Abstract
The benefits of early mobilization for adult patients in the intensive care unit (ICU) are reduced length of ICU and hospital stays, fewer readmissions to the ICU, decreased duration of mechanical ventilation, fewer days of detrimental bedrest, minimal adverse or unsafe events, and improved walking distance. Because there are no available tools to specifically measure mobility status of patients in the ICU setting, there is an urgent need to create a reliable tool that measures and standardizes the assessment of mobility status for these patients. The purpose of this study was to describe the development of this novel ICU-specific tool to assess a patient’s mobility status, examine the initial reliability of the tool, and address its clinical application. The Perme ICU Score was quickly and easily administered by physical therapists. Overall, the inter-rater agreement was 94%. A total of six items had kappa values of < .6, and these low scores may have been the result of the procedure to collect inter-rater scores, wherein one rater assisted with the activity while a second rater observed. In order to improve reliability, the authors developed directions to standardize the assessment. The Perme ICU Mobility Score is a tool developed to measure the patient’s mobility status starting with the ability to follow commands and culminating in the distance walked in two minutes. Preliminary data suggest that the validity of this tool is supported by expert concurrence, its overall reliability is high, and its clinical use is acceptable.
Keywords: outcomes, assessment, critical care, mobility, early ambulation, intensive care unit, physical therapy, early mobilization

Introduction
There are many benefits of early mobilization for adult patients in the ICU, including reduced length of ICU and hospital stays and, therefore, fewer days of detrimental bedrest; fewer ICU readmissions; decreased duration of mechanical ventilation; minimal adverse or unsafe events; and improved walking distance.1-14 In a study by Bailey et al., patients treated with an early activity protocol were able to walk more than 100 feet at the time of ICU discharge, and patients considered ambulation to be important to meet their goal of returning home.2 In fact, early mobilization is advocated as a treatment to reduce ICU-acquired weakness and delirium.15, 16 Emphasis should be placed on progressive mobility, individual functional capability, and ambulation of patients who meet specific criteria.17
Patients in the ICU who receive early mobilization have had variable functional responses.4, 18, 19 It is possible that this variability may be a result of the different tools used to capture function. In many of the ICU studies related to mobility interventions, the tools used to measure mobility status were not designed for patients tethered to tubes and lines, nor were they designed to detect changes in function in critically ill patients.
Several functional mobility tools have been used in published studies, including the Functional Independence Measure (FIM),20 Katz Index of Independence in Activities of Daily Living,21 Barthel Index,22 Acute Care Index of Function,23 University of Rochester Acute Care Evaluation,24 Physical Function ICU Test,25 and Functional Status Score for Intensive Care Unit (FSS-ICU).26 However, these tools are not sensitive to measuring ICU mobility status over the course of ICU stay or in recognizing limitations, where equipment specifically related to ICU care could potentially be barriers to progressive mobility.
There is an urgent need to create a reliable tool that specifically measures and standardizes the assessment of mobility status for patients in the ICU. The purpose of this paper is to describe the development of this novel ICU-specific mobility status measurement tool, examine the reliability of the tool, and address its clinical application.
Method
Development of the Perme ICU Mobility Score
The Perme ICU Mobility Score was developed to measure a patient’s mobility status starting with the ability to follow commands and culminating in the distance walked in 2 minutes. Lack of a specific tool to measure mobility status, specifically walking mobility, of patients in the ICU was the impetus for developing the Perme ICU Mobility Score. The sequence of items was organized using a systematic approach based on the progression of mobility activities routinely used by physical therapists when mobilizing patients. The initial version of the tool was used repeatedly in an informal manner over several years, with multiple changes made to address issues and improve clarity and applicability. Expert input from an intensivist, physical therapists, occupational therapists, registered nurses, and a statistician was used to support validity in the tool’s current form and throughout its refinement.
