scholar]
- 50.Galderisi M, Anderson KM, Wilson PW, Levy D. Echocardiographic evidence for the existence of a distinct diabetic cardiomyopathy (the framingham heart study). Am J Cardiol. 1991;68:85–89. doi: 10.1016/0002-9149(91)90716-x. [DOI] [PubMed] [Google Scholar]
- 51.Devereux RB, Roman MJ, Paranicas M, O'Grady MJ, Lee ET, Welty TK, Fabsitz RR, Robbins D, Rhoades ER, Howard BV. Impact of diabetes on cardiac structure and function: The strong heart study. Circulation. 2000;101:2271–2276. doi: 10.1161/01.cir.101.19.2271. [DOI] [PubMed] [Google Scholar]
- 52.Buono F, Crispo S, Pagano G, Rengo G, Petitto M, Grieco F, Trimarco B, Morisco C. Determinants of left ventricular hypertrophy in patients with recent diagnosis of essential hypertension. J Hypertens. 2014;32:166–173. doi: 10.1097/HJH.0b013e328365c87d. [DOI] [PubMed] [Google Scholar]
- 53.Chrostowska M, Szyndler A, Hoffmann M, Narkiewicz K. Impact of obesity on cardiovascular health. Best Pract Res Clin Endocrinol Metab. 2013;27:147–156. doi: 10.1016/j.beem.2013.01.004. [DOI] [PubMed] [Google Scholar]
- 54.de Simone G. Morbid obesity and left ventricular geometry. Hypertension. 2007;49:7–9. doi: 10.1161/01.HYP.0000251714.60547.06. [DOI] [PubMed] [Google Scholar]
- 55**.Owan T, Avelar E, Morley K, Jiji R, Hall N, Krezowski J, Gallagher J, Williams Z, Preece K, Gundersen N, Strong MB, Pendleton RC, Segerson N, Cloward TV, Walker JM, Farney RJ, Gress RE, Adams TD, Hunt SC, Litwin SE. Favorable changes in cardiac geometry and function following gastric bypass surgery: 2-year follow-up in the utah obesity study. J Am Coll Cardiol. 2011;57:732–739. doi: 10.1016/j.jacc.2010.10.017. [This study provides empiric evidence of the reversibility of cardiac changes associated with obesity.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Luaces M, Cachofeiro V, Garcia-Munoz-Najar A, Medina M, Gonzalez N, Cancer E, Rodriguez-Robles A, Canovas G, Antequera-Perez A. Anatomical and functional alterations of the heart in morbid obesity. Changes after bariatric surgery. Rev Esp Cardiol (Engl) 2012;65:14–21. doi: 10.1016/j.recesp.2011.06.018. [DOI] [PubMed] [Google Scholar]
- 57.Cuspidi C, Rescaldani M, Sala C, Grassi G. Left-ventricular hypertrophy and obesity: A systematic review and meta-analysis of echocardiographic studies. J Hypertens. 2014;32:16–25. doi: 10.1097/HJH.0b013e328364fb58. [DOI] [PubMed] [Google Scholar]
- 58.Foley RN, Parfrey PS, Harnett JD, Kent GM, Martin CJ, Murray DC, Barre PE. Clinical and echocardiographic disease in patients starting end-stage renal disease therapy. Kidney Int. 1995;47:186–192. doi: 10.1038/ki.1995.22. [DOI] [PubMed] [Google Scholar]
- 59.Schiffrin EL, Lipman ML, Mann JF. Chronic kidney disease: Effects on the cardiovascular system. Circulation. 2007;116:85–97. doi: 10.1161/CIRCULATIONAHA.106.678342. [DOI] [PubMed] [Google Scholar]
- 60.Grabysa R, Wankowicz Z. Echocardiographic markers of left ventricular dysfunction among men with uncontrolled hypertension and stage 3 chronic kidney disease. Med Sci Monit. 2013;19:838–845. doi: 10.12659/MSM.889586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Vakili BA, Okin PM, Devereux RB. Prognostic implications of left ventricular hypertrophy. Am Heart J. 2001;141:334–341. doi: 10.1067/mhj.2001.113218. [DOI] [PubMed] [Google Scholar]
