Abstract
Introduction
Sacral insufficiency fractures are an important cause of lower back pain in the elderly. Clinically and radiologically, they must be distinguished from osseous metastases, which frequently coexist. To date, no case report has comprehensively explored the full range of diagnostic hurdles and potential pitfalls.
Case presentation
We report the case of a 70-year-old Caucasian female who presented to our services with a short history of progressive back pain without any history of trauma. A prior history of breast cancer was noted. Bone scintigraphy was initially reported as consistent with metastatic sacral deposits. Further characterization with magnetic resonance imaging and computed tomography revealed bilateral insufficiency fractures of the sacral alar. The patient responded well to conservative management.
Conclusion
To avoid misdiagnosis, particularly in those who are also at risk of osseous metastases, sacral insufficiency fractures must always be considered as a cause of lower back pain.
Keywords: sacral fractures, insufficiency fractures, misdiagnosis, metastatic disease
Introduction
Stress fractures can be classified as either fatigue or insufficiency fractures.1 Intuitively, the first describes fractures occurring within normal bone architecture that has been exposed to abnormal or repetitive stresses.2 Conversely, insufficiency fractures occur in abnormal bone under normal stress. Insufficiency fractures of the sacrum (SIFs) were first described by Lourie in 1982.3 Patients undergoing radiotherapy to treat malignant tumors may be at particular risk of SIFs,4 with a prevalence of 89% for patients undergoing radiotherapy for cervical cancer.5 Elderly women with osteoporosis are also at high risk,6 with almost all patients with SIFs demonstrating severe osteopenia on dual X-ray absorptiometry.7 Additionally, rheumatoid arthritis, Paget’s disease, renal osteodystrophy, and hyperparathyroidism have been reported as risk factors.8,9 Sacral stress fractures have occasionally been reported during the last trimester of pregnancy and the early postpartum period.10,11 While preceding trauma may be reported, it is usually minor12 or often completely absent.13
Patients suffering from SIFs often present with limited mobility caused by acute and intractable lumbar or pelvic pain without clear evidence of trauma. Neurological symptoms are usually absent, but radiculopathy has a reported incidence of 5%–6%7 and sphincter disturbance has also been described.14 Pain typically improves on lying supine and increases on weight-bearing. Patients may also complain of parasymphyseal discomfort due to the high incidence of concomitant pubic rami fractures.15
The lack of specific clinical findings makes diagnosis challenging and SIFs remain an under-recognized cause of lower back pain. In fact, there is often a delay of up to 2 months before dedicated sacral imaging is performed.16 In this report, we describe the diagnostic challenge of detecting SIFs and aim to increase awareness of the potential pitfalls.
Case presentation
A 70-year-old Caucasian patient was admitted through the emergency department with severe back pain. She had first experienced discomfort 14 days previously, which had progressively worsened. No history of trauma, however minor, could be recalled. The pain was localized to her lower back with no radicular symptoms. One week after the initial discomfort, the patient was unable to mobilize and had become bedridden. No neurology was demonstrable on examination. Palpation of the lumbar vertebrae was unremarkable but direct pressure over both sacroiliac joints resulted in a marked exacerbation of her pain.
A history of primary breast cancer was reported. The disease was detected during mammographic screening with no radiographic or histological evidence of distant metastasis. As such, the patient had undergone a wide local excision and local radiotherapy 4 years prior. Additionally, she described a longstanding history of rheumatoid arthritis which was controlled with disease-modifying antirheumatic drugs.
Upon admission, our patient was apyrexial and had a normal white blood cell count. Interestingly, raised alkaline phosphatase (ALP) was found at 278 IU/L (reference range: 30–130 IU/L) with normal adjusted calcium. The remaining liver function tests were normal. Marginally raised C-reactive protein was seen at 15 mg/L (reference range: <10 mg/L).
Plain film radiographs of her lumbar spine demonstrated scoliosis but no fractures or suspicious lesions. Similarly, radiographs of her pelvis did not detect any abnormalities. In view of her medical history, bone scintigraphy was performed. This demonstrated a bilateral increase in uptake of technetium-99m in the sacrum and pubic rami (Figure 1). Initially, this was thought to be consistent with metastatic disease. Subsequently, spinal magnetic resonance imaging (MRI) was performed to characterize the extent of the lesions. T1-weighted images of the sacrum demonstrated symmetrical hypointense areas within both sacral alar (Figure 2). Whilst symmetry was not in keeping with a neoplastic process, no fracture line was evident. A computed tomography (CT) scan of the sacral region highlighted bilateral fracture lines through the sacral alar in keeping with insufficiency fractures (Figure 3). CT also demonstrated a right-sided anterior pubic rami fracture.