The Perme ICU Mobility Score presented in Figure 1A and 1B ranges from 0 to 32. The score is derived from 15 items grouped in 7 categories: mental status, potential mobility barriers, functional strength, bed mobility, transfers, gait, and endurance. The score uses a maximum range of 2 to 4 points for each of the 15 items, and it provides a total score that reflects the patient’s mobility status at one particular moment in time. A high score indicates few potential mobility barriers and decreased assistance whereas a low score indicates more potential barriers to mobility and more assistance needed for mobility.
Figure 1A.
Perme Intensive Care Unit Mobility Score Instructions.
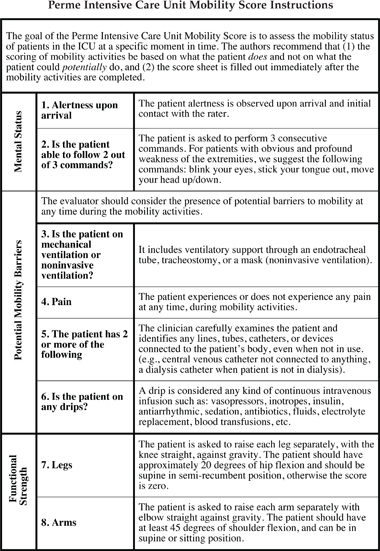
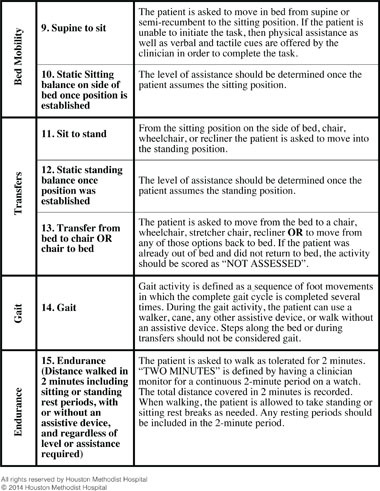
Figure 1B.
Perme ICU Mobility Score.
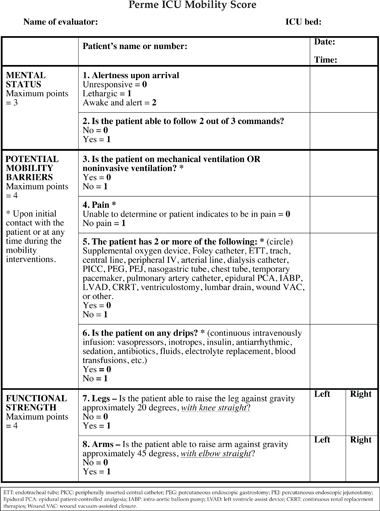

The categories were designed to reflect the impaired mobility of patients in the ICU, which can stem from a variety of factors including but not limited to severity of critical illness, mental status, equipment specifically related to ICU care, and neuromuscular deficits. The items included in the “mental status” category are variable levels of arousal and ability to follow commands, which reflect the patient’s ability to participate in planned mobility activities. The “potential mobility barriers” category identifies pain, the use of a ventilator, multiple lines and tubes routinely used in ICU, and continuous infusion of fluids or medications. This category was included because patients can be mobilized even in the presence of one or more of the above items; however, it is less likely that early mobility will occur under these circumstances.
It is possible that a patient who is able to move limbs against gravity will have the functional strength necessary for progressive mobility. “Functional strength” focused on the ability to raise arms and legs against gravity.3, 20, 21 Based on the Oxford Scale for muscle strength testing, patients should be able to raise arms and legs with a score of at least 3 out of 5.27 The upper and lower extremities, as well as the right and left sides of the body, were addressed separately to detect individual strength impairments in cases such as stroke or spinal cord injury. It is important to note that a patient should have approximately 20 degrees of hip flexion and 45 degrees of shoulder flexion in order to complete items 7 and 8 of the Perme ICU Mobility Score.
“Bed mobility” measured a patient’s ability to move from a supine or semirecumbent position to sitting and the sitting balance on the side of the bed.
It is imperative that patients have enough head and trunk control to start standing activities. The “transfers” category addressed a patient’s ability to move from a sitting position to standing at the side of the bed, static standing balance, and the ability to transfer from the bed to various surfaces including a chair, wheelchair, bedside commode, or recliner.
The “gait” category assessed a patient’s ability to walk using any assistive devices, such as a walker or cane, or without an assistive device.
The “endurance” category assessed the distance walked in 2 minutes. It measured the functional capacity by addressing the total distance covered after walking for 2 minutes, including sitting or standing rest periods, with or without an assistive device, and regardless of the level of assistance required.
The scoring system adopted for questions 1 to 8 was based on yes or no answers. For questions 9 to 14, a score of “0” was assigned for patients who needed total assistance (< 25% of the effort) or when the activity did not occur. A score of “3” was assigned for patients who needed minimum assistance (> 75% of the effort) or when the activity occurred with supervision. Item 15 was scored from “0” to “3” based on the distance walked in 2 minutes.
Subjects
During a period of 8 weeks, from October to November 2012, we observed consecutive patients in the 40-bed cardiovascular intensive care unit (CVICU) at The Methodist Hospital in Houston, Texas. We included 35 patients to provide 90% power to detect inter-rater reliability with a kappa coefficient of .9, using a two-tailed test with alpha set at .05. The inclusion criteria were CVICU patients older than 18 years who met the criteria to start physical therapy according to ICU guidelines.17
Data Collection
The Perme ICU Mobility Scores were collected on the physical therapy evaluation by two physical therapists with more than 5 years of clinical experience in the ICU. They did not participate in the development of this measurement tool but were trained and acquainted with it. One physical therapist assessed the patient and the other observed the entire process. Both raters completed the score sheet immediately after finishing the mobility interventions. To avoid bias, the score sheets were completed without any contact or discussion between raters. The same two raters collected data in the same fashion on all 35 patients included in the study.
Statistical Analysis
All analyses were performed with STATA version 11 (StataCorp LP; College Station, TX). Data are presented using descriptive statistics including median and interquartile range (IQR) for continuous data and percentages for categorical data. The kappa coefficient (k) was used to compare the observed and expected agreement of individual scores of each item on the Perme ICU Mobility Score. The kappa measures the degree of agreement between the scores and includes a correction for any agreement that may occur by chance.
Results
The 35 patients included in the study had a median IQR age of 67 (26-92) years. Eleven patients (31.42%) had a lung transplant with a median IQR ICU length of stay of 6 (1-24) days and hospital length of stay of 14 (4-31) days. The median IQR of the APACHE II score was 20 (7-31). In terms of discharge location, 18 (51.43%) patients were discharged home, 7 (20%) to long-term acute care, 4 (11.43%) to inpatient rehabilitation, 3 (8.57%) to skilled nursing facilities (SNF), and 3 (8.57%) expired while in the CVICU. All sample demographics are presented in Table 1. The agreement between the two raters for each item in the Perme ICU Mobility Score and kappa values are described in Table 2. The overall agreement between the raters had a median of 94.29% (68.57%-100%).
Table 1.
Patient Characteristics.
| Characteristics | Median / Percentage |
| Age (y) median (IQR) | 67 (26-92) |
| Gender Male Female |
60% 40% |
| BMI (kg/m2) | 28.3 (17.9-45.8) |
| Surgical Procedures Lung transplant Valve replacement Coronary artery bypass Aortic aneurysm repair LVADI Heart transplant Other |
11 (31.42%) 6 (17.14%) 5 (14.29%) 3 (8.58%) 2 (5.71%) 1 (2.85%) 7 (20%) |
| Length of Stay (LOS) median (IQR) ICU (days) Hospital (days) |
6 (1-24) 14 (4-31) |
| APACHE II score, median (IQR) | 20 (7-31) |
| Discharge Location Home LTACa Rehabb SNFc Otherd |
18 (51.43%) 7 (20%) 4 (11.43%) 3 (8.57%) 3 (8.57%) |
LTAC: long-term acute care; Rehab: inpatient rehabilitation; SNF: skilled nursing facility; Other: hospice, nursing home; LVAD: left ventricular assist device.