- 62.Foley RN, Curtis BM, Randell EW, Parfrey PS. Left ventricular hypertrophy in new hemodialysis patients without symptomatic cardiac disease. Clin J Am Soc Nephrol. 2010;5:805–813. doi: 10.2215/CJN.07761109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hashimoto J, Westerhof BE, Westerhof N, Imai Y, O'Rourke MF. Different role of wave reflection magnitude and timing on left ventricular mass reduction during antihypertensive treatment. J Hypertens. 2008;26:1017–1024. doi: 10.1097/HJH.0b013e3282f62a9b. [DOI] [PubMed] [Google Scholar]
- 64.Kobayashi S, Yano M, Kohno M, Obayashi M, Hisamatsu Y, Ryoke T, Ohkusa T, Yamakawa K, Matsuzaki M. Influence of aortic impedance on the development of pressure-overload left ventricular hypertrophy in rats. Circulation. 1996;94:3362–3368. doi: 10.1161/01.cir.94.12.3362. [DOI] [PubMed] [Google Scholar]
- 65.Lai S, Coppola B, Dimko M, Galani A, Innico G, Frassetti N, Mariotti A. Vitamin d deficiency, insulin resistance, and ventricular hypertrophy in the early stages of chronic kidney disease. Ren Fail. 2014;36:58–64. doi: 10.3109/0886022X.2013.832308. [DOI] [PubMed] [Google Scholar]
- 66.Martinez-Vea A, Marcas L, Bardaji A, Romeu M, Gutierrez C, Garcia C, Compte T, Nogues R, Peralta C, Giralt M. Role of oxidative stress in cardiovascular effects of anemia treatment with erythropoietin in predialysis patients with chronic kidney disease. Clin Nephrol. 2012;77:171–181. doi: 10.5414/cn107309. [DOI] [PubMed] [Google Scholar]
- 67.Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Battistelli M, Bartoccini C, Santucci A, Santucci C, Reboldi G, Porcellati C. Adverse prognostic significance of concentric remodeling of the left ventricle in hypertensive patients with normal left ventricular mass. J Am Coll Cardiol. 1995;25:871–878. doi: 10.1016/0735-1097(94)00424-O. [DOI] [PubMed] [Google Scholar]
- 68.Pierdomenico SD, Lapenna D, Bucci A, Manente BM, Cuccurullo F, Mezzetti A. Prognostic value of left ventricular concentric remodeling in uncomplicated mild hypertension. Am J Hypertens. 2004;17:1035–1039. doi: 10.1016/j.amjhyper.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 69.Muiesan ML, Salvetti M, Monteduro C, Bonzi B, Paini A, Viola S, Poisa P, Rizzoni D, Castellano M, Agabiti-Rosei E. Left ventricular concentric geometry during treatment adversely affects cardiovascular prognosis in hypertensive patients. Hypertension. 2004;43:731–738. doi: 10.1161/01.HYP.0000121223.44837.de. [DOI] [PubMed] [Google Scholar]
- 70*.Apostolakis S, Sullivan RM, Olshansky B, Lip GY. Left ventricular geometry and outcomes in patients with atrial fibrillation: The affirm trial. Int J Cardiol. 2014;170:303–308. doi: 10.1016/j.ijcard.2013.11.002. [This study demonstrates that even in a population at high-risk for cardiovascular events, hypertension-associated changes in cardiac structure provides independent prognostic information.] [DOI] [PubMed] [Google Scholar]
- 71.Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Gattobigio R, Zampi I, Santucci A, Santucci C, Reboldi G, Porcellati C. Prognostic value of left ventricular mass and geometry in systemic hypertension with left ventricular hypertrophy. Am J Cardiol. 1996;78:197–202. doi: 10.1016/s0002-9149(96)90395-1. [DOI] [PubMed] [Google Scholar]
