Abstract
Background:
The purpose of this study was to compare the resistance of intramedullary single screw device (Gamma nail) and double screw device proximal femoral nail (PFN) in unstable trochanteric fractures in terms of the number of cycles sustained, subsidence and implant failure in an axial loading test in cadaveric femora.
Materials and Methods:
The study was conducted on 18 dry cadaveric femoral specimens, 9 of these were implanted with a Gamma nail and 9 with PFN. There was no significant difference found in average dual energy X-ray absorptiometry value between both groups. The construct was made unstable (AO type 31A3.3) by removing a standard sized posteromedial wedge. These were tested on a cyclic physiological loading machine at 1 cycle/s with a load of 200 kg. The test was observed for 50,000 loading cycles or until implant failure, whichever occurred earlier. Peak displacements were measured and analysis was done to determine construct stiffness and gap micromotion in axial loading.
Result:
It was observed that there was statistically significant difference in terms of displacement at the fracture gap and overall construct stiffness of specimens of both groups. PFN construct group showed a mean subsidence of 1.02 mm and Gamma nail construct group showed mean subsidence of 2.36 mm after cycling. The average stiffness of Gamma nail group was 62.8 ± 8.4 N/mm which was significantly lower than average stiffness of the PFN group (80.4 ± 5.9 N/mm) (P = 0.03). In fatigue testing, 1 out of 9 PFN bone construct failed, while 5 of 9 Gamma nail bone construct failed.
Conclusion:
When considering micromotion (subsidence) and incidence of implant/screw failure, double screw device (PFN) had statistically significant lower micromotion across the fracture gap with axial compression and lower incidence of implant failure. Hence, double screw device (PFN) construct had higher stability compared to single screw device (GN) in an unstable trochanteric fracture femur model.
Keywords: Cyclic loading, Gamma nail, proximal femoral nail, subsidence
INTRODUCTION
Trochanteric femoral fractures are very common in elderly patients. The unstable fracture (AO 31A2 and 31A3) is usually difficult to manage with implant failure and other complications being relatively common. Conservative treatment of such injuries is also not without serious complications. Clinical success has been reported with operative treatment of these fractures and is preferred over nonoperative treatment. Treatment goals are to restore axial alignment, anatomic reduction of fracture fragments, early weight bearing, with minimal soft tissue disruption.
There are large number of devices available for surgical fixation of trochanteric fractures. They can be divided into two broad groups namely; extra medullary and intramedullary devices.1 The extra medullary device are the dynamic hip screw (DHS), dynamic condylar screw and the angled blade plate. The common intramedullary devices used are intramedullary hip screw, like proximal femoral nail (PFN) and Gamma nail and Ender's nail.2 Until recently, most of these fractures were treated by a sliding hip screw system. Since this device performed less well in unstable trochanteric fracture with a high rate of failure, intramedullary fixation devices have become increasingly popular.3 Two varieties of intramedullary nail are available one with single proximal screw and other with double screw.4,5 Both permit medialization. Medialization improves the success rate, but may also leads to shortening. Excessive medialization, implant failure and explantation difficulties (backing out of screw) are more likely in single screw intramedullary nails.6,7
This biomechanical cadaveric study was performed to compare the fixation stability of a PFN with Gamma nail in simulated proximal femur 31 A3-3 fractures. In this study, we aim to establish modes of failure for each device tested and to correlate these with the commonly seen fracture patterns in vivo especially those which are clinically proven to be prone to implant failure.
MATERIALS AND METHODS
This research study was approved by the ethical committee and the institutional review board. Power analysis was performed to decide the required sample size which was 9 for each group. Some other studies in the literature have used the same sample size. Nine pairs of dry human cadaveric femora were selected. Dual energy X-ray absorptiometry (DEXA) was used to assess the quality of each cadaveric specimen [Tables 1 and 2]. All the specimens were randomized in two groups and implanted with either a PFN or a Gamma nail. Nine of them were implanted with Gamma nail [Figure 1] and 9 with PFN [Figure 2]. Fixation was done under image intensification. Fresh implants of the same size and same manufacturer (Yogeshwar private limited, Mumbai, India), made of stainless steel were used and these implants were FDA (Food and Drug Administration) certified.
Table 1.
DEXA for measure of bone quality in both PFN and Gamma nail group
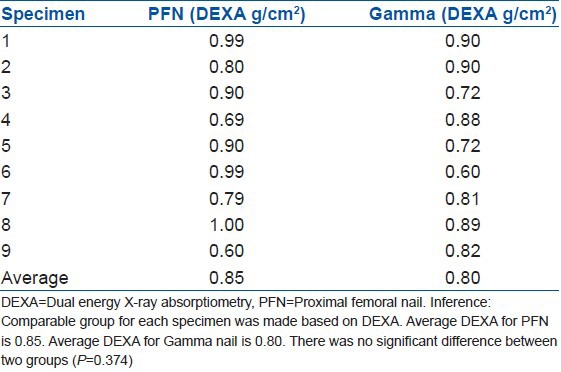
Table 2.
Comparison of bone mineral density of both the groups
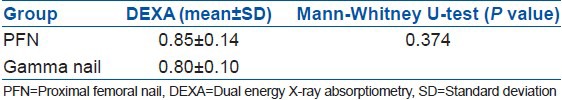
Figure 1.
Fluoroscopic view showing specimen of cadaveric femur fixed with Gamma nail and made unstable after creating posteromedial defect. This bone implant construct is mounted on MTS machine and tested with 200 kg load and 50,000 cycles
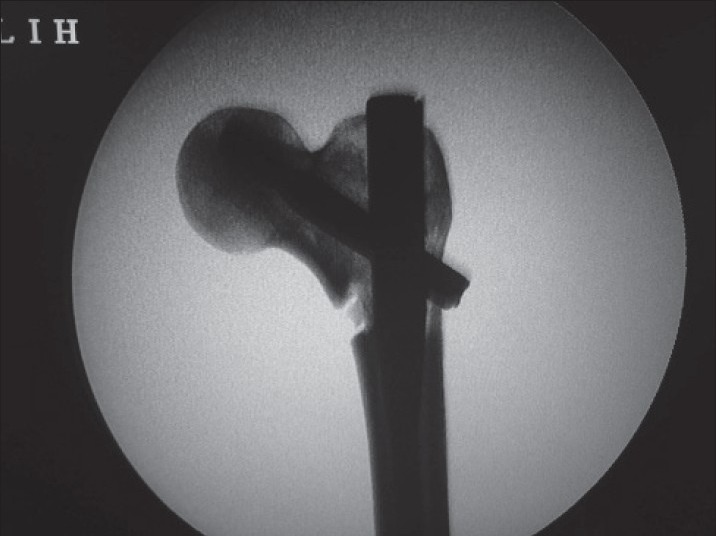
Figure 2.

Fluoroscopic view showing specimen of cadaveric femur fixed with PFN and made unstable after creating posteromedial defect. This bone implant construct is mounted on MTS machine and tested with 200 kg load and 50,000 cycles
Standard techniques described in AO manual of internal fixation were followed to implant the Gamma nail and the PFN in the cadaveric femora. The construct was made unstable (AO type 31A3.3) by removing a standard sized posteromedial wedge at the level of the lesser trochanter (gap-osteotomy) to simulate loss of medial buttress in all the femoral specimens with the help of a standard cutting jig The implants were mounted in such a way that they represented the normal anatomic loading conditions of the hip in stance, phase.
After the fixation images were critically analyzed. Those specimens which failed to obey the standard norms were removed from the study. Tip apex distance was kept constant to 25 mm for each specimen.
Cyclic loading test and fatigue test of the implanted specimens was conducted using a computer controlled servo-hydraulic materials testing system (MTS) testing machine (modal 810) of ±50 KN capacity. The specimens were cut at the midshaft and mounted on the base which was designed to fix the shaft of the femur, which was done using cement to reinforce the construct.
The upper portion of the MTS was used to give cyclic load to the femoral construct. Tests were conducted under load control made in compression at a frequency of 1 Hz using a triangular wave form. Each construct was subjected to a cyclic loading of 2 kN, for 50,000 cycles or until failure/cut out, which ever occurred earlier. 2 kN loading was chosen to simulate single leg stance phase in a young adult of a 70 kg weight (700 N). We attempted to simulate the forces and stresses the construct would be subjected to during regular walking. It was suggested that testing for 10,000-20,000 cycles simulates 2-6 months of in vivo cyclic loading of the femur.8,9 We have arbitrarily chosen 50000 cycles for our study. similar to those by other authors described in literature.10,11
All tested constructs were checked for implant bending, fracture, screw bending and screw back-out. Deformation in the implant seen by the naked eye was considered as macroscopic deformation and radiological comparison was made to look for any subtle changes (microscopic deformation). After the specimens were cycled, postcycling osteotomy gap displacement (subsidence) with preload was again measured. Subsidence was defined as “the difference between the displacement measured with preload applied, before cyclic loading and the displacement measured with preload applied, after cyclic loading”. Subsidence was measured with a direct measuring device (verniers calipers).
Statistical analysis
All the statistical analyses were performed using InStat software for windows (GraphPad version 3.00, SanDiego, California, USA). Fisher's exact test and Mann-Whitney U-test were used to analyze the difference of mean for bone mineral density, number of cycles sustained, subsidence and stiffness of the constructs. The test was referenced for two-tailed P value and 95% confidence interval was constructed around sensitivity proportion using a normal approximation method. P < 0.05 was considered to be statistically significant.
RESULTS
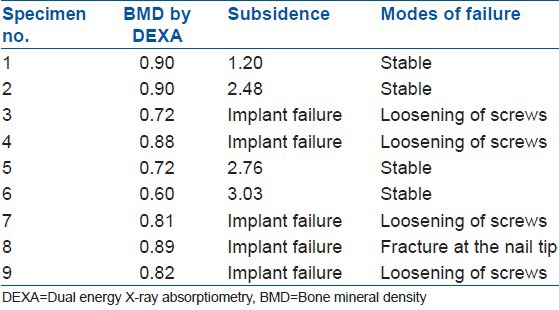
In PFN group, one implant failed and the remaining 8 specimens were stable [Figure 3] after sustained 50,000 cycles [Tables 3 and 4]. Four out of 9 specimens completed 50,000 cycles and five constructs failed [Figures 4 and 5] in the Gamma nail group [Tables 5 and 6]. There was a significant difference found between both the groups (P = 0.046). Though the bone quality as assessed by DEXA was comparable in both PFN (0.85 ± 0.10) and the Gamma nail group (0.80 ± 0.10); (P = 0.374), subsidence was 1.02 ± 0.34 mm (range, 0.62-1.60 mm) which was 56.78% lower (P = 0.027) than subsidence in the Gamma nail group (2.36 ± 0.81; range, 1.20-3.03 mm) [Tables 7-9]. The average number of cycles sustained by Gamma nail (38700 ± 10816.65) was significantly lower (P = 0.031) than the average number of cycles sustained by the PFN (49100 ± 2666.66) [Table 10]. In the PFN group, one construct failed at 40,000 cycles with back out of both the screws. In the Gamma nail group, five constructs failed [Table 11]. Mode of failure in two of these was lag screw loosening. One construct failed due to the breakage of lag screw and one because of fracture at the nail tip. One more construct in the Gamma nail group failed due to screw loosening and screw bending of 15°. The average stiffness of the Gamma nail group was 62.8 ± 8.4 N/mm which was significantly lower than the average stiffness of the PFN group (80.4 ± 5.9 N/mm) (P = 0.03).
Figure 3.
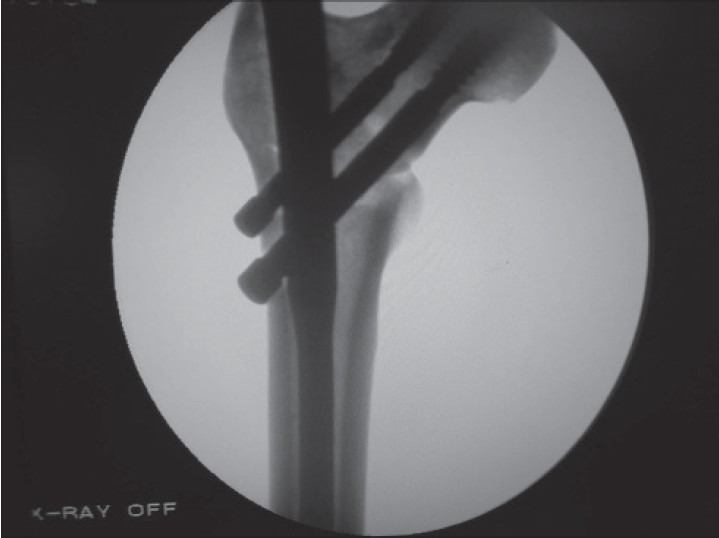
Fluoroscopic view showing this bone implant constuct fixed with pfn remained stable after testing for 50,000 cycles with a load of 200 kg.this shows pfn(double screw device) provide greater fixation stability and minimal subsidence.there is no migration of screws
Table 3.
Observations of PFN group for number of cycles sustained and modes of failure
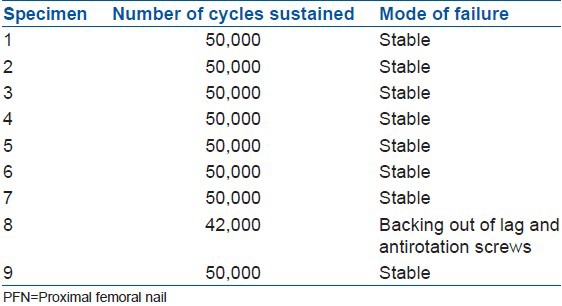
Table 4.
Observations of PFN group for bone mineral density and modes of failure
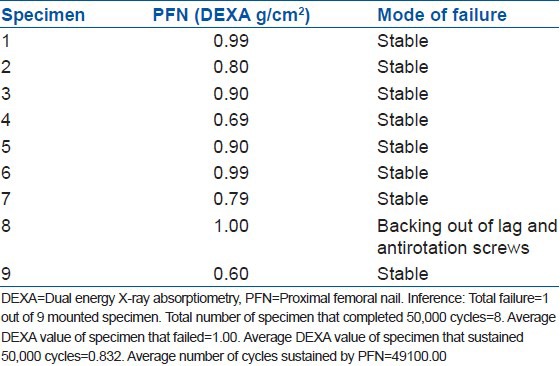
Figure 4.

Fluoroscopic view showing this bone implant constuct fixed with Gamma nail showed backing out of lag screw after 28,000 cycles.there is also displacement at the fracture site suggesting increased subsidence.this concludes Gamma nail is less stable in comparison to Gamma nail in unstable trochanteric fractures
Figure 5.

Fluoroscopic view showing this bone implant constuct fixed with Gamma nail showed backing out of lag screw after 28,000 cycles.there is also displacement at the fracture site suggesting increased subsidence.this concludes Gamma nail is less stable in comparison to Gamma nail in unstable trochanteric fractures
Table 5.
Observations of Gamma nail group for number of cycles sustained and modes of failure
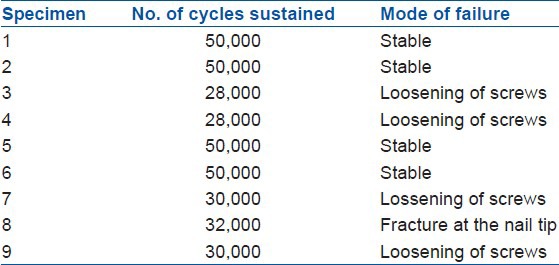
Table 6.
Correlation of bone quality and mode of failure in Gamma nail group
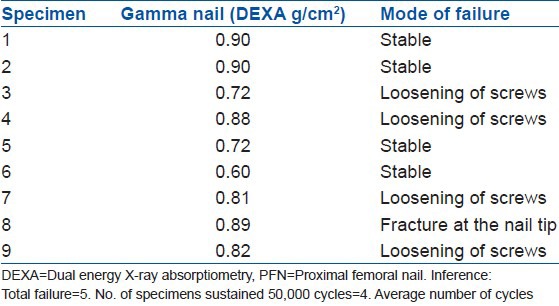
Table 7.
Correlation of bone quality and subsidence with mode of failure in PFN group
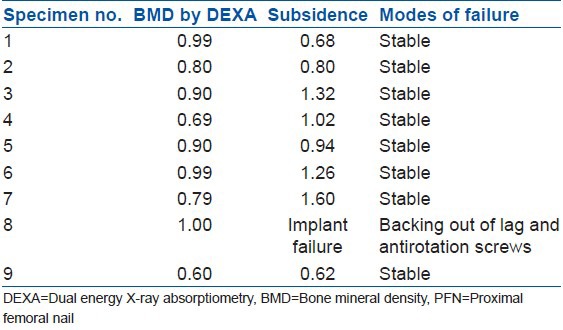
Table 9.
Correlation and calculation of subsidence
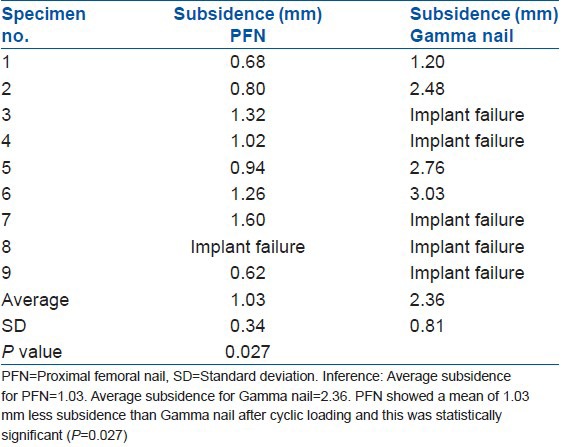
Table 10.
Comparison of average number of cycles completed in both the groups
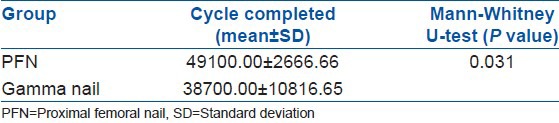
Table 11.
Comparison of specimens of PFN and Gamma nail group