Table 2.
Inter-rater agreement.
| Number of ratings (n = 35) | ||||
| Item | Agreement | Non-Agreement | % Agreement | Kappa |
| 1 | 31 | 4 | 88.57% | 0.2784* |
| 2 | 34 | 1 | 97.14% | 0.0000* |
| 3 | 34 | 1 | 97.14% | 0.9057 |
| 4 | 32 | 3 | 88.57% | 0.7727 |
| 5 | 33 | 2 | 94.29% | 0.4776* |
| 6 | 34 | 1 | 97.14% | 0.9398 |
| 7 | 33 | 2 | 94.29% | 0.7941 |
| 8 | 34 | 1 | 97.14% | 0.8759 |
| 9 | 27 | 8 | 77.14% | 0.6631 |
| 10 | 26 | 9 | 71.43% | 0.4224* |
| 11 | 27 | 8 | 77.14% | 0.6721 |
| 12 | 24 | 11 | 68.57% | 0.5534* |
| 13 | 26 | 9 | 74.29% | 0.5987* |
| 14 | 34 | 1 | 97.14% | 0.9474 |
| 15 | 35 | 0 | 100% | 1.0000 |
*kappa values lower than 0.60.
Kappa values for specific items were as follows: no agreement (k = 0) for item 2, fair agreement (k = 0.21 to 0.40) for item 1, and moderate agreement (k = 0.41 to 0.60) for items 5, 10, 12, and 13. There was substantial agreement (k = 0.61 to 0.80) for items 4, 7, 9, and 11, and high agreement (k = 0.81 to 1.00) for items 3, 6, 8, 14, and 15.
Discussion
The Perme ICU Mobility Score was conceived as an ICU-specific tool to measure mobility status of patients with limited independent activities that often present during a critical illness. It is indicative of functional performance, and particularly the patient’s walking capability, in the ICU at a specific moment in time. Preliminary data suggest that the validity of this tool is supported by expert concurrence, its overall reliability is high, and its clinical use is acceptable.
Kasotakis et al.28 recently reported the use of the Surgical ICU Optimal Mobility Score (SOMS), a simple numeric scale that describes mobilization capacity of patients and an algorithm developed to select the optimal activity level. The results demonstrated it to be a reliable and valid tool to predict both mortality and ICU/hospital length of stay in surgical critically ill patients without preexisting impairment of mobility status. Its main use, however, is as an algorithm to advance activity rather than a tool to measure mobility status, as the Perme ICU Mobility Score was designed to do.
In a retrospective study, Montagnani et al. reported that all 18 items of the FIM could be used as a functional status outcome measure in a small group of patients with a tracheostomy and difficulty weaning from mechanical ventilation.29 While the FIM is possibly suitable for stable patients in a weaning unit, it has limited validity and usefulness in patients with unstable critical illness or during periods of complex monitoring in the ICU. The FIM has a strong focus on activities of daily living (ADL), which are not commonly performed or expected in the ICU.
The Functional Status Score for the Intensive Care Unit (FSS-ICU) included 3 of the 18 FIM items: grooming, bathing, and ambulation. Four other functional tasks relevant to the ICU setting were also included: rolling, transfer from supine to sit, sitting at the edge of bed, and transfer from sit to stand.13 This mix of ADL and ICU activities may lead to low scores that are not specific to ICU clinician expectations of functional performance. In contrast, all 15 activities in the Perme ICU Mobility Score are feasible for patients in the ICU. Activities such as wheelchair mobility and ADL were not included in the Perme ICU Mobility Score because an expert panel determined that wheelchair mobility activities and independent or assisted self-care activities are not routinely performed in the ICU.
The FIM and FSS-ICU use the same scoring system, with items scored according to the patient’s level of independence. Patients assigned a score of “0” are unable to perform the task. Each item is rated using a scale from 1 to 7, with a score of “1” corresponding to total assistance and “7” corresponding to complete independence.26, 30 The FIM scores “6” (modified independence) and “7” (complete independence) were not considered for the Perme ICU Mobility Score because we determined that patients in the ICU are not likely to have such a high level of independence. The scoring system adopted in the Perme ICU Mobility Score is similar to the FIM and FSS-ICU but instead ranges from 0 to 3.
Of the 15 items on the Perme ICU Mobility Score, 6 had kappa values of < .60, which is considered moderate to nonagreement.31 To improve agreement, we developed instructions to standardize the use of the tool. Future testing of reliability is planned using the new instructions sheet.
Item 2 in the Perme ICU Mobility Score had a kappa value of “0,” which means non-agreement between two raters. The authors decided to retain the item, as the real and expected agreement for this item was 97.17%. This represented just one patient with non-agreement, leading to the decision to keep the item in the tool. In our study, the “real agreement” between raters for all items had a median IQR percentage of 94.29% (68.57-100%), and items in the categories of “bed mobility” and “transfers” showed moderate agreement.
For the “bed mobility” category, the “supine to sit” item showed an agreement of 77.14% and “sitting balance on the side of bed” showed an agreement of 71.43%. For the “transfers” category, the “sit to stand” item showed an agreement of 77.14%, “standing balance” showed an agreement of 68.57%, and “transfer to chair” showed an agreement of 74.29%. One reason for the moderate agreement between raters in these items could be a different perception of patient’s effort, since one physical therapist assisted the patient while the other only observed without physically touching the patient. In the future, we plan to test the same patient repeatedly and randomize the two raters’ sequence of assisting versus observing.
The Perme ICU Mobility Score is a well-defined quantitative tool that provides a reliable assessment of an ICU patient’s mobility status. It is also practical in that it can be completed in just a few minutes at the end of mobility interventions. This is clinically relevant for clinicians, as it provides an objective evaluation of the mobility status in the ICU setting.
The tool is intended for use in any ICU population and in both clinical and research applications. However, in the present study the tool was only applied in a CVICU, which can be considered a limitation. Further studies are needed to test its validity, reliability, and applicability across different ICU populations.
Conclusion
The Perme ICU Mobility Score is a tool developed to measure the patient’s mobility status starting with the ability to follow commands and culminating in the distance walked in 2 minutes. Preliminary data suggest that the validity of this tool is supported by expert concurrence, its overall reliability is high, and its clinical use is acceptable.
Acknowledgements: The authors would like to thank Colleen Lettvin, Terry Throckmorton, and Sarah Holmer for their cooperation in this study. We also thank Catherine Currier-Buckingham and Sharon Cormier for administrative support.
Funding Statement
Funding/Support: The authors have no funding disclosures.
Footnotes
Conflict of Interest Disclosure: The authors have completed and submitted the Methodist DeBakey Cardiovascular Journal Conflict of Interest Statement and none were reported.
References
- 1.Perme CS, Southard RE, Joyce DL, Noon GP, Loebe M. Early mobilization of LVAD recipients who require prolonged mechanical ventilation. Tex Heart Inst J. 2006;33(2):130–3.. [PMC free article] [PubMed] [Google Scholar]
- 2.Bailey P, Thomsen GE, Spuhler VJ, Blair R, Jewkes J, Bezdjian L, et al. Early activity is feasible and safe in respiratory failure patients. Crit Care Med. 2007 Jan;35(1):139–45.. doi: 10.1097/01.CCM.0000251130.69568.87. [DOI] [PubMed] [Google Scholar]
- 3.Morris PE, Goad A, Thompson C, Taylor K, Harry B, Passmore L, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008 Aug;36(8):2238–43.. doi: 10.1097/CCM.0b013e318180b90e. [DOI] [PubMed] [Google Scholar]
- 4.Morris PE, Griffin L, Berry M, Thompson C, Hite RD, Winkelman C, et al. Receiving early mobility during an intensive care unit admission is a predictor of improved outcomes in acute respiratory failure. Am J Med Sci. 2011 May;341(5):373–7.. doi: 10.1097/MAJ.0b013e31820ab4f6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schweickert WD, Pohlman MC, Pohlman AS, Nigos C, Pawlik AJ, Esbrook CL, et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: a randomised controlled trial. Lancet. 2009 May 30;373(9678):1874–82.. doi: 10.1016/S0140-6736(09)60658-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nava S. Rehabilitation of patients admitted to a respiratory intensive care unit. Arch Phys Med Rehabil. 1998 Jul;79(7):849–54.. doi: 10.1016/s0003-9993(98)90369-0. [DOI] [PubMed] [Google Scholar]
- 7.Martin UJ, Hincapie L, Nimchuk M, Gaughan J, Criner GJ. Impact of whole-body rehabilitation in patients receiving chronic mechanical ventilation. Crit Care Med. 2005 Oct;33(10):2259–65.. doi: 10.1097/01.ccm.0000181730.02238.9b. [DOI] [PubMed] [Google Scholar]
- 8.Chiang LL, Wang LY, Wu CP, Wu HD, Wu YT. Effects of physical training on functional status in patients with prolonged mechanical ventilation. Phys Ther. 2006 Sep;86(9):1271–81.. doi: 10.2522/ptj.20050036. [DOI] [PubMed] [Google Scholar]
- 9.Chen S, Su CL, Wu YT, Wang LY, Wu CP, Wu HD, et al. Physical training is beneficial to functional status and survival in patients with prolonged mechanical ventilation. J Formos Med Assoc. 2011 Sep;110(9):572–9.. doi: 10.1016/j.jfma.2011.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Thomsen GE, Snow GL, Rodriguez L, Hopkins RO. Patients with respiratory failure increase ambulation after transfer to an intensive care unit where early activity is a priority. Crit Care Med. 2008 Apr;36(4):1119–24.. doi: 10.1097/CCM.0b013e318168f986. [DOI] [PubMed] [Google Scholar]
- 11.Stiller K, Lynch E, Phillips AC, Lambert P. Clinical education of physiotherapy students in Australia: perceptions of current models. Aust J Physiother. 2004;50(4):243–7.. doi: 10.1016/s0004-9514(14)60114-8. [DOI] [PubMed] [Google Scholar]
- 12.Stiller K, Phillips AC, Lambert P. The safety of mobilization and its effect on hemodynamic and respiratory status of intensive care patients. Physiother Theory Pract. 2004;20(3):175–85.. [Google Scholar]
- 13.Zanni JM, Korupolu R, Fan E, Pradhan P, Janjua K, Palmer JB, et al. Rehabilitation therapy and outcomes in acute respiratory failure: an observational pilot project. J Crit Care. 2010 Jun;25(2):254–62.. doi: 10.1016/j.jcrc.2009.10.010. [DOI] [PubMed] [Google Scholar]
- 14.Bahadur K, Jones G, Ntoumenopoulos G. An observational study of sitting out of bed in tracheosomised patients in the intensive care unit. Physiotherapy. 2008 Dec;94(4):300–5.. [Google Scholar]
- 15.Schweickert WD, Hall J. ICU-acquired weakness. Chest. 2007 May;131(5):1541–9.. doi: 10.1378/chest.06-2065. [DOI] [PubMed] [Google Scholar]
- 16.Barr J, Fraser GL, Puntillo K, Ely EW, Gélinas C, Dasta JF, et al. Clinical practice guidelines for the management of pain, agitation, and delirium in adult patients in the intensive care unit. Crit Care Med. 2013 Jan;41(1):263–306.. doi: 10.1097/CCM.0b013e3182783b72. [DOI] [PubMed] [Google Scholar]
- 17.Perme C, Chandrashekar R. Early mobility and walking program for patients in intensive care units: creating a standard of care. Am J Crit Care. 2009 May;18(3):212–21.. doi: 10.4037/ajcc2009598. [DOI] [PubMed] [Google Scholar]
- 18.Burtin C, Clerckx B, Robbeets C, Ferdinande P, Langer D, Troosters T, et al. Early exercise in critically ill patients enhances short-term functional recovery. Crit Care Med. 2009 Sep;37(9):2499–505.. doi: 10.1097/CCM.0b013e3181a38937. [DOI] [PubMed] [Google Scholar]
- 19.Browning L, Denehy L, Scholes RL. The quantity of early upright mobilization performed following upper abdominal surgery is low: an observational study. Aust J Physiother. 2007;53(1):47–52.. doi: 10.1016/s0004-9514(07)70061-2. [DOI] [PubMed] [Google Scholar]
- 20.Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. Adv Clin Rehabil. 1987;1:6–18.. [PubMed] [Google Scholar]
- 21.Katz S, Downs TD, Cash HR, Grotz RC. Progress in development of the index of ADL. Gerontologist. 1970 Spring;10(1):20–30.. doi: 10.1093/geront/10.1_part_1.20. [DOI] [PubMed] [Google Scholar]
- 22.Mahoney FI, Barthel DW. Functional evaluation: The Barthel Index. Md State Med J. 1965 Feb;14:61–5.. [PubMed] [Google Scholar]
- 23.Scherer SA, Hammerich AS. Outcomes in cardiopulmonary physical therapy: acute care index of function. Cardiopulm Phys Ther J. 2008 Sept;19(3):94–7.. [PMC free article] [PubMed] [Google Scholar]
- 24.DiCicco J, Whalen D. University of Rochester acute care evaluation: Development of a new functional outcome measure for the acute care setting. J Acute Care Phys Ther. 2010;1:14–20.. [Google Scholar]
- 25.Skinner EH, Berney S, Warrillow S, Denehy L. Development of a physical function outcome measure (PFIT) and a pilot exercise training protocol for use in intensive care. Crit Care Resusc. 2009 Jun;11(2):110–5.. [PubMed] [Google Scholar]
- 26.Thrush A, Rozek M, Dekerlegand JL. The clinical utility of the functional status score for the intensive care unit (FSS-ICU) at a long-term acute care hospital: a prospective cohort study. Phys Ther. 2012 Dec;92(12):1536–45.. doi: 10.2522/ptj.20110412. [DOI] [PubMed] [Google Scholar]
- 27.Daniels L, Worthingham C. Muscle Testing: Techniques of Manual Examination. Philadelphia: WB Saunders; 1995. [Google Scholar]
- 28.Kasotakis G, Schmidt U, Perry D, Grosse-Sundrup M, Benjamin J, Ryan C, et al. The surgical intensive care unit optimal mobility score predicts mortality and length of stay. Crit Care Med. 2012 Apr;40(4):1122–8.. doi: 10.1097/CCM.0b013e3182376e6d. [DOI] [PubMed] [Google Scholar]
- 29.Montagnani G, Vagheggini G, Panait Vlad E, Berrighi D, Pantani L, Ambrosino N. Use of the Functional Independence Measure in people for whom weaning from mechanical ventilation is difficult. Phys Ther. 2011 Jul;91(7):1109–15.. doi: 10.2522/ptj.20100369. [DOI] [PubMed] [Google Scholar]
- 30.Dodds TA, Martin DP, Stolov WC, Deyo RA. A validation of the functional independence measurement and its performance among rehabilitation inpatients. Arch Phys Med Rehabil. 1993 May;74(5):531–6.. doi: 10.1016/0003-9993(93)90119-u. [DOI] [PubMed] [Google Scholar]
- 31.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977 Mar;33(1):159–74.. [PubMed] [Google Scholar]