- 72.Ghali JK, Liao Y, Cooper RS. Influence of left ventricular geometric patterns on prognosis in patients with or without coronary artery disease. J Am Coll Cardiol. 1998;31:1635–1640. doi: 10.1016/s0735-1097(98)00131-4. [DOI] [PubMed] [Google Scholar]
- 73.Krumholz HM, Larson M, Levy D. Prognosis of left ventricular geometric patterns in the framingham heart study. J Am Coll Cardiol. 1995;25:879–884. doi: 10.1016/0735-1097(94)00473-4. [DOI] [PubMed] [Google Scholar]
- 74.Velagaleti RS, Gona P, Pencina MJ, Aragam J, Wang TJ, Levy D, D'Agostino RB, Lee DS, Kannel WB, Benjamin EJ, Vasan RS. Left ventricular hypertrophy patterns and incidence of heart failure with preserved versus reduced ejection fraction. Am J Cardiol. 2014;113:117–122. doi: 10.1016/j.amjcard.2013.09.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75**.Gaasch WH, Zile MR. Left ventricular structural remodeling in health and disease: With special emphasis on volume, mass, and geometry. J Am Coll Cardiol. 2011;58:1733–1740. doi: 10.1016/j.jacc.2011.07.022. [A comprehensive review of the importance of considering geometric cardiac changes in a wide spectrum of cardiovascular diseases.] [DOI] [PubMed] [Google Scholar]
- 76.Khouri MG, Peshock RM, Ayers CR, de Lemos JA, Drazner MH. A 4-tiered classification of left ventricular hypertrophy based on left ventricular geometry: The dallas heart study. Circ Cardiovasc Imaging. 2010;3:164–171. doi: 10.1161/CIRCIMAGING.109.883652. [DOI] [PubMed] [Google Scholar]
- 77*.Bang CN, Gerdts E, Aurigemma GP, Boman K, Dahlof B, Roman MJ, Kober L, Wachtell K, Devereux RB. Systolic left ventricular function according to left ventricular concentricity and dilatation in hypertensive patients: The losartan intervention for endpoint reduction in hypertension study. J Hypertens. 2013;31:2060–2068. doi: 10.1097/HJH.0b013e328362bbd6. [Echocardiographic substudy of a clinical trial demonstrating that including left ventricle volume in the classification of cardiac geometry can improve the detection of systolic dysfunction in hypertensive patients.] [DOI] [PubMed] [Google Scholar]
- 78.Bella JN, Palmieri V, Roman MJ, Liu JE, Welty TK, Lee ET, Fabsitz RR, Howard BV, Devereux RB. Mitral ratio of peak early to late diastolic filling velocity as a predictor of mortality in middle-aged and elderly adults: The strong heart study. Circulation. 2002;105:1928–1933. doi: 10.1161/01.cir.0000015076.37047.d9. [DOI] [PubMed] [Google Scholar]
- 79.Redfield MM, Jacobsen SJ, Burnett JC, Jr., Mahoney DW, Bailey KR, Rodeheffer RJ. Burden of systolic and diastolic ventricular dysfunction in the community: Appreciating the scope of the heart failure epidemic. Jama. 2003;289:194–202. doi: 10.1001/jama.289.2.194. [DOI] [PubMed] [Google Scholar]
- 80.de Simone G, Kitzman DW, Chinali M, Oberman A, Hopkins PN, Rao DC, Arnett DK, Devereux RB. Left ventricular concentric geometry is associated with impaired relaxation in hypertension: The hypergen study. Eur Heart J. 2005;26:1039–1045. doi: 10.1093/eurheartj/ehi019. [DOI] [PubMed] [Google Scholar]
- 81.Effects of perindopril-indapamide on left ventricular diastolic function and mass in patients with type 2 diabetes: The advance echocardiography substudy. J Hypertens. 2011;29:1439–1447. doi: 10.1097/HJH.0b013e3283480fe9. [DOI] [PubMed] [Google Scholar]
