Abstract
Background
Bioabsorbable polymer stents with drug elution only on the abluminal surface may be safer than durable polymer drug-eluting stents.
Objective
To report the experimental findings with the InspironTM stent - a bioabsorbable polymer-coated stent with sirolimus release from the abluminal surface only, recently approved for clinical use.
Methods
45 stents were implanted in the coronary arteries of 15 pigs. On day 28 after implantation, angiographic, intracoronary ultrasonographic and histomorphological data were collected. Five groups were analyzed: Group I (nine bare-metal stents); Group II (nine coated with bioabsorbable polymer on the luminal and abluminal surfaces); Group III (eight stents coated with bioabsorbable polymer on the abluminal surface); Group IV (nine stents with bioabsorbable polymer and sirolimus on the luminal and abluminal surfaces); and Group V (ten stents with bioabsorbable polymer and sirolimus only on the abluminal surface).
Results
The following results were observed for Groups I, II, III, IV and V, respectively: percentage stenosis of 29 ± 20; 36 ± 14; 33 ± 19; 22 ± 13 and 26 ± 15 (p = 0.443); late lumen loss (in mm) of 1.02 ± 0.60; 1.24 ± 0.48; 1.11 ± 0.54; 0.72 ± 0.44 and 0.78 ± 0.39 (p = 0.253); neointimal area (in mm2) of 2.60 ± 1.99; 2.74 ± 1.51; 2.74 ± 1.30; 1.30 ± 1.14 and 0.97 ± 0.84 (p = 0.001; Groups IV and V versus Groups I, II and III); and percentage neointimal area of 35 ± 25; 38 ± 18; 39 ± 19; 19 ± 18 and 15 ± 12 (p = 0.001; Groups IV and V versus Groups I, II and III). Injury and inflammation scores were low and with no differences between the groups.
Conclusion
The InspironTM stent proved to be safe and was able to significantly inhibit the neointimal hyperplasia observed on day 28 after implantation in porcine coronary arteries.
Keywords: Drug-Eluting Stents, Sirolimus, Epidemiology, Experimental
Introduction
In the years of 2002 and 2003, the CypherTM (Cordis Corp, Miami Lakes, USA) and TaxusTM (Boston Scientific, Natick, USA) drug-eluting coronary stents were approved for clinical use and provided a major breakthrough in the percutaneous treatment of coronary stenoses, thanks to a significant reduction of the incidence of in-stent restenosis and of the need for a new target-vessel revascularization1,2. However, the occurrence of cases of late and very late thrombosis3,4 after implantation was an alert for the safety of these drug-eluting stents.
Among the multiple pathophysiological processes pointed as predisposing factors for late and very late thrombosis are: delayed strut endothelialization; positive remodeling with acquired poor apposition; endothelial dysfunction; and inflammatory reaction due to the presence of a durable polymer5.
With the purpose of overcoming the limitations and adverse events related to first-generation stents, several new drug-eluting stents have been developed. These new stents show variations either in the composition of the alloy, in the strut thickness, in the mesh design, in the drug-carrying polymer, in the drug class and dosage, or in the place on the stent surface from which the drug is released.
We hypothesized that, after drug release and degradation of the biodegradable polymer, only the metallic platform would remain in the arterial wall (like in a bare-metal stent), thus reducing the late and very late thrombosis rates of these stents, without compromising the anti-restenotic efficacy. Drug release from the abluminal surface only (stent surface in contact with the vessel wall) could also prevent delayed endothelialization of the stent struts, which is another mechanism pointed as responsible for thrombosis.
This study presents preclinical data on the InspironTM stent (Scitech ® Medical Products Inc., Goiânia, Goiás, Brazil) - a stent composed of a chromium-cobalt L605 alloy, which is coated with a sirolimus and biodegradable polymer mixture only on its abluminal surface, and was recently approved for clinical use.
In this experimental study, the results observed in porcine coronary arteries by means of angiographic, intracoronary ultrasonographic, and histomorphological assessment on day 28 after implantation of the InspironTM stent versus stents with polymer and sirolimus on the luminal and abluminal surfaces, and bare-metal stents were compared.
Methods
Ethical Aspects
The study protocol was approved by the Institutional Research Ethics Committee and was carried out according to the Good Laboratory Practices guidelines.
Animal species
A total of 15 non-atherosclerotic juvenile pigs from a commercial farm were used. Their mean weight was 28.9 kg (26 to 31.5 kg), and they received oral acetylsalicylic acid (200 mg) and clopidogrel (300 mg) one day prior to stent implantation.
Stents
Forty five pre-assembled stents manufactured by ScitechTM Medical Products, Inc., with 2.5, 3.0 and 3.5-mm diameters and 19-mm length were used. These stents are made of a chromium-cobalt L605 alloy, and have a thin strut (75-µm thickness), forming rings with short cells (1.1 mm) linked to each other by 65-µm struts6.
Except for 9 stents with no polymer or drug coating, the other stents were coated with biodegradable polymer, a mixture of poly (lactic acid) and poly (lactic acid-co-glycolic acid); this layer was 5-µm thick, and water- and CO2 degradable within 6 to 9 months (Figure 1).
Figure 1.
Detail of the metal mesh (left), strut thickness (top right), and polymer (bottom right) of the chromium-cobalt L605 coronary stent (Scitech© Medical Products Inc., Goiânia, Goiás, Brazil).
The drug used in the drug-eluting stents was sirolimus, with 60% release in the first week and 90% within up to 4 weeks. The sirolimus dose used was 8.8 µg per mm of stent in the sirolimus-releasing stent from the luminal and abluminal stent surfaces; or 4.4 µg per mm of stent, on the sirolimus-releasing stent only from the abluminal surface (InspironTM stent).
Thus, five types of stents were assessed: nine stents without polymer or antiproliferative drug coating (Group I, bare-metal stent); nine bioabsorbable polymer-coated stents on the luminal and abluminal surfaces (Group II); eight bioabsorbable polymer-coated stents on the abluminal surface (Group III); nine bioabsorbable polymer and sirolimus coated stents on the luminal and abluminal surfaces (Group IV) and ten bioabsorbable polymer- and sirolimus-coated stents only on the abluminal surface (Group V, InspironTM stent).
Stent implantation procedure
Intramuscular preanesthetic medications were administered (ketamine 3 mg/kg and midazolam 0.5 mg/kg). Then, after intravenous infusion of thiopental, the animals underwent endotracheal intubation, mechanical ventilation, maintenance of the anesthetic plan with isoflurane and monitoring of their heart rhythms, heart rates, and oxygen saturation.
An arterial line for the stent implantation procedure was obtained by dissecting the common femoral artery, with arterial puncture under direct visualization and insertion of a 6-French valved introducer. Under fluoroscopy (Philips BV - The Netherlands), a 6-French Judkins Right therapeutic catheter was manipulated for selective catheterization of the coronary arteries; next, intracoronary nitroglycerin (200 µg) was administered and coronary angiography was performed in the left anterior oblique view at 45 degrees.
Then, a 0.014-inch Choice PRTM guidewire (Boston Scientific, Natick, USA) was inserted with its distal tip positioned in the target-coronary artery. Following a previous raffle, one stent per artery was implanted, preferably in an arterial segment with few lateral branches and without significant lumen reduction and deployment pressure enough to reach a stent deployment balloon diameter: artery rate of 1.1:1 (Table 1).
Table 1.
Individual data on the stent implantation procedure
| Animal number | Weight (kg) | Target coronary-artery | Group | Stent size (mm) (diameter x length) | Implantation pressure (ATM) |
|---|---|---|---|---|---|
| 1 | 31 | CD | I | 3.0 x 19 | 8 |
| CX | III | 3.0 x 19 | 6 | ||
| DA | IV | 3.0 x 19 | 7 | ||
| 2 | 30 | CD | I | 3.0 x 19 | 10 |
| CX | III | 3.5 x 19 | 8 | ||
| DA | II | 3.0 x 19 | 10 | ||
| 3 | 30 | CD | II | 3.0 x 19 | 6 |
| CX | IV | 3.5 x 19 | 10 | ||
| DA | III | 3.0 x 19 | 5 | ||
| 4 | 31.5 | CD | IV | 3.0 x 19 | 8 |
| CX | I | 3.0 x 19 | 6 | ||
| DA | II | 3.0 x 19 | 9 | ||
| 5 | 28.5 | CD | IV | 3.0 x 19 | 10 |
| CX | II | 3.0 x 19 | 6 | ||
| DA | III | 3.0 x 19 | 7 | ||
| 6 | 30 | CD | III | 3.0 x 19 | 10 |
| CX | V | 3.0 x 19 | 10 | ||
| DA | I | 3.5 x 19 | 10 | ||
| 7 | 30 | CD | V | 3.0 x 19 | 10 |
| CX | I | 3.0 x 19 | 12 | ||
| DA | III | 3.0 x 19 | 11 | ||
| 8 | 26 | CD | III | 3.0 x 19 | 10 |
| CX | V | 2.5 x 19 | 8 | ||
| DA | I | 2.5 x 19 | 9 | ||
| 9 | 31 | CD | V | 2.5 x 19 | 6 |
| CX | II | 3.0 x 19 | 7 | ||
| DA | IV | 2.5 x 19 | 10 | ||
| 10 | 27.5 | CD | II | 3.0 x 19 | 8 |
| CX | I | 3.5 x 19 | 8 | ||
| DA | V | 2.5 x 19 | 7 | ||
| 11 | 26.5 | CD | IV | 3.0 x 19 | 12 |
| CX | IV | 3.5 x 19 | 10 | ||
| DA | V | 3.0 x 19 | 10 | ||
| 12 | 27.5 | CD | III | 3.5 x 19 | 7 |
| CX | V | 3.0 x 19 | 5 | ||
| DA | II | 3.5 x 19 | 10 | ||