Figure 1.
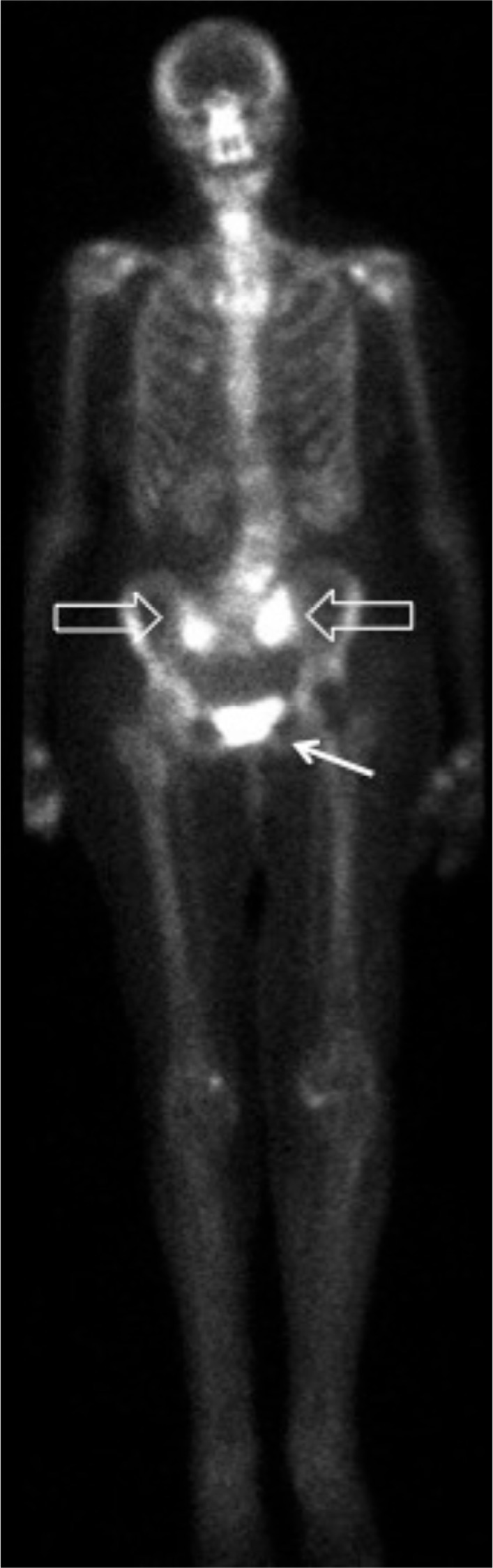
Bone scintigraphy showing increased sacral uptake bilaterally (hollow arrows) and pubic bone (solid arrow).
Figure 2.
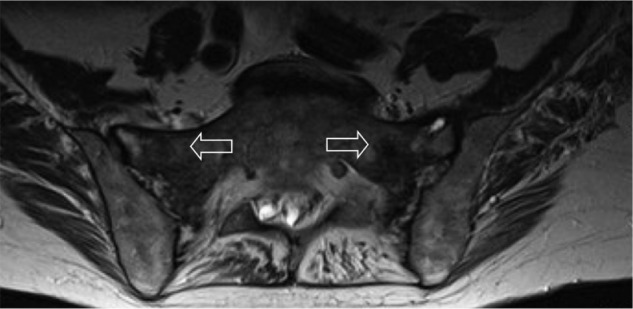
Axial T1-weighted MRI image of sacrum.
Note: Patchy, low-intensity edema evident (arrows).
Abbreviation: MRI, magnetic resonance imaging.
Figure 3.
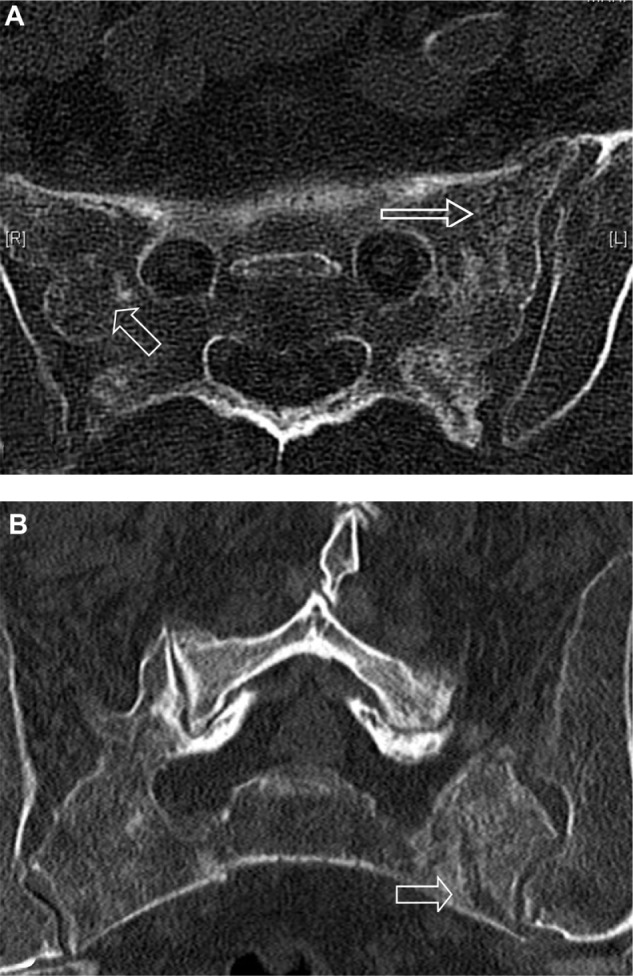
CT images of sacrum.
Notes: (A) axial and (B) sagittal views demonstrating cortical breaks with mottled sclerosis/lucency (arrows).
Abbreviation: CT, computed tomography.
Her pain was successfully managed with a combination of simple and transcutaneous opioid analgesia. The patient was able to mobilize with the aid of a walking frame and was discharged home on day 12 of admission. Subsequent follow-up at 1 month found her pain, mobility, and independence to be gradually improving.
Discussion
Several reports have previously highlighted the variable and nonspecific presentation of SIFs that makes diagnosis challenging.6,9 Whilst not specific for SIFs, Denis et al have classified traumatic sacral fractures into zones,17 which can help predict the clinical features. Zone 1 fractures lie laterally, involving the sacral alar, with zones 2 and 3 fractures progressing medially to involve the neural foramina and sacral bodies, respectively. Consequently, unilateral radicular symptoms are often reported with zone 2 fractures and bilateral neurological symptoms with sphincter dysfunction can occur with involvement of zone 3.
Laboratory investigations are of limited value. Often, no abnormality is found, although a mildly raised ALP, a marker of bone formation, is sometimes seen.18 Of note, ALP is also raised in metastatic disease.19 Radiographs of the pelvis, sacrum, and lumbar spine may initially be used to identify fractures. However, the presence of fecal material, vascular calcifications, and bowel gas can mask incomplete fractures, and radiographs detect SIFs in less than 40% of cases.20
Diagnostic difficulty is compounded by a history of malignancy in approximately 45% of patients with SIFs.21 Consideration of this clinical entity is therefore paramount if overdiagnosis of osseous metastasis is to be avoided. Bone scintigraphy with technetium-99m-labeled medronic acid is one of the most sensitive (96%) examinations.22 While present in less than 40% of patients, the H-sign is considered pathognomonic for SIFs.23 However, isolated sacral metastases presenting with focal sacral uptake have also been reported.24
MRI, with sensitivity approaching 100%, is considered to be the gold standard for identifying SIFs.24 Most cases demonstrate both marrow edema and a fracture line, although the latter is absent in 7% of cases.24 The absence of a fracture line can create uncertainty. Although less sensitive (60%–75%),24 CT can be used in combination with MRI. Previous reports have noted that the absence of cortical destruction and/or a soft tissue mass effectively rules out bone metastases (Table 1).25,26
Table 1.
Summary of articles published on the imaging modalities utilized for the investigation of SIFs
| Author | Study type | Number of patients | Imaging method | Findings |
|---|---|---|---|---|
| Gotis-Graham et al7 | CS/MA | 110 | Plain films | Images reviewed retrospectively. Vertical bands of sclerosis (50%) or fracture lines (11%) present. |
| Schneider et al38 | CS | 23 | Nuclear medicine | Described three patterns of radionuclide uptake. H-shaped was the most common (78%). Other patterns include, uptake in a single alar (13%) or a T-shaped uptake, involving the sacral body and only one alar (9%). |
| Finiels et al13 | MA | 508 | H-shaped pattern present in only 42% of reported cases. | |
| Fujii et al22 | CS | 26 | Sensitivity of NM for diagnosis of SIFs was 96% and PPV 92%. | |
| Cabarrus et al24 | CS | 64 | MRI | Images reviewed retrospectively. Marrow edema demonstrated in 100% and a fracture line in 94%. |
| Grangier et al16 | CS | 17 | Use of IV gadolinium and/or fat suppression may improve detection of fracture lines. | |
| Byun et al39 | CS | 22 | Diffusion-weighted MRI may help differentiate between marrow edema from fracture or metastasis. | |
| Gotis-Graham et al7 | CS | 12 | CT | Images reviewed retrospectively. Fracture lines (42%) or sclerosis (17%) present. |
| Cabarrus et al24 | CS | 64 | Images reviewed retrospectively. Fractures detected in 75% of proven SIFs. |
Abbreviations: CS, case series; CT, computed tomography; IV, intravenous; MA, meta-analysis; MRI, magnetic resonance imaging; NM, nuclear medicine; PPV, positive predictive value; SIFs, sacral insufficiency fractures.
Traditionally, treatment of SIFs has been limited to conservative management strategies comprising bed rest, pain control, and physical therapy, with symptoms usually improving within 12 months.27,28 However, prolonged bed rest, particularly in elderly patients, has a significant morbidity. In particular, high incidences of deep vein thrombosis and pulmonary embolism have been reported.29 Early physical therapy has been advocated as a means of reducing this morbidity and encouraging fracture healing through the promotion of osteoblast-mediated bone formation.30 However, good quality prospective trials supporting early physical therapy in SIFs are currently lacking.
Sacroplasty has also emerged as a potential treatment and involves fluoroscopic or CT-guided injection of cement into the fractured sacrum. Initially used as a treatment for sacral metastases, it was first described as a treatment for SIFs in 2002 by Garant.31 As yet, no randomized trials are available, and the literature is restricted to small retrospective case series with variable, and often invalidated, outcome measures. Whilst these need to be interpreted cautiously, they suggest a rapid and sustained improvement in pain, reduced use of narcotic analgesia, and improvement in mobility scores.32,33 In addition, an improved ability to perform activities of daily living has also been reported.34 The main risk of sacroplasty is leakage of cement outside of the fracture line, with risk of neurological compromise. Leakage of cement has been reported but in only one case did this result in transient radiculopathy,32 and in none were long-term sequelae described.33 As a means of reducing complications, augmentation with a balloon-assisted technique, sacral kyphoplasty, has been proposed.35 The creation of a compacted bony layer outside the balloon could, in theory, reduce cement extravasation. Supporting this technique, a cadaveric study demonstrated that cement deposition was better localized within the cortical boundaries.36
Clearly, stronger evidence is required before the widespread use of sacroplasty over conservative management can be supported. It has also been suggested that since sacroplasty disrupts normal osseous healing, it may only be indicated in patients with delayed union or pain not responding to conservative measures.37 However, the best method of conservative management remains equally uncertain. This is an area of much needed research (Table 2).
Table 2.
A selection of previously reported case series on the various treatments of SIFs
| Authors | Study type | Number of patients | Treatment | Outcome |
|---|---|---|---|---|
| Aretxabala et al15 | CS | 9 | Bed rest + analgesia | Mean recovery time of 3.3 months. |
| Weber et al28 | CS | 20 | Analgesia and early physical therapy | 100% of patients pain-free at 9 weeks. |
| Leroux et al40 | CS | 10 | Bed rest + analgesia | Mean time to symptomatic improvement of 4 weeks. |
| Gotis-Graham et al7 | CS | 20 | Analgesia ± bed rest | 85% reported complete resolution of pain and return to independence at 9 months. |
| Brook et al41 | CS | 2 | CT-guided sacroplasty | Improvement in pre-procedure VAS. Improvement sustained at 8–16 months. |
| Frey et al32 | CS | 52 | CT-guided sacroplasty | Improvement in pre-procedure VAS. Improvement sustained at 1 year. |
| Strub et al42 | CS | 13 | CT-guided sacroplasty | Improvement in pre-procedure pain. Improvement sustained at 15 months. |
Abbreviations: CS, case series; CT, computed tomography; SIFs, sacral insufficiency fractures; VAS, visual analog scale.
Conclusion
The diagnostic difficulty of SIFs has previously been recognized. To our knowledge, this is the first report to highlight the full range of diagnostic hurdles; in particular, we draw attention to the limitations of each imaging modality. Awareness of SIFs is important if an erroneous misinterpretation for metastatic disease is to be avoided.
Consent
Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images. A copy of the written consent is available for review from the Editor-in-Chief of this journal.
Acknowledgment
With thanks to Sarah Brice for her support and academic input.
Author contributions
All authors contributed toward data analysis, drafting and revising the paper and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Pentecost RL, Murray RA, Brindley HH. Fatigue, insufficiency, and pathologic fractures. JAMA. 1964;187:1001–1004. doi: 10.1001/jama.1964.03060260029006. [DOI] [PubMed] [Google Scholar]
- 2.Pommering TL, Kluchurosky L. Overuse injuries in adolescents. Adolesc Med State Art Rev. 2007;18(1):95–120. ix. [PubMed] [Google Scholar]
- 3.Lourie H. Spontaneous osteoporotic fracture of the sacrum. An unrecognized syndrome of the elderly. JAMA. 1982;248(6):715–717. [PubMed] [Google Scholar]
- 4.Mammone JF, Schweitzer ME. MRI of occult sacral insufficiency fractures following radiotherapy. Skeletal Radiol. 1995;24(2):101–104. doi: 10.1007/BF00198070. [DOI] [PubMed] [Google Scholar]
- 5.Blomlie V, Rofstad E, Talle K, Sundfør K, Winderen M, Lien HH. Incidence of radiation-induced insufficiency fractures of the female pelvis: evaluation with MR imaging. AJR Am J Roentgenol. 1996;167(5):1205–1210. doi: 10.2214/ajr.167.5.8911181. [DOI] [PubMed] [Google Scholar]
- 6.Wild A, Jaeger M, Haak H, Mehdian SH. Sacral insufficiency fracture, an unsuspected cause of low back pain in elderly women. Arch Orthop Trauma Surg. 2002;122(1):58–60. doi: 10.1007/s004020100333. [DOI] [PubMed] [Google Scholar]
- 7.Gotis-Graham I, McGuigan L, Diamond T, et al. Sacral insufficiency fractures in the elderly. J Bone Joint Surg Br. 1994;76(6):882–886. [PubMed] [Google Scholar]
- 8.De Smet AA, Neff JR. Pubic and sacral insufficiency fractures: clinical course and radiologic findings. AJR Am J Roentgenol. 1985;145(3):601–606. doi: 10.2214/ajr.145.3.601. [DOI] [PubMed] [Google Scholar]
- 9.Dasgupta B, Shah N, Brown H, Gordon TE, Tanqueray AB, Mellor JA. Sacral insufficiency fractures: an unsuspected cause of low back pain. Br J Rheumatol. 1998;37(7):789–793. doi: 10.1093/rheumatology/37.7.789. [DOI] [PubMed] [Google Scholar]
- 10.Rousière M, Kahan A, Job-Deslandre C. Postpartal sacral fracture without osteoporosis. Joint Bone Spine. 2001;68(1):71–73. doi: 10.1016/s1297-319x(01)00262-7. [DOI] [PubMed] [Google Scholar]
- 11.Schmid L, Pfirrmann C, Hess T, Schlumpf U. Bilateral fracture of the sacrum associated with pregnancy: a case report. Osteoporos Int. 1999;10(1):91–93. doi: 10.1007/s001980050200. [DOI] [PubMed] [Google Scholar]
- 12.Newhouse KE, el-Khoury GY, Buckwalter JA. Occult sacral fractures in osteopenic patients. J Bone Joint Surg Am. 1992;74(10):1472–1477. [PubMed] [Google Scholar]
- 13.Finiels H, Finiels PJ, Jacquot JM, Strubel D. Fractures du sacrum par insuffisance osseuse: meta-analyse de 508 cas [Fractures of the sacrum caused by bone insufficiency: meta-analysis of 508 cases] La Presse Medicale. 1997;26(33):1568–1573. French. [PubMed] [Google Scholar]
- 14.Muthukumar T, Butt SH, Cassar-Pullicino VN, McCall IW. Cauda equina syndrome presentation of sacral insufficiency fractures. Skeletal Radiol. 2007;36(4):309–313. doi: 10.1007/s00256-006-0239-5. [DOI] [PubMed] [Google Scholar]
- 15.Aretxabala I, Fraiz E, Pérez-Ruiz F, Ríos G, Calabozo M, Alonso-Ruiz A. Sacral insufficiency fractures. High association with pubic rami fractures. Clin Rheumatol. 2000;19(5):399–401. doi: 10.1007/pl00011178. [DOI] [PubMed] [Google Scholar]
- 16.Grangier C, Garcia J, Howarth NR, May M, Rossier P. Role of MRI in the diagnosis of insufficiency fractures of the sacrum and acetabular roof. Skeletal Radiol. 1997;26(9):517–524. doi: 10.1007/s002560050278. [DOI] [PubMed] [Google Scholar]
- 17.Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res. 1988;227:67–81. [PubMed] [Google Scholar]
- 18.Schindler OS, Watura R, Cobby M. Sacral insufficiency fracture: an under-recognized condition. Curr Orthopaed. 2003;17(3):234–239. [Google Scholar]
- 19.Mayne PD, Thakrar S, Rosalki SB, Foo AY, Parbhoo S. Identification of bone and liver metastasis from breast cancer by measurement of plasma alkaline phosphatase isoenzyme activity. J Clin Pathol. 1987;40(4):398–403. doi: 10.1136/jcp.40.4.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Peh WC, Khong PL, Sham JS, Ho WY, Yeung HW. Sacral and pubic insufficiency fractures after irradiation of gynaecological malignancies. Clin Oncol (R Coll Radiol) 1995;7(2):117–122. doi: 10.1016/s0936-6555(05)80814-3. [DOI] [PubMed] [Google Scholar]
- 21.Lundin B, Björkholm E, Lundell M, Jacobsson H. Insufficiency fractures of the sacrum after radiotherapy for gynaecological malignancy. Acta Oncol. 1990;29(2):211–215. doi: 10.3109/02841869009126547. [DOI] [PubMed] [Google Scholar]
- 22.Fujii M, Abe K, Hayashi K, et al. Honda sign and variants in patients suspected of having a sacral insufficiency fracture. Clin Nucl Med. 2005;30(3):165–169. doi: 10.1097/00003072-200503000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Ries T. Detection of osteoporotic sacral fractures with radionuclides. Radiology. 1983;146(3):783–785. doi: 10.1148/radiology.146.3.6828693. [DOI] [PubMed] [Google Scholar]
- 24.Cabarrus MC, Ambekar A, Lu Y, Link TM. MRI and CT of insufficiency fractures of the pelvis and the proximal femur. AJR Am J Roentgenol. 2008;191(4):995–1001. doi: 10.2214/AJR.07.3714. [DOI] [PubMed] [Google Scholar]
- 25.Gacetta DJ, Yandow DR. Computed tomography of spontaneous osteoporotic sacral fractures. J Comput Assist Tomogr. 1984;8(6):1190–1191. doi: 10.1097/00004728-198412000-00032. [DOI] [PubMed] [Google Scholar]
- 26.Tsuchida T, Kosaka N, Sugimoto K, Itoh H. Sacral insufficiency fracture detected by FDG-PET/CT: report of 2 cases. Ann Nucl Med. 2006;20(6):445–448. doi: 10.1007/BF03027382. [DOI] [PubMed] [Google Scholar]
- 27.Rawlings CE, 3rd, Wilkins RH, Martinez S, Wilkinson RH., Jr Osteoporotic sacral fractures: a clinical study. Neurosurgery. 1988;22(1 Pt 1):72–76. doi: 10.1227/00006123-198801010-00011. [DOI] [PubMed] [Google Scholar]
- 28.Weber M, Hasler P, Gerber H. Insufficiency fractures of the sacrum. Twenty cases and review of the literature. Spine (Phila Pa 1976) 1993;18(16):2507–2512. doi: 10.1097/00007632-199312000-00021. [DOI] [PubMed] [Google Scholar]
- 29.Babayev M, Lachmann E, Nagler W. The controversy surrounding sacral insufficiency fractures: to ambulate or not to ambulate? Am J Phys Med Rehabil. 2000;79(4):404–409. doi: 10.1097/00002060-200007000-00014. [DOI] [PubMed] [Google Scholar]
- 30.Chao EY, Inoue N, Koo TK, Kim YH. Biomechanical considerations of fracture treatment and bone quality maintenance in elderly patients and patients with osteoporosis. Clin Orthop Relat Res. 2004;(425):12–25. doi: 10.1097/01.blo.0000132263.14046.0c. [DOI] [PubMed] [Google Scholar]
- 31.Garant M. Sacroplasty: a new treatment for sacral insufficiency fracture. J Vasc Interv Radiol. 2002;13(12):1265–1267. doi: 10.1016/s1051-0443(07)61976-9. [DOI] [PubMed] [Google Scholar]
- 32.Frey ME, Depalma MJ, Cifu DX, Bhagia SM, Carne W, Daitch JS. Percutaneous sacroplasty for osteoporotic sacral insufficiency fractures: a prospective, multicenter, observational pilot study. Spine J. 2008;8(2):367–373. doi: 10.1016/j.spinee.2007.05.011. [DOI] [PubMed] [Google Scholar]
- 33.Bayley E, Srinivas S, Boszczyk BM. Clinical outcomes of sacroplasty in sacral insufficiency fractures: a review of the literature. Eur Spine J. Sep. 2009;18(9):1266–1271. doi: 10.1007/s00586-009-1048-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Whitlow CT, Mussat-Whitlow BJ, Mattern CW, Baker MD, Morris PP. Sacroplasty versus vertebroplasty: comparable clinical outcomes for the treatment of fracture-related pain. AJNR Am J Neuroradiol. 2007;28(7):1266–1270. doi: 10.3174/ajnr.A0561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Deen HG, Nottmeier EW. Balloon kyphoplasty for treatment of sacral insufficiency fractures. Report of three cases. Neurosurg Focus. 2005;18(3):e7. [PubMed] [Google Scholar]
- 36.Betts A. Sacral vertebral augmentation: confirmation of fluoroscopic landmarks by open dissection. Pain Physician. 2008;11(1):57–65. [PubMed] [Google Scholar]
- 37.Ehara S. Percutaneous sacroplasty for osteoporotic insufficiency fractures. AJR Am J Roentgenol. 2006;186(2):580. doi: 10.2214/AJR.06.5009. author reply 580–581. [DOI] [PubMed] [Google Scholar]
- 38.Schneider R, Yacovone J, Ghelman B. Unsuspected sacral fractures: detection by radionuclide bone scanning. AJR Am J Roentgenol. 1985;144(2):337–341. doi: 10.2214/ajr.144.2.337. [DOI] [PubMed] [Google Scholar]
- 39.Byun WM, Jang HW, Kim SW, Jang SH, Ahn SH, Ahn MW. Diffusion-weighted magnetic resonance imaging of sacral insufficiency fractures: comparison with metastases of the sacrum. Spine (Phila Pa 1976) 2007;32(26):E820–E824. doi: 10.1097/BRS.0b013e31815ce70c. [DOI] [PubMed] [Google Scholar]
- 40.Leroux JL, Denat B, Thomas E, Blotman F, Bonnel F. Sacral insufficiency fractures presenting as acute low-back pain. Biomechanical aspects. Spine (Phila Pa 1976) 1993;18(16):2502–2506. doi: 10.1097/00007632-199312000-00020. [DOI] [PubMed] [Google Scholar]
- 41.Brook AL, Mirsky DM, Bello JA. Computerized tomography guided sacroplasty: a practical treatment for sacral insufficiency fracture: case report. Spine (Phila Pa 1976) 2005;30(15):E450–E454. doi: 10.1097/01.brs.0000172182.35619.d1. [DOI] [PubMed] [Google Scholar]
- 42.Strub WM, Hoffmann M, Ernst RJ, Bulas RV. Sacroplasty by CT and fluoroscopic guidance: is the procedure right for your patient? AJNR Am J Neuroradiol. 2007;28(1):38–41. [PMC free article] [PubMed] [Google Scholar]