- 82.Sharp AS, Tapp RJ, Thom SA, Francis DP, Hughes AD, Stanton AV, Zambanini A, O'Brien E, Chaturvedi N, Lyons S, Byrd S, Poulter NR, Sever PS, Mayet J. Tissue doppler e/e' ratio is a powerful predictor of primary cardiac events in a hypertensive population: An ascot substudy. Eur Heart J. 2010;31:747–752. doi: 10.1093/eurheartj/ehp498. [DOI] [PubMed] [Google Scholar]
- 83.Wachtell K, Smith G, Gerdts E, Dahlof B, Nieminen MS, Papademetriou V, Bella JN, Ibsen H, Rokkedal J, Devereux RB. Left ventricular filling patterns in patients with systemic hypertension and left ventricular hypertrophy (the life study). Losartan intervention for endpoint. Am J Cardiol. 2000;85:466–472. doi: 10.1016/s0002-9149(99)00773-0. [DOI] [PubMed] [Google Scholar]
- 84.Pearson AC, Labovitz AJ, Mrosek D, Williams GA, Kennedy HL. Assessment of diastolic function in normal and hypertrophied hearts: Comparison of doppler echocardiography and m-mode echocardiography. Am Heart J. 1987;113:1417–1425. doi: 10.1016/0002-8703(87)90657-0. [DOI] [PubMed] [Google Scholar]
- 85.Douglas PS, Berko B, Lesh M, Reichek N. Alterations in diastolic function in response to progressive left ventricular hypertrophy. J Am Coll Cardiol. 1989;13:461–467. doi: 10.1016/0735-1097(89)90527-5. [DOI] [PubMed] [Google Scholar]
- 86.Chahal NS, Lim TK, Jain P, Chambers JC, Kooner JS, Senior R. New insights into the relationship of left ventricular geometry and left ventricular mass with cardiac function: A population study of hypertensive subjects. Eur Heart J. 2010;31:588–594. doi: 10.1093/eurheartj/ehp490. [DOI] [PubMed] [Google Scholar]
- 87.Abhayaratna WP, Seward JB, Appleton CP, Douglas PS, Oh JK, Tajik AJ, Tsang TS. Left atrial size: Physiologic determinants and clinical applications. J Am Coll Cardiol. 2006;47:2357–2363. doi: 10.1016/j.jacc.2006.02.048. [DOI] [PubMed] [Google Scholar]
- 88.Tsioufis C, Stougiannos P, Taxiarchou E, Skiadas I, Chatzis D, Thomopoulos C, Lalos S, Stefanadis C, Kallikazaros I. The interplay between haemodynamic load, brain natriuretic peptide and left atrial size in the early stages of essential hypertension. J Hypertens. 2006;24:965–972. doi: 10.1097/01.hjh.0000222768.15100.00. [DOI] [PubMed] [Google Scholar]
- 89.Cuspidi C, Rescaldani M, Sala C. Prevalence of echocardiographic left-atrial enlargement in hypertension: A systematic review of recent clinical studies. Am J Hypertens. 2013;26:456–464. doi: 10.1093/ajh/hpt001. [DOI] [PubMed] [Google Scholar]
- 90.Kizer JR, Bella JN, Palmieri V, Liu JE, Best LG, Lee ET, Roman MJ, Devereux RB. Left atrial diameter as an independent predictor of first clinical cardiovascular events in middle-aged and elderly adults: The strong heart study (shs). Am Heart J. 2006;151:412–418. doi: 10.1016/j.ahj.2005.04.031. [DOI] [PubMed] [Google Scholar]
- 91.Verdecchia P, Angeli F, Gattobigio R, Sardone M, Porcellati C. Asymptomatic left ventricular systolic dysfunction in essential hypertension: Prevalence, determinants, and prognostic value. Hypertension. 2005;45:412–418. doi: 10.1161/01.HYP.0000154822.37141.f6. [DOI] [PubMed] [Google Scholar]
- 92.The solvd investigattors Effect of enalapril on mortality and the development of heart failure in asymptomatic patients with reduced left ventricular ejection fractions. N Engl J Med. 1992;327:685–691. doi: 10.1056/NEJM199209033271003. [DOI] [PubMed] [Google Scholar]
- 93.Aurigemma GP, Silver KH, Priest MA, Gaasch WH. Geometric changes allow normal ejection fraction despite depressed myocardial shortening in hypertensive left ventricular hypertrophy. J Am Coll Cardiol. 1995;26:195–202. doi: 10.1016/0735-1097(95)00153-q. [DOI] [PubMed] [Google Scholar]
- 94.de Simone G, Devereux RB, Koren MJ, Mensah GA, Casale PN, Laragh JH. Midwall left ventricular mechanics. An independent predictor of cardiovascular risk in arterial hypertension. Circulation. 1996;93:259–265. doi: 10.1161/01.cir.93.2.259. [DOI] [PubMed] [Google Scholar]
- 95.Narayanan A, Aurigemma GP, Chinali M, Hill JC, Meyer TE, Tighe DA. Cardiac mechanics in mild hypertensive heart disease: A speckle-strain imaging study. Circ Cardiovasc Imaging. 2009;2:382–390. doi: 10.1161/CIRCIMAGING.108.811620. [DOI] [PubMed] [Google Scholar]
- 96.Kosmala W, Plaksej R, Strotmann JM, Weigel C, Herrmann S, Niemann M, Mende H, Stork S, Angermann CE, Wagner JA, Weidemann F. Progression of left ventricular functional abnormalities in hypertensive patients with heart failure: An ultrasonic two-dimensional speckle tracking study. J Am Soc Echocardiogr. 2008;21:1309–1317. doi: 10.1016/j.echo.2008.10.006. [DOI] [PubMed] [Google Scholar]
- 97.Leggio M, Sgorbini L, Pugliese M, Mazza A, Bendini MG, Fera MS, Giovannini E, Leggio F. Systo-diastolic ventricular function in patients with hypertension: An echocardiographic tissue doppler imaging evaluation study. Int J Cardiovasc Imaging. 2007;23:177–184. doi: 10.1007/s10554-006-9139-y. [DOI] [PubMed] [Google Scholar]
- 98.Rosen BD, Edvardsen T, Lai S, Castillo E, Pan L, Jerosch-Herold M, Sinha S, Kronmal R, Arnett D, Crouse JR, 3rd, Heckbert SR, Bluemke DA, Lima JA. Left ventricular concentric remodeling is associated with decreased global and regional systolic function: The multi-ethnic study of atherosclerosis. Circulation. 2005;112:984–991. doi: 10.1161/CIRCULATIONAHA104.500488. [DOI] [PubMed] [Google Scholar]
- 99.de Simone G, Kitzman DW, Palmieri V, Liu JE, Oberman A, Hopkins PN, Bella JN, Rao DC, Arnett DK, Devereux RB. Association of inappropriate left ventricular mass with systolic and diastolic dysfunction: The hypergen study. Am J Hypertens. 2004;17:828–833. doi: 10.1016/j.amjhyper.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 100*.Cuspidi C, Sala C, Muiesan ML, De Luca N, Schillaci G. Right ventricular hypertrophy in systemic hypertension: An updated review of clinical studies. J Hypertens. 2013;31:858–865. doi: 10.1097/HJH.0b013e32835f17e5. [A recent review that calls attention to the impact of hypertension on the right ventricle.] [DOI] [PubMed] [Google Scholar]
- 101.Cuspidi C, Negri F, Giudici V, Valerio C, Meani S, Sala C, Esposito A, Masaidi M, Zanchetti A, Mancia G. Prevalence and clinical correlates of right ventricular hypertrophy in essential hypertension. J Hypertens. 2009;27:854–860. doi: 10.1097/HJH.0b013e328324eda0. [DOI] [PubMed] [Google Scholar]
- 102.Ivanovic BA, Tadic MV, Celic VP. To dip or not to dip? The unique relationship between different blood pressure patterns and cardiac function and structure. J Hum Hypertens. 2013;27:62–70. doi: 10.1038/jhh.2011.83. [DOI] [PubMed] [Google Scholar]
- 103.Lourenco AP, Roncon-Albuquerque R,, Jr., Bras-Silva C, Faria B, Wieland J, Henriques-Coelho T, Correia-Pinto J, Leite-Moreira AF. Myocardial dysfunction and neurohumoral activation without remodeling in left ventricle of monocrotaline-induced pulmonary hypertensive rats. Am J Physiol Heart Circ Physiol. 2006;291:H1587–1594. doi: 10.1152/ajpheart.01004.2005. [DOI] [PubMed] [Google Scholar]
- 104.Laks MM, Morady F. Norepinephrine--the myocardial hypertrophy hormone? Am Heart J. 1976;91:674–675. doi: 10.1016/s0002-8703(76)80156-1. [DOI] [PubMed] [Google Scholar]
- 105.Tadic M, Cuspidi C, Suzic-Lazic J, Andric A, Stojcevski B, Ivanovic B, Hot S, Scepanovic R, Celic V. Is there a relationship between right-ventricular and right atrial mechanics and functional capacity in hypertensive patients? J Hypertens. 2014 doi: 10.1097/HJH.0000000000000102. [DOI] [PubMed] [Google Scholar]
- 106**.Barron AJ, Hughes AD, Sharp A, Baksi AJ, Surendran P, Jabbour RJ, Stanton A, Poulter N, Fitzgerald D, Sever P, O'Brien E, Thom S, Mayet J. Long-term antihypertensive treatment fails to improve e/e' despite regression of left ventricular mass: An anglo-scandinavian cardiac outcomes trial substudy. Hypertension. 2014;63:252–258. doi: 10.1161/HYPERTENSIONAHA.113.01360. [An echocardiographic substudy of a hypertension therapeutic trial demonstrating a divergent effect of antihypertensive treatment on left ventricle hypertrophy and diastolic function.] [DOI] [PubMed] [Google Scholar]
- 107.Fagard RH, Celis H, Thijs L, Wouters S. Regression of left ventricular mass by antihypertensive treatment: A meta-analysis of randomized comparative studies. Hypertension. 2009;54:1084–1091. doi: 10.1161/HYPERTENSIONAHA.109.136655. [DOI] [PubMed] [Google Scholar]
- 108.Wachtell K, Dahlof B, Rokkedal J, Papademetriou V, Nieminen MS, Smith G, Gerdts E, Boman K, Bella JN, Devereux RB. Change of left ventricular geometric pattern after 1 year of antihypertensive treatment: The losartan intervention for endpoint reduction in hypertension (life) study. Am Heart J. 2002;144:1057–1064. doi: 10.1067/mhj.2002.126113. [DOI] [PubMed] [Google Scholar]
- 109.Solomon SD, Janardhanan R, Verma A, Bourgoun M, Daley WL, Purkayastha D, Lacourciere Y, Hippler SE, Fields H, Naqvi TZ, Mulvagh SL, Arnold JM, Thomas JD, Zile MR, Aurigemma GP. Effect of angiotensin receptor blockade and antihypertensive drugs on diastolic function in patients with hypertension and diastolic dysfunction: A randomised trial. Lancet. 2007;369:2079–2087. doi: 10.1016/S0140-6736(07)60980-5. [DOI] [PubMed] [Google Scholar]
- 110.Solomon SD, Verma A, Desai A, Hassanein A, Izzo J, Oparil S, Lacourciere Y, Lee J, Seifu Y, Hilkert RJ, Rocha R, Pitt B. Effect of intensive versus standard blood pressure lowering on diastolic function in patients with uncontrolled hypertension and diastolic dysfunction. Hypertension. 2010;55:241–248. doi: 10.1161/HYPERTENSIONAHA.109.138529. [DOI] [PubMed] [Google Scholar]
- 111.Almuntaser I, Mahmud A, Brown A, Murphy R, King G, Crean P, Feely J. Blood pressure control determines improvement in diastolic dysfunction in early hypertension. Am J Hypertens. 2009;22:1227–1231. doi: 10.1038/ajh.2009.173. [DOI] [PubMed] [Google Scholar]
- 112.Diez J, Frohlich ED. A translational approach to hypertensive heart disease. Hypertension. 2010;55:1–8. doi: 10.1161/HYPERTENSIONAHA.109.141887. [DOI] [PubMed] [Google Scholar]
- 113.Burchfield JS, Xie M, Hill JA. Pathological ventricular remodeling: Mechanisms: Part 1 of 2. Circulation. 2013;128:388–400. doi: 10.1161/CIRCULATIONAHA.113.001878. [DOI] [PMC free article] [PubMed] [Google Scholar]