Abstract
Background:
While limb salvage surgery has long been established as the standard of care for osteosarcoma, large studies from Indian centers are few. Given the diverse socio economic milieu of our patients, it becomes significant to determine the feasibility and outcome of management of osteosarcoma in our population. We analyzed the early outcome of limb salvage surgery with multimodality treatment of osteosarcoma of the extremity/girdle bones at a tertiary North Indian Cancer Centre.
Materials and Methods:
A total of 51 limb salvage surgeries performed during the months between November 2008 and November 2012 were studied. Neoadjuvant/adjuvant chemotherapy was given by the pediatric/adult medical oncology teams as applicable. The mean followup was 19.45 months (range 2-50 months). The oncological outcome was correlated with age, sex, size of tumor, stage at presentation, site, histological subtype, type of chemotherapy protocol followed and necrosis seen on postoperative examination of resected specimen. The functional outcome of the patients was evaluated using the musculoskeletal tumor society (MSTS) scoring system.
Results:
Out of a total of 37 males and 14 females with an average age of 18.8 years, the 3 year overall survival was 66% and 3 year event free survival was 61.8%. In this group of patients with a short followup, a better oncological outcome was associated with good postoperative tumor necrosis, nonchondroblastic histology and age <14 years. The average MSTS score was highest in patients with proximal or distal femur prosthesis and the lowest in patients undergoing a knee arthrodesis.
Conclusion:
The present study shows oncological and functional outcomes of limb salvage combined with chemotherapy in Indian patients with osteosarcoma comparable to those in world literature. Larger studies on Indian population with longer followup are recommended.
Keywords: Limb salvage surgery, osteosarcoma, oncological outcome, neoadjuvant chemotherapy
INTRODUCTION
Management of osteosarcoma of extremity and girdle bones is challenging.1,2,3,4 Multiagent chemotherapy combined with limb salvage surgery has been established as the standard of care of osteosarcoma world-wide and most studies now report 5 year survival rates of 60-70%, with limb salvage being possible in up to 90% patients at most specialized centers.1
While the developed world has seen advancements in both oncological and functional outcome of osteosarcoma management much earlier, the developing world has lagged behind on these advancements. As far as Indian patients are concerned, single institution studies on contemporary treatment of osteosarcoma have been few.5 The present study was conducted with the aim of analyzing the oncological and functional outcome of osteosarcoma patients undergoing limb salvage surgery at a tertiary cancer center of Northern India.
MATERIALS AND METHODS
One hundred and sixteen patients underwent limb salvage surgery (a limb sparing segmental resection of an extremity or girdle bone for a malignant or benign aggressive tumor) between November 2008 and November 2012 at our institute. Out of these, 51 patients with proven diagnosis of osteosarcoma of girdle or extremity bones who underwent limb salvage surgery in the above period were included in this retrospective study. Clinical charts of all patients were reviewed after obtaining institutional review board approval. The records were analyzed in detail for demographic profile, clinical features, histopathological features, imaging studies, treatment and outcome. The final outcome information was obtained telephonically and by e-mails in 13 patients.
The diagnosis was established on the basis of in house biopsy in 42 patients (core needle biopsy done as an out-patient department procedure under local anesthesia in 38 patients and open biopsy under regional/general anesthesia in four patients) and as a review of outside slides in nine patients. Metastatic work-up included either computed tomography (CT) scan of the chest combined with whole body bone scan or, alternatively, positron emission tomography scan (n=7). Tumor was designated as small or large (tumor size 8 cm or less vs. more than 8 cm) based on postoperative gross histopathological examination. The type of reconstruction was classified as nonbiological (prosthesis/cement spacer), biological (vascular/nonvascular autograft, extra corporeally irradiated tumor bone), or no reconstruction. The megaprostheses used for limb salvage were either ResTOR megaprosthesis (Adler Mediequip Pvt. Ltd., Devrukh, India) or GMRS megaprosthesis (Stryker Orthopedics, Mahwah, USA). Necrosis of tumor postneoadjuvant chemotherapy was graded as good (more than or equal to 90% of tumor) or poor (less than 90% of tumor).6 Two patients with a parosteal osteosarcoma received no chemotherapy while all other patients received neoadjuvant chemotherapy before surgery and adjuvant chemotherapy afterwards. The patients were treated by two different oncology teams (pediatric and adult medical oncology) and received either ifosfamide, Adriamycin and cisplatin (IAP) based (three cycles of neoadjuvant chemotherapy and three cycles of adjuvant chemotherapy) or high dose methotrexate (HDMTX) based [EUROMOS 1 protocol; (methotrexate, adriamycin, cisplatin) in patients with localized disease and good responders and addition of etoposide and ifosfamide in patients with metastatic disease or poor responders] chemotherapy. Twenty eight patients received IAP based chemotherapy (three of them at other institutes) while 21 patients received HDMTX based chemotherapy. Surgery was performed between 2 and 3 weeks after the last cycle of chemotherapy, depending on the fitness for surgery including hematological and biochemical parameters. The same orthopedic oncologist (AT) was involved in all the limb salvage surgeries. Chemotherapy was restarted after 2-3 weeks of surgery if satisfactory wound healing was seen. After completion of treatment, the followup was 3-monthly for the initial 2 years and 6-monthly thereafter. Every followup visit consisted of local examination (clinical evaluation to rule out recurrence of swelling and for functional assessment). Moreover regional examination to rule out lymphadenopathy, CT scan of chest (noncontrast) and local imaging (X-rays routinely, complimented by magnetic resonance imaging/CT/ultrasounds where suspicion of a local relapse was present) were also done. Local or systemic relapse and progression of disease (appearance of new metastatic lesions) were labeled as events. The oncological outcome (overall survival [OS] and event free survival [EFS]) was correlated with age, sex, size of tumor, stage at presentation, site, histological subtype, type of chemotherapy protocol followed and necrosis seen on postoperative examination of resected specimen. The functional outcome of the patients was evaluated using the musculoskeletal tumor society (MSTS) scoring system7 and was correlated with site, type of reconstruction and length of resection. The time taken by patients to rehabilitate (to get back to optimum function of the limb) was also evaluated and was correlated to the type of reconstruction. The patients were also evaluated for early and late postoperative complications. The overall and event-free survivals were evaluated for all patients using the Kaplan Meier curve (SPSS version 16.0).
RESULTS
There were 37 males and 14 females. The mean age was 18.8 years (range 10-38 years). Five patients had metastatic disease (all pulmonary metastases) while all others had localized disease at presentation. The most common site was distal femur (n=18) followed by proximal tibia (n=12). The average followup was 19.45 months (range: 2-50 months, median 15 months). The average MSTS score was highest in patients with a proximal or distal femur prosthesis 26.5 (range 26-27) and 26 (range 24-28) respectively (barring a lone patient with an intercalary resection and extra corporeal radiotherapy (ECRT) and reimplantation of tumor with vascularized fibula, MSTS 28) and the lowest in patients undergoing a knee arthrodesis (average 19.5; range 19-20). The average MSTS score was statistically similar for a nonbiological reconstruction as compared to a biological reconstruction (average 23.6 [range 14-28] and 22.7 [range 19-28] respectively). However, the rehabilitation time (calculated as the time when uninhibited function/full weight bearing was allowed) was significantly higher (P = 0.00) in patients having a biological reconstruction.
On survival analysis, the 3 year OS was 66% and 3 year EFS was 61.8% [Figures 1 and 2]. While OS was significantly worse with chondroblastic histologic subtype (P = 0.04), EFS was significantly better in the age group <14 years (P = 0.05) and patients with good necrosis on postoperative analysis (P = 0.05). The average duration of surgery was highest for those undergoing vascularized fibula graft (4 patients, 8.25 h) followed by pelvic osteosarcomas (2 patients, 5.6 h). The average resection length was 17.44 cm (range 8.7-34 cm) and the average blood loss was 547 ml (range 80-1800 ml, average 1800 ml for pelvic osteosarcomas). All patients had a microscopically negative margin except one. The patient with a microscopically positive margin had a parosteal osteosarcoma and developed a local recurrence 1 year later and underwent amputation. He remains disease free at a followup of 37 months.
Figure 1.
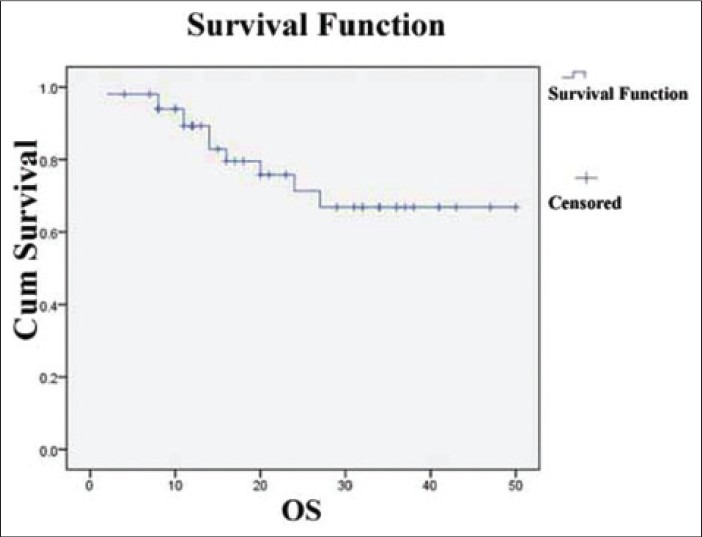
A Kaplan Meier survival curve showing overall survival
Figure 2.
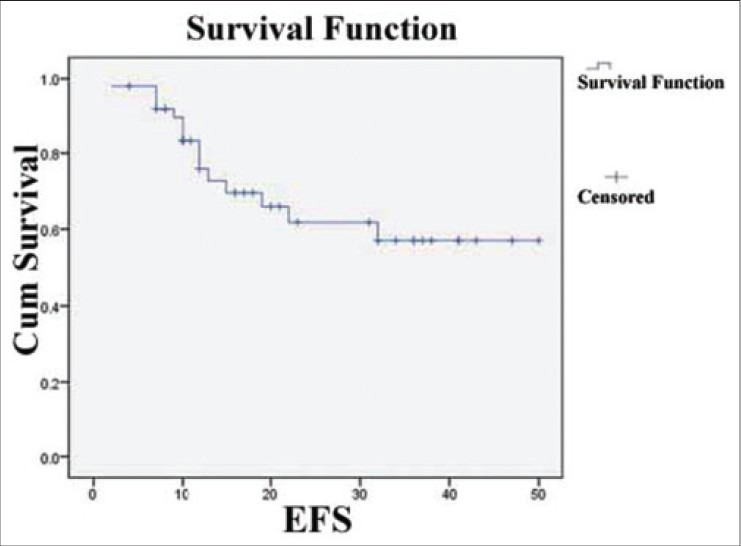
A Kaplan Meier survival curve showing event free survival
Thirty five patients underwent a nonbiological reconstruction [Figure 3], 12 patients had biological reconstruction [Figures 4-6], whereas four patients required no reconstruction [Table 1]. A total of 22 complications were seen in 20 patients [Table 2], seven of which were minor and required conservative management only. Three limbs had to be amputated (one for infection and two for local recurrence, including one patient with parosteal osteosarcoma), while two more patients with a local recurrence refused amputation. The average number of repeat surgeries (for nononcological, reconstruction related indications, barring primary surgery) undergone by patients was 0.14/patient for nonbiological reconstructions, none for no reconstructions and 0.6/patient for biological reconstructions.
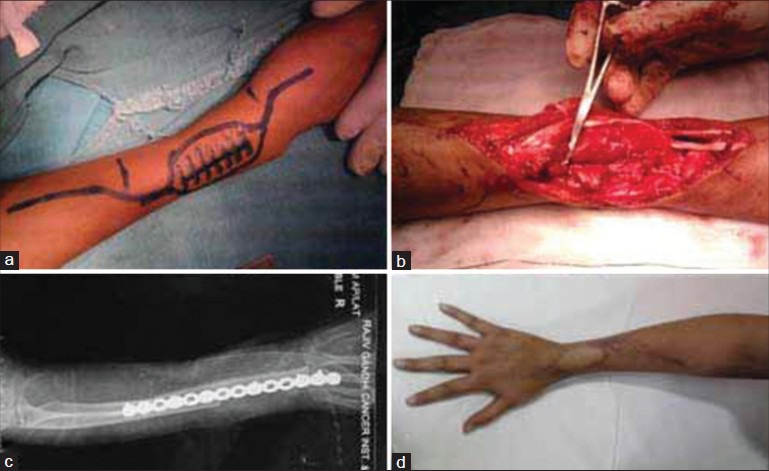
Figure 3A.

X-ray anteroposterior and lateral views (a) and coronal MRI T2W (b) and T1W (c) (preoperative imaging) showing osteosarcoma distal femur
Figure 4.
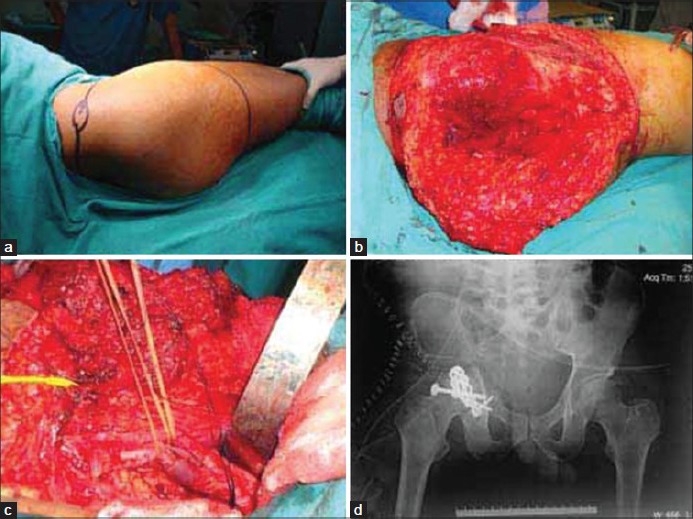
Biological reconstruction (a) clinical photograph showing markings of skin incision in a case of osteosarcoma of pelvis (b and c) peroperative photographs showing internal hemipelvectomy type I + II (d) x-ray pelvis with both hip joints anteroposterior view showing hip arthrodesis
Figure 6.
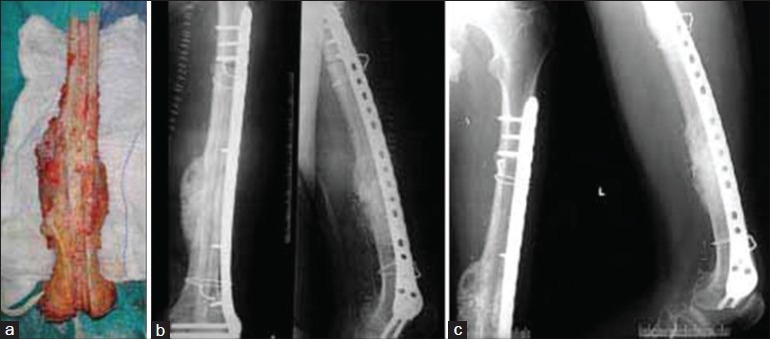
Biological reconstruction using extra corporeally irradiated, osteosarcoma femur shaft a) resected intercalary segment of femoral shaft after extracorporeal irradiation. (b) Anteroposterior and lateral posteoperative x rays showing implant in situ holding extracorporeally irradiated bone to proximal and distal cut ends (c) followup x-ray showing union
Table 1.
Methods of reconstruction
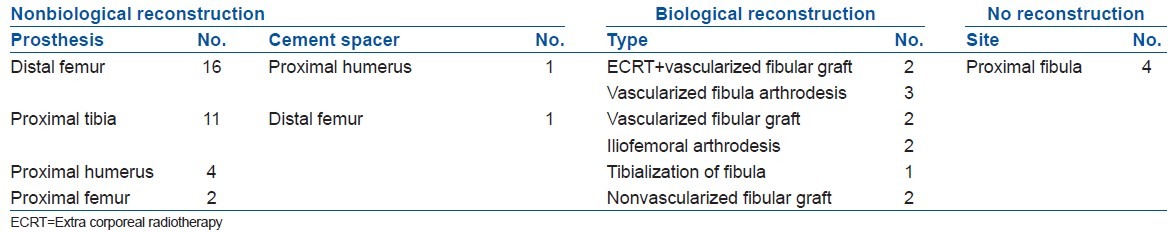
Table 2.
Complications
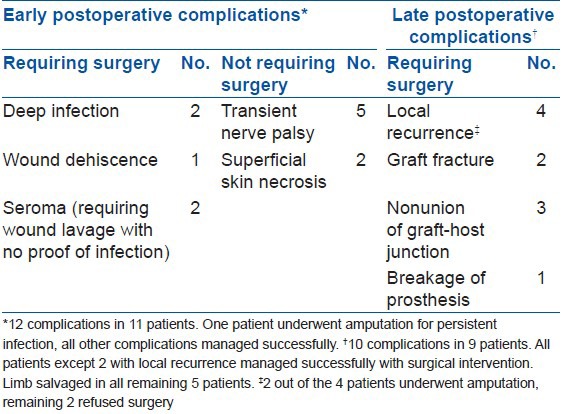
Figure 3B.

X-ray anteroposterior (a) and lateral view (b) Immediate postoperative x-ray showing distal femur prosthesis in situ
Figure 3C.

Clinical photographs of same patient (distal femoral prosthesis) at 6 month followup showing range of motion
Figure 5.
Biological reconstruction with vascular fibular graft (a) clinical photograph of forearm, wrist showing the markings of skin incision for osteosarcoma distal radius (b) peroperative photograph showing defect after resection of distal radius (c) X-ray of forearm wrist showing reconstruction plate in situ with wrist arthrodesis (d) clinical photograph of same patient after vascularised fibular graft and wrist arthrodesis
DISCUSSION
Limb salvage surgery has long been established as the standard of care for osteosarcoma.1,2,3,8 It is widely accepted that these procedures should be performed only at centers with adequate expertise in not just orthopedic oncology, but also other diagnostic and therapeutic oncological specialties. There is not much data on limb salvage surgery for osteosarcoma in Indian patients treated at single/multiple institutions.5 Scarcity of dedicated multidisciplinary teams, lack of a structured referral system and limitation of resources available are some of the reasons behind this paucity. It has been shown that both racial and socio-economic factors influence the outcome of osteosarcoma patients9 and it is imperative that the outcome of contemporary treatment of osteosarcoma in Indian patients be analyzed. The survival rates in our study, though short term, concur with world literature.
The various important factors affecting the outcome in osteosarcoma include stage at the time of presentation, tumor size, tumor histology and response to chemotherapy.4,10,11 In our study, a good histological response to chemotherapy was associated with a statistically better EFS (81.5% vs. 50% 3 year EFS for good vs. poor responders), also shown by Bacci et al. (66.9% vs. 49% 5 year EFS for good vs. poor responders).12 McTiernan et al. also showed a strong correlation between histological response and oncological outcome (5 year OS 71% for good responders vs. 47% for poor responders).6 However, tumor size failed to show any correlation with the outcome and correlation of age and histological subtype in our patients also does not match with these studies. Factors contributing to this observation may be a very high proportion of patients with large disease burden at diagnosis (signifying late diagnosis in the developing world) and short followup of the cohort. Interestingly, there is no data regarding use of HDMTX in osteosarcoma from India and long term followup of these patients may help us to conclude the feasibility, safety and efficacy of HDMTX administration in these patients.
Out of the various options available, the method of reconstruction after resection of bone sarcomas should be chosen taking into account the age, site, socioeconomic profile, occupation, activity level and prognosis of the particular patient.13 In our short term results, we can infer that a biological reconstruction has a higher chance of a repeat surgery for a nononcological indication such as nonunion/implant failure, as reported earlier too.14 Moreover, in the present study time for rehabilitation was the highest in patients undergoing a biological reconstruction. This makes it logical to choose a biological method of reconstruction for patients who are more likely to have survival long enough to justify the long rehabilitation time.
The longevity and the functional outcome are the other two very important factors that are kept in mind while selecting the reconstruction method in a given patient undergoing limb salvage surgery. Due to earlier rehabilitation, immediate and early postoperative functional outcome with nonbiological reconstruction was better than that following biological reconstruction. However, our results show that the functional outcome at final followup in patients undergoing reconstruction by a nonbiological means was similar to those undergoing a biological reconstruction, as most other studies report.14,15 The followup in our study is too small to determine the advantage of a biological reconstruction in terms of durability and our patients need to be followed up for a longer time to be able to precisely compare the results of biological versus nonbiological means of reconstruction.
It is well established that limb salvage surgery is associated with a significant rate of major complication varying from 20% to 40%.16,17 Our patients experienced 15 major complications requiring surgical intervention in 14 patients (27.4%) and another seven (13.7%) minor complications all of which healed conservatively. This complication rate may increase with a longer followup. The rate of infection reported in most series limb salvage with endoprosthesis is around 10-15% while we had a proven deep infection in three (one with an endoprosthesis, two with biological reconstruction) (5.9%) patients.16,18,19 A prompt management of complications is mandatory for a satisfactory outcome and only one of our patients had to have a secondary amputation for a nononcological indication.
The outcome of metastatic osteosarcoma continues to be poor.1 The treatment has to be customized to the patient, depending on the site (pulmonary or extra pulmonary), number and time of presentation. Exclusive lung metastases without extra pulmonary involvement, small in number, resectable and presenting late carry a better prognosis and are good candidates for pulmonary metastectomy.20 There have been reports of improvement in longevity of patients undergoing repeated pulmonary metastectomies.21 As we only included patients undergoing limb salvage surgery, just five patients with metastatic disease (only pulmonary metastases) at presentation were included in this study. All of these five patients showed a good response or complete regression of pulmonary disease with neoadjuvant chemotherapy and two of these patients underwent staged bilateral pulmonary metastectomy. However, at final followup, only one patient remained disease free. Another 3 patients underwent a pulmonary metastasectomy during followup, out of which one patient was not found to have histopathological evidence of disease, as is well reported in literature.22
Ours is a retrospective study with a short followup. Larger single/multicenter studies with longer followup are required to evaluate the outcome of limb salvage surgery in Indian patients with osteosarcoma. However, we can infer that the outcome of limb salvage surgery in Indian patients with osteosarcoma is oncologically and functionally comparable to world literature. State of the art treatment including limb salvage surgery with various methods of reconstruction and multimodal chemotherapy including those with HDMTX based regimen were found to be effective, feasible and safe in this group of Indian patients.
Footnotes
Source of Support: Nil.
Conflict of Interest: None.
REFERENCES
- 1.Allison DC, Carney SC, Ahlmann ER, Hendifar A, Chawla S, Fedenko A, et al. A meta-analysis of osteosarcoma outcomes in the modern medical era. Sarcoma 2012. 2012 doi: 10.1155/2012/704872. 704872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Picci P. Osteosarcoma (osteogenic sarcoma) Orphanet J Rare Dis. 2007;2:6. doi: 10.1186/1750-1172-2-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jaffe N, Puri A, Gelderblom H. Osteosarcoma: Evolution of treatment paradigms. Sarcoma 2013. 2013 doi: 10.1155/2013/203531. 203531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bacci G, Forni C, Ferrari S, Longhi A, Bertoni F, Mercuri M, et al. Neoadjuvant chemotherapy for osteosarcoma of the extremity: Intensification of preoperative treatment does not increase the rate of good histologic response to the primary tumor or improve the final outcome. J Pediatr Hematol Oncol. 2003;25:845–53. doi: 10.1097/00043426-200311000-00006. [DOI] [PubMed] [Google Scholar]
- 5.Agarwal M, Anchan C, Shah M, Puri A, Pai S. Limb salvage surgery for osteosarcoma: Effective low-cost treatment. Clin Orthop Relat Res. 2007;459:82–91. doi: 10.1097/BLO.0b013e31805d85c4. [DOI] [PubMed] [Google Scholar]
- 6.McTiernan A, Jinks RC, Sydes MR, Uscinska B, Hook JM, van Glabbeke M, et al. Presence of chemotherapy-induced toxicity predicts improved survival in patients with localised extremity osteosarcoma treated with doxorubicin and cisplatincisplatin: A report from the European Osteosarcoma Intergroup. Eur J Cancer. 2012:703–12. doi: 10.1016/j.ejca.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–6. [PubMed] [Google Scholar]
- 8.Simon MA, Aschliman MA, Thomas N, Mankin HJ. Limb-salvage treatment versus amputation for osteosarcoma of the distal end of the femur. J Bone Joint Surg Am. 1986;68:1331–7. [PubMed] [Google Scholar]
- 9.Nathan SS, Healey JH. Demographic determinants of survival in osteosarcoma. Ann Acad Med Singapore. 2012;41:390–9. [PubMed] [Google Scholar]
- 10.Ferrari S, Bertoni F, Mercuri M, Picci P, Giacomini S, Longhi A, et al. Predictive factors of disease-free survival for nonmetastatic osteosarcoma of the extremity: An analysis of 300 patients treated at the Rizzoli Institute. Ann Oncol. 2001;12:1145–50. doi: 10.1023/a:1011636912674. [DOI] [PubMed] [Google Scholar]
- 11.Meyers PA, Gorlick R, Heller G, Casper E, Lane J, Huvos AG, et al. Intensification of preoperative chemotherapy for osteogenic sarcoma: Results of the Memorial Sloan-Kettering (T12) protocol. J Clin Oncol. 1998;16:2452–8. doi: 10.1200/JCO.1998.16.7.2452. [DOI] [PubMed] [Google Scholar]
- 12.Bacci G, Longhi A, Versari M, Mercuri M, Briccoli A, Picci P. Prognostic factors for osteosarcoma of the extremity treated with neoadjuvant chemotherapy: 15-year experience in 789 patients treated at a single institution. Cancer. 2006;106:1154–61. doi: 10.1002/cncr.21724. [DOI] [PubMed] [Google Scholar]
- 13.Mangat KS, Jeys LM, Carter SR. Latest developments in limb-salvage surgery in osteosarcoma. Expert Rev Anti cancer Ther. 2011;11:205–15. doi: 10.1586/era.10.225. [DOI] [PubMed] [Google Scholar]
- 14.Brien EW, Terek RM, Healey JH, Lane JM. Allograft reconstruction after proximal tibial resection for bone tumors. An analysis of function and outcome comparing allograft and prosthetic reconstructions. Clin Orthop Relat Res. 1994;303:116–27. [PubMed] [Google Scholar]
- 15.Manfrini M, Tiwari A, Ham J, Colangeli M, Mercuri M. Evolution of surgical treatment for sarcomas of proximal humerus in children: Retrospective review at a single institute over 30 years. J Pediatr Orthop. 2011;31:56–64. doi: 10.1097/BPO.0b013e318202c223. [DOI] [PubMed] [Google Scholar]
- 16.Shehadeh A, Noveau J, Malawer M, Henshaw R. Late complications and survival of endoprosthetic reconstruction after resection of bone tumors. Clin Orthop Relat Res. 2010;468:2885–95. doi: 10.1007/s11999-010-1454-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lindner NJ, Ramm O, Hillmann A, Roedl R, Gosheger G, Brinkschmidt C, et al. Limb salvage and outcome of osteosarcoma. The University of Muenster experience. Clin Orthop Relat Res. 1999;358:83–9. doi: 10.1097/00003086-199901000-00011. [DOI] [PubMed] [Google Scholar]
- 18.Jeys LM, Grimer RJ, Carter SR, Tillman RM. Periprosthetic infection in patients treated for an orthopaedic oncological condition. J Bone Joint Surg Am. 2005;87:842–9. doi: 10.2106/JBJS.C.01222. [DOI] [PubMed] [Google Scholar]
- 19.Graci C, Maccauro G, Muratori F, Spinelli MS, Rosa MA, Fabbriciani C. Infection following bone tumor resection and reconstruction with tumoral prostheses: A literature review. Int J Immunopathol Pharmacol. 2010;23:1005–13. doi: 10.1177/039463201002300405. [DOI] [PubMed] [Google Scholar]
- 20.Rusch VW. Pulmonary metastasectomy. Current indications. Chest. 1995;107(6 Suppl):322S–31. doi: 10.1378/chest.107.6_supplement.322s. [DOI] [PubMed] [Google Scholar]
- 21.Buddingh EP, Anninga JK, Versteegh MI, Taminiau AH, Egeler RM, van Rijswijk CS, et al. Prognostic factors in pulmonary metastasized high-grade osteosarcoma. Pediatr Blood Cancer. 2010;54:216–21. doi: 10.1002/pbc.22293. [DOI] [PubMed] [Google Scholar]
- 22.Picci P, Vanel D, Briccoli A, Talle K, Haakenaasen U, Malaguti C, et al. Computed tomography of pulmonary metastases from osteosarcoma: The less poor technique. A study of 51 patients with histological correlation. Ann Oncol. 2001;12:1601–4. doi: 10.1023/a:1013103511633. [DOI] [PubMed] [Google Scholar]