| 13 | 27 | CD | II | 3.5 x 19 | 8 |
| CX | IV | 3.0 x 19 | 7 | ||
| DA | V | 3.0 x 19 | 11 | ||
| 14 | 26.5 | CD | V | 3.0 x 19 | 11 |
| CX | III | 3.5 x 19 | 5 | ||
| DA | I | 3.0 x 19 | 7 | ||
| 15 | 31.5 | CD | I | 3.0 x 19 | 10 |
| CX | IV | 3.5 x 19 | 10 | ||
| DA | V | 3.5 x 19 | 10 |
RC: right coronary artery; CX: circumflex artery; AD: anterior descending artery; Group I: bare-metal stents; Group II: stents with bioabsorbable polymer on the luminal and abluminal surfaces; Group III: stents with bioabsorbable polymer on the abluminal surface; Group IV: stents with bioabsorbable polymer and sirolimus on the luminal and abluminal surfaces; Group V: stents with bioabsorbable polymer and sirolimus only on the abluminal surface.
Post-Procedure follow-up
After the procedure, the animals were observed regarding their anesthetic recovery and were given prophylactic intramuscular antibiotic therapy with benzyl penicillin 1,200,000 units and gentamicin 40 mg. They were extubated when well awake, and sent to individual pens. They later received commercial feed for growing pigs (CooperTM, São José dos Campos, São Paulo, Brazil) and water ad libitum. For 28 days, oral antiplatelet agents were administered (acetylsalicylic acid 100 mg a day and clopidogrel 75 mg a day); the animals were seen daily by veterinarians, who observed them and made notes on their general status, level of physical activity, feed intake, and presence of fever; they also diagnosed and treated occasional surgical wound infections.
On day 28 after stent implantation, the animals were sent back to the animal experimentation laboratory and underwent control coronary angiography with quantitative coronary angiography and intracoronary ultrasonography. They were euthanized by deepening the level of anesthesia and administration of a lethal intravenous injection of potassium chloride (30 to 40 mL).
Histological processing
After euthanasia and left paramedian thoracotomy, the heart of each animal was carefully removed, with minimal handling, to prevent external stent compression; the blood in the cardiac chambers was washed out with drinking water and 0.9% saline solution. A 10% formaldehyde solution was then infused in the aortic root at a 100-mmHg pressure for 30 minutes. The arterial segments containing the stents were dissected from the adjacent tissues, removed, and placed in a 10% formaldehyde solution for 24 hours, and later, in 70% absolute alcohol. These arterial segments containing the stents were desiccated in alcohol solutions, embedded in methacrylate plastic resins, and subsequently subjected to cross sections (mean thickness of 3.5 µm), with a tungsten knife in a proper microtome (RM 2265, Leica, Germany).
Quantitative Coronary Angiography
All angiographies of the stent implants and the control studies performed at day 28 were analyzed by means of off-line quantitative coronary angiography using the CASS II software (Pie Medical, Maastrich, The Nederlands). The minimum lumen diameter (MLD, in mm), reference diameters (RD, in mm), percentage angiographic stenosis (%), and late lumen losses (in mm) were determined.
Intracoronary ultrasonography
40-MHZ AtlantisTM SR Pro (Boston Scientific, Natick, MA, USA) intracoronary sonography catheters were used, with automatic pull back at 0.5 mm/s. The images acquired were analyzed by the built-in measurement software of the intracoronary ultrasound imaging system (Ilab®, Boston Scientific, Natick, MA, USA); using planimetry, the lumen areas (in mm2), stent areas (in mm2), neointimal hyperplasia areas (in mm2), and percentage neointimal hyperplasia areas (%) were determined.
Histomorphology
Three histological slides were obtained per third of stent segment (proximal, mid-, and distal). These slides were stained with hematoxylin-eosin and Verhoeff's method for elastic fibers; later, they underwent histomorphological analyses. These analyses were blind as regards the type of stent implanted and semiquantitative scores were used for the assessment of inflammation7, fibrin deposits8, and degree of injury9.
Statistical Analysis
Quantitative data are expressed as mean ± standard deviation (SD) or median. After verifying that the data were normally distributed, the simple analysis of variance (one-way ANOVA) was calculated for comparison of the means between the groups; post-hoc analysis was carried out when statistically significant differences were observed between these groups. The Statistical Package for the Social Sciences (SPSS) software, version 20.0, was used for data analysis and the significance level was set at 5%.
Financial disclosure
Office of Science and Technology and Strategic Inputs (SCTIE)/Department of Science and Tecnnology (DECIT) of the Ministry of Health (MS), National Council of Scientific and Technological Development (CNPq), Studies and Projects Financer (FINEP) of the Ministry of Science and Technology (MCT) and Foundation for Research Support of the State of São Paulo (Fapesp).
Results
The stents were successfully implanted in all target coronary arteries, with no complications during the implantation procedures or in the immediate post-procedure period.
One animal (number 10) died on day six after stent implantation. The death cause determined by pathological study of the heart was acute inferior myocardial infarction due to occlusion of the right coronary artery in which a stent coated with biodegradable polymer on the luminal and abluminal surfaces had been implanted (Group II stent). The other arteries - anterior descending and circumflex, and the stents implanted in these arteries, were patent, with no firmly adherent intraluminal thrombi. This early death determined an early mortality rate of 6.6% (one in 15 animals), which, according to an Investigators Consensus, is representative of "good implantation technique and stent technology"10 (rate should be lower than 10%).
On day 28 after stent implantation, control coronary angiography performed in the surviving animals showed arterial segments with patent stents and no image suggestive of thrombus.
Findings of quantitative coronary angiography, intracoronary ultrasonography and histopathology are described in Table 2.
Table 2.
Results of quantitative coronary angiography, intracoronary ultrasonography and histomorphology
| Group | p value | |||||
|---|---|---|---|---|---|---|
| I (N = 9) | II (N = 9) | III (N = 8) | IV (N = 9) | V (N = 10) | ||
| Baseline RD (mm) | 2.59 ± 0.21 | 2.62 ± 0.20 | 2.63 ± 0.30 | 2.61 ± 0.24 | 2.50 ± 0.43 | 0.901 |
| Ballon inflation pressure (ATM) | 9.0 ± 1.9 | 8.0 ± 1.7 | 7.6 ± 2.2 | 9.3 ± 1.6 | 9.0 ± 2.1 | 0.348 |
| Balloon diameter (mm) | 2.76 ± 0.27 | 2.79 ± 0.24 | 2.89 ± 0.32 | 2.83 ± 0.19 | 2.71 ± 0.26 | 0.716 |
| Balloon/artery ratio | 1.06 ± 0.04 | 1.06 ± 0.08 | 1.10 ± 0.07 | 1.09 ± 0.10 | 1.10 ± 0.10 | 0.845 |
| MLD at procedure termination (mm) | 2.67 ± 0.23 | 2.74 ± 0.22 | 2.69 ± 0.21 | 2.73 ± 0.22 | 2.59 ± 0.26 | 0.749 |
| RD on control angiography (mm) | 2.30 ± 0.30 | 2.49 ± 0.32 | 2.39 ± 0.30 | 2.48 ± 0.22 | 2.54 ± 0.30 | 0.470 |
| MLD on control angiography (mm) | 1.64 ± 0.61 | 1.59 ± 0.45 | 1.57 ± 0.49 | 1.95 ± 0.43 | 1.85 ± 0.36 | 0.379 |
| Percentage stenosis (%) | 29 ± 20 | 36 ± 14 | 33 ± 19 | 22 ± 13 | 26 ± 15 | 0.443 |
| Late lumen loss(mm) | 1.02 ± 0.60 | 1.24 ± 0.48 | 1.11 ± 0.54 | 0.72 ± 0.44 | 0.78 ± 0.39 | 0.253 |
| Luminal area (mm2) | 4.49 ± 2.16 | 4.29 ± 1.53 | 4.33 ± 1.40 | 5.77 ± 3.32 | 6.03 ± 2.18 | 0.001 * |
| Vessel area (mn2) | 6.95 ± 1.40 | 6.90 ± 1.27 | 6.97 ± 0.87 | 7.00 ± 1.10 | 7.00 ± 1.58 | 0.305 |
| Stent area (mm2) | 7.09 ± 1.40 | 7.03 ± 1.27 | 7.07 ± 0.87 | 7.07 ± 1.10 | 7.00 ± 1.70 | 0.676 |
| Neointimal area (mm2) | 2.60 ± 1.99 | 2.74 ± 1.51 | 2.74 ± 1.30 | 1.30 ± 1.14 | 0.97 ± 0.84 | 0.001 * |
| Percentage neointimal area (%) | 35 ± 25 | 38 ± 18 | 39 ± 19 | 19 ± 18 | 15 ± 12 | 0.001 * |
| Inflammation (median) (min-max) | 1 (0 - 2) | 1 (0 - 2) | 1 (0 - 3) | 1 (0 - 1) | 1 (0 - 1) | 0.999 |
| Schwartz injury (median) (min-max) | 1 (0 - 3) | 1 (0 - 2) | 1 (1 - 3) | 1 (0 - 2) | 1 (0 - 2) | 0.999 |
Group IV versus Groups I, II, III and Group V versus Groups I, II, III.
Group I: bare-metal stents; Group II: stents with bioabsorbable polymer on the luminal and abluminal surfaces; Group III: stents with bioabsorbable polymer on the abluminal surface; Group IV: stents with bioabsorbable polymer and sirolimus on the luminal and abluminal surfaces; Group V: stents with bioabsorbable polymer and sirolimus only on the abluminal surface; RD: reference diameter; MLD: minimum lumen diameter.
Quantitative Coronary Angiography
On quantitative coronary angiography, the porcine coronary arteries had a reference diameter of approximately 2.6 mm during the stent implantation procedure. The inflation pressure for stent implantation was, on average, of 8.5 ATM (5 to 12 ATM; p = 0.348), reaching a balloon: artery ratio of 1.1:1 to cause moderate injury to the arterial wall.
Control quantitative coronary angiography on day 28 after the procedure did not show any statistically significant difference between the groups.
Intracoronary ultrasonography
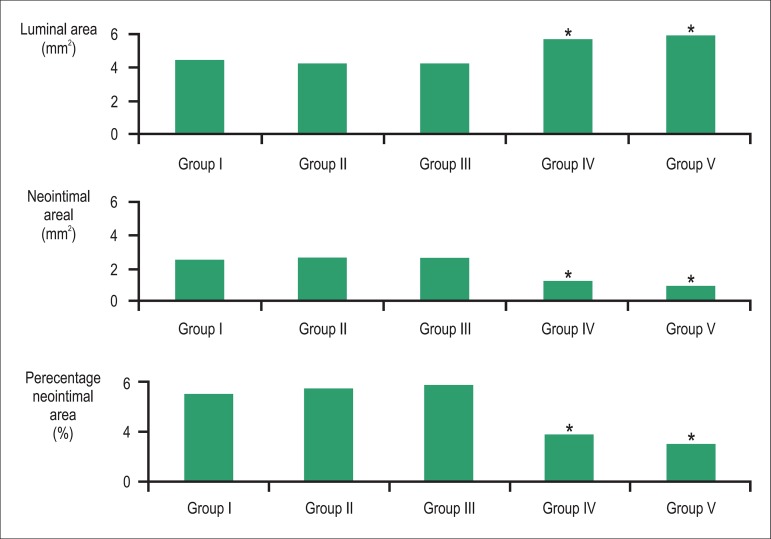
On intracoronary ultrasonography, adequate stent strut apposition was observed in all cases on day 28 after implantation. Also, statistically significant larger luminal areas (mm2) were observed in the drug-eluting stents (Groups IV and V) in relation to control stents (Groups I, II and III) (p = 0.001). Likewise, the neointimal area and percentage neointimal area were significantly smaller in these drug-eluting stents in relation to control stents (p = 0.001 for comparisons of Groups IV and V individually versus Groups I, II and III), as shown in Figure 2.
Figure 2.
Luminal area (mm2), neointimal area (mm2), and percentage neointimal area (%) observed in the experimental groups I to V. * p value < 0.05 for Group IV versus Groups I, II and III, and Group V versus Groups I, II and III.
The neointimal hyperplasia observed in the stents coated with bioabsorbable polymer and sirolimus only on the abluminal surface (Group V, InspironTM stent) was equivalent to that observed in stents with the same coating on the luminal and abluminal surfaces (Group IV), with no statistically significant difference (p = 0.913).
Histomorphology
The injury and inflammation scores were low and showed no statistically significant differences between the groups (p = 0.999). Figure 3 shows histological images of the neointimal hyperplasia on day 28 after implantation of a bare-metal stent (on the left) and of a drug-eluting stent (on the right) in arteries.
Figure 3.
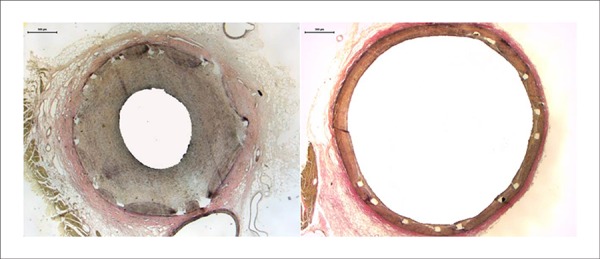
Cross-sectional views of porcine coronary arteries on day 28 after bare-metal stent implantation (Group I, left) and biodegradable polymer-coated stent with sirolimus elution on the abluminal surface (Group V) (right). Magnification 40X.
Discussion
Preclinical studies in laboratory animals for the development and improvement of coronary stents are important to provide an initial idea of the mechanical performance, safety and efficacy profile of the stents, in addition to being required by regulatory agencies for the approval of these devices for clinical use11.
Despite all the benefits from the first-generation drug-eluting stents which brought a revolution in the treatment of atherosclerotic coronary disease, questions arose on the long-term safety of these devices, especially in relation to late thrombosis12.
After the initial reduction in the number of drug-eluting stents implantation observed at that time, new efforts have focused on the development of stents with the use of different alloys (chromium-cobalt and platinum-chromium), new biocompatible or biodegradable polymers, and the incorporation of new drugs (everolimus, zotarolimus and biolimus A9), aiming to increase the safety of these devices.
Although the pathophysiology of stent thrombosis is multifactorial, several animal and clinical evidences have pointed to the presence of durable polymers as responsible for inflammation and delayed vascular repair13. These evidences have fostered the development of biodegradable polymer-based stents and bioabsorbable stents.
In the present preclinical study on porcine coronary arteries, we observed that biodegradable polymer-coated stents with sirolimus release only from the abluminal surface (Group V, InspironTM stent) showed neointimal hyperplasia quantitatively similar to that of polymer and sirolimus-coated stents on the luminal and abluminal surfaces (Group IV). The groups with sirolimus-releasing stents (Groups IV and V) showed lower neointimal area in relation to the bare-metal stents (Groups I, II and III). No difference was observed between the five groups in relation to the injury and inflammation scores, thus showing that both the bioabsorbable polymer and the antiproliferative drug used were safe and effective.
The InspironTM eluting-stent is characterized by being composed of a chromium-cobalt L605 alloy, biodegradable polymer coating, and sirolimus elution only on the abluminal surface. Possibly because of being coated with a biodegradable polymer, it is safer than durable-polymer stents. In a meta-analysis of randomized clinical trials comparing stent thrombosis rates up to 4 years after use of the Yukon (Translumina, Hechingen, Germany) and BiomatrixTM Flex (Biosensors International, Singapore) biodegradable polymer-based drug-eluting stents versus the CypherTM (Cordis Corp, Miami Lakes, Fl, USA) durable-polymer stent, the biodegradable polymer-based stents showed less definitive stent thrombosis, less clinical endpoints and less target-lesion revascularization than the CypherTM durable-polymer stent14.
An experimental study in a porcine model compared the endothelial activity and inflammation scores in animals undergoing NoboriTM stent implantation - a stent coated with bioabsorbable polymer and biolimus only on its abluminal surface, to that of animals undergoing CypherTM stent implantation, and found increased endothelial relaxation, decreased production of superoxide anion, and less inflammation in the coronary segments in the group receiving the NoboriTM stent15.
Recent findings, however, suggest that the presence of a durable polymer per se does not determine a greater risk of late thrombosis16,17. In an experimental study, Kolandaivelu et al18 observed that drug-eluting stents with durable polymer (XIENCE) showed less early thrombogenicity than a corresponding bare-metal stent (Multilink Vision), i.e., polymer and drug coating provided a protective effect for acute thrombogenicity. Factors such as the stent design and strut thickness emerged as other important factors predisposing stent thrombosis.
Several other stents using biodegradable polymer and antiproliferative drugs released only from the abluminal surface have been developed. Examples of these stents are the stainless steel biolimus A9-eluting NoboriTM (Terumo Corp., Japan) and BiomatrixTM (Biosensors International, Singapore) stents ; the stainless steel paclitaxel-eluting JACTAXTM stent (Boston Scientific, Natick, USA) , and the chromium-cobalt sirolimus-eluting FirehawkTM stent (MicroPort Medical, Shanghai, China).
The InspironTM stent has been extensively studied in experimental animals with results comparable to those of other drug-eluting stents as regards safety, stent-strut endothelialization, and neointimal hyperplasia19,20.
Clinical studies are underway to evaluate the efficacy of this new drug-eluting stent. The preliminary clinical results of the InspironTM stent (INSPIRON I) have shown a good angiographic response, with late lumen loss of 0.18 mm; good ultrasonographic response, with percentage neointimal obstruction of 8.2%; and target-vessel revascularization of 0%.
A randomized clinical trial (DESTINY) comparing the InspironTM stent with BiomatrixTM stent is currently being conducted, expected to include 165 randomized patients 2:1 (InspironTM stent versus BiomatrixTM).
Study limitations
The model used in the present study was healthy porcine coronary arteries, which may not represent the progression in a vascular segment with atherosclerotic disease. Atherosclerotic animal models have been developed in rabbits and pigs; however, these models are still uncommonly used in preclinical studies for the development and improvement of coronary stents.
Intracoronary ultrasonography was used only in the control on day 28 after stent implantation with the purpose of assessing in-stent neointimal hyperplasia, and not to guide stent implantation. However, despite the known limitations of quantitative coronary angiography, the findings of this method revealed that the stents were adequately implanted (balloon: artery ratio of 1.1:1) and the intracoronary ultrasonographic findings showed adequate stent strut apposition in all cases.
Optical coherence tomography is a method that has been widely used in preclinical and clinical validation studies of new stents; however, this method was not yet available for experimental animal use in our institution at the time the study was carried out.
Conclusions
In this experimental study, the drug-eluting stents coated with sirolimus and bioabsorbable polymer in porcine coronary arteries showed less neointimal hyperplasia when compared to control bare-metal stents. The bioabsorbable polymer-based stent with sirolimus released only from its abluminal surface (InspironTM stent) showed the same neointimal antiproliferative efficacy as the stent with sirolimus released from both the luminal and abluminal surfaces.
Footnotes
Author contributions
Conception and design of the research: Takimura CK, Campos CAH; Acquisition of data: Takimura CK, Campos CAH, Campos JC, Gutierrez PS; Statistical analysis: Takimura CK; Analysis and interpretation of the data: Takimura CK; Writing of the manuscript: Takimura CK, Craveiro PHM; Supervision / as principal investigator: Takimura CK; Critical revision of the manuscript for intellectual content: Campos CAH, Craveiro PHM, Borges TFC, Curado L, Morato SP, Laurindo FRM, Lemos Neto PA.
Sources of Funding
This study was partially funded by SCTIE/ DECIT do Ministério da Saúde, CNPQ, FINEP, FAPESP.
Study Association
This study is not associated with any thesis or dissertation work.
References
- 1.Morice MC, Serruys PW, Sousa JE, Fajadet J, Ban Hayashi E, Perin M, et al. A randomized comparison of a sirolimus-eluting stent with a standard stent for coronary revascularization. N Engl J Med. 2002;346(23):1773–1780. doi: 10.1056/NEJMoa012843. [DOI] [PubMed] [Google Scholar]
- 2.Stone GW, Ellis SG, Cox DA, Hermiller J, et al. O'Shaughnessy C, Mann JT. One-year clinical results with the slow-release, polymer-based, paclitaxel-eluting taxus stent: The TAXUX-IV trial. Circulation. 2004;109(16):1942–1947. doi: 10.1161/01.CIR.0000127110.49192.72. [DOI] [PubMed] [Google Scholar]
- 3.Pfisterer M, Brunner-La Rocca HP, Buser PT, Rickenbacher P, Hunziker P, Mueller C, et al. Late clinical events after clopidogrel discontinuation may limit the benefit of drug-eluting stents: an observational study of drug-eluting versus bare-metal stents. J Am Coll Cardiol. 2006;48(12):2584–2591. doi: 10.1016/j.jacc.2006.10.026. [DOI] [PubMed] [Google Scholar]
- 4.Stone GW, Moses JW, Ellis SG, Schofer J, Dawkins KD, Morice MC, et al. Safety and efficacy of sirolimus- and paclitaxel-eluting coronary stents. N Engl J Med. 2007;356(10):998–1008. doi: 10.1056/NEJMoa067193. [DOI] [PubMed] [Google Scholar]
- 5.Iakovou I, Schmidt T, Bonizzoni E, Ge L, Sangiorgi GM, Stankovic G, et al. Incidence, predictors, and outcome of thrombosis after successful implantation of drug-eluting stents. JAMA. 2005;293(17):2126–2130. doi: 10.1001/jama.293.17.2126. [DOI] [PubMed] [Google Scholar]
- 6.Lemos PA, Laurindo FR, Morato SP, Takimura C, Campos CA, Gutierrez OS, et al. Stent coronário de liga cobalto-cromo concebido no Brasil: Achados histológicos preliminares em modelo experimental porcino. Rev Bras Cardiol Invas. 2007;15(4):378–385. [Google Scholar]
- 7.Kornowski R, Hong MK, Tio FO, Bramwell O, Wu H, Leon MB. In-stent restenosis: contributions of inflammatory responses and arterial injury to neointimal hyperplasia. J Am Coll Cardiol. 1998;31(1):224–230. doi: 10.1016/s0735-1097(97)00450-6. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki T, Kopia G, Hayashi S, Bailey LR, Llanos G, Wilensky R, et al. Stent-based delivery of sirolimus reduces neointimal formation in a porcine coronary model. Circulation. 2001;104(10):1188–1193. doi: 10.1161/hc3601.093987. [DOI] [PubMed] [Google Scholar]
- 9.Schwartz RS, Edelman ER, Carter A, Chronos N, Rogers C, Robinson KA, et al. Drug-eluting stents in preclinical studies recommended evaluation from a consensus group. Circulation. 2002;106(14):1867–1873. doi: 10.1161/01.cir.0000033485.20594.6f. [DOI] [PubMed] [Google Scholar]
- 10.Schwartz RS, Edelman E, Virmani R, Carter A, Granada JF, Kaluza GL, et al. Drug-eluting stents in preclinical studies: updated consensus recommendations for preclinical evaluation. Circ Cardiovasc Intervent. 2008;1(2):143–153. doi: 10.1161/CIRCINTERVENTIONS.108.789974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Suzuki Y, Yeung AC, Ikeno F. The pre-clinical animal model in the translational research of interventional cardiology. JACC Cardiovasc Interv. 2009;2(5):373–383. doi: 10.1016/j.jcin.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 12.Camenzind E, Steg PG, Wijns W. Stent thrombosis late after implantation of first-generation drug-eluting stents: a cause for concern. Circulation. 2007;115(11):1440–1455. doi: 10.1161/CIRCULATIONAHA.106.666800. [DOI] [PubMed] [Google Scholar]
- 13.Nakazawa G, Finn AV, Vorpahl M, Ladich ER, Kolodgie FD, Virmani R. Coronary responses and differential mechanisms of late stent thrombosis attributed to first-generation sirolimus- and paclitaxel-eluting stents. J Am Coll Cardiol. 2011;57(4):390–398. doi: 10.1016/j.jacc.2010.05.066. [DOI] [PubMed] [Google Scholar]
- 14.Stefanini GG, Byrne RA, Serruys PW, de Waha A, Meier B, Massberg S, et al. Biodegradable polymer drug-eluting stents reduce the risk of stent thrombosis at 4 years in patients undergoing percutaneous coronary intervention: a pooled analysis of individual patient data from the ISAR-test 3, ISAR-test 4, and LEADERS randomized trials. Eur Heart J. 2012;33(10):1214–1222. doi: 10.1093/eurheartj/ehs086. [DOI] [PubMed] [Google Scholar]
- 15.Pendyala LK, Matsumoto D, Shinke T, Iwasaki T, Sugimoto R, Hou D, et al. Nobori stent shows less vascular inflammation and early recovery of endothelial function compared with Cypher stent. JACC Cardiovasc Interv. 2012;5(4):436–444. doi: 10.1016/j.jcin.2011.11.013. [DOI] [PubMed] [Google Scholar]
- 16.Sabate M, Cequier A, Iniguez A, Serra A, Hernandez-Antolin R, Mainar V, et al. Everolimus-eluting stent versus bare-metal stent in ST-segment elevation myocardial infarction (examination): 1 year results of a randomised controlled trial. Lancet. 2012;380(9852):1482–1490. doi: 10.1016/S0140-6736(12)61223-9. [DOI] [PubMed] [Google Scholar]
- 17.Palmerini T, Biondi-Zoccai G, Della Riva D, Stettler C, Sangiorgi D, et al. D'Ascenzo F. Stent thrombosis with drug-eluting and bare-metal stents: Evidence from a comprehensive network meta-analysis. Lancet. 2012;379(9824):1393–1402. doi: 10.1016/S0140-6736(12)60324-9. [DOI] [PubMed] [Google Scholar]
- 18.Kolandaivelu K, Swaminathan R, Gibson WJ, Kolachalama VB, Nguyen-Ehrenreich KL, Giddings VL, et al. Stent thrombogenicity early in high-risk interventional settings is driven by stent design and deployment and protected by polymer-drug coatings clinical perspective. Circulation. 2011;123(13):1400–1409. doi: 10.1161/CIRCULATIONAHA.110.003210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Takimura CK, Galon MZ, Lopes A, Jr, Carvalho J, Ferreira SK, Chaves MJ, et al. Avaliação pela tomografia de coerência óptica de stent nacional recoberto com polímero biodegradável eluidor de sirolimus vs. Stent eluidor de biolimus a9 em artérias coronárias porcinas. Rev Bras Cardiol Invasiva. 2011;19(2):138–144. [Google Scholar]
- 20.Takimura CK, Watanabe IS, Laurindo FR, Gutierrez PS, Aiello VD, Morato SP, et al. Assessment of stent strut endothelialization in iliac arteries of rabbits. Arq Bras Cardiol. 2012;99(6):1123–1128. doi: 10.1590/s0066-782x2012005000103. [DOI] [PubMed] [Google Scholar]