Abstract
BACKGROUND
The incidence and associated risk factors for readmission after hepato-pancreato-biliary surgery are poorly characterized. The objective of the current study was to compare readmission after pancreatic vs hepatobiliary surgical procedures, as well as to identify potential factors associated with higher readmission within 30 days of discharge.
STUDY DESIGN
Using Surveillance, Epidemiology and End Results–Medicare linked data from 1986–2005, we identified 9,957 individuals aged 66 years and older who underwent complex hepatic, biliary, or pancreatic procedures for cancer treatment and were eligible for analysis. In-hospital morbidity, mortality, and 30-day readmission were examined.
RESULTS
Primary surgical treatment consisted of a pancreatic(46.7%), hepatic (50.0%), or biliary (3.4%) procedure. Mean patient age was 72.6 years and most patients were male (53.2%). The number of patients with multiple preoperative comorbidities increased over time (patients with Elixhauser’s comorbidity score >13: 1986–1990, 47.0% vs 2001–2005, 62.9%; p < 0.001). Pancreatic operations had higher inpatient mortality vs hepatobiliary procedures (9.2% vs 7.3%; p < 0.001). Mean length of stay after pancreatic procedures was longer compared with hepatobiliary procedures (19.7 vs 10.3 days; p < 0.001). The proportion of patients readmitted after a pancreatic (1986–1990, 17.7%; 1991–1995,16.1%; 1996–2000, 18.6%; 2001–2005, 19.6%; p = 0.15) or hepatobiliary (1986–1990, 14.3%; 1991–1995, 14.1%; 1996–2000, 15.2%; 2001–2005, 15.5%; p = 0.69) procedure did not change over time. Factors associated with increased risk of readmission included preoperative Elixhauser comorbidities > 13 (odds ratio = 1.90) and prolonged index hospital stay ≥10 days (odds ratio = 1.54; both p < 0.05). During the readmission, additional morbidity and mortality were 46.5% and 8.0%, respectively.
CONCLUSIONS
Although the incidence of readmission did not change across the time periods examined, readmission was higher among patients undergoing a pancreatic procedure vs a hepatobiliary procedure. Other factors associated with risk of readmission included number of patient comorbidities and prolonged hospital stay. Readmission was associated with additional short-term morbidity and mortality.
Readmission after discharge subsequent to surgery has recently become a topic of much interest. Readmission can be associated with increased hospital-related patient morbidity and mortality, as well as much higher costs to the health care system.1 As such, readmission has been proposed as a quality metric, and readmission rates for surgeons can increasingly become a quality indicator of performance.2 At the same time, providers have increasingly implemented “fasttrack” programs 3,4 and clinical care pathways5,6 to optimize perioperative care and accelerate postoperative recovery and discharge. Amidst these changes, relatively little is known about the incidence and factors predisposing patients to readmission after major abdominal surgical procedures. Although our group and others have reported on the rates of readmission after colorectal surgery7 and abdominal surgery in general,2 little data exist on readmission after complex hepato-pancreato-biliary surgery.
Diseases of the liver, pancreas, and biliary tree frequently require a major surgical procedure. Data on outcomes after these procedures have largely focused on either hospital-related morbidity and mortality or long-term survival. Specifically, several studies have noted that morbidity and mortality associated with surgery for pancreatic, biliary and hepatic diseases has improved during the last several decades.8–12 Little is known, however, about the incidence and impact of readmission among patients undergoing these procedures. Although a few studies have examined readmission after hepato-pancreato-biliary surgery, these studies have suffered from several shortcomings 13–16. In particular, the few studies published previously have reported exclusively on readmission after pancreatic surgery, but failed to examine and compare readmission rates among patients undergoing other complex hepatobiliary procedures. Of note, no previous study has specifically focused on the rate and impact of readmission among patients undergoing hepatobiliary procedures. Previous studies are also problematic because the definition of readmission has varied without being standardized, making data difficult to interpret.
Reduction of avoidable rehospitalizations can result in lower morbidity and mortality for patients undergoing hepato-pancreato-biliary procedures and cost savings for the health care system. Given the importance of readmission and the lack of current data, we sought to define the incidence of readmission after hepato-pancreato-biliary surgery in a large national cohort of patients. Using the Surveillance, Epidemiology and End Results (SEER)–Medicare linked database, we evaluated 30-day readmission rates among patients undergoing complex pancreatic and hepatobiliary surgical procedures for an underlying malignancy. We also compared the incidence of readmission after pancreatic vs hepatobiliary surgical procedures. In addition, factors associated with higher incidence of readmission within 30 days of index discharge were identified.
METHODS
Data source
This was a retrospective cohort study based on analysis of prospectively collected data from the linked SEER–Medicare database from 1986 to 2005. Details of the SEER-Medicare database and linkage techniques have been described previously by our group and others 7,17,18.
Study population
The study cohort was Medicare beneficiaries undergoing curative intent surgery for hepato-pancreato-biliary malignancies. Patients were identified using the ICD-9-CM procedure codes for various surgical procedures used to treat these malignancies (ie, 50.11, 50.12, 50.22, 50.3, 51.37, 51.64, 51.69, 52.22, 52.51–52.53, 52.59, 52.6, 52.7, 52.96). Patients with nonmalignant conditions were excluded from the analysis, as were those undergoing procedures without curative intent. Simple cholecystectomy was also excluded. We restricted the study cohort to patients older than 66 years of age at the time of diagnosis, who had been enrolled in both Medicare part A and B for at least 12 months, and were not enrolled in a managed care plan during the study duration.
Independent and dependent variables
Data on clinicopathological characteristics, including patient age, sex, race, and preoperative comorbidities, were obtained. The Elixhauser comorbidity measures were abstracted; Elixhauser comorbidities are a measurement tool that uses ICD-9-CM codes to define 30 comorbid conditions that have been shown to be a valid prognostic measure of poor outcomes in studies based on large, population-based databases.19 Elixhauser scores were calculated using the method proposed by van Walraven and colleagues.20 When available (ie, 1996–2005), hospital-level data were reported, including number of hospital beds, teaching status, and whether the hospital was located in a rural or urban area. Admission type was classified as emergent, urgent, or elective. Complications were identified from the inpatient database using ICD-9-CM codes. Discharge destination was identified from the inpatient files for the admission in which the procedure was performed or the corresponding readmission, and categorized as home/self care vs skilled/ nursing care facility. We defined a readmitted patient as someone who was discharged from an acute care hospital and was subsequently admitted to an acute care hospital within 30 days of the index discharge.7 Readmission excluded admissions to skilled nursing care or rehabilitation facilities and admissions associated with discharge from the index hospital directly to a short-term general hospital or any other type of long-term care hospital.7,21 Length of stay, incidence of complications, and inpatient mortality for both the index admission and readmission were calculated.
Statistical analysis
Continuous variables were described as means and standard deviations, and discrete variables were described as medians and interquartile range. Categorical variables were described as totals and frequencies. Cells with < 11 patients per variable were relabeled as “< 11 (<0.4%)” in compliance with the National Cancer Institute’s regulations for reporting of SEER-Medicare data. Univariate comparisons were assessed using ANOVA, Kruskal-Wallis test, or chi-square test as appropriate. When analyzing temporal trends, the data were separated into 5-year periods (ie, 1986–1990, 1991–1995, 1996–2000, and 2001–2005) based on year of discharge. Univariate and multivariate logistic regression models were constructed to explore the association of covariates with readmission. Variables with a univariate significance <0.20 were entered into the multivariate model in combination with important clinical variables and confounders. All reported p values were 2-tailed and for all tests p < 0.05 was considered statistically significant. Survival was calculated using the Kaplan-Meier method and medians were compared using the log-rank test. Overall survival time was calculated from the date of the index procedure to the date of death as reported in the SEER database. Those not dead by the date of last follow-up were assigned a censoring date of January 1, 2006. All statistical analyses were performed using SAS 9.3 (SAS Inc.).
RESULTS
Patient and operative details
Between 1986 and 2005, a total of 9,957 patients underwent curative intent procedures for hepato-pancreat-obiliary malignancies and met inclusion criteria. The demographic and clinical characteristics of these patients are presented in Table 1. Mean patient age was 72.6 ± 6.9 years. More patients were men (n = 5,296; 53.2%) and white (n = 8,118; 81.5%). Over time, mean age of patients undergoing hepato-pancreato-biliary malignancies increased slightly (1986–1990, mean age 72.1 years vs 1991–1995, mean age 72.0 years vs 1996–2000, mean age 73.0 years vs 2001–2005, mean age 72.8 years; p < 0.001). Median Elixhauser comorbidity score for the entire cohort was 13. Patients in later time periods were also more likely to have more medical comorbidities. Specifically, 47.0% of patients undergoing a hepato-pancreato-biliary procedure between 1986 and 1990 had a comorbidity score >13 compared with 62.9% patients undergoing surgery between 2001 and 2005 (p < 0.001).
Table 1.
Comparison of Patient Characteristics Stratified by Type of Surgery
| Patient characteristics | Pancreatic surgery (n=4,646) | Hepatobiliary surgery (n = 5,311) | p value |
|---|---|---|---|
| Male sex, n (%) | 2,363 (50.9) | 2,933 (55.2) | <0.001 |
| Age, mean ± SD, y | 72.7 ± 6.3 | 72.3 ± 7.3 | 0.01 |
| No. of Elixhauser comorbidities, median (IQR) | 4 (2–6) | 4 (2–6) | 0.41 |
| Elixhauser score, median (IQR) | 12 (5–19) | 15 (9–22) | 0.16 |
| Race, n (%) | |||
| White | 3,883 (83.6) | 4,235 (79.7) | <0.001 |
| Black | 332 (7.2) | 381 (7.2) | |
| Other | 257 (5.5) | 383 (7.2) | |
| Asian | 80 (2.7) | 176 (3.3) | |
| Hispanic | 42 (0.9) | 67(1.3) | |
| North American native | <11 (<0.4) | <11 (<0.4) | |
| Unknown | 51(1.1) | 65 (1.2) | |
| Admission type, n (%) | |||
| Emergent | 646 (13.9) | 4,532 (10.0) | <0.001 |
| Urgent | 1,071 (23.1) | 933 (17.6) | |
| Elective | 2,911 (62.7) | 3,830(72.1) | |
| Other/unknown | 18 (0.4) | 16 (0.3) | |
| No. of hospital beds, median (IQR) | 388 (236–559)* | 396 (243–565)† | 0.14 |
| Teaching hospitals, n (%) | 1,666(85.0)* | 2,177 (87.3)† | 0.03 |
| Rural hospitals, n (%) | 71 (3.6)* | 53 (2.1)† | 0.06 |
| Discharge year; n (%) | |||
| 1986–1990 | 727(15.7) | 905 (17.0) | <0.001 |
| 1991–1995 | 1,170 (25.2) | 1,182(22.3) | |
| 1996–2000 | 1,545 (33.3) | 1,439 (27.1) | |
| 2001–2005 | 1,204 (25.9) | 1,785 (33.6). | |
Data were missing for 2,686 patients.
Data were missing for 2,816 patients.
IQR, interquartile range.
According to the SEER historic stage, among patients with a pancreatic malignancy, 1,023 had localized disease (23.4%); among the 4,118 patients for whom information was available, 2,448 (59.5%) had lymph node metastasis. Among patients undergoing a hepatobiliary procedure, 2,531 (47.7%) patients had a secondary liver tumor (ie, metastasis) and 2,446 (46.1%) had a primary liver tumor. Among patients with a primary liver tumor, 960 (39.2%) had localized disease. A small subset of patients had a biliary tumor (n = 297; 5.6%).
Surgical resection consisted of a pancreatic (n = 4,646; 46.7%), hepatic (n = 4,977; 50.0%), or biliary (n = 334; 3.4%) procedure. Of the 4,646 patients who underwent pancreatic resection, 3,487 (75.1%) had a pancreaticoduodenectomy, 568 (12.2%) had a distal pancreatectomy, 193 (4.2%) were managed with total pancreatectomy, and 398 (8.6%) had various other pancreatic resections, including partial and near total pancreatectomy. Of the 4,977 patients who underwent a liver procedure, only a subset underwent a hemi-hepatectomy/lobectomy (n = 1,179; 23.7%). Biliary procedures included bile duct resection and hepaticojejunostomy (n = 343). Because of the relatively small numbers of patients in the biliary procedure cohort, hepatic and biliary procedures were combined into one category (ie, hepatobiliary procedures) for subsequent analyses.
After surgery, 4,097 patients experienced a complication, for a postoperative complication incidence of 41.2%. More patients undergoing pancreatic surgery experienced a complication compared with patients undergoing a hepatobiliary procedure (48.3% vs 34.9%, respectively; p < 0.001). Complications more frequently seen after a pancreatic procedure compared with hepatobiliary procedure included postoperative hemorrhage (6.7% vs 3.2%; p < 0.001), postoperative infection (8.4% vs 2.3%; p < 0.001), gastrointestinal complications, not otherwise specified (13.0% vs 6.3%; p < 0.001), and cardiac complications (4.4% vs 3.2%; p < 0.001). Patients undergoing pancreatic surgery were also more likely to receive a peri-operative blood transfusion compared with a hepatobiliary procedure (15.5% vs 11.5%, respectively; p < 0.001). The only complication that was more frequent among patients undergoing a hepatobiliary procedure was the need for operative re-exploration (1.6% vs 5.2%; p < 0.001). Overall postoperative morbidity varied over the time periods examined (1986–1990, 47.9%; 1991–1995, 48.0%; 1996–2000,43.3%; 2001–2005, 35.3%; p < 0.001). There were 813 inpatient hospital deaths, for an overall mortality of 8.2%. Inpatient hospital mortality decreased during the time periods studied (1986–1990, 14.0%; 1991–1995, 9.1%; 1996–2000, 7.3%; 2001–2005, 5.1%; p < 0.001). Pancreatic operations had higher inpatient mortality vs hepatobiliary procedures (9.2% vs 7.3%; p < 0.001). Although inpatient mortality decreased after both pancreas (1986–1990, 14.6%; 1991–1995, 9.6%; 1996–2000, 8.1%; 2001–2005, 7.0%; p < 0.001) and hepatobiliary procedures (1986–1990, 13.6%; 1991–1995, 8.7%; 1996–2000, 6.4%; 2001–2005, 3.8%; p < 0.001), the decrease was more pronounced in the latter group.
Overall mean length of stay after surgery for a hepato-pancreato-biliary procedure was 14.7 days. Length of stay did decrease over time (1986–1990, 19.0 days; 1991–1995, 16.7 days; 1996–2000, 14.0 days; 2001–2005, 11.5 days; p < 0.001; Fig. 1). Of note, mean length of stay after pancreatic procedures was almost twice as long compared with hepatobiliary procedures (19.7 vs 10.3 days; p < 0.001). At discharge from the index admission, 7,937 (79.7%) patients were discharged to home and 1,207 (12.1%) were discharged to skilled nursing or other inpatient facilities. Patients undergoing a hepatobiliary procedure were more likely to be discharged to home (pancreas, 74.8% vs hepatobiliary, 84.0%; p < 0.001).
Figure 1.
Data on index admission length of stay (LOS), mortality, as well as incidence of readmission, readmission LOS, and readmission mortality for pancreas procedures (A) and hepatobiliary procedures (B).
Readmission analyses
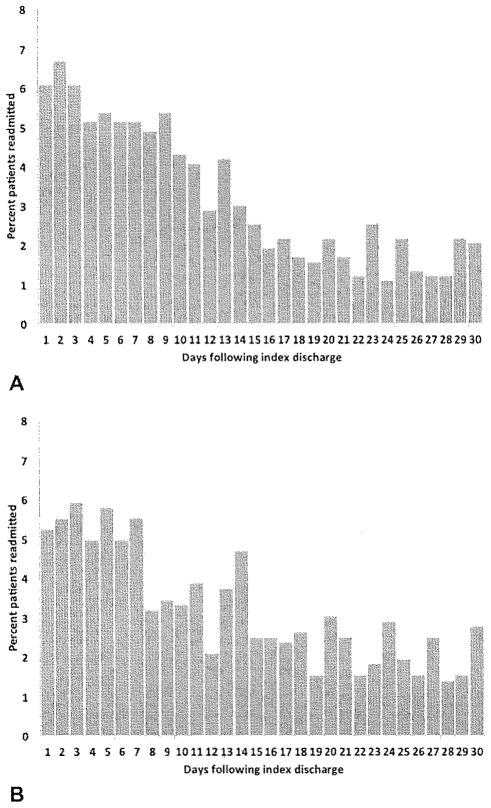
There were a total of 1,631 readmissions within 30 days of index discharge, for an overall readmission rate of 16.4%. The incidence of readmission did not change remarkably across the time periods examined (1986–1990, 15.8%; 1991–1995, 15.1%; 1996–2000, 16.9%; 2001–2005, 17.2%; p = 0.15). Incidence of readmission was higher among patients who underwent a pancreatic procedure compared with a hepatobiliary procedure (18.1% vs 14.9%; p < 0.001). The proportion of patients readmitted after a pancreatic (1986–1990, 17.7%; 1991–1995, 16.1%; 1996–2000, 18.6%; 2001–2005, 19.6%; p = 0.15) or hepatobiliary (1986–1990, 14.3%; 1991–1995, 14.1%; 1996–2000, 15.2%; 2001–2005, 15.5%; p = 0.69) procedure did not change over time. The mean time to readmission for all readmitted patients was 11.3 days (SD 8.5 days), and was no different among patients readmitted after a pancreatic procedure (10.4 days, SD 8.3 days) vs a hepatobiliary procedure (11.9 days, SD 8.7 days; Fig. 2). In examining the timing of readmission, 42.1% of readmissions occurred during the first 7 days after discharge and only 16.3% occurred after 3 weeks (readmission within first 7 days: pancreatic, 43.1% vs hepatobiliary, 41.1%; p = 0.41). The most common readmission diagnoses at readmission were dehydration (n = 397; 24.3%), followed by operative complications (n = 356; 21.8%) and postoperative infection (n = 218; 13.4%).
Figure 2.
Proportion of readmissions within 30 days stratified by number of days after index charge for pancreas procedures (A) and hepatobiliary procedures (B).
Several factors were associated with an increased risk of readmission after hepato-pancreato-biliary surgery (Table 2). As noted, patients who were readmitted were more likely to have undergone a pancreatic procedure (odds ratio [OR] = 1.26; 95% CI, 1.13–1.40; p < 0.001). Among patients undergoing a pancreatic procedure, receipt of pancreaticoduodenectomy (18.1%) was not associated with an increased risk of readmission compared with other types of pancreatic procedures (18.1%; OR = 1.00; 95% CI, 0.84–1.18; p = 0.97). Although patients undergoing a hepatobiliary procedure were less likely to be readmitted, among this cohort, patients who underwent a hepaticojejunostomy (18.7%) were more likely to be readmitted than patients having undergone other hepatobiliary procedures (14.6%; OR = 1.36; 95% CI, 1.02–1.81; p = 0.04). Among all patients, other factors associated with readmission included male sex (OR =1.15; 95% CI, 1.03–1.28; p = 0.01), more medical comorbidities at admission (OR = 1.90; 95% CI, 1.61–2.23; p < 0.001), a history of a perioperative surgical complication during the index admission (OR =1.11; 95% CI, 1.01–1.24; p = 0.04), and an index hospital stay length of stay ≥10 days (OR= 1.54; 95% CI, 1.38–1.88; p < 0.001). Mean duration of initial hospital stay was 16.1 ± 12.5 days among patients who were readmitted vs 14.4 ± 13.6 days for the no-readmission group of patients (p < 0.001). On multivariate analysis, factors that remained independently associated with increased risk of readmission included male sex (OR = 1.18; 95% CI, 1.06–1.32; p = 0.01), Elixhauser’s comorbidity score > 13 (OR = 1.99; 95% CI, 1.77–2.24; p < 0.001), and index length of stay ≥10 days (OR = 1.54; 95% CI, 1.35–1.76; p < 0.001; Table 3).
Table 2.
Comparison of Patient Characteristics Stratified by Whether Patients Were Readmitted within 30 Days of Index Discharge
| Variable | Readmitted within 30 d (n=1,631) | Not readmitted within 30 d (n = 8,051) | Not readmitted but died ≤30 d (n= 275) | p Value |
|---|---|---|---|---|
| Male sex, n (%) | 914 (56.0) | 4,251 (52.8) | 131 (47.6) | 0.01 |
| Age, mean ± SD, y | 72.4 ± 7.2 | 72.5 ± 6.8 | 74.9 ± 7.8 | <0.001 |
| No. of Elixhauser comorbidities, median (IQR) | 5 (3–7) | 4 (2–6) | 3(2–4) | <0.001 |
| Elixhauser score, median (IQR) | 16 (9–23) | 13 (5–20) | 12(9–18) | <0.001 |
| Race, n (%) | ||||
| White | 1,297 (79.5) | 6,592(81.9) | 229 (83.3) | 0.18 |
| Black | 135 (8.3) | 556 (6.9) | 22 (8.0) | |
| Other | 119(7.3) | 508 (6.3) | 13 (4.7) | |
| Asian | 37 (2.3) | 217 (2.7) | <11 (<0.4) | |
| Hispanic | 23 (1.4) | 82(1.0) | <11 (<0.4) | |
| North American native | <11 (<0.4) | <11 (<0.4) | 0 | |
| Unknown | 19 (1.2) | 92(1.1) | 5(1.8) | |
| Admission type, n (%) | ||||
| Emergent | 217(13.3) | 890(11.1) | 71 (25.8) | <0.001 |
| Urgent | 365 (22.4) | 1,536(19.1) | 103 (37.5) | |
| Elective | 1,046(64.1) | 5,595 (69.5) | 100 (36.4) | |
| Other/unknown | <11 (<0.4) | 30 (0.4) | <11 (0.4) | |
| No. of hospital beds, median (IQR) | 400 (242–565)* | 396 (242–565)† | 256 (165–381)‡ | <0.001 |
| Teaching hospitals, n (%) | 651 (84.2)* | 3,122(86.8)† | 70(81.4)‡ | 0.08 |
| Rural hospitals, n (%) | 21 (2.7)* | 94 (2.6)† | <11 (<0.4%)‡ | 0.002 |
| Hepatic procedure, n (%) | 728 (44.6) | 4,061 (50.4) | 188 (68.4) | <0.001 |
| Pancreatic procedure, n (%) | 840(51.5) | 3,733 (46.4) | 73 (25.7) | <0.001 |
| Discharge year, n (%) | ||||
| 1986–1990 | 258(15.8) | 1,317(16.4) | 57 (20.7) | 0.01 |
| 1991–1995 | 355 (21.8) | 1,921 (23.9) | 76 (27.6) | |
| 1996–2000 | 505 (31.0) | 2,394 (29.7) | 85 (30.9) | |
| 2001–2005 | 513 (31.5) | 2,419 (30.1) | 57 (20.7) | |
Data were missing for 858 patients.
Data were missing for 4,455 patients.
Data were missing for 189 patients.
IQR, interquartile range.
Table 3.
Logistic Regression Analysis of Variables Associated with Readmission within 30 Days of Discharge from Index Admission
| Prognostic factor | Univariate
|
Multivariate
|
||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% CI | p value | odds ratio | 95% ci | p value | |
| Male sex | 1.15 | 1.03–1.28 | 0.01 | 1.18 | 1.06–1.32 | 0.01 |
|
| ||||||
| Age 75 y or older | 0.99 | 0.90–1.11 | 0.90 | |||
|
| ||||||
| Regional or distant disease | 1.02 | 0.91–1.14 | 0.78 | |||
|
| ||||||
| Discharge year
| ||||||
| 1986–1990 | Referent | Referent | ||||
|
| ||||||
| 1991–1995 | 0.95 | 0.80–1.13 | 0.08 | 0.83 | 0.69–1.00 | 0.03 |
|
| ||||||
| 1996–2000 | 1.09 | 0.92–1.28 | 0.26 | 0.92 | 0.77–1.10 | 0.84 |
|
| ||||||
| 2001–2005 | 1.10 | 0.94–1.30 | 0.13 | 0.97 | 0.81–1.16 | 0.36 |
|
| ||||||
| Index length of stay ≥10 d | 1.54 | 1.38–1.88 | <0.001 | 1.54 | 1.35–1.76 | <0.001 |
|
| ||||||
| Elixhauser’s comorbidity score >13 | 1.90 | 1.61–2.23 | <0.001 | 1.99 | 1.77–2.24 | <0.001 |
|
| ||||||
| Any postsurgical complication | 1.11 | 1.01–1.24 | 0.04 | 0.99 | 0.88–1.10 | 0.81 |
|
| ||||||
| Transfusion during index admission | 1.04 | 0.89–1.22 | 0.59 | |||
|
| ||||||
| Pancreatic procedure | 1.26 | 1.13–1.40 | <0.001 | 1.05 | 0.93–1.18 | 0.42 |
Among patients readmitted, mean length of stay for readmission was 8.57 ±8.4 days (pancreas, 9.0 days vs hepatobiliary, 8.1 days). The incidence of additional complications during the second admission was 46.5% (n = 759). Among patients readmitted, 130 died during the readmission, for an additional mortality of 8.0%. In-hospital mortality during second admission decreased during the study duration (1986–1990, 14.3%; 1991–1995, 9.0%; 1996–2000, 6.3%; 2001–2005, 5.9%; p < 0.001). In-hospital mortality during readmission was higher among patients who underwent a hepatobiliary procedure during the index admission, as compared with those patients who underwent a pancreatic procedure (10.5% vs 5.6%; p < 0.001).
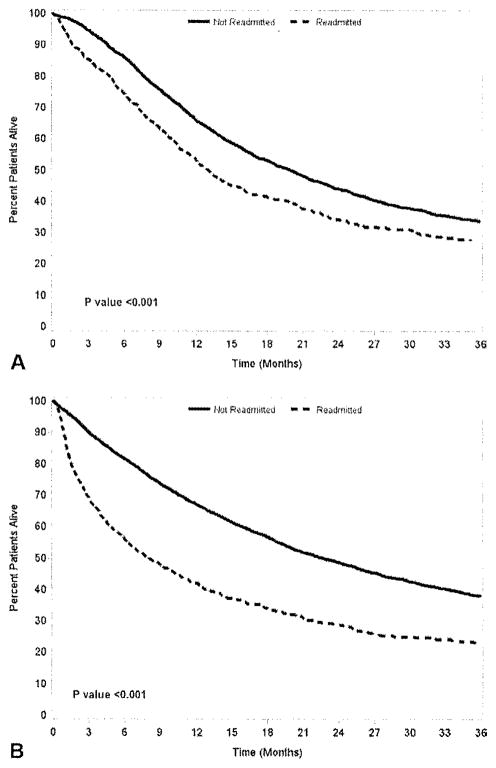
Median survival for the whole cohort was 19.5 months (95% CI, 18.6–20.2 months) and overall 5-year survival was 32.6%. Patients who were readmitted had a worse survival compared with patients who were not readmitted (median 10.9 vs 21.3 months, respectively; 5 year: 24.8% vs 35.0%, respectively; both, p < 0.001; Fig. 3). Among all patients who underwent pancreatic surgery, median survival for readmitted vs non-readmitted patients was 13.1 months (95% CI, 11.9–14.6 months) and 20.0 months (95% CI, 18.7–21.1 months; p < 0.001), respectively. For patients who underwent hepatobiliary surgery, median survival for readmitted vs non-readmitted patients was 8.1 months (95% CI, 6.6–9.8 months) and 22.8 months (95% CI, 21.4–24.3 months; p < 0.001), respectively.
Figure 3.
Long-term overall survival stratified by readmission status and type of surgical procedure: pancreas (A) and hepatobiliary (B).
DISCUSSION
Data on readmission after hepato-pancreato-biliary procedures remain poorly defined. Although a few studies have examined readmission after pancreatic surgery,13,14,22 data on readmission after hepatic surgery has not been examined. In addition, although our group has previously reported on the differences in mortality after various hepato-pancreato-biliary procedures,23 the relative impact of procedure type on readmission has not been explored. Decreasing readmission has been identified as an important focus of the Center for Medicare and Medicaid Services0 and future hospital reimbursement can be tied to standardized readmission rates.7 Perhaps more importantly, readmission can be associated with increased mortality and, therefore, lowering readmission has been proposed as an important quality metric.24 Hepato-pancreato-biliary surgery has traditionally been associated with some of the highest risk of morbidity and mortality. Defining the incidence of readmission after these high-risk procedures, as well as gaining a better understanding of possible factors associated with readmission after hepato-pancreato-biliary surgery, is critical to improving outcomes in this group of patients. The current study is important because it demonstrated that the overall incidence of readmission after hepato-pancreato-biliary procedures was 16.4%. We noted that patients who were readmitted were more likely to have undergone a pancreatic procedure (OR = 1.26; 95% CI, 1.13–1.40; p < 0.001). Although a shorter length of stay was not associated with risk of readmission, patient comorbidities were. Importantly, we also noted that readmission was associated with an additional mortality of 8.0%.
Previous data on readmission after hepatobiliary procedures have been difficult to interpret. Definitions of readmission have lacked standardization and have included patients readmitted at 30 days, 1 year, or at any time point.13,14,16 In turn, readmission after pancreatic surgery has been reported to range from 16% to >50%— undoubtedly due in part to the varied definitions of readmission. In the current study, we used a 30-day definition of readmission. In addition, our definition of readmission specifically excluded subsequent admission to a skilled nursing facility or other nonacute inpatient facility. Using these criteria, we noted a readmission incidence of 18% after pancreatic surgery, which was consistent with previous data reported by Reddy and colleagues.13 Unlike other studies, we also examined readmission after hepatobiliary surgery, as well as trends over time. The proportion of patients readmitted after pancreatic surgery did decrease over time; however, at no time was it lower than readmission after hepatobiliary surgery (14.9%). Readmission most commonly occurred relatively soon after the index discharge, with 42.1% of readmissions occurring during the first 7 days. These data are consistent with previously published data from our group that noted 43.7% of readmissions after colorectal surgery occurred within the first week of discharge.7 Collectively, these data should help inform the surgeon about the risk of readmission relative to date of discharge, as well as assist in the patient counseling at the time of discharge.
A shorter length of stay was not associated with higher risk of readmission. In fact, we noted that a prolonged index hospital length of stay of 10 or more days was associated with a >50% increased risk of readmission. The impact of prolonged length of stay was the same among patients undergoing either pancreatic or hepatobiliary procedure. Although the exact cause of a prolonged hospitalization could not be fully explicated using the current data, protracted hospital stays were most likely due to some deviation in the clinical care plan. Perhaps it is not surprising, therefore, that such patients were more likely to experience a readmission. Prolonged hospital stays are often more common among patients with increased medical acuity (eg, more medical comorbidities) and among those who suffer a perioperative complication. In the current study, more medical comorbidities at admission and a prolonged hospital stay were both associated with risk of readmission. Despite a general perception that shorter lengths of stay might be contributing to increased rates of readmission, our data do not support this theory. Similar to our previous work examining length of stay among colon cancer patients7, data here presented on hepato-pancreato-biliary patients strongly suggest an increasing number of medical comorbidities and those with a long index hospital admission are at the greatest risk of readmission, especially after pancreatic surgery.
Readmission had a number of implications. Specifically, readmission accounted for a considerable increase in the total hospital stay, with a mean additional 8 to 9 days in the hospital. Once readmitted, patients also had a high incidence of additional complications, as well as mortality. In fact, the mortality during the readmission hospital stay (8.0%) was comparable with the mortality associated with the index admission—in essence, doubling the risk of death. Interestingly, although patients undergoing a hepatobiliary procedure were less likely to be readmitted compared with pancreatic surgery patients, readmission after a hepatobiliary procedure had a higher in-hospital mortality (hepatobiliary: 10.5% vs pancreas: 5.6%; p < 0.001). Readmission also impacted long-term survival. Our group had previously noted that 30-day readmission adversely impacted long-term survival after colorectal surgery 7. In a separate study, Reddy and colleagues noted that median survival was worse among patients readmitted after pancreatic surgery.13 We similarly found that among all patients who underwent pancreatic surgery, median survival for readmitted vs non-readmitted patients was worse. In addition, we noted the same effect for patients who underwent hepatobiliary surgery.
The current data expand on previous findings and lend additional support to the notion that short-term outcomes, such as unplanned readmission, can lead to worse long-term consequences.
The current study had several limitations. As with all SEER-Medicare analyses, only Medicare beneficiaries were included and therefore the general application of these data to younger patient populations might not be appropriate. However, given that many patients with pancreatic and hepatobiliary cancers are 65 years or older, the current study provides important data on a large subset of patients with these underlying malignancies. Similar to our previous report, the current study is also subject to coding inaccuracies and limitations associated with the use of any large administrative dataset.7 The current study also might not necessarily be reflective of outcomes from high-volume tertiary centers. The purpose of the current study, however, was to examine data on outcomes for older adult Medicare patients undergoing hepato-pancreato-biliary procedures.
CONCLUSIONS
Based on a population based large national dataset, the incidence of readmission after hepato-pancreato-biliary surgery was noted to be 16.4%. Although the incidence of readmission did not change remarkably across the time periods examined, we did note that risk of readmission among patients undergoing a pancreatic procedure was higher compared with a hepatobiliary procedure. Other factors associated with risk of readmission include number of patient comorbidities and prolonged hospital stay. Readmission was associated with substantial additional short-term morbidity and mortality, as well as worse long-term survival. Future studies will need to build on the current work to design possible intervention strategies to prevent unplanned readmissions and improve outcomes for patients undergoing hepato-pancreato-biliary surgery.
Footnotes
Disclosure Information; Authors have nothing to disclose. Timothy J Eberlein, Editor-in-Chief, has nothing to disclose.
Author Contributions
Study conception and design: Schneider, Hyder, Pawlik Acquisition of data: Schneider, Hyder, Pawlik
Analysis and interpretation of data: Schneider, Hyder, Wolfgang, Hirose, Choti, Makary, Herman, Cameron, Pawlik
Drafting of manuscript: Schneider, Hyder, Pawlik
Critical revision: Schneider, Hyder, Wolfgang, Hirose, Choti, Makary, Herman, Cameron, Pawlik
Final approval: Schneider, Hyder, Wolfgang, Hirose, Choti, Makary, Herman, Cameron, Pawlik
References
- 1.Jencks SF. Defragmenting care. Ann Intern Med. 2010;153:757–758. doi: 10.7326/0003-4819-153-11-201012070-00010. [DOI] [PubMed] [Google Scholar]
- 2.Martin RC, Brown R, Puffer L, et al. Readmission rates after abdominal surgery: the role of surgeon, primary caregiver, home health, and subacute rehab. Ann Surg. 2011;254:591–597. doi: 10.1097/sla.0b013e3182300a38. [DOI] [PubMed] [Google Scholar]
- 3.Spelt L, Ansari D, Sturesson C, et al. Fast-track programmes for hepatopancreatic resections: where do we stand? HPB (Oxford) 2011;13:833–838. doi: 10.1111/j.1477-2574.2011.00391.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Bree SH, Vlug MS, Bemelman WA, et al. Faster recovery of gastrointestinal transit after laparoscopy and fast-track care in patients undergoing colonic surgery. Gastroenterology. 2011;141:872–880. e1–e4. doi: 10.1053/j.gastro.2011.05.034. [DOI] [PubMed] [Google Scholar]
- 5.Kennedy EP, Rosato EL, Sauter PK, et al. Initiation of a critical pathway for pancreaticoduodenectomy at an academic institution—the first step in multidisciplinary team building. J Am Coll Surg. 2007;204:917–923. doi: 10.1016/j.jamcollsurg.2007.01.057. discussion 923–924. [DOI] [PubMed] [Google Scholar]
- 6.Porter GA, Pisters PW, Mansyur C, et al. Cost and utilization impact of a clinical pathway for patients undergoing pancreaticoduodenectomy. Ann Surg Oncol. 2000;7:484–489. doi: 10.1007/s10434-000-0484-0. [DOI] [PubMed] [Google Scholar]
- 7.Schneider EB, Hyder O, Brooke BS, et al. Patient readmission and mortality after colorectal surgery for colon cancer: impact of length of stay relative to other clinical factors. J Am Coll Surg. 2012;214:390–398. doi: 10.1016/j.jamcollsurg.2011.12.025. [DOI] [PubMed] [Google Scholar]
- 8.Mayo SC, Shore AD, Nathan H, et al. National trends in the management and survival of surgically managed gallbladder adenocarcinoma over 15 years: a population-based analysis. J Gastrointest Surg. 2010;14:1578–1591. doi: 10.1007/s11605-010-1335-3. [DOI] [PubMed] [Google Scholar]
- 9.Mayo SC, Shore AD, Nathan H, et al. Refining the definition of perioperative mortality following hepatectomy using death within 90 days as the standard criterion. HPB (Oxford) 2011;13:473–482. doi: 10.1111/j.1477-2574.2011.00326.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nathan H, Segev DL, Mayo SC, et al. National trends in surgical procedures for hepatocellular carcinoma: 1998–2008. Cancer. 2012;118:1838–1844. doi: 10.1002/cncr.26501. [DOI] [PubMed] [Google Scholar]
- 11.Mayo SC, Gilson MM, Herman JM, et al. Management of patients with pancreatic adenocarcinoma: national trends in patient selection, operative management, and use of adjuvant therapy. J Am Coll Surg. 2012;214:33–45. doi: 10.1016/j.jamcollsurg.2011.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mayo SC, Heckman JE, Shore AD, et al. Shifting trends in liver-directed management of patients with colorectal liver metastasis: a population-based analysis. Surgery. 2011;150:204–216. doi: 10.1016/j.surg.2011.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reddy DM, Townsend CM, Jr, Kuo YE, et al. Readmission after pancreatectomy for pancreatic cancer in Medicare patients. J Gastrointest Surg. 2009;13:1963–1974. doi: 10.1007/s11605-009-1006-4. discussion 1974–1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emick DM, Riall TS, Cameron JL, et al. Hospital readmission after pancreaticoduodenectomy. J Gastrointest Surg. 2006;10:1243–1252. doi: 10.1016/j.gassur.2006.08.016. discussion 1252–1253. [DOI] [PubMed] [Google Scholar]
- 15.van Geenen RC, van Gulik TM, Busch OR, et al. Readmissions after pancreatoduodenectomy. Br J Surg. 2001;88:1467–1471. doi: 10.1046/j.0007-1323.2001.01900.x. [DOI] [PubMed] [Google Scholar]
- 16.Yermilov I, Bentrem D, Sekeris E, et al. Readmissions following pancreaticoduodenectomy for pancreas cancer: a population-based appraisal. Ann Surg Oncol. 2009;16:554–561. doi: 10.1245/s10434-008-0178-6. [DOI] [PubMed] [Google Scholar]
- 17.Mayo SC, Gilson MM, Herman JM, et al. Management of patients with pancreatic adenocarcinoma: national trends in patient selection, operative management, and use of adjuvant therapy. J Am Coll Surg. 2012;214:33–45. doi: 10.1016/j.jamcollsurg.2011.09.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Warren JL, Klabunde CN, Schrag D, et al. Overview of the SEER-Medicare data: content, research applications, and generalizability to the United States elderly population. Med Care. 2002;40(Suppl):IV3–18. doi: 10.1097/01.MLR.0000020942.47004.03. [DOI] [PubMed] [Google Scholar]
- 19.Elixhauser A, Steiner C, Harris DR. Comorbidity measures for use with administrative data. Med Care. 1998;36:8–27. doi: 10.1097/00005650-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 20.van Walraven C, Austin PC, Jennings A, et al. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47:626–633. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 21.Lidor AO, Schneider E, Segal J, et al. Elective surgery for diverticulitis is associated with high risk of intestinal diversion and hospital readmission in older adults. J Gastrointest Surg. 2010;14:1867–1874. doi: 10.1007/s11605-010-1344-2. [DOI] [PubMed] [Google Scholar]
- 22.Kent TS, Sachs TE, Callery MP, Vollmer CM., Jr Readmission after major pancreatic resection: a necessary evil? J Am Coll Surg. 2011;213:515–523. doi: 10.1016/j.jamcollsurg.2011.07.009. [DOI] [PubMed] [Google Scholar]
- 23.Nathan H, Cameron JL, Choti MA, et al. The volume outcomes effect in hepato-pancreato-biliary surgery: hospital versus surgeon contributions and specificity of the relationship. J Am Coll Surg. 2009;208:528–538. doi: 10.1016/j.jamcollsurg.2009.01.007. [DOI] [PubMed] [Google Scholar]
- 24.Ansari MZ, Collopy BT, Booth JL. Hospital characteristics associated with unplanned readmissions. Aust Health Rev. 1995;18:63–75. [PubMed] [Google Scholar]