Abstract
Objective
To measure discontinuation within 6 months among users of the levonorgestrel intrauterine system, copper intrauterine device (IUD), and etonogestrel implant, and identify baseline characteristics associated with early discontinuation.
Methods
This was an analysis of the Contraceptive CHOICE Project, a cohort study of 9,256 participants provided with no-cost contraception and followed with telephone interviews at 3 and 6 months. We used logistic regression to investigate characteristics associated with early discontinuation of the two IUDs and implant and described reasons for discontinuation.
Results
A total of 6,167 participants were eligible for this analysis. Follow-up data were available for 5,928 participants; 5,495 (93%) were using their method at 6 months and 433 (7%) had discontinued. Discontinuation rates were 7.3%, 8.0%, and 6.9% for the levonorgestrel intrauterine system, copper IUD, and implant, respectively. After adjusting for age, race, marital status, low socioeconomic status, and history of sexually transmitted infection, we found that single and divorced,/separated and widowed women were slightly more likely to discontinue compared to married women (ORadj 1.26, 95% CI 1.01, 1.59, and ORadj 1.62, 95% CI 1.11, 2.37, respectively). No other baseline characteristics, including younger age (14-19 years), were associated with early discontinuation. The most common reason given for discontinuation was cramping among IUD users and irregular or frequent bleeding among implant users.
Conclusion
Rates of discontinuation of long-acting reversible contraception at 6 months is low and not increased in adolescents and young women. IUDs and the implant should be considered as first-line contraceptive options among all women to reduce unintended pregnancy.
INTRODUCTION
Unintended pregnancy remains an important public health problem. Approximately 3 million unplanned or mistimed pregnancies occur each year in the United States.1 Despite a decrease worldwide,2 unintended pregnancy rates remain unchanged in the U.S.1,3 Increasing access to effective contraception may prevent the negative health and economic consequences associated with unplanned pregnancy.4
Long-acting reversible contraceptive (LARC) methods, including the intrauterine device (IUD) and subdermal implant, offer women the most effective protection against pregnancy. Adolescents and women who use oral contraceptive pills (OCPs), contraceptive patch, or vaginal ring have a 20-fold failure rate compared to women who use LARC methods.5 Results from the Contraceptive CHOICE Project (CHOICE) have shown that LARC methods have higher rates of continuation and satisfaction rates at 12 and 24 months compared to short-acting reversible contraception and that continuation is equally high among adolescent females.6-8 Despite these high rates of effectiveness and continuation, less than 10% of women in the United States currently use an IUD or implant compared to many European countries with higher rates of uptake.9,10
The American College of Obstetricians and Gynecologists has recommended LARC methods as first-line contraceptive options for both adults and adolescents.11,12 However, concerns among health care providers about rapid discontinuation of LARC methods, especially among adolescents, may discourage use.13 Other studies have demonstrated that contraceptive dissatisfaction contributes to early discontinuation. 14,15. Rates of LARC discontinuation at 6 months vary between 6 and 17% with cramping and changes in bleeding patterns commonly reported as reasons for removal of the IUD and implant.16-18 Our objective in this analysis was to measure 6-month discontinuation rates among users of the levonorgestrel intrauterine system, copper IUD, and etonogestrel implant and to investigate factors associated with early discontinuation of LARC methods.
MATERIALS AND METHODS
The methods of CHOICE have been previously described in detail;19 therefore, we present a brief review and detailed description of the procedures relevant to this analysis. CHOICE is a prospective cohort study of 9,256 adolescents and women who were provided with no-cost reversible contraception. The primary goal of the project was to promote the use of LARC methods and decrease the rate of unintended pregnancy. CHOICE was a convenience sample of adolescents and women living in the St. Louis area. Eligible participants were between 14 and 45 years of age, residents of St. Louis City or County, at risk for pregnancy and did not desire pregnancy in the next year, and willing to start a new contraceptive method. Participants completed follow-up surveys by telephone at 3 and 6 months and then every 6 months for 3 years (first 5,090 participants) or 2 years (remainder of the cohort). We enrolled participants at our university clinical research site and 13 partner community clinics. Participants who enrolled at the university research site were provided with standardized, comprehensive contraceptive counseling20. Participants who enrolled at partner clinics underwent the usual counseling for that site. All participants were offered screening for Neisseria gonorrhoeae and Chlamydia trachomatis infection at the time of enrollment with self-collected vaginal swabs. The study was approved by the Washington University Human Research Protection Office and written informed consent was obtained from participants prior to enrollment.
For inclusion in this analysis, participants must have received a LARC method at or within 3 months of enrollment. We obtained information about LARC method discontinuation from survey data and from our ancillary removal log (a separately maintained record of any participant who came to the university clinical research site for a removal, called to report a removal, or reported a removal during a follow-up telephone survey). Those who experienced an expulsion of an IUD were offered a replacement device. Participants who had a second IUD inserted within 28 days of the expulsion were defined as continuers in this analysis. In order to determine reasons for removal, two research assistants extracted and coded data regarding the reason for removal from the removal log and participant charts (D.G. and T.C.). Up to three reasons were coded for each participant. Codes were reviewed by the principal investigator (T.M.) and any discrepancies were resolved through discussion, chart review, and consensus. We then calculated frequencies for the primary reasons for requesting removal for each discontinuer.
Our analysis compared the baseline characteristics between 6-month continuers and discontinuers. Percentages and frequencies were calculated to compare early discontinuation rates among LARC users. Chi-square tests were used to compare categorical variables. Continuation at 6 months was evaluated between continuers and discontinuers for each LARC method. We investigated factors associated with discontinuation before 6 months using crude and adjusted logistic regression. We calculated odds ratios (OR) and 95% confidence intervals (CI). Any covariates that were significant in the crude analysis were included in the adjusted model. We planned a priori to include age in the final model as we hypothesized that adolescents and young women (aged 14 to 19) may have higher rates of early discontinuation of LARC methods. Interaction terms were used to test for significant relationships between race and age, low socioeconomic status (SES), and history of a sexually transmitted infection (STI). None of the interactions were found to be statistically significant and, therefore, were not included in the model. Statistical analyses were performed using SAS 9.2 software, and the significance level (alpha) was set at 0.05.
RESULTS
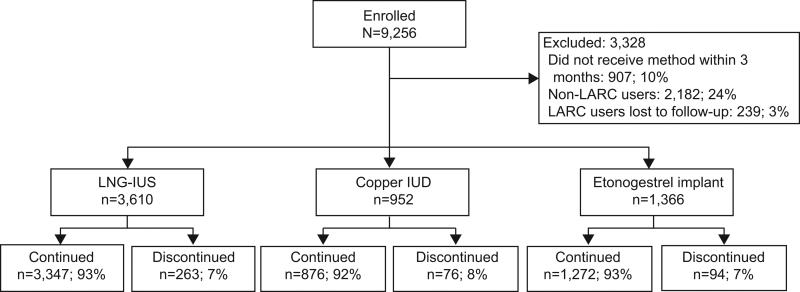
Among the 9,256 adolescents and women in the CHOICE cohort, there were 7074 participants who chose an IUD or an implant at baseline. Of these, 760 (8%) participants did not receive their baseline chosen method within the first 3 months and 147 (2%) started their method prior to enrollment leaving 6,167 participants eligible for this analysis. The participant flowchart is shown in Figure 1. There were 239 (3%) participants without any data about method use at 6 months and were considered lost to follow-up. These participants were more likely to have chosen the implant at baseline (34% compared to 23%, p<0.01), be of Hispanic ethnicity (8% compared to 5%, p=0.04), report low SES (70% compared to 59%, p<0.01), have higher parity (21% compared to 12%, p<0.01), and have reported a prior unintended pregnancy (75% compared to 67%, p=0.01) compared to those who followed up. They were also less likely to have been enrolled at the university clinical research site (46% compared to 68%, p<.01), have a college education (9% compared to 23%, p<0.01), and to be single (49% compared to 58%, p=0.03). Participants lost to follow-up were equally likely to be aged 14 to 19 years as those who followed up (14% for both groups). Therefore, a total of 5,928 participants met our inclusion criteria and had follow-up data available. Of these, 3,610 (61%) received the levonorgestrel intrauterine system, 952 (16%) chose the copper IUD, and 1,366 (23%) received the implant at or within 3 months of baseline. There were 5,495 (93%) participants who were still using their baseline LARC method at 6 months and were considered continuers. The remaining 433 (7%) had discontinued their baseline method within the first 6 months of use. When stratified by age, there was no significant differences in early discontinuation by LARC method between adolescents and young women (age 14-19 years) and older women (8.5% versus 7.1% respectively, p=0.72).
Figure 1.
Schematic of study population included and excluded from the analysis.
Table 1 compares the baseline characteristics between the continuers and discontinuers. Our overall sample was racially and ethnically diverse; 49% were black, and approximately 5% were of Hispanic ethnicity. There were 835 (14%) adolescents and young women aged 14-19 in our sample. A history of a prior unintended pregnancy was common, reported by 67% of the sample. Characteristics among continuers and discontinuers were similar except that discontinuers were less likely to be married (29% compared to 36%, p=0.01) and more likely to be black (55% compared to 48%, p=0.04), have low SES (63% compared to 58%, p=0.04), and to have reported a past STI (35% compared to 30%, p=0.02). Discontinuation rates at 6 months were similar across the three LARC methods; 7.3% of levonorgestrel intrauterine system users, 8.0% of copper IUD users, and 6.9% of implant users (p=0.60).
Table 1.
Baseline Demographic and Reproductive Characteristics of Continuers at 6 Months Compared to Discontinuers
| Total N= 5928 | Continuers at 6 Months n= 5495 | Discontinuers at 6 Months n= 433 | P | |
|---|---|---|---|---|
| Age | ||||
| 14-19 | 835 (14%) | 764 (14%) | 71 (16%) | 0.15 |
| 20+ | 5093 (86%) | 4731 (86%) | 362 (84%) | |
| Race | ||||
| Black | 2903 (49%) | 2666 (48%) | 237 (55%) | 0.04 |
| White | 2565 (43%) | 2400 (44%) | 165 (38%) | |
| Other | 460 (8%) | 429 (8%) | 31 (7%) | |
| Hispanic ethnicity | ||||
| Yes | 314 (5%) | 293 (5%) | 21 (5%) | 0.67 |
| No | 5614 (95%) | 5202 (95%) | 412 (95%) | |
| Marital Status (missing data = 5) | ||||
| Single/Never Married | 3407 (58%) | 3140 (57%) | 267 (62%) | 0.01 |
| Married/Living with Partner | 2097 (35%) | 1970 (36%) | 127 (29%) | |
| Separated/Divorced/Widowed | 419 (7%) | 380 (7%) | 39 (9%) | |
| Education (missing data = 2) | ||||
| High school or less | 2072 (35%) | 1915 (35%) | 157 (36%) | 0.11 |
| Some College | 2464 (42%) | 2272 (41%) | 192 (44%) | |
| College or more | 1390 (23%) | 1306 (24%) | 84 (20%) | |
| Low SES* (missing data = 1) | ||||
| Yes | 3475 (59%) | 3201 (58%) | 274 (63%) | 0.04 |
| No | 2452 (41%) | 2293 (42%) | 159 (37%) | |
| Insurance (missing data = 31) | ||||
| None | 2309 (39%) | 2148 (39%) | 161 (37%) | 0.17 |
| Private | 2564 (44%) | 2383 (44%) | 181 (42%) | |
| Public | 1024 (17%) | 935 (17%) | 89 (21%) | |
| Parity | ||||
| 0 | 2491 (42%) | 2308 (42%) | 183 (42%) | 0.46 |
| 1 | 1544 (26%) | 1437 (26%) | 107 (25%) | |
| 2 | 1165 (20%) | 1085 (20%) | 80 (18%) | |
| 3 or more | 728 (12%) | 665 (12%) | 63 (15%) | |
| Prior unintended pregnancy (missing data = 6) | ||||
| Yes | 3972 (67%) | 3675 (67%) | 297 (69%) | 0.44 |
| No | 1950 (33%) | 1815 (33%) | 135 (31%) | |
| History of STI† | ||||
| Yes | 1791 (30%) | 1639 (30%) | 152 (35%) | 0.02 |
| No | 4137 (70%) | 3856 (70%) | 281 (65%) | |
| BMI (missing data = 63) | ||||
| <18.5 | 76 (1%) | 69 (1%) | 7 (2%) | 0.82 |
| 18.5 – 24.9 | 2233 (38%) | 2077 (38%) | 156 (36%) | |
| 25 – 29.9 | 1566 (27%) | 1450 (27%) | 116 (27%) | |
| 30+ | 1990 (34%) | 1840 (34%) | 150 (35%) | |
| Baseline Method | ||||
| LNG-IUS | 3610 (61%) | 3347 (61%) | 263 (61%) | 0.60 |
| Copper IUD | 952 (16%) | 876 (16%) | 76 (17%) | |
| Implant | 1366 (23%) | 1272 (23%) | 94 (22%) |
SES – low socioeconomic status; STI – sexually transmitted infection; LNG-IUS – levonorgestrel intrauterine system; IUD – intrauterine device
Percents may not add up to 100% due to missing values.
Low SES defined as either receiving public assistance or reporting trouble paying for basic needs such as food, housing, transportation, or medical care.
History of STI included any history of gonorrhea, chlamydia, or trichomoniasis.
Data are n (%) unless otherwise specified.
Table 2 presents the results of the crude and adjusted logistic regression investigating participant characteristics associated with early discontinuation of any LARC method. In the crude model, we found that black participants were 29% more likely to discontinue their method early compared to white participants (OR 1.29, CI: 1.05, 1.59). Marital status, socioeconomic status, and history of STI were also associated with a slight increase in discontinuation. Therefore, we present both crude and adjusted odds ratios from our analyses. After adjusting for age, race, marital status, low SES, and past STI, we found that single (ORadj 1.26, 95% CI: 1.01, 1.59) and divorced, separated, and widowed (ORadj 1.62, 95% CI: 1.11, 2.37) participants were more likely to discontinue their LARC method by 6 months. Young age (14-19 years) was not associated with early discontinuation in either the crude or adjusted model (ORadj 1.16; 95% CI: 0.87, 1.54).
Table 2.
Crude and Adjusted Logistic Regression of Baseline Characteristics Associated With Early Discontinuation
| Crude Odds Ratio (95% CI) | Adjusted* Odds Ratio (95% CI) | |
|---|---|---|
| Age | ||
| 14-19 | 1.22 (0.93, 1.58) | 1.16 (0.87, 1.54) |
| 20+ | referent | referent |
| Race | ||
| Black | 1.29 (1.05, 1.59) | 1.12 (0.89, 1.41) |
| White | referent | referent |
| Other | 1.05 (0.71, 1.56) | 1.02 (0.68, 1.52) |
| Marital status | ||
| Single/never married | 1.32 (1.06, 1.64) | 1.26 (1.01, 1.59) |
| Married/living with partner | referent | Referent |
| Separated/divorced/widowed | 1.59 (1.09, 2.32) | 1.62 (1.11, 2.37) |
| Education | ||
| High school or less | 1.28 (0.97, 1.68) | -- |
| Some college | 1.31 (1.01, 1.71) | -- |
| 4+ years of college | referent | -- |
| Low socioeconomic status† | ||
| Yes | 1.23 (1.01, 1.51) | 1.20 (0.97, 1.49) |
| No | referent | referent |
| Insurance | ||
| None | 0.99 (0.79, 1.23) | -- |
| Private | referent | -- |
| Public | 1.25 (0.96, 1.63) | -- |
| Parity | ||
| 0 | referent | -- |
| 1 | 0.94 (0.73, 1.20) | -- |
| 2 | 0.93 (0.71, 1.22) | -- |
| 3 or more | 1.20 (0.89, 1.61) | -- |
| Prior unintended pregnancy | ||
| Yes | 1.09 (0.88, 1.34) | -- |
| No | referent | -- |
| History of STI‡ | ||
| Yes | 1.27 (1.04, 1.56) | 1.17 (0.94, 1.47) |
| No | referent | referent |
| BMI | ||
| <18.5 | 1.35 (0.61, 2.99) | -- |
| 18.5 – 24.9 | referent | -- |
| 25 – 29.9 | 1.07 (0.83, 1.37) | -- |
| 30+ | 1.09 (0.86, 1.37) | -- |
| LARC method | ||
| Levonorgestrel intrauterine system | 0.91 (0.69, 1.18) | -- |
| Copper IUD | referent | -- |
| Implant | 0.85 (0.62, 1.17) | -- |
Adjusted for age, race, marital status, low SES, and history of STI.
STI, sexually transmitted infection; BMI, body mass index; LARC, long-acting reversible contraceptive; IUD, intrauterine device.
Low socioeconomic status defined as either receiving public assistance or reporting trouble paying for basic needs such as food, housing, transportation, or medical care.
History of STI included any history of gonorrhea, chlamydia, or trichomoniasis.
Table 3 presents the most commonly reported reason for requesting removal of each of the LARC methods. Participants could report up to three reasons for discontinuation; however, we included only the primary or first reason given by each person for discontinuation during the follow-up surveys, telephone contact, or clinic visits as we assumed women would list their most bothersome complaint first. The most common reason for requesting removal among IUD users was pain or cramping; 41 (28%) levonorgestrel intrauterine system discontinuers and 18 (35%) copper IUD discontinuers (p=0.38). Complaints of heavy bleeding were most common among copper IUD discontinuers (17%). Removal for irregular or frequent bleeding was cited across all three LARC methods: 9% of levonorgestrel intrauterine system discontinuers, 19% of copper IUD discontinuers, and 53% of implant discontinuers (p-value for IUD comparison = 0.08; p-value for IUD and implant comparison <0.001). Only 3% of participants requested removal of their LARC method at or before 6 months due to desired pregnancy.
Table 3.
Most Common Reasons for Requesting Removal Prior to 6 Months of Use
| Levonorgestrel Intrauterine System | Copper IUD | Implant | ||||
|---|---|---|---|---|---|---|
| n=148* | % | n=52* | % | n=94 | % | |
| Pain/cramping | 41 | 27.7 | 18 | 34.6 | 0 | 0.0 |
| Irregular/Frequent bleeding | 14 | 9.5 | 10 | 19.2 | 50 | 53.2 |
| Heavy Bleeding | 3 | 2.0 | 9 | 17.3 | 0 | 0.0 |
| Acne | 13 | 8.8 | 0 | 0.0 | 4 | 4.3 |
| Mood changes | 8 | 5.4 | 0 | 0.0 | 4 | 4.3 |
| Vaginal symptoms (odor/discharge/itching) | 6 | 4.1 | 3 | 5.8 | 0 | 0.0 |
| Headache | 6 | 4.1 | 1 | 1.9 | 7 | 7.5 |
| Weight gain | 5 | 3.4 | 0 | 0.0 | 4 | 4.3 |
| Amenorrhea | 5 | 3.4 | 0 | 0.0 | 1 | 1.1 |
| Desires pregnancy | 5 | 3.4 | 0 | 0.0 | 3 | 3.2 |
| Desires permanent sterilization | 1 | 0.7 | 1 | 1.9 | 0 | 0.0 |
| Pain with intercourse | 0 | 0.0 | 1 | 1.9 | 0 | 0.0 |
| Private provider recommended removal | 5 | 3.4 | 3 | 5.8 | 1 | 1.1 |
| Hair Loss | 1 | 0.7 | 0 | 0.0 | 3 | 3.2 |
| Arm Pain | 0 | 0.0 | 0 | 0.0 | 4 | 4.3 |
| Other Complaints† | 35 | 23.7 | 6 | 11.5 | 13 | 13.8 |
115 levonorgestrel intrauterine system and 24 copper IUD expulsions were excluded.
IUD, intrauterine device.
Other complaints included decreased libido, fatigue, dizziness, IUD strings poking partner, pelvic infection, pain other than abdominal, allergic reaction, nausea or vomiting, perforation, fear of infertility, fear of foreign body, gastrointestinal complaints, nipple discharge, breast pain, excessive hair growth, hot flashes, and pregnancy.
DISCUSSION
Our study found low rates of discontinuation by 6 months across the three LARC methods which do not differ among adolescents and young women compared to older women. The only characteristic associated with early discontinuation in our sample was being unmarried, although the effect sizes were relatively small. Unmarried participants may be less likely to be in stable relationships or sexually active and thus more likely to discontinue their contraceptive method as compared to married or cohabitating participants. There were no other significant associations between early discontinuation and most demographic or reproductive characteristics.
Previously published analyses from the CHOICE cohort show high rates of LARC continuation at 12- and 24-months. At 12 months, continuation rates were 88% for the levonorgestrel intrauterine system, 84% for the copper IUD, and 83% for the implant.6 And at 24 months, continuation rates were 79% for the levonorgestrel intrauterine system, 77% for the copper IUD and 69% for the implant.7 The results of this analysis together with the above 12-and 24-month continuation rates, suggest that discontinuation happens steadily over time rather than a large proportion discontinuing early in use. Although there are limited data about continuation of LARC at 6 months, other studies have found similar or slightly lower rates of continuation. A study of 283 copper IUD users found that 11% had discontinued by 6 months, and younger age was not associated with discontinuation.16 A study of 439 IUD and implants users found 89% and 83% respectively, were still using their method at 6 months.17 A retrospective study of 976 implant users found that that 94% were still using the implant at 6 months, and younger age was not associated with continuation.18
Among the IUD discontinuers in our study, cramping was the most common reason for requesting removal by 6 months. While irregular bleeding has been a common reason reported for levonorgestrel intrauterine system removal in other studies, 17,21 only 9% of levonorgestrel intrauterine system discontinuers reported bleeding disturbances as the reason for discontinuation. Our study did, however, identify irregular vaginal bleeding as the main concern among implant discontinuers. All CHOICE participants enrolled at the university clinical research site underwent a standardized contraceptive counseling session focused on evidence-based information.20 Participants were counseled about the possibility of irregular bleeding with the levonorgestrel intrauterine system and the implant. Participants were encouraged to call study staff or make an appointment to address method complaints, and staff encouraged continuation by providing reassurance about the common side effects. Clinicians offered medical management for bleeding irregularities such as nonsteroidal anti-inflammatory drugs or oral contraceptive pills to users with persistent complaints. 22,23 The majority of bleeding irregularities with progestin-only contraception typically occur within the first 6 months of method initiation.22 Therefore, 6-month discontinuers may reflect the population with intolerable bleeding side effects.
Our study had a number of strengths which include a relatively large, racially and socioeconomically diverse cohort of reproductive-aged adolescents and women using LARC methods, including over 800 participants aged 14 to 19 years.. We systematically collected data regarding discontinuation at 3 and 6 months and used multiple data sources to code discontinuation and reasons for discontinuation. There are also several limitations to our study. As this was a secondary analysis, we did not plan to enroll an adequate sample of adolescents to specifically stratify continuation by age. However, a post hoc power calculation shows that we had >90% power to detect a statistically significant difference between the observed discontinuation rate of 7% among older women, and a two-fold increased risk of discontinuation in participants under 20 years of age. There were differences in baseline characteristics between those who completed follow-up surveys and those lost to follow-up. However, our overall loss to follow-up was very low at 3% so this likely has a minimal effect on our findings. In addition, data about method continuation was self-reported and could be subject to misclassification bias. Because CHOICE was restricted to a single geographical area, it is possible that our findings are not generalizable to other populations or the entire U.S. However, our large and diverse cohort increases the likelihood that these findings may be generalizable to other populations of adolescents and women seeking contraception.
LARC methods have a number of potential advantages for adolescent females.12 Many adolescents desire to delay pregnancy for a number of years; therefore, the long-lasting action of IUDs and implant is beneficial. In addition, LARC methods do not require the user to be adherent which may be especially advantageous for adolescents. Lastly, adolescents have higher failure rates with shorter-acting methods such as OCPs, the contraceptive patch, or the vaginal ring. However, LARC methods are equally effective in adolescents and older women.5 Our study findings show that rates of early discontinuation are low among both adolescents and older women. Due to the numerous benefits of LARC, IUDs and the implant should be considered as first-line contraceptive options among all adolescents and women to reduce unintended pregnancy.
Acknowledgments
Supported in part by: 1) The Susan Thompson Buffett Foundation; 2) Award number K23HD070979 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD); and 3) Grant number UL1 TR000448 from the NIH-National Center for Advancing Translational Sciences (NCATS). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NICHD or NIH.
Footnotes
Financial Disclosure: Dr. Peipert receives research funding from Bayer Healthcare Pharmaceuticals and Merck & Co, Inc. and honorarium for serving on an advisory board for TEVA Pharmaceuticals and Watson/Activis. Dr. Madden receives research funding from Merck & Co, Inc and honorarium for serving on an advisory board for Bayer Healthcare Pharmaceuticals. The other authors did not report any potential conflicts of interest.
REFERENCES
- 1.Finer LB, Zolna MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478–485. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singh S, Sedgh G, Hussain R. Unintended pregnancy: worldwide levels, trends, and outcomes. Stud Fam Plann. 2010;41:241–250. doi: 10.1111/j.1728-4465.2010.00250.x. [DOI] [PubMed] [Google Scholar]
- 3.Finer LB, Henshaw SK. Disparities in rates of unintended pregnancy in the United States, 1994 and 2001. Perspect Sex Reprod Health. 2006;38:90–96. doi: 10.1363/psrh.38.090.06. [DOI] [PubMed] [Google Scholar]
- 4.Gipson JD, Koenig MA, Hindin MJ. The effects of unintended pregnancy on infant, child, and parental health: a review of the literature. Stud Fam Plann. 2008;39:18–38. doi: 10.1111/j.1728-4465.2008.00148.x. [DOI] [PubMed] [Google Scholar]
- 5.Winner B, Peipert JF, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med. 2012;366:1998–2007. doi: 10.1056/NEJMoa1110855. [DOI] [PubMed] [Google Scholar]
- 6.Peipert JF, Zhao Q, Allsworth JE, et al. Continuation and satisfaction of reversible contraception. Obstet Gynecol. 2011;117:1105–1113. doi: 10.1097/AOG.0b013e31821188ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Rosenstock JR, Peipert JF, Madden T, Zhao Q, Secura GM. Continuation of reversible contraception in teenagers and young women. Obstet Gynecol. 2012;120:1298–1305. doi: 10.1097/aog.0b013e31827499bd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.O'Neil M, Peipert JF, Zhao Q, Madden T, Secura GM. 24-Month Continuation of Reversible Contraception. Obstet Gynecol. doi: 10.1097/AOG.0b013e3182a91f45. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sonfield A. Popularity Disparity: Attitudes About the IUD in Europe and the United States. Guttmacher Policy Review. 2007;10:19–24. [Google Scholar]
- 10.Finer LB, Jerman J, Kavanaugh ML. Changes in use of long-acting contraceptive methods in the United States, 2007-2009. Fertil Steril. 2012;98:893–897. doi: 10.1016/j.fertnstert.2012.06.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.American Congress of Obstetricians and Gynecologists Committee Opinion No. 450: Increasing use of contraceptive implants and intrauterine devices to reduce unintended pregnancy. Obstet Gynecol. 2009;114:1434–1438. doi: 10.1097/AOG.0b013e3181c6f965. [DOI] [PubMed] [Google Scholar]
- 12.American Congress of Obstetricians and Gynecologists Committee Opinion No. 539: Adolescents and long-acting reversible contraception: implants and intrauterine devices. Obstet Gynecol. 2012 Oct;120(4):983–988. doi: 10.1097/AOG.0b013e3182723b7d. [DOI] [PubMed] [Google Scholar]
- 13.Kavanaugh ML, Frohwirth L, Jerman J, Popkin R, Ethier K. Long-acting reversible contraception for adolescents and young adults: patient and provider perspectives. J Pediatr Adolesc Gynecol. 2013;26:86–95. doi: 10.1016/j.jpag.2012.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moreau C, Cleland K, Trussell J. Contraceptive discontinuation attributed to method dissatisfaction in the United States. Contraception. 2007;76:267–272. doi: 10.1016/j.contraception.2007.06.008. [DOI] [PubMed] [Google Scholar]
- 15.Behringer T, Reeves MF, Rossiter B, Chen BA, Schwarz EB. Duration of use of a levonorgestrel IUS amongst nulliparous and adolescent women. Contraception. 2011;84:e5–e10. doi: 10.1016/j.contraception.2011.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garbers S, Haines-Stephan J, Lipton Y, Meserve A, Spieler L, Chiasson MA. Continuation of copper-containing intrauterine devices at 6 months. Contraception. 2013;87:101–106. doi: 10.1016/j.contraception.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 17.Wong RC, Bell RJ, Thunuguntla K, McNamee K, Vollenhoven B. Implanon users are less likely to be satisfied with their contraception after 6 months than IUD users. Contraception. 2009;80:452–456. doi: 10.1016/j.contraception.2009.03.021. [DOI] [PubMed] [Google Scholar]
- 18.Harvey C, Seib C, Lucke J. Continuation rates and reasons for removal among Implanon users accessing two family planning clinics in Queensland, Australia. Contraception. 2009;80:527–532. doi: 10.1016/j.contraception.2009.05.132. [DOI] [PubMed] [Google Scholar]
- 19.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203:115, e111–117. doi: 10.1016/j.ajog.2010.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Madden T, Mullersman JL, Omvig KJ, Secura GM, Peipert JF. Structured contraceptive counseling provided by the Contraceptive CHOICE Project. Contraception. 2013;88:243–249. doi: 10.1016/j.contraception.2012.07.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jensen JT, Nelson AL, Costales AC. Subject and clinician experience with the levonorgestrel-releasing intrauterine system. Contraception. 2008:7722–29. doi: 10.1016/j.contraception.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 22.Abdel-Aleem H, d'Arcangues C, Vogelsong K, Gulmezoglu AM. Treatment of vaginal bleeding irregularities induced by progestin only contraceptives. Cochrane Database Syst Rev. 2007;(2):CD003449. doi: 10.1002/14651858.CD003449.pub2. [DOI] [PubMed] [Google Scholar]
- 23.Madden T, Proehl S, Allsworth JE, Secura GM, Peipert JF. Naproxen or estradiol for bleeding and spotting with the levonorgestrel intrauterine system: a randomized controlled trial. Am J Obstet Gynecol. 2012;206:129, e121–128. doi: 10.1016/j.ajog.2011.09.021. [DOI] [PMC free article] [PubMed] [Google Scholar]