Abstract
Background:
Allograft–prosthetic composite can be divided into three groups names cemented, uncemented, and partially cemented. Previous studies have mainly reported outcomes in cemented and partially cemented allograft–prosthetic composites, but have rarely focused on the uncemented allograft–prosthetic composites. The objectives of our study were to describe a surgical technique for using proximal femoral uncemented allograft–prosthetic composite and to present the radiographic and clinical results.
Materials and Methods:
Twelve patients who underwent uncemented allograft–prosthetic composite reconstruction of the proximal femur after bone tumor resection were retrospectively evaluated at an average followup of 24.0 months. Clinical records and radiographs were evaluated.
Results:
In our series, union occurred in all the patients (100%; range 5-9 months). Until the most recent followup, there were no cases with infection, nonunion of the greater trochanter, junctional bone resorption, dislocation, allergic reaction, wear of acetabulum socket, recurrence, and metastasis. But there were three periprosthetic fractures which were fixed using cerclage wire during surgery. Five cases had bone resorption in and around the greater trochanter. The average Musculoskeletal Tumor Society (MSTS) score and Harris hip score (HHS) were 26.2 points (range 24-29 points) and 80.6 points (range 66.2-92.7 points), respectively.
Conclusions:
These results showed that uncemented allograft–prosthetic composite could promote bone union through compression at the host–allograft junction and is a good choice for proximal femoral resection. Although this technology has its own merits, long term outcomes are yet not validated.
Keywords: Bone tumor, uncemented allograft prosthetic composite, proximal femur
INTRODUCTION
Surgical treatment for primary malignant and aggressive benign tumors of the proximal femur involves wide excision of the proximal part. Reconstruction of these surgically created bone defects is challenging because improved survival of patients with musculoskeletal tumors is resulting in greater demands on the limb reconstruct.
Allograft prosthesis composites (APCs) have been used since the late 1980s in managing defects following tumor resections.1 Because of its known advantages compared with the megaprosthesis,2 APC has been used widely for the reconstruction of the proximal femur following tumor resection.
Depending on the method of fixation, APC can be divided into three groups; cemented, uncemented (interference fit or press fit), and partially cemented. Partially cemented fixation means cementing the prosthesis into the allograft and pressing the composite into the host bone without cement.
Most of the previous studies have reported the functional evaluation, radiographic outcomes, and complications of cemented and partially cemented APC,3,4,5,6,7,8,9,10,11,12 but rarely the uncemented APC has been focused upon. We would like to share our experience with the use of uncemented APC in limb salvage surgery. In this study, we aim to describe the surgical technique for proximal femoral uncemented APC and present the radiographic and clinical results.
MATERIALS AND METHODS
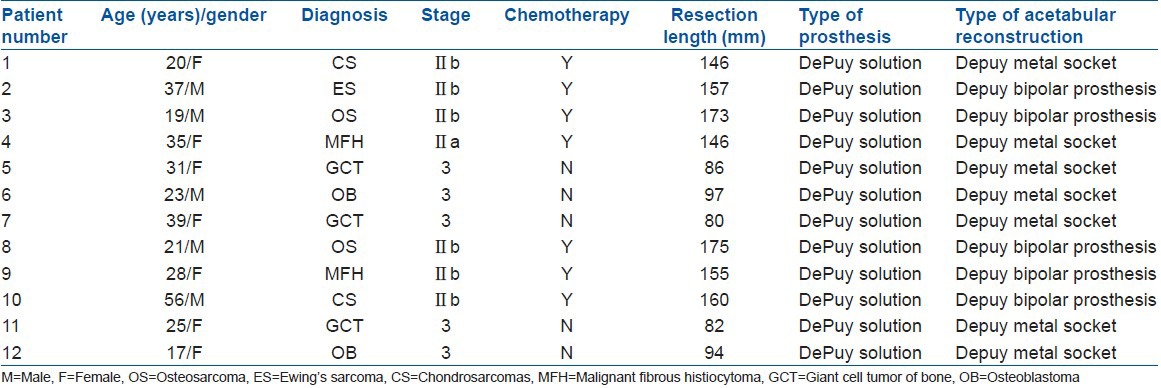
We retrospectively reviewed 12 patients with bone tumors of the proximal femur who underwent reconstruction with uncemented APC between 2007 and 2010. All operations were performed in West China Hospital by the senior surgeon (CT). There were five male and seven female patients, with age ranging from 17 to 56 years (average, 29 years). The diagnosis was chondrosarcoma in two patients, osteosarcoma in two patients, Ewing's sarcoma in one patient, malignant fibrous histiocytoma in two patients, osteoblastoma in two patients, and giant cell tumor of bone in three patients [Table 1]. Among the 12 patients, 2 cases of giant cell tumor of bone and osteoblastoma had surgeries before. The others had no previous treatment.
Table 1.
Details of surgical technique and results in 12 patients
Preoperative assessment
All patients were required to undergo 100% magnified X-ray, computed tomography scan, magnetic resonance imaging, and emission computed tomography [Figure 1a-c]. On the basis of these imaging results, we measured the exact boundary of the tumor, the resection length, diameter and the cortex thickness of the narrowest part of the medullary cavity, and the distance between the site of the osteotomy and the narrowest part of the medullary cavity. Next, the matched allograft was selected. Before surgery, biopsy was done. Patients diagnosed as malignant bone tumor were treated with neoadjuvant chemotherapy routinely.
Figure 1.

Radiographs show fixation with reconstruction interlocking nail after curettage and bone grafting of osteoblastoma (Enneking 3) of the left proximal femur. (a) The preoperative anteroposterior radiograph. (b) Immediate postoperative anteroposterior radiograph. (c) 7 month postoperative anteroposterior radiograph the white arrow indicates the recurrence site. (d-f) These radiographs show an uncemented allograft–prosthesis composite after resection of a recurrent osteoblastoma. (d) The immediate postoperative anteroposterior radiograph after APC reconstruction. (e) 3-month postoperative anteroposterior radiograph with the white arrow indicates blurring with bridging trabeculae at the junction. (f) 7 month postoperative anteroposterior radiograph with the black arrow indicates bone union and the white arrow indicates bone resorption in the greater trochanter. (g) 28-month postoperative anteroposterior the black arrow indicates the bone union is strengthened and the white arrow indicates severe bone resorption in the greater trochanter
The allografts were harvested from cadaver donors and the fresh frozen allografts were cryopreserved in a freezer at −80°C with addition of dimethyl sulfoxide and rifampicin. All the grafts were obtained from the bone bank in Sichuan province, China.
Perioperative management
The patients were put in lateral position. Lateral approach was used in all cases and the incision from the previous procedure was used if possible and excised the previous scar was excised. All previous biopsy sites including any needle biopsy tracks were removed en bloc. The surgical procedure included two major steps, resection and reconstruction.
During surgery, the abductor muscle was preserved if possible. There were three patients in whom part of the greater trochanter was preserved. Of these two cases were diagnosed as giant cell tumor of bone and one was a case of osteoblastoma. The range of tumor resections conformed to the principles: For aggressive benign tumors, an en bloc excision with at least 2 cm margin was performed; for primary malignant tumors, an en bloc excision with at least 5 cm margin of the bone and 1 cm margin of the surrounding normal soft tissue was performed. The distal femoral cut was horizontal. The resection length, measured from the tip of the greater trochanter, ranged from 8.0 to 17.5 cm (average 12.9 cm). Before osteotomy, 1.0-1.5 cm normal periosteal cuff was left with the normal femur if possible to help bony union. After osteotomy, the medullary tissue of distal femur and the soft tissues from eight random points of the tumor bed were sent for frozen biopsy in order to ensure the clearance of the en bloc resection.
Reconstruction was performed during the same surgery. Allograft was prepared to match the length of the bone defect correctly. Next, the allograft and host femur were reamed to fit the prosthesis and the greater and lesser trochanters were prepared for the soft tissue reconstruction using drill holes in the graft. The allograft was degreased by medical alcohol and pulsatile lavaged by abundant normal saline. Reaming of the medullary cavity is very important; the diameter of the reaming should be a little less than that of the prosthetic stem and the depth of the reaming should be 2 cm shorter than the distance that the stem can reach. After trial fitting, we pressed the prosthetic stem into the allograft and the composite into the host bone. The allograft host bone junctions were covered with granular allogenous spongy bone and covered with the periosteal cuff. Five patients underwent bipolar replacement, whereas the others underwent total hip replacement.
Finally, the attachment of the important muscles was reconstructed. For the three patients who had insertion of the gluteus medius preserved, 2.0-mm nonabsorbable suture was used to suture insertion onto the allograft greater trochanter. For others, the gluteus medius and gluteus minimus were sutured to the greater trochanter of the allograft directly by 2.0-mm nonabsorbable suture and the gluteus medius, the vastus lateralis, and the fascia lata were sutured together. The iliopsoas muscle was sutured back to lesser trochanter.
Postoperative management
After surgery, prophylactic iv antibiotics were used for 1-2 days. The rehabilitation program was designed on the basis of the surgeon's assessment during operation. Generally, the lower extremity was fixed in the abduction neutral position by a brace and the quadriceps femoris was exercised for 4 weeks in bed after surgery. During the process, deep vein thrombosis (DVT) prophylaxis was used until partial weight bearing. Partial and full weight bearing were permitted 4 and 12 weeks after surgery, respectively.
Followup
All patients were followed up clinically every month during the first 6 months, every 3 months during the first 2 years, and then once in 1 year. We performed radiographic assessment at 1 month, 3 months, 6 months, 9 months, and 12 months after surgery and then annually. Radiographs were assessed for evidence of union at the junction of allograft and the host bone and for trochanteric resorption [Figure 1d-f]. We defined union at the allograft and host bone junction by radiographic evidence of blurring, with bridging trabeculae at the junction with no radiolucent lines around the junction.15 Nonunion was not diagnosed until at least 1 year without further progress.16 The general followup ranged from 16 to 35 months, with an average followup of 24.0 months. The Musculoskeletal Tumor Society (MSTS) scoring system13 and Harris Hip Score14 (HHS; for which a score of <70 is poor, 70-79 is fair, 80-89 is good, and 90-100 is excellent) were used to assess functional outcome. Manual testing (grade 0-5) was used to evaluate abductor muscle force.
In all cases, the abductors were reattached to the allograft, so we also measured the abductor muscle force. We measured the abductor muscle force by physical examination, and we tested the muscle force by Manual Muscle-Testing. This is the most popular strength test. The physical therapist will push on your body in specific directions while you resist the pressure. A score or grade is then assigned, depending on how much you were able to resist the pressure. Strength is measured on a five-point scale: 0/5. A 0/5 score means that you are unable to create any visible or noticeable contraction in a specific muscle. This occurs when a muscle is paralyzed, such as after a stroke, spinal cord injury or cervical or lumbar radiculopathy. Sometimes pain can prevent a muscle from contracting at all. 1/5. A grade of 1/5 occurs when muscle contraction is noted but no movement occurs. The muscle is not strong enough to lift the particular body part against gravity or move it when in a gravity reduced position. 2/5. This muscle-strength grade is assigned when your muscle can contract but cannot move the body part fully against gravity. When gravity is reduced or eliminated during a change in body position, the muscle is able to move the body part through its full range of motion. 3/5. A 3/5 grade means that you are able to fully contract your muscle and move your body part through its full range of motion against the force of gravity. But when resistance is applied, the muscle is unable to maintain the contraction. 4/5. A 4/5 grade indicates that the muscle yields to maximum resistance. The muscle is able to contract and provide some resistance, but when your physical therapist presses on the body part, the muscle is unable to maintain the contraction. 5/5. This means the muscle is functioning normally and is able to maintain its position even when maximum resistance is applied. so we admitted that will be some subjective, but in our opinion.
Statistical analysis
Wilcoxon signed-rank test was employed for two related nonparametric data. Mann–Whitney test was employed for two independent nonparametric data. A P value of 0.05 or less was considered statistically significant.
RESULTS
In our series, union occurred in all patients (100%; range 5-9 months). There was no periprosthetic bone resorption at the junction of the allograft and the host bone, but mild resorption could be seen in the greater trochanter in five patients [Table 2, Figure 1f, g].
Table 2.
Details of the surgical technique and results in the 12 patients
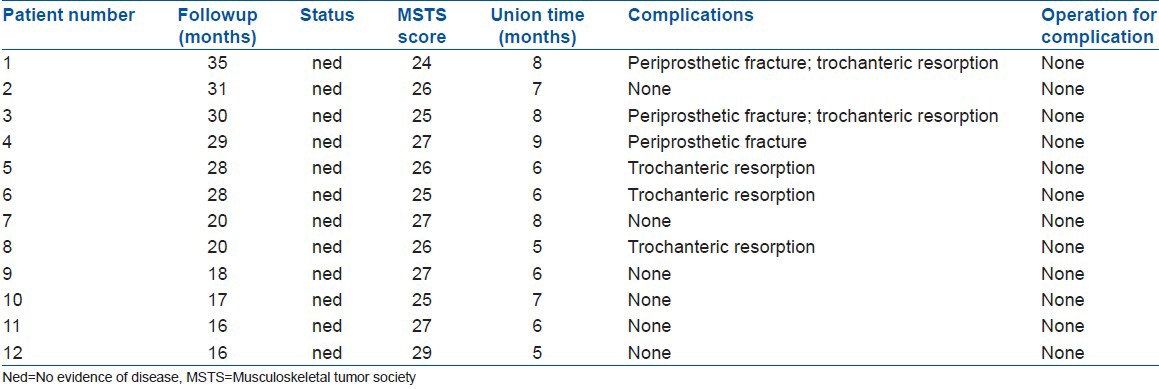
Functional results were evaluated in 12 patients with a followup of at least 16 months. The MSTS system was used for evaluation. The average preoperative score was 11.5 points (range 7-15 points) and the average postoperative score was 26.2 points (range 24-29 points) [Table 2]. Wilcoxon signed-rank test showed a significant difference between the preoperative MSTS score and the postoperative score (P = 0.002). Mann–Whitney test showed that there was no significant difference in MSTS score at the last followup between patients with benign tumor and those with a malignant lesion (P = 0.268) and there was no significant difference in the MSTS score at the last followup between patients with total hip and those with bipolar prosthesis (P = 0.432).
We compared preoperative Harris hip score (HHS) score with the score at the last followup examination. The average preoperative score was 48.0 points (range 40.3-58.5 points) and the average postoperative score was 80.6 points (range 66.2-92.7 points). Wilcoxon signed-rank test showed that there was a significant difference between the preoperative HHS score and the postoperative score (P = 0.002). Mann–Whitney test showed that there was a significant difference in HHS score at the last followup between patients with benign and those with malignant tumor (P = 0.010) and there was no significant difference in HHS score at the last followup between patients with total hip and those with bipolar prosthesis (P = 0.149).
The average postoperative manual muscle grade was 4.3 (range 3-5) without nerve palsy. Mann–Whitney test showed that there was no significant difference in abductor muscle force at the last followup between the three patients with insertion of the gluteus medius preserved and the others (P = 0.064). No recurrence, metastasis, or deaths were reported until the most recent followup [Table 2].
During surgery, there was no neurovascular injury, fat embolism, coagulopathy, or pulmonary edema. But there were three periprosthetic fractures which were fixed by cerclage wire [Table 2, Figure 2]. Among the three cases, it happened in host bone in one case and in allograft in two cases. They all occurred in the early stage of the surgeon's experience. The fracture line were all longitudinal, the cerclage wire was just locally used to avoid destroying the periosteum, so its effect on the bone junction was small, and the fracture sometimes happened in the allograft which itself was dead, therefore the fracture made little influence. So during followup, we did not find any different outcome for these three cases. Until the most recent followup points, there were no complications such as infection, nonunion, resorption, wear of acetabulum socket, dislocation, and chronic allergic reaction.
Figure 2.
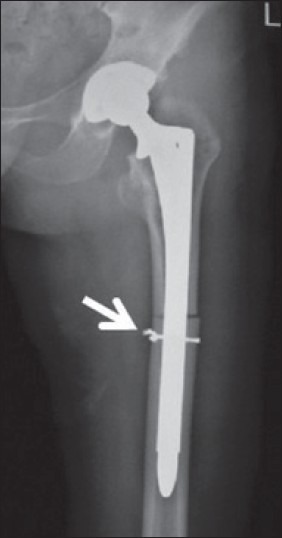
The immediate postoperative anteroposterior radiograph white arrow indicates intraoperative fracture which was fixed by cerclage wire
DISCUSSION
The most common methods for reconstruction of proximal femur include APC and proximal femoral replacement prosthesis (megaprosthesis).9,10,11,17 Although as compared to APC, the biggest advantage of megaprosthesis is no allograft-related complications but there are many hardware complications, such as loosening, fracture, and revision difficulty. Therefore, to the patient with a long expected survival time, megaprosthesis may be not the first choice. APC has its own merits such as the effective reattachment of the tendons of the hip abductors to prevent dislocation, allowing better function, restoration of bone stock, load sharing after union, and the ability to precisely adjust graft length. But the limitations are also obvious, which include infection, fracture, nonunion, resorption, difficulty in revision, etc.3,4,5,6,7,8,9,10,11,12
Nowadays, cemented and partially cemented APC is widely accepted.8,10,12,18,19 But the risks of cement-related adverse effects such as cardiovascular toxicity are inevitable. During surgery there will be a risk that cement is left between the allograft and host bone to block bone union. Cemented APC would be more difficult and destructive if removal of the implant is necessary. And previous studies showed that the incidence of nonunion ranged from 3.5 to 23%.18,20,21
Uncemented APC is highlighted by its fixation pattern which is using interference fit (press fit). Its main advantage is bone ingrown and revascularization after weight bearing.19 Previous studies about cemented or partially cemented APC showed that the incidence of nonunion ranged from 3.7 to 25.0%, but seldom described the time for junctional union after operation.1,2,9,10,15,22 In our series union was observed in all patients, the time of union ranged from 5 to 9 months. Resorption was not observed until the most recent followup point.
Stable fixation of the noncemented APC is more challenging. Obviously, it is easy to fix the prosthesis into the allograft tightly. We should achieve at least 4-6 cm distal fixation to the host bone, and the size and length of the stem will depend on the size of the medullary cavity of the host bone and the level of resection. Therefore, before surgery, the diameter of the narrowest part of medullary cavity and the length of resection should be measured. During surgery, firstly, reaming should abide by the preoperative plan. Secondly, in order to gain a perfect distal fit, the diameter of reaming can be a little smaller than that of the prosthetic stem Thirdly, the host bone should be reamed 2 cm shorter than the length of the distal prosthetic stem, so that the distal part of the stem can be pressed directly into the host bone to increase stability. Fourthly, template trials should be done in time. When the reaming is a little loose, we can bend the distal part of prosthetic stem (about 1°-3°) before insertion to gain stable fixation. Meanwhile, we should avoid tight reaming to avoid periprosthetic fracture. In our series, there were three cases with periprosthetic fracture, but after our proper management there was no significant difference between them and the others.
Bone resorption in the greater trochanter and periprosthetic fracture are the main complications in this surgery. Bone resorption in the greater trochanter could be caused by the modes of reconstruction of the abductor mechanism. Probably just suturing the abductor mechanism back is not enough. Also, the stress is just on the tip of the greater trochanter. This should be improved to decentralize the stress. Perioperative fracture could be seen in both allograft and host bone. This could be due to many reasons such as lack of experience of the surgeon in the early stage, fragile allograft after proper management, and so on.
Up to now, the indications for uncemented APC are not absolutely established. Gross and Hutchison23 support proximal femoral allograft for the reconstruction of circumferential defects of more than 3 cm in length from the calcar, some combined defects, and in some cases of femoral discontinuity. Donati7 believed the APC can be used in younger patients with a longer life expectancy, when substantial portions of the periacetabular muscles and tendons can be spared and it is not planned to use radiation therapy that can interfere with bone healing. In our opinion, besides the indications of limb salvage surgery, the specific indications for APC reconstruction of proximal femur are: (1) all the patients should have long expected nondisease survival time; (2) the site of osteotomy should be at least lower than the lesser trochanter; (3) the important surrounding soft tissue and muscles could be reconstructed; and (4) the complications of allograft can be accepted by the patient and his/her family. In our series, there were five patients with greater trochanter resorption (Gruen zone 1). A previous study of over 10 years followup of normal total hip arthroplasty has shown that the resorption of the proximal femur was always observed in the Gruen zones 1 and 7.24,25 Lee et al.19 reported on seven hips (46.6%) in which there was resorption, and resorption was most common in Gruen zone 7 (5 hips) and zone 1 (1 hip), and one hip had resorption in both zones. But the reason for this is still not clear. In our opinion, the high rate of greater trochanter resorption was caused by stress concentration by the reconstruction of the abductor mechanism. Therefore, we advise to increase the contact area of the muscle and the great trochanter in order to decentralize the local stress.
From the functional result, there was a significant difference between the preoperative and postoperative scores, both in MSTS system and HHS system. But when comparing the scores at the last followup between patients with benign tumor and those with malignant tumor, these two systems showed different results. The reasons could be: The relatively small sample and certain criteria (such as pain, emotional acceptance) in these two systems were highly subjective. Because there was no significant difference in the scores at the last followup between patients with acetabulum socket and those with bipolar prosthesis in both scoring systems, we suppose that acetabulum reconstruction has little effect on the functional result if the bone quality of acetabulum is good enough. Although there was no significant difference in the abductor muscle force at the last followup between the three patients with insertion of the gluteus medius preserved and the others, the P value (P = 0.064) was much more closer to 0.05. Therefore, we can also conclude that if possible, we should preserve insertion of the gluteus medius and even part of the greater trochanter for abductor reconstruction.
CONCLUSION
Although APC provides a means of improving functional outcome after reconstruction of the proximal femur, there are still many improvements that need to be accomplished to have perfect outcomes and avoid the incidence of complications. Uncemented fixation is such an improvement. The midterm clinical results show that this reliable and satisfactory technique can promote union through compression at the host–allograft junction with weight-bearing, but to the patients and the surgeons, not only the function reconstruction but also the longevity of reconstruction is significant; therefore, long term and larger sample outcome is expected.
Footnotes
Source of Support: Nil.
Conflict of Interest: We have no conflict of interest with any company or organization or entity with financial interest in the subject matter or the materials mentioned in the manuscript.
REFERENCES
- 1.Jofe MH, Gebhardt MC, Tomford WW, Mankin HJ. Reconstruction for defects of the proximal part of the femur using allograft arthroplasty. J Bone Joint Surg. 1988;70:507–16. [PubMed] [Google Scholar]
- 2.Park YS, Moon YW, Lee BT, Wang JH. Structural allograft for femoral deficiency in revision total hip arthroplasty. J Korean Orthop Assoc. 2004;39:7. [Google Scholar]
- 3.Zehr RJ, Enneking WF, Scarborough MT. Allograft-prosthesis composite versus megaprosthesis in proximal femoral reconstruction. Clin Orthop Relat Res. 1996;322:207–23. [PubMed] [Google Scholar]
- 4.Kabukcuoglu Y, Grimer RJ, Tillman RM, Carter SR. Endoprosthetic replacement for primary malignant tumors of the proximal femur. Clin Orthop Relat Res. 1999;358:8–14. [PubMed] [Google Scholar]
- 5.McGoveran BM, Davis AM, Gross AE, Bell RS. Evaluation of the allograft-prosthesis composite technique for proximal femoral reconstruction after resection of a primary bone tumour. Can J Surg. 1999;42:37–45. [PMC free article] [PubMed] [Google Scholar]
- 6.Anract P, Coste J, Vastel L, Jeanrot C, Mascard E, Tomeno B. Proximal femoral reconstruction with megaprosthesis versus allograft prosthesis composite: A comparative study of functional results, complications and longevity in 41 cases. Rev Chir Orthop Reparatrice Appar Mot. 2000;86:278–88. [PubMed] [Google Scholar]
- 7.Donati D, Giacomini S, Gozzi E, Mercuri M. Proximal femur reconstruction by an allograft prosthesis composite. Clin Orthop Relat Res. 2002;394:192–200. doi: 10.1097/00003086-200201000-00023. [DOI] [PubMed] [Google Scholar]
- 8.Langlais F, Lambotte JC, Collin P, Thomazeau H. Long term results of allograft composite total hip prostheses for tumors. Clin Orthop Relat Res. 2003;414:197–211. doi: 10.1097/01.blo.0000079270.91782.23. [DOI] [PubMed] [Google Scholar]
- 9.Menendez LR, Ahlmann ER, Kermani C, Gotha H. Endoprosthetic reconstruction for neoplasms of the proximal femur. Clin Orthop Relat Res. 2006;450:46–51. doi: 10.1097/01.blo.0000229332.91158.05. [DOI] [PubMed] [Google Scholar]
- 10.Farid Y, Lin PP, Lewis VO, Yasko AW. Endoprosthetic and allograft-prosthetic composite reconstruction of the proximal femur for bone neoplasms. Clin Orthop Relat Res. 2006;442:223–9. doi: 10.1097/01.blo.0000181491.39048.fe. [DOI] [PubMed] [Google Scholar]
- 11.Finstein JL, King JJ, Fox EJ, Ogilvie CM, Lackman RD. Bipolar proximal femoral replacement prostheses for musculoskeletal neoplasms. Clin Orthop Relat Res. 2007;459:66–75. doi: 10.1097/BLO.0b013e31804f5474. [DOI] [PubMed] [Google Scholar]
- 12.Biau DJ, Larousserie F, Thévenin F, Piperno-Neumann S, Anract P. Results of 32 Allograft-prosthesis Composite Reconstructions of the Proximal Femur. Clin Orthop Relat Res. 2010;468:834–45. doi: 10.1007/s11999-009-1132-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Enneking WF, Dunham W, Gebhardt MC, Malawar M, Pritchard DJ. A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop. 1993;286:241–6. [PubMed] [Google Scholar]
- 14.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: Treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–55. [PubMed] [Google Scholar]
- 15.Head WC, Wagner RA, Emerson RH, Jr, Malinin TI. Revision total hip arthroplasty in the deficient femur with a proximal loaded bearing prosthesis. Clin Orthop Relat Res. 1994;298:119–26. [PubMed] [Google Scholar]
- 16.Gross AE, Hutchison CR, Alexeeff M, Mahomed N, Leitch K, Morsi E. Proximal femoral allografts for reconstruction of bone stock in revision arthroplasty of the hip. Clin Orthop Relat Res. 1995;319:151–8. [PubMed] [Google Scholar]
- 17.Selek H, Basarir K, Yildiz Y, Saglik Y. Cemented endoprosthetic replacement for metastatic bone disease in the proximal femur. J Arthroplasty. 2008;23:112–7. doi: 10.1016/j.arth.2006.11.016. [DOI] [PubMed] [Google Scholar]
- 18.Maclachlan CE, Ries MD. Intramedullary step-cut osteotomy for revision total hip arthroplasty with allograft host bone size mismatch. J Arthroplasty. 2007;22:657–62. doi: 10.1016/j.arth.2006.09.005. [DOI] [PubMed] [Google Scholar]
- 19.Lee SH, Ahn YJ, Chung SJ, Kim BK, Hwang JH. The use of allograft prosthesis composite for extensive proximal femoral bone deficiencies. A 2- to 9.8-year followup study. J Arthroplasty. 2009;24:1241–8. doi: 10.1016/j.arth.2009.06.006. [DOI] [PubMed] [Google Scholar]
- 20.Biau DJ, Davis A, Vastel L, Tomeno B, Anract P. Function, disability and health-related quality of life after allograft-prosthesis composite reconstructions of the proximal femur. J Surg Oncol. 2008;97:210–5. doi: 10.1002/jso.20936. [DOI] [PubMed] [Google Scholar]
- 21.Steinberg EL, Luger E, Zwas T, Katznelson A. Very long term radiographic and bone scan results of frozen autograft and allograft bone grafting in 17 patients (20 grafts): A 30- to 35- year followup. Cell Tissue Bank. 2004;5:97–104. doi: 10.1023/B:CATB.0000034084.27772.66. [DOI] [PubMed] [Google Scholar]
- 22.Finstein JL, King JJ, Fox EJ, Ogilvie CM, Lackman RD. Bipolar proximal femoral replacement prostheses for musculoskeletal neoplasms. Clin Orthop Relat Res. 2007;459:66–75. doi: 10.1097/BLO.0b013e31804f5474. [DOI] [PubMed] [Google Scholar]
- 23.Gross AE, Hutchison CR. Proximal femoral allografts for reconstruction of bone stock in revision hip arthroplasty. Orthopedics. 1998;21:999–1001. doi: 10.3928/0147-7447-19980901-23. [DOI] [PubMed] [Google Scholar]
- 24.Breusch SJ, Lukoschek M, Thomsen M, Mau H, Ewerbeck V, Aldinger PR. Ten-year results of an cemented hip stems for failed intertrochanteric osteotomy. Arch Orthop Trauma Surg. 2005;125:304–9. doi: 10.1007/s00402-005-0800-z. [DOI] [PubMed] [Google Scholar]
- 25.Götze C, Tschugunow A, Götze HG, Böttner F, Pötzl W, Gosheger G. Long term results of the metal-cancellous cementless Luberk total hip arthroplasty: A critical review at 12.8 years. Arch Orthop Trauma Surg. 2006;126:28–35. doi: 10.1007/s00402-005-0064-7. [DOI] [PubMed] [Google Scholar]


