Abstract
Background:
The aim of the following study is to evaluate the morbidity, oncologic results and functional outcome in nonmetastatic patients with primary osteosarcoma of the pelvis treated with surgical resection.
Materials and Methods:
Twelve cases of nonmetastatic osteosarcoma of pelvis were operated as part of their multimodality treatment regime between November 2003 and May 2011. There were 5 males and 7 females with a median age of 22 years (range 8-39 years). Ten patients underwent limb sparing resections while 2 had a hindquarter amputation. All 10 cases of limb sparing surgery included resection of the acetabulum. A pseudarthrosis was carried out in 7 cases. Extracorporeal radiation therapy and reimplantation of the bone followed by fixation with plates was used in 1 case and an ischiofemoral arthrodesis was carried out in 2 cases.
Results:
Surgical margins were free in 11 patients. Seven patients had a poor histological response to chemotherapy while 4 patients had a good response to chemotherapy. In the patient reconstructed with radiated auto bone graft, the histological response to chemotherapy could not be assessed. Surgery related complications were seen in 8 out of 12 patients (67%). Three of these patients (25%) required additional surgical intervention for their complications. All patients were available for followup. The median followup of survivors was 56 months (range 24-102 months). Four patients (33%) developed a local recurrence. At 5 years, overall survival was 67%. Patients with a good response to chemotherapy had a better overall survival when compared with patients with a poor response to chemotherapy. The mean Musculoskeletal Tumor Society functional score was 22 (range12-27).
Conclusions:
Though complex and challenging, surgery provides good local control and oncologic outcomes with acceptable function in patients with osteosarcoma of the pelvis treated with appropriate surgical resection as part of their multimodality treatment.
Keywords: Hindquarter, limb salvage, pseudarthrosis, resection
INTRODUCTION
Pelvic osteosarcomas are uncommon and account for approximately 5-10% of these cases including those that arise secondary to Paget's disease or radiotherapy.1,2
In the era of multimodality management, survival for osteosarcoma has improved remarkably. Surgery remains the mainstay of achieving adequate local control in osteosarcoma. Though there is considerable literature regarding appendicular lesions, series documenting the results of surgical excision in pelvic osteosarcoma are not so common.3,4,5 Pelvic tumors besides being uncommon offer a unique challenge to adequate oncologic resection because of their location, large size at presentation and close proximity to neurovascular structures and visceral organs. The perceived poor prognosis in pelvic tumors as compared to extremity lesions, prolonged surgical time with associated blood loss and the possibility of postoperative complications associated with pelvic resections are some of the other daunting features that make surgical treatment of these lesions challenging.3,4,5
While ablative surgery was the accepted treatment until not very long ago, advances in imaging the development of effective adjuvant modalities and refinements in surgical techniques have made limb salvage an oncologically safe option without compromising long term survival even in these daunting lesions. The obvious cosmetic and functional disadvantages because of the loss of the limb associated with a hemipelvectomy has spurred surgeons to develop several methods for reconstruction of the hip and pelvis which give a functional and cosmetically acceptable limb in patients who have had pelvic resections for tumors.1,4 The purpose of this study was to evaluate the morbidity, functional outcome and oncologic results in nonmetastatic patients with primary osteosarcoma of the pelvis treated with surgical resection.
MATERIALS AND METHODS
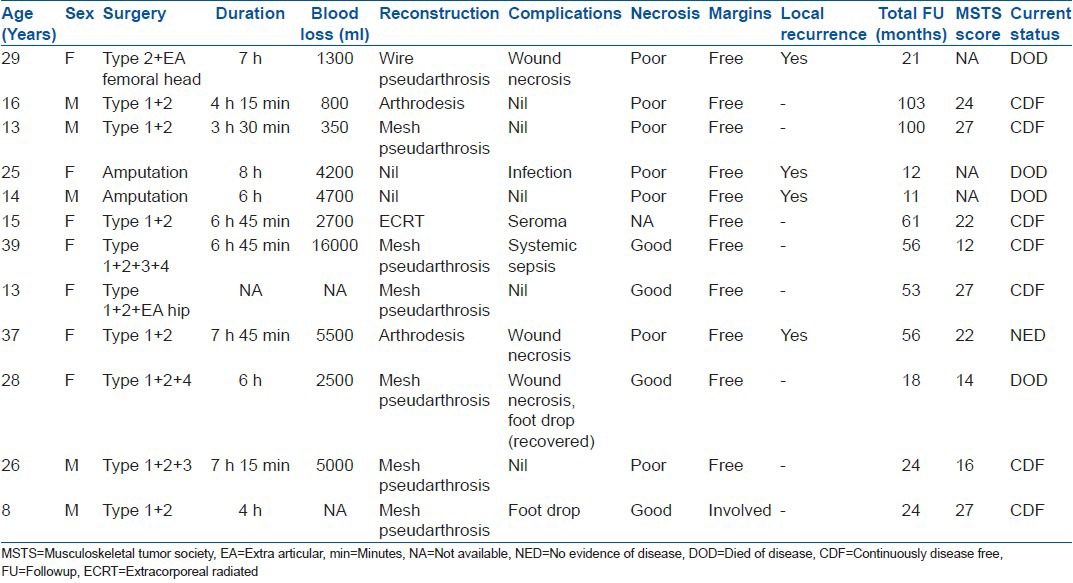
We reviewed 120 malignant tumors of the pelvis which were treated with surgery at our institute between November 2003 and May 2011. The patients were identified by a retrospective review from a prospectively maintained database. These included 12 cases of nonmetastatic osteosarcoma, which were further analyzed for the purpose of this study [Table 1]. The medical records, imaging, oncologic and functional status were reviewed. There were 5 males and 7 females with a median age of 22 years (range 8-39 years).
Table 1.
Clinical details of patients
Histopathological diagnosis was obtained or reviewed in all cases. We preferred a core needle biopsy for diagnosis. Patients with a prior biopsy outside our institute had their slides/blocks reviewed and the diagnosis confirmed. Seven patients had a needle biopsy and 4 patients had an open biopsy. In 1 case the details were not available. Prior to surgery all patients underwent a thorough oncological assessment to determine the extent of local disease and exclude the presence of distant metastases. Staging studies included plain radiographs and magnetic resonance imaging (MRI) of the limb, computed tomography scans of the chest and total body scintigraphy. All patients were nonmetastatic at presentation. Patients received chemotherapy as per the existing hospital protocol. It included a combination of drugs (ifosfamide, adriamycin, cisplatin and etoposide) in alternating cycles. No patient received postoperative radiotherapy with curative intention.
MRI was used to define the extent of the lesion, the involvement of the soft-tissues, relation to the neurovascular bundle and the level of transection of the bone. Proximity to the neurovascular bundle, visceral structures, involvement of the sacro-iliac and hip joints and disease extension across the symphysis pubis were specifically evaluated. The decision to offer surgical excision to these patients was taken at a multidisciplinary tumor board meeting based on the possibility of achieving tumor free resection margins as evaluated on preoperative imaging. The primary goal of surgery was complete excision of the tumor. Limb sparing resection was planned only if oncologically free margins could be achieved with sparing of at least 2 of these 3 structures - lumbosacral plexus/hip joint/femoral neurovascular bundle.
Ten patients underwent limb sparing resections. In 2 cases limb salvage with tumor free margins was not considered possible and they had a hindquarter amputation. Limb sparing pelvic resections were classified according to Enneking and Dunham into 4 types [Figure 1]; iliac (T1), acetabular (T2), pubis or ischium (T3) and sacral (T4).6 Combinations of these resections were also performed. In patients with hip joint involvement an extra articular resection of the hip (EA hip) along with the pelvic segment was performed.
Figure 1.
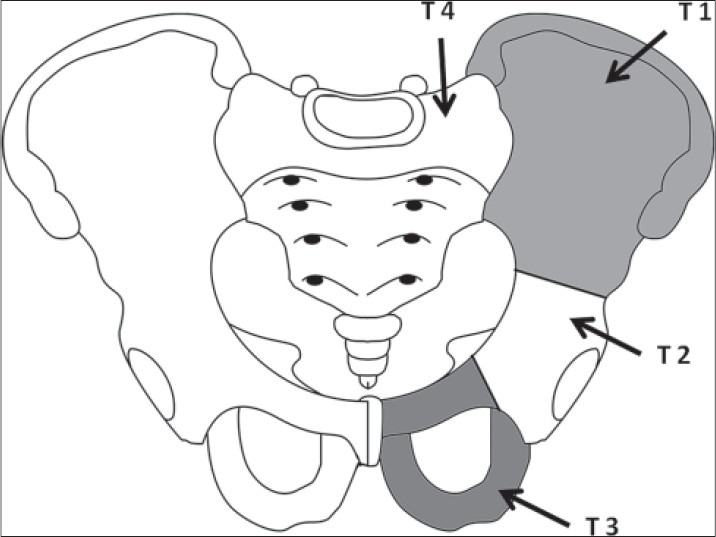
A schematic diagram showing enneking and Dunham's classification of pelvic resection
All 10 cases of limb sparing surgery included resection of the acetabulum. T1 + T2 resection was done in 5 cases, T1 + T2 + T3, T1 + T2 + T4, T1 + T2 + T3 + T4, T1 + T2 + EA hip and T2 + EA hip resection was done in 1 case each respectively.
After resection, various methods of reconstruction were adopted [Table 1]. These were based on the type of resection, amount of residual bone, individual surgeon preference and the functional desires of the patient as assessed during preoperative counseling. A pseudarthrosis was done in 7 cases. In the majority of the pseudarthrosis (6 cases) we performed a hip transposition, stabilizing the femoral head to either the sacrum, residual ilium or ischium using a prolene meshes to create a pseudocapsule [Figure 2]. Stainless steel wire loop was used for temporary stabilization where eventual fibrosis occurred. Extracorporeal radiation therapy and reimplantation of the bone followed by fixation with plates was used in 1 case and an ischiofemoral arthrodesis was done in 2 cases [Table 1].
Figure 2.
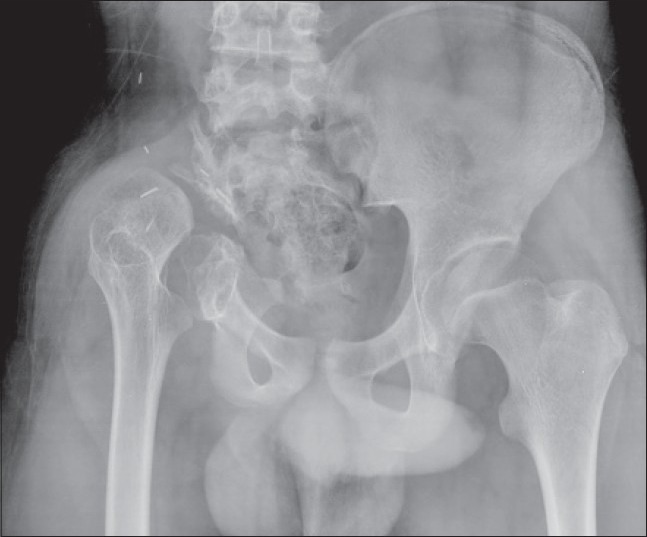
Followup radiograph of pelvis with both hip joints anteroposterior view after T1 + T2 resection with mesh pseudarthrosis
The resected specimens were examined for surgical margins. Margins were classified as free or involved. The histological response to chemotherapy was also assessed. Response to chemotherapy was considered good when the tumor necrosis was more than 90% and poor when the necrosis was less than 90%.
Patients were followed up every 3 months for the first 2 years, every 6 months for the next 3 years and annually thereafter. All patients were available for followup. Followup was calculated from the time of diagnosis to the last date of review or death. Besides screening for disease surveillance, radiographs of the local part were assessed at each visit. Functional status was assessed at the time of last followup using the Musculoskeletal Tumor Society (MSTS) scoring system.7
Survival rates were analyzed with the Kaplan-Meier method. Overall survival was taken from the date of diagnosis to the last date when the patient was documented to be alive or the date of death. Disease-free survival was defined as the time from the date of diagnosis to recurrence of disease at local, regional, or distant sites.
RESULTS
The duration of surgery for the 2 patients who had an external hemipelvectomy was 6 h and 8 h respectively. The average blood loss for this group was 4450 ml (range 4200-4700 ml). The duration of surgery for the limb salvage group ranged from 3.5 h to 7.5 h (mean: 6 h). The average blood loss for this group was 4268 ml (range 350-16000 ml).
Surgical margins were free in 11 patients and involved in 1 patient. This margin was subsequently revised. Seven patients had a poor histological response to chemotherapy while 4 patients had a good response to chemotherapy. In the patient reconstructed with radiated auto bone graft, the histological response to chemotherapy could not be assessed.
Complications
The most common complications were related to wound healing. Three patients had wound necrosis, 2 of which required subsequent debridement. One patient had a postoperative seroma, which settled after conservative treatment and one patient required a wound lavage for suspected infection.
Two patients had a 5th lumbar nerve root injury leading to permanent foot drop while another had transient postoperative foot drop which recovered after 6 months. One patient had signs of early sepsis in the immediate postoperative period and needed admission in the intensive care unit for 10 days. Sexual dysfunction was not assessed in the present series.
Thus, surgery related complications were seen in 8 out of 12 patients (67%). Three patients (25%) required additional surgical intervention for their complications.
Oncological results
All patients were available for followup. The followup ranged from 8 to 102 months (median: 41.5 months, mean: 44 months). All survivors had a minimum 24 month followup.
Four patients (33%) developed a local recurrence. All these patients had a biopsy prior to presenting to our institute (3 patients had an open biopsy and in 1 patient details were not available). The resection margins were free in all these cases. All patients with local recurrence had a poor response to chemotherapy. Two of these patients were offered best supportive care in view of unresectable local recurrent disease. One patient was treated with excision of the recurrent disease. Another patient was offered external hemipelvectomy but refused and was treated with palliative radiotherapy. Of the 4 patients, only one is currently disease free and 3 patients have died due to disease progression.
One patient developed pulmonary metastasis in spite of good response to chemotherapy. A pulmonary metastetectomy was attempted, but the disease was found to be unresectable and the patient was offered best supportive care.
Eight patients are currently alive and disease free. Of these 7 patients are continuously diseases free. The median followup of survivors was 55.5 months (24-102 months). At 5 years, disease free survival was 53.3% and overall survival [Figure 3] was 66.7%. Patients with a good response to chemotherapy had a better overall survival when compared to patients with a poor response to chemotherapy (80% vs. 57%) (P = 0.412) [Figure 4].
Figure 3.
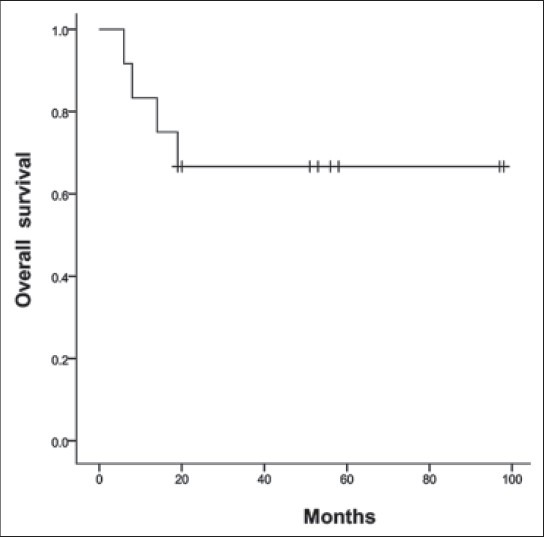
Kaplan-Meier curve depicting overall survival
Figure 4.
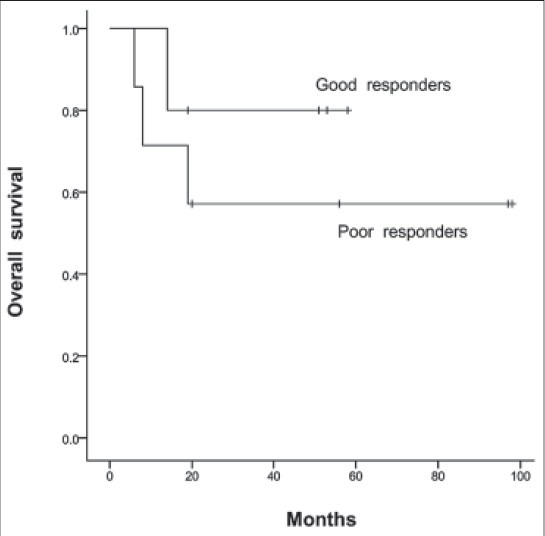
Kaplan-Meier curve depicting survival based on response to chemotherapy
Functional results
The functional status was determined at final followup using the MSTS scoring system. This was based on the analysis of six factors (pain, functional activities, emotional acceptance, use of supports for ambulation, walking ability and gait). For each of the six factors, values of 0 to 5 were assigned based on established criteria. The result was expressed as a sum total with a maximum score of 30. The MSTS score was available in all 8 survivors. It ranged from 12-27 (mean: 22). The 2 patients with an arthrodesis had a score of 22 and 24 respectively. Among these, patients under 18 years (n=3) had a better score than patients older than 18 years (n=2) (27 vs. 14). The patient with an extracorporeal radiated and reimplantation had a MSTS score of 26.
DISCUSSION
Pelvic osteosarcomas are far rarer than extremity lesions and their resection and reconstruction is much more challenging.8 Most of these tumors present with a large intra pelvic mass due to the absence of conventional restrictive barriers like deep fascia. Resectability may be compromised because of the size, involvement of visceral organs or medial extension with involvement of neural structures in the sacrum.1 There is a perception that pelvic osteosarcomas have a dismal prognosis.1,2,4,9 This series selectively analyses the morbidity, functional and oncologic outcomes of nonmetastatic primary pelvic osteosarcomas appropriately treated with adequate resection in a multidisciplinary setting. Though the superiority of limb salvage surgery over an amputation in maintaining the patient's image of body integrity and enhancing limb function is well documented, at no stage must limb salvage be attempted if oncologic clearance is likely to be compromised.1,10
Surgical complications can include infection, hematoma, delayed healing skin problems and nerve injuries which can affect more than 50% of patients in some series.2,4,9,11 Two thirds of our patients had a surgical complication and 25% of our cases required a second intervention for surgical complications. Only 1 patient needed a lavage for infection in our series. The type of reconstruction modality employed can influence the rate of infection.12 Reconstruction varies according to the anatomical location, extent of resection, patient's functional demands and individual surgeon preference.13 In the present series we have not used pelvic prosthesis or allografts for reconstruction and have largely preferred pseudarthrosis/hip transposition. The absence of large implants and allografts helps reduce surgical time, facilitate closure and may decrease the incidence of infection and late revision because of implant failure.14,15,16 Hillman et al. in their study have reported that hip transposition had the least incidence of complications after resection of the acetabulum as compared to the use of prosthesis or prosthesis and allograft.12 Free from the constraints of being dependent on a custom made endoprosthesis or on a chosen allograft, the resection can be done without being overly concerned about the reconstruction. If there has been some additional tumor growth since the imaging on which a custom made prosthesis was planned, the surgeon has the flexibility to further widen the resection margins based on the latest preoperative imaging.17 This may have contributed to our ability to achieve tumor free margins in all but 1 case. Advances in imaging technology have also helped the surgeon plan surgical margins with greater accuracy than in earlier eras.10
In spite of adequate oncologic clearance our local recurrence rate was 33%, including both cases who had an amputation. Though these rates are similar to other reports, the fact that all these patients had been biopsied elsewhere with nonadherence to oncologic principles could have been a causative factor.18 The poor response to chemotherapy in these patients was an additional contributor. It has been shown that in spite of adequate margins, local recurrence rates are higher in those patients that show a poor response to chemotherapy.19
Our overall survival at 5 years of 67% is better than results of most other series.4,5 The fact that our series only included a selective cohort of nonmetastatic patients with primary osteosarcoma treated at a specialty center could account for this. It has been well established that survival decreases in cases of secondary osteosarcoma and those that have metastasis at presentation.4 Our results for these pelvic tumors are comparable to those achieved for our extremity lesions thus belying the fact that appropriately treated pelvic lesions have a dismal prognosis.20,21
Our MSTS scores showed little difference between arthrodesis and pseudarthrosis. Over the years we have tended to favor the latter. The mobility retained at the area of the hip after pseudarthrosis is invaluable in cultures where patients need to squat or sit on the floor, functions that are difficult to perform after an arthrodesis or prosthesis. Patients less than 18 years had better functional outcomes compared with older patients and it is well established that younger patients adapt to functional limitations better.11
The strength of the present study lies in the fact that it spans a short duration (8 years) during which patients were treated at a specialty center by the same multidisciplinary team. Treatment protocols were well established and rigidly adhered to. The small numbers in this series may be considered as a limitation by some. Osteosarcomas of the pelvis are uncommon lesions and the fact that only 12 cases were operated in an 8 year period from a tertiary cancer hospital with a wide experience of managing pelvic malignancies bears testimony to that fact.22 Similarly, a high volume globally recognized European center documented the results of only 22 primary high grade pelvic osteosarcomas over a 25 year period.4
The oncologic outcomes of patients with osteosarcoma of the pelvis treated with appropriate surgical resection as part of their multimodality treatment are very encouraging. Though limb salvage in these tumors is challenging with its inherent complications the ultimate functional outcomes are good.
Footnotes
Source of Support: Nil.
Conflict of Interest: None.
REFERENCES
- 1.Guo W, Sun X, Ji T, Tang X. Outcome of surgical treatment of pelvic osteosarcoma. J Surg Oncol. 2012;106:406–10. doi: 10.1002/jso.23076. [DOI] [PubMed] [Google Scholar]
- 2.Isakoff MS, Barkauskas DA, Ebb D, Morris C, Letson GD. Poor survival for osteosarcoma of the pelvis: A report from the Children's Oncology Group. Clin Orthop Relat Res. 2012;470:2007–13. doi: 10.1007/s11999-012-2284-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fuchs B, O’Connor MI, Kaufman KR, Padgett DJ, Sim FH. Iliofemoral arthrodesis and pseudarthrosis: A long term functional outcome evaluation. Clin Orthop Relat Res. 2002;397:29–35. doi: 10.1097/00003086-200204000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Grimer RJ, Carter SR, Tillman RM, Spooner D, Mangham DC, Kabukcuoglu Y. Osteosarcoma of the pelvis. J Bone Joint Surg Br. 1999;81:796–802. doi: 10.1302/0301-620x.81b5.9241. [DOI] [PubMed] [Google Scholar]
- 5.Ozaki T, Flege S, Kevric M, Lindner N, Maas R, Delling G, et al. Osteosarcoma of the pelvis: Experience of the cooperative osteosarcoma study group. J Clin Oncol. 2003;21:334–41. doi: 10.1200/JCO.2003.01.142. [DOI] [PubMed] [Google Scholar]
- 6.Enneking WF, Dunham WK. Resection and reconstruction for primary neoplasms involving the innominate bone. J Bone Joint Surg Am. 1978;60:731–46. [PubMed] [Google Scholar]
- 7.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res. 1993;286:241–6. [PubMed] [Google Scholar]
- 8.Dominkus M, Darwish E, Funovics P. Reconstruction of the pelvis after resection of malignant bone tumours in children and adolescents. Recent Results Cancer Res. 2009;179:85–111. doi: 10.1007/978-3-540-77960-5_8. [DOI] [PubMed] [Google Scholar]
- 9.Kawai A, Huvos AG, Meyers PA, Healey JH. Osteosarcoma of the pelvis. Oncologic results of 40 patients. Clin Orthop Relat Res. 1998;348:196–207. [PubMed] [Google Scholar]
- 10.Schwameis E, Dominkus M, Krepler P, Dorotka R, Lang S, Windhager R, et al. Reconstruction of the pelvis after tumor resection in children and adolescents. Clin Orthop Relat Res. 2002;402:220–35. doi: 10.1097/00003086-200209000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Rödl RW, Hoffmann C, Gosheger G, Leidinger B, Jürgens H, Winkelmann W. Ewing's sarcoma of the pelvis: Combined surgery and radiotherapy treatment. J Surg Oncol. 2003;83:154–60. doi: 10.1002/jso.10256. [DOI] [PubMed] [Google Scholar]
- 12.Hillmann A, Hoffmann C, Gosheger G, Rödl R, Winkelmann W, Ozaki T. Tumors of the pelvis: Complications after reconstruction. Arch Orthop Trauma Surg. 2003;123:340–4. doi: 10.1007/s00402-003-0543-7. [DOI] [PubMed] [Google Scholar]
- 13.O’Connor MI. Malignant pelvic tumors: Limb-sparing resection and reconstruction. Semin Surg Oncol. 1997;13:49–54. doi: 10.1002/(sici)1098-2388(199701/02)13:1<49::aid-ssu8>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 14.Angelini A, Drago G, Trovarelli G, Calabrò T, Ruggieri P. Infection after surgical resection for pelvic bone tumors: An analysis of 270 patients from one institution. Clin Orthop Relat Res. 2014;472:349–59. doi: 10.1007/s11999-013-3250-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Aydinli U, Ozturk C, Yalcinkaya U, Tirelioglu O, Ersozlu S. Limb-sparing surgery for primary malignant tumours of the pelvis. Acta Orthop Belg. 2004;70:417–22. [PubMed] [Google Scholar]
- 16.Beadel GP, McLaughlin CE, Wunder JS, Griffin AM, Ferguson PC, Bell RS. Outcome in two groups of patients with allograft-prosthetic reconstruction of pelvic tumor defects. Clin Orthop Relat Res. 2005;438:30–5. doi: 10.1097/01.blo.0000180048.43208.2f. [DOI] [PubMed] [Google Scholar]
- 17.Gebert C, Gosheger G, Winkelmann W. Hip transposition as a universal surgical procedure for periacetabular tumors of the pelvis. J Surg Oncol. 2009;99:169–72. doi: 10.1002/jso.21212. [DOI] [PubMed] [Google Scholar]
- 18.Fuchs B, Hoekzema N, Larson DR, Inwards CY, Sim FH. Osteosarcoma of the pelvis: Outcome analysis of surgical treatment. Clin Orthop Relat Res. 2009;467:510–8. doi: 10.1007/s11999-008-0495-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Grimer RJ, Taminiau AM, Cannon SR Surgical Subcommitte of the European Osteosarcoma Intergroup. Surgical outcomes in osteosarcoma. J Bone Joint Surg Br. 2002;84:395–400. doi: 10.1302/0301-620x.84b3.12019. [DOI] [PubMed] [Google Scholar]
- 20.Puri A, Gulia A. The results of total humeral replacement following excision for primary bone tumour. J Bone Joint Surg Br. 2012;94:1277–81. doi: 10.1302/0301-620X.94B9.29697. [DOI] [PubMed] [Google Scholar]
- 21.Puri A, Gulia A, Jambhekar N, Laskar S. The outcome of the treatment of diaphyseal primary bone sarcoma by resection, irradiation and reimplantation of the host bone: Extracorporeal irradiation as an option for reconstruction in diaphyseal bone sarcomas. J Bone Joint Surg Br. 2012;94:982–8. doi: 10.1302/0301-620X.94B7.28916. [DOI] [PubMed] [Google Scholar]
- 22.Puri A, Pruthi M, Gulia A. Outcomes after limb sparing resection in primary malignant pelvic tumors. Eur J Surg Oncol. 2014;40:27–33. doi: 10.1016/j.ejso.2013.10.017. [DOI] [PubMed] [Google Scholar]


