Abstract
Background
The treatment of heart failure has evolved in recent decades suggesting that survival is increasing.
Objective
To verify whether there has been improvement in the survival of patients with advanced heart failure.
Methods
We retrospectively compared the treatment and follow-up data from two cohorts of patients with systolic heart failure admitted for compensation up to 2000 (n = 353) and after 2000 (n = 279). We analyzed in-hospital death, re-hospitalization and death in 1 year of follow-up. We used Mann-Whitney U test and chi-square test for comparison between groups. The predictors of mortality were identified by regression analysis through Cox proportional hazards model and survival analysis by the Kaplan-Meier survival analysis.
Results
The patients admitted until 2000 were younger, had lower left ventricular impairment and received a lower proportion of beta-blockers at discharge. The survival of patients hospitalized before 2000 was lower than those hospitalized after 2000 (40.1% vs. 67.4%; p<0.001). The independent predictors of mortality in the regression analysis were: Chagas disease (hazard ratio: 1.9; 95% confidence interval: 1.3-3.0), angiotensin-converting-enzyme inhibitors (hazard ratio: 0.6; 95% confidence interval: 0.4-0.9), beta-blockers (hazard ratio: 0.3; 95% confidence interval: 0.2-0.5), creatinine ≥ 1.4 mg/dL (hazard ratio: 2.0; 95% confidence interval: 1.3-3.0), serum sodium ≤ 135 mEq/L (hazard ratio: 1.8; 95% confidence interval: 1.2-2.7).
Conclusions
Patients with advanced heart failure showed a significant improvement in survival and reduction in re-hospitalizations. The neurohormonal blockade, with angiotensin-converting-enzyme inhibitors and beta-blockers, had an important role in increasing survival of these patients with advanced heart failure.
Keywords: Heart Failure / therapy, Prognosis, Heart Failure / mortality, Chagas Disease
Introduction
Heart failure (HF) is a clinical syndrome of which evolution is known to have high morbidity and mortality1,2. In epidemiological studies, HF patients showed a significant reduction in quality of life and a worse evolution than many types of cancer3.
Treatment with neurohormonal blockers has modified this history, reducing the high mortality, the rate of re-hospitalizations and improving quality of life in patients with this syndrome4. This improvement has been demonstrated in clinical trials and controlled studies, but we do not know whether this improvement has also been observed in the real world, among patients in the institutions, clinics and offices, and particularly, we have no data on the Brazilian population4.
Working in a tertiary hospital in São Paulo, we followed the evolution of HF patients in the last two decades and observed that the population we treated during these years has not changed substantially regarding characteristics, as the admission criteria have not changed. This fact allowed us to compares the outcome of patients, considering two periods: before and after the year 2000.
This study sought to assess whether the outcomes of patients with HF changed when comparing the two periods and verify, among the studied variables, which were associated with prognosis of this syndrome.
Methods
A total of 632 hospitalized patients were prospectively studied in a tertiary hospital in São Paulo, all with advanced HF, systolic dysfunction with ejection fraction < 40%, in NYHA (New York Heart Association) III / IV. Patients in this hospital came from the emergency room and were transferred there when they did not compensate after the first measures or because they required inotropic support for compensation. These selection criteria for hospitalization led to the admission of more severe patients with severe clinical manifestation.
All patients underwent clinical and laboratory assessment, including biochemical analysis, CBC, echocardiography and radiological examinations. Regarding the etiology of heart disease, patients were divided into three groups: those with chagasic etiology, those with ischemic etiology and those with nonischemic etiology. The diagnosis of Chagasic heart disease was established by the presence of positive serological reactions, and ischemic heart disease was confirmed by the presence of a history of heart attack, angina or confirmed by coronary angiography. In the absence of these characteristics, the patient was considered to have non-ischemic heart disease.
These patients are part of a prospective study database of patients hospitalized in our service, due to advanced, decompensated HF and all met the same abovementioned inclusion criteria2,5-8. Patients were included in different years, which allowed us to perform a temporal analysis regarding the evolution of prognosis and treatment of this syndrome. For the purpose of this analysis, performed retrospectively, the patients were divided into two groups: those admitted until December 31, 2000 and those admitted after that date. Patients included in the study admitted before 2000 were part of prospective studies in the years 1992, 1994, 1996 and 19995-8. Patients enrolled after 2000 were studied in 2005 and 20062. We compared the characteristics of the two groups, considering clinical, laboratory, and evolution aspects.
Patients were followed for 1 year, and the vital status of the patients, number of visits to the emergency room and need for rehospitalization were determined by telephone or by reviewing electronic medical records. The clinical outcome analyzed was mortality from all causes during the follow-up period.
Among these patients, a subgroup had the treatment analyzed during and after discharge, and predictors of mortality were assessed in this subgroup, consisting of 333 patients (52.7% of total)2,8. This subgroup was selected based on the availability of data on drug therapy used during hospitalization and pre-hospital discharge.
Continuous variables were shown as means ± standard deviation and categorical variables as frequencies and percentages. We compared the characteristics of patients regarding mortality at the end of follow-up. Continuous variables were analyzed by Mann-Whitney U test and categorical variables by the chi-square test or Fisher exact test.
Predictors of mortality were determined by uni- and multivariate analysis, using the Cox proportional hazards method. A regression model was constructed for the primary endpoint, adjusted for clinical and laboratory characteristics as well as those of administered drugs. The criterion for model variable selection was a p value < 0.200 in the univariate analysis. The final model was built using a stepwise forward procedure. All predictor variables with p < 0.05 were mantained in the final model. Hazard ratio was shown, with the corresponding confidence interval of 95% (95% CI) and p value.
Based on the follow-up data, survival curves were constructed using the Kaplan-Meier method. All statistical analyses were performed using the statistical software Statistical Package for Social Sciences (SPSS).
P values are two-tailed and the significance level was set at 5%.
Results
The mean age of patients was 54.8 ± 15.1 years and most were males, 435 (68.8%). The mean left ventricular ejection fraction (LVEF) was 28.2 ± 7.2% and mean Systolic Blood Pressure (SBP) was 104.6 ± 22.9 mmHg. The most frequent cause of heart disease was non-ischemic, followed by chagasic and ischemic.
Most patients had non-dialytic kidney failure.
A total of 353 patients hospitalized from 1992 to December 31, 2000, and 279 patients hospitalized between 2005 and 2006 were included in the study.
Table 1, shows the comparison of baseline characteristics between patients admitted until 2000 and after 2000.
Table 1.
Comparison of characteristics between the groups before and after 2000
| Characteristics | Population (n = 632) | Year of treatment | p value | |
|---|---|---|---|---|
| Before 2000 (n = 353) | After 2000 (n = 279) | |||
| Age (years) | 54.8 ± 15.1 | 59.0 ± 14.8 | 51.5 ± 14.5 | < 0.001 |
| Male gender | 435 (68.8) | 255 (72.2) | 180 (64.5) | 0.037 |
| Etiology: | ||||
| Ischemic | 132 (20.9) | 56 (15.0) | 76 (27.2) | < 0.001 |
| Non-ischemic (non- chagasic) | 312 (49.4) | 173 (49.0) | 139 (49.8) | 0.839 |
| Chagasic | 188 (29.7) | 124 (35.1) | 64 (22.9) | 0.001 |
| LVEF (%) | 28.2 ± 7.2 | 30.8 ± 5.9 | 24.7 ± 7.3 | < 0.001 |
| Creatinine (mg/dL) | 1.5 ± 0.7 | 1.5 ± 0.5 | 1.5 ± 0.5 | 0.239 |
| Sodium (mEq/L) | 135.7 ± 5.0 | 136.7 ± 4.7 | 134.9 ± 5.1 | < 0.001 |
| SBP (mmHg) | 103.6 (25.4) | 102.6 ± 21.9 | 105.0 ± 30.1 | 0.163 |
| Mortality (1 year) | 264 (41.8) | 200 (56.7) | 63 (22.8) | < 0.001 |
LVEF: left ventricular ejection fraction; SBP: systolic blood pressure.
Patients hospitalized until the year 2000 were 7.5 years younger than those admitted after 2000 and had a less impaired LVEF and lower levels of plasma sodium. The percentage of patients with Chagas disease was higher in admissions until 2000.
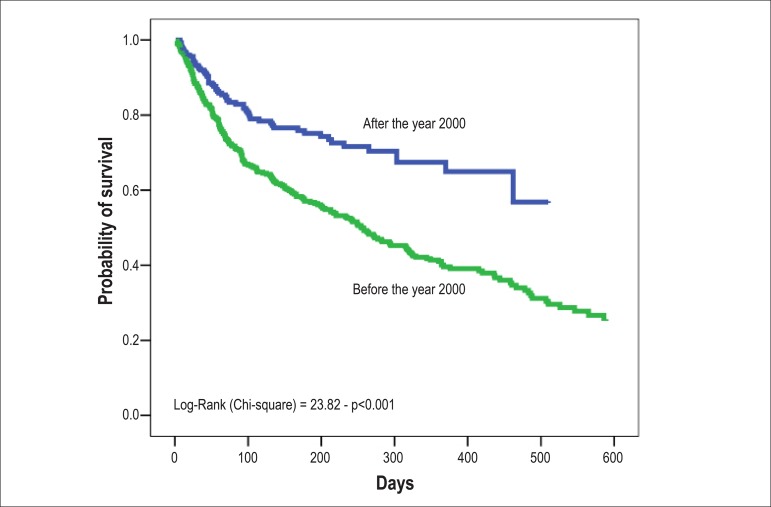
The survival of patients hospitalized until the year 2000 was 40.1% and 67.4%, among those hospitalized after the year 2000, with a 68% increase in the survival rate in the first year of follow-up (Figure 1).
Figure 1.
Survival of patients hospitalized for decompensated heart failure before and after the year 2000. The probability of survival at 1 year of follow-up was 40.1% in hospitalized patients before 2000 and 67.4% in hospitalized patients after 2000 (p < 0.001).
To analyze the possible variables related to survival, we evaluated the data of 333 patients (52.7% of the total). These data are shown in Table 2. This analysis showed that 209 patients (62.8%) needed inotropes in the compensation period. At discharge, most patients were receiving a prescription of renin-angiotensin system blocker (72.4%) and a beta-blocker (59.8%). A total of 186 (55.9%) patients were treated with carvedilol and 13 patients (3.9%) with metoprolol succinate. When comparing the two groups, patients admitted until 2000 received a lower proportion of beta-blocker prescriptions and a higher proportion of digoxin.
Table 2.
Comparison of patients in relation to the year of treatment
| Characteristics | Population (n = 333) | Year of treatment | p value | |
|---|---|---|---|---|
| Before 2000 (n = 70) | After 2000 (n = 263) | |||
| Age (years) | 58.7 ± 15.4 | 54.2 ± 15.8 | 59.9 ± 15.1 | 0.011 |
| Male gender | 213 (64.0) | 48 (68.6) | 165 (62.7) | 0.366 |
| Etiology: | ||||
| Ischemic | 94 (28.2) | 18 (25.7) | 76 (28.9) | 0.599 |
| Non-ischemic (non-chagasic) | 163 (48.9) | 33 (47.1) | 130 (49.4) | 0.734 |
| Chagasic | 76 (22.8) | 19 (27.1) | 57 (21.7) | 0.333 |
| LVEF (%) | 28.0 ± 11.4 | 31.3 ± 8.4 | 27.1 ± 11.9 | < 0.001 |
| Hemoglobin (g/L) | 13.2 ± 2.0 | 13.9 ± 2.1 | 13.0 ± 1.9 | 0.001 |
| Urea (mg/dL) | 74.7 ± 42.5 | 72.9 ± 35.2 | 75.1 ± 44.2 | 0.842 |
| Creatinine (mg/dL) | 1.5 ± 0.7 | 1.4 ± 0.5 | 1.5 ± 0.8 | 0.699 |
| Sodium (mEq/L) | 136.6 ± 4.9 | 135.9 ± 5.4 | 136.7 ± 4.7 | 0.083 |
| SBP (mmHg) | 105.3 ± 23.3 | 111.7 ± 25.4 | 103.5 ± 22.4 | 0.017 |
| DBP (mmHg) | 68.7 ± 18.1 | 76.7 ± 17.9 | 66.3 ± 17.5 | < 0.001 |
| Medications: | ||||
| Dobutamine | 187 (57.9) | 36 (51.4) | 151 (57.4) | 0.216 |
| Dobutamine | 6 (1.9) | 0 (0.0) | 6 (2.3) | 0.346 |
| Levosimendan | 16 (5.0) | 0 (0.0) | 16 (6.1) | 0.028 |
| ACEI | 241 (72.4) | 60 (85.7) | 181 (68.8) | 0.005 |
| Beta-blockers | 199 (59.8) | 8(11.4) | 191 (72.6) | < 0.001 |
| Losartan | 42 (12.7) | 0 (0.0) | 42 (16.0) | < 0.001 |
| Nitrates | 117 (35.2) | 39 (55.7) | 78 (29.7) | < 0.001 |
| Hydralazine | 108 (32.5) | 16 (22.9) | 92 (35.0) | 0.052 |
| Digoxin | 194 (58.6) | 64 (92.8) | 130 (49.4) | < 0.001 |
| Spironolactone | 48 (14.5) | 0 (0.0) | 48 (18.3) | < 0.001 |
| Furosemide | 261 (78.6) | 70 (100.0) | 191 (72.6) | < 0.001 |
| Hydrochlorothiazide | 59 (17.8) | 0 (0.0) | 59 (22.4) | < 0.001 |
| Clinical results: | ||||
| Mortality in-Hospital | 37 (11.1) | 14 (20.0) | 23 (8.7) | 0.008 |
| Mortality at follow-up (1 year) | 106 (31.8) | 44 (62.9) | 62 (23.6) | < 0.001 |
| Rehospitalization | 109 (32.8) | 36 (51.4) | 73 (27.9) | < 0.001 |
| Clinical events | 168 (49.2) | 56 (80.0) | 108 (41.1) | < 0.001 |
Data are expressed as mean ± standard deviation or number (percentage). LVEF: left ventricular ejection fraction; SBP: systolic blood pressure; DBP: diastolic blood pressure; ACEI: angiotensin-converting enzyme inhibitor.
Clinical events, death or rehospitalization within 1 year.
In this analysis, patients admitted until the year 2000 had higher in-hospital mortality (20.0% vs 8.7%, p = 0.008) and a higher number of re-hospitalizations than those admitted after 2000 (51.4% vs. 27.9%, p < 0.001). At 1 year of follow up, mortality of those admitted until the year 2000 was 62.9% vs. 23.6% for those hospitalized after 2000 (p < 0.001).
The length of hospital stay did not differ between the two groups, being 28.3 ± 21.1 days in those admitted until 2000 and 25.1 ± 16.7 days (p = 0.251) in those hospitalized after the year 2000.
Tables 3 and 4 show the comparison of patient characteristics regarding mortality at 1 year of follow up and the univariate and multivariate regression analysis of predictors of death in this period. Chagasic etiology, presence of renal impairment (higher urea levels and creatinine), lower levels of sodium and nitrate use were predictors of increased mortality. Variables associated with reduced mortality were the prescription of Angiotensin-Converting Enzyme Inhibitor (ACEI) and beta-blockers. In the multivariate regression analysis, five variables were identified as independent predictors of mortality, with three being associated with worse prognosis (Chagas disease, creatinine ≥ 1.4 mg/dL, and sodium ≤ 135 mEq/L) and two associated with improved prognosis: the prescription of ACEI and beta-blockers.
Table 3.
Comparison of patients in relation to 1-year mortality
| Characteristics | 1-year mortality | p value | |
|---|---|---|---|
| Yes (n = 106) | No (n = 227) | ||
| Age (years) | 58.2 ± 17.3 | 58.9 ± 14.5 | 0.928 |
| Male gender | 63 (59.4) | 150 (66.1) | 0.239 |
| Etiology: | |||
| Ischemic | 27 (25.5) | 67 (29.5) | 0.445 |
| Non-ischemic (non-chagasic) | 44 (41.5) | 119 (52.4) | 0.063 |
| Chagasic | 35 (33.0) | 41 (18.1) | 0.002 |
| LVEF (%) | 28.9 ± 9.5 | 27.6 ± 12.1 | 0.116 |
| Hemoglobin (g/L) | 13.3 ± 2.2 | 13.1 ± 1.8 | 0.311 |
| Hemoglobin (g/L) | 80.8 ± 42.8 | 71.8 ± 42.1 | 0.016 |
| Creatinine (mg/dL) | 1.5 ± 0.5 | 1.5 ± 0.8 | 0.043 |
| Sodium (mEq/L) | 135.3 ± 4.9 | 137.1 ± 4.8 | 0.001 |
| SBP (mmHg) | 103.1 ± 20.7 | 106.4 ± 24.5 | 0.505 |
| DBP (mmHg) | 69.3 ± 15.3 | 68.4 ± 19.3 | 0.503 |
| Medications | |||
| Inotropic agents | 75 (71.4) | 127 (57.5) | 0.015 |
| ACEI | 69 (65.1) | 172 (75.8) | 0.042 |
| Beta-blocker | 36 (34.0) | 163 (71.8) | < 0.001 |
| Losartan | 12 (11.3) | 30 (13.2) | 0.649 |
| Nitrates | 47 (44.3) | 70 (30.8) | 0.014 |
| Hydralazine | 38 (35.8) | 70 (30.8) | 0.333 |
| Digoxin | 76 (71.7) | 118 (52.0) | < 0.001 |
| Spironolactone | 11 (10.4) | 37 (16.3) | 0.161 |
| Furosemide | 90 (84.9) | 171 (75.3) | 0.032 |
| Hydrochlorothiazide | 18 (17.0) | 41 (18.1) | 0.839 |
Data are expressed as mean ± standard deviation or number (percentage). LVEF: left ventricular ejection fraction; SBP: systolic blood pressure; DBP: diastolic blood pressure; ACEI: angiotensin-converting enzyme inhibitor.
Table 4.
Univariate and multivariate analysis regression (Cox) of predictors of death
| Predictor (univariate analysis) | Hazard ratio | 95% Confidence Interval (95%CI) | p value |
|---|---|---|---|
| Age > 60 years | 1.0 | 0.7 - 1.5 | 0.998 |
| Male gender | 0.8 | 0.5 - 1.2 | 0.247 |
| Etiology: | |||
| Ischemic | 0.8 | 0.5 - 1.3 | 0.389 |
| Non-ischemic (non-chagasic) | 0.7 | 0.5 - 1.1 | 0.124 |
| Chagasic | 1.8 | 1.2 - 2.7 | 0.008 |
| LVEF < 0.25 | 0.8 | 0.6 - 1.3 | 0.382 |
| Anemia | 1.0 | 0.7 - 1.6 | 0.939 |
| Urea ≥ 60 mg/dL | 1.7 | 1.1 - 2.5 | 0.013 |
| Creatinine ≥ 1.4 mg/dL | 1.6 | 1.1 - 2.4 | 0.013 |
| Sodium ≤ 135 mEq/L | 1.8 | 1.2 - 2.6 | 0.004 |
| SBP < 90 mmHg | 0.9 | 0.5 - 1.5 | 0.640 |
| Medications | |||
| Inotropic agents | 1.7 | 1.1 - 2.7 | 0.008 |
| ACEI | 0.6 | 0.4 - 0.9 | 0.020 |
| Beta-blocker | 0.3 | 0.2 - 0.5 | <0.001 |
| Losartan | 1.1 | 0.6 - 2.0 | 0.788 |
| Nitrates | 1.6 | 1.1 - 2.4 | 0.017 |
| Hydralazine | 1.4 | 0.9 - 2.1 | 0.097 |
| Digoxin | 1.4 | 0.9 - 2.2 | 0.106 |
| Spironolactone | 0.7 | 0.4 - 1.3 | 0.274 |
| Hydrochlorothiazide | 1.2 | 0.7 - 2.0 | 0.483 |
| Furosemide | 1.4 | 0.8 - 2.4 | 0.205 |
| Predictor (multivariate analysis) | Hazard ratio | 95% confidence Interval | p value |
| Creatinine ≥ 1,4 mg/dL | 2.0 | 1.3 - 3.0 | 0.002 |
| Chagasic etiology | 1.9 | 1.3 - 3.0 | 0.002 |
| ACEI | 0.6 | 0.4 - 0.9 | 0.040 |
| Beta-blocker | 0.3 | 0.2 - 0.5 | < 0.001 |
| Sodium ≤ 135 mEq/L | 1.8 | 1.2 - 2.7 | 0.003 |
LVEF: left ventricular ejection fraction; SBP: systolic blood pressure; ACEI: angiotensin-converting enzyme inhibitor.
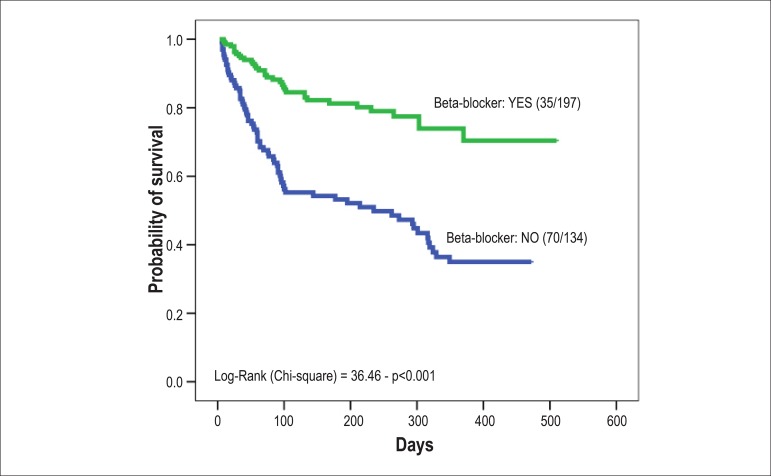
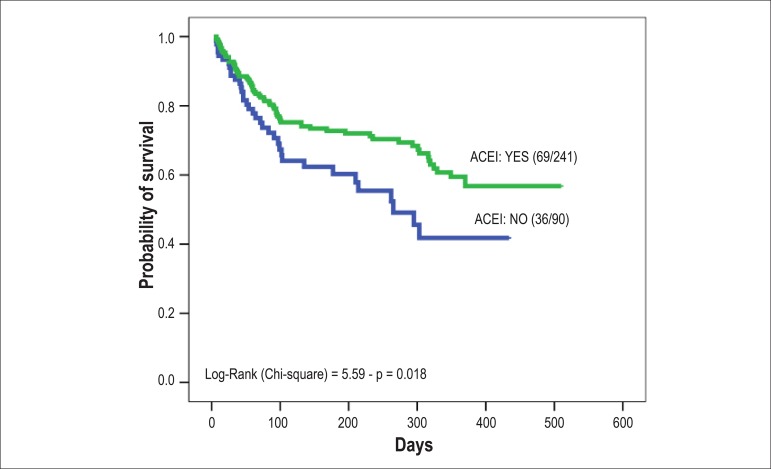
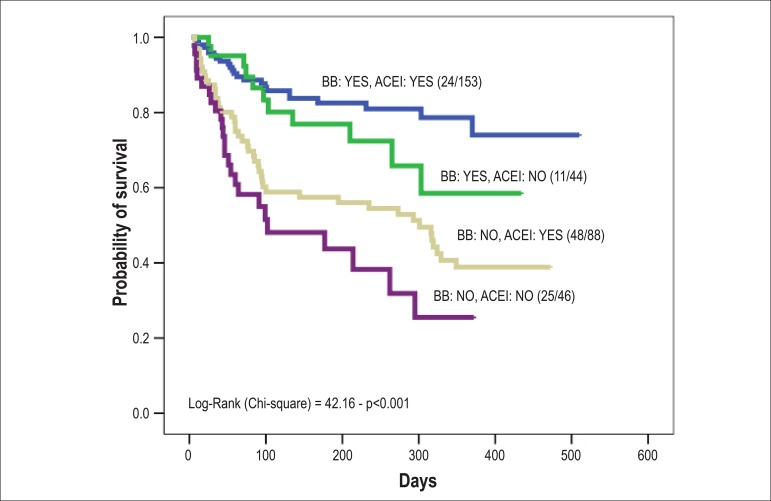
Figures 2 and 3 show survival curves stratified for ACEI and beta-blockers. In Figure 4, the survival curve was stratified for the combined use of ACEI and beta-blockers, demonstrating improvement in survival of patients who received the combined therapy with the two medications.
Figure 2.
Survival at 1 year of follow-up of patients hospitalized for decompensated heart failure, according to the use of beta-blockers: 73.9% vs. 35.0% (p <0.001).
Figure 3.
Survival at 1 year of follow-up of patients hospitalized for decompensated heart failure according to the use of angiotensin-converting enzyme inhibitors: 59.5% vs. 41.8% (p = 0.018).
Figure 4.
Survival at 1 year of follow-up of patients hospitalized for heart failure, according to the combined use of beta-blockers (BB) and angiotensin-converting enzyme inhibitors (ACEI). Patients were stratified into four groups according to the use of BB / ACEI: yes/yes, yes/no, no/yes, no/no. The probability of survival was, respectively: 78.7%, 58.5%, 38.9% and 25.5% (p < 0.001).
Discussion
According to the results of this observational study, we observed that in this new century, the survival of patients with advanced HF has improved significantly, as well as the rates of re-hospitalization. Treatment with neurohormonal blockers, especially ACEI and beta-blockers, was associated with this increase in survival rates.
Heart failure, in its advanced form, is a malignant disease with a higher mortality rate than a few types of cancer3. Even with the current treatment, mortality can be high in the most severe forms, as it has an association with the intensity of the heart disease and its clinical manifestations9. Patients with advanced disease are referred to our institution, a tertiary hospital in São Paulo, which results in higher mortality than that observed in other institutions. Our current mortality rate is approximately 8% and we observed that approximately a quarter of patients who were discharged died in the first year of follow-up2.
Although this mortality rate is still high, when we compared data from patients hospitalized until the year 2000, we found a significant reduction. It should be noted that when comparing the characteristics of the study population in two periods, before and after 2000, we observed that they are quite similar, but the hospitalized population after 2000 shows alterations that indicate more pronounced clinical manifestations, such as higher levels of urea and creatinine at admission and lower LVEF. Despite these signs of greater severity, when comparing the two periods, there was a significant reduction in mortality, which decreased from 20% to the current 8.8%2. This reduction was probably due to more aggressive management of cardiac decompensation and the higher proportion of patients currently being treated with ACEI and beta-blockers10,11.
In our institution, ACEI and beta-blockers are not systematically withdrawn at hospitalization for cardiac decompensation12. In general, ACEI have their dose increased, as vasoconstriction is the major pathophysiological alteration in cardiac decompensation. The beta-blocker is maintained and in cases that need inotropes, the dose of the beta-blocker is halved, which results in the fact many patients continue taking 6.25 mg or 12.5 mg of carvedilol twice daily. In the multivariate analysis, the prescription of ACEI and beta-blockers was associated with reduced mortality. Therefore, the most intense neurohormonal blockade played an important role in this increase in in-hospital survival. Thus, although the mortality rate is still high, it is decreasing, when one considers the data from the two periods at our institution. It is noteworthy the fact that data from the National Health System (SUS) do not show the occurrence of the reduction we observed, but showing in fact, an increase in mortality (5.41 % to 6.97 %) from 1992 to 2002, when analyzing all hospitalizations for HF in Brazil2.
When comparing our rates with data from Europe and the United States in different registries of HF, mortality in our hospitals is higher in general. But much of this high mortality is probably due to the greater severity of patients admitted to our service. When comparing the characteristics of hospitalized patients, this greater severity can be observed among Brazilian patients.
For instance, when we compare our data with those of the U.S. ADHERE registry, it can be seen that 74.9% of hospitalized patients in our hospital had systolic BP < 115 mm Hg, whereas in the ADHERE registry only 18.5% were hypotensive9. Low BP is an important prognostic marker in several studies, including the ADHERE registry. An important point to note is that, despite the higher overall mortality rate of our patients, when we analyzed the total number of more severe patients (BUN > 43 mg/dL, BP < 115 mmHg and creatinine > 2.75 mg/dL), mortality did not differ significantly, with our patient population being numerically lower than that of the American study (14.0% vs. 15.3%), suggesting that our treatment, in addition to being adequate, have reduced the mortality a severe group of patients9.
Even regarding hospitals in Brazil, although data are scarce, we observed that mortality in our hospital, despite the greater severity of our cases, was lower than that observed in these other institutions. In Rio de Janeiro, among patients treated at the emergency room of a private institution, the mortality was 10.6% and, in Porto Alegre, a teaching hospital like ours, it was 11%13,14. These differences in mortality are probably due to selection criteria for admission and the period of data collection, but the numbers are very similar to ours.
More significant, however, was the reduction in mortality at the follow-up. We observed a reduction in mortality in the first year of follow up, going from more than 50% to the current 23.6%, a relative reduction of approximately 50%. This result was similar to that observed in Spain, where mortality in the 1991-1996 period was 24%, decreasing to 16% in 2000 and 200115. Improved prognosis was also reported in Baltimore and Sweden, and in these studies, the authors reported that this improvement occurred after the establishment of treatment with ACEI and beta-blockers, but did not specifically analyze the role of their prescriptions, different from our study16,17.
The year 2000 can be considered a watershed for the treatment of chronic HF, as in 1999, two important studies were published on beta blockers in HF, the MERIT-HF and the CIBIS-II study, which reinforced the indication of beta-blockers for treatment of chronic HF18,19. We observed this increase in the prescription in our hospital as, until 2000, at the outpatient clinic, the prescription of beta-blockers reached about 10% of patients, increasing 70% in the 2004 assessment20. This increased prescription of beta-blockers unquestionably played a key role in improving the prognosis of HF in our hospital.
At the univariate analysis of predictors of mortality, it can be observed that the prescription of ACEI and beta-blockers was associated with improved prognosis. Markers of increased cardiac and systemic involvement, usually identified in studies evaluating prognosis (renal and ventricular function) were associated with a worse prognosis, as well as Chagas etiology. In the multivariate analysis, ACEI and beta blockers persisted as markers, with the latter having a greater impact.
In addition to the recording of the neurohormonal blockade value promoting increased survival, this study also shows that Chagas disease was accompanied by worse prognosis, confirming the findings of other Brazilian studies21,22.
Study limitations
Although the analyzed groups (before and after 2000) are not homogeneous (Table 2) due to the nature of this study (observational and retrospective), it is noteworthy the fact that, although patients in the group after 2000 were more severe (older mean age, lower LVEF and lower mean SBP), this group - the most severe - was precisely the one that had the best clinical outcomes at follow-up with lower mortality and lower rates of re-hospitalization. One must consider that these results are observational and that other factors such as improved treatment adherence and cointerventions (e.g., cardiac surgery and interventional procedures), after discharge, were not quantified and may have influenced the improvement in prognosis, in addition to the higher rate of prescription of neurohormonal blockers, particularly beta-blockers. It should be noted that a possible selection bias was the fact that we performed analyses of survival in little more than 50% of the study patients, of which data regarding therapy used was available. Moreover, regarding therapy, we performed the qualitative analysis, while the quantitative analysis of the dose at discharge and at follow-up would be important to evaluate the influence of optimized dose of these medications on patients' prognosis. However, these issues could be addressed in future studies.
Conclusion
This study provided some evidence that, in the real world, the survival of patients with heart failure has increased and that treatment optimization with neurohormonal blockers have had an important role in improving prognosis.
Footnotes
Author contributions
Conception and design of the research, Analysis and interpretation of the data and Critical revision of the manuscript for intellectual content: Del Carlo CH, Cardoso JN, Ochia ME, Oliveira Jr. MT, Ramires JAF, Pereira-Barretto AC; Acquisition of data: Del Carlo CH, Cardoso JN, Ochia ME, Oliveira Jr. MT; Statistical analysis: Del Carlo CH; Writing of the manuscript: Del Carlo CH, Ramires JAF, Pereira-Barretto AC.
Sources of Funding
There were no external funding sources for this study.
Study Association
This study is not associated with any post-graduation program.
References
- 1.Cleland JG, Khand A, Clark A. The heart failure epidemic: exactly how big is it? Eur Heart J. 2001;22(8):623–626. doi: 10.1053/euhj.2000.2493. [DOI] [PubMed] [Google Scholar]
- 2.Pereira-Barretto AC, Del Carlo CH, Cardoso JN, Morgado PC, Munhoz RT, Eid MO, et al. Re-hospitalizações e morte por insuficiência cardíaca: índices ainda alarmantes. Arq Bras Cardiol. 2008;91(5):335–341. doi: 10.1590/s0066-782x2008001700009. [DOI] [PubMed] [Google Scholar]
- 3.McMurray JJ, Stewart S. The burden of heart failure. Eur Heart J. 2002;4(Suppl D):50–58. [Google Scholar]
- 4.Fonarow GC, Heywood T, Heidenreich PA, Lopatin M, Yancy CW. Temporal trends in clinical characteristics, treatments, and outcomes for heart failure hospitalizations, 2002 to 2004: findings from acute decompensated Heart Failure National Registry (ADHERE) Am Heart J. 2007;153(6):1021–1028. doi: 10.1016/j.ahj.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 5.Veloso LG, de Oliveira MT Jr, Munhoz RT, Morgado PC, Ramires JA, Barretto AC. Repercussão nutricional na insuficiência cardíaca avançada e seu valor na avaliação prognóstica. Arq Bras Cardiol. 2005;84(6):480–485. doi: 10.1590/s0066-782x2005000600009. [DOI] [PubMed] [Google Scholar]
- 6.de Oliveira MT Jr, Canesin MF, Munhoz RT, Del Carlo CH, Scipioni AR, Ramires JA. Principais características clínicas de pacientes que sobrevivem 24 meses ou mais após uma hospitalização devido a descompensação cardíaca. Arq Bras Cardiol. 2005;84(2):161–166. [PubMed] [Google Scholar]
- 7.Canesin MF, Giorgi D, Oliveira MT, Jr, Wajngarten M, Mansur A, Ramires JA, et al. Ambulatory blood pressure monitoring of patients with heart failure: a new prognosis marker. Arq Bras Cardiol. 2002;78(1):83–89. doi: 10.1590/s0066-782x2002000100007. [DOI] [PubMed] [Google Scholar]
- 8.Del Carlo CH, Pereira-Barretto AC, Cassaro-Strunz C, Latorre Mdo R, Ramires JA. Serial measure of cardiac troponin T levels for prediction of clinical events in decompensated heart failure. J Card Fail. 2004;10(1):43–48. doi: 10.1016/s1071-9164(03)00594-3. [DOI] [PubMed] [Google Scholar]
- 9.Fonarow GC, Adams KJ, Jr, Abraham WT, Yancy CW, Boscardin WJ, ADHERE Scientific advisory committee.study group and investigators Risk stratification for in-hospital mortality in acutely decompensated heart failure: classification and regression tree analysis. JAMA. 2005;293(5):572–580. doi: 10.1001/jama.293.5.572. [DOI] [PubMed] [Google Scholar]
- 10.Bocchi EA, Marcondes-Braga FG, Ayub-Ferreira SM, Rohde LE, Oliveira WA, Almeida DR, et al. Sociedade Brasileira de Cardiologia III Diretriz brasileira de insuficiência cardíaca crônica. Arq Bras Cardiol. 2009;93(1) supl.1:1–71. [PubMed] [Google Scholar]
- 11.Bocchi EA, Marcondes-Braga FG, Bacal F, Ferraz AS, Albuquerque D, Rodrigues D, et al. Sociedade Brasileira de Cardiologia Atualização da Diretriz Brasileira de Insuficiência Cardíaca Crônica - 2012. Arq Bras Cardiol. 2012;98(1) supl. 1:1–33. doi: 10.1590/s0066-782x2012001000001. [DOI] [PubMed] [Google Scholar]
- 12.Lima MV, Cardoso JN, Ochiai ME, Grativol KM, Grativol OS, Brancalhão EC, et al. É necessário suspender o betabloqueador na insuficiência cardíaca descompensada com baixo débito. Arq Bras Cardiol. 2010;95(4):530–535. doi: 10.1590/s0066-782x2010005000108. [DOI] [PubMed] [Google Scholar]
- 13.VillaCorta H, Mesquita ET, Cardoso R, Bonates T, Maia ER, Silva AC, et al. Preditores de sobrevida obtidos na unidade de emergência em pacientes atendidos por insuficiência cardíaca descompensada. Rev Port Cardiol. 2003;22(4):495–507. [PubMed] [Google Scholar]
- 14.Rohde LE, Clausell N, Ribeiro JP, Goldraich L, Netto R, William Dec GW, et al. Heath outcomes in decompensated congestive heart failure: a comparison of tertiary hospitals in Brazil and United States. Int J Cardiol. 2005;102(1):71–77. doi: 10.1016/j.ijcard.2004.04.006. [DOI] [PubMed] [Google Scholar]
- 15.Grigorian Shamagian L, Gonzalez-Juanatey JR, Roman AV, Acuna JM, Lamela AV. The death rate among hospitalized heart failure patients with normal and depressed left ventricular ejection fraction in the year following discharge: evolution over a 10-year period. Eur Heart J. 2005;26(21):2251–2258. doi: 10.1093/eurheartj/ehi383. [DOI] [PubMed] [Google Scholar]
- 16.Feinglass J, Martin GJ, Lin E, Johnson MR, Gheorghiade M. Is heart failure survival improving? Evidence from 2323 elederly patients hospitalized between 1989-2000. Am Heart J. 2003;146(1):111–114. doi: 10.1016/S0002-8703(03)00116-9. [DOI] [PubMed] [Google Scholar]
- 17.Schaufelberger M, Swedberg K, Koster M, Rosen M, Rosengren A. Decreasing one-year mortality and hospitalization rates for heart failure in Sweden. Data from Swedish Hospital discharge Registry 1988 to 2000. Eur Heart J. 2004;25(4):300–307. doi: 10.1016/j.ehj.2003.12.012. [DOI] [PubMed] [Google Scholar]
- 18.The cardiac insufficiency bisoprolol study II (CIBIS-II): a randomized trial. Lancet. 1999;353(9146):9–13. [PubMed] [Google Scholar]
- 19.Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomized Intervention Trial in Congestive Heart Failure (MERIT-HF) Lancet. 1999;353(9169):2001–2007. [PubMed] [Google Scholar]
- 20.Pereira-Barretto AC. Nobre F, Serrano CV., Jr . Tratado de cardiologia SOCESP. Barueri (São Paulo): Editora Manole; 2009. Tratamento da insuficiência cardíaca crônica; pp. 1065–1074. [Google Scholar]
- 21.Freitas HG, Chizzola PR, Paes AT, Lima AC, Mansur AJ. Risk stratification in a Brazilian hospital-based cohort of 1220 outpatients with heart failure: role of Chagas' disease. Int J Cardiol. 2005;102(2):239–247. doi: 10.1016/j.ijcard.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 22.Silva CP, Del Carlo CH, Oliveira MT, Jr, Scipioni A, Strunz-Cassaro C, Ramires JAF, et al. Porque o portadores de cardiomiopatia chagásica têm pior evolução que os não chagásicos? Arq Bras Cardiol. 2008;91(6):389–394. [Google Scholar]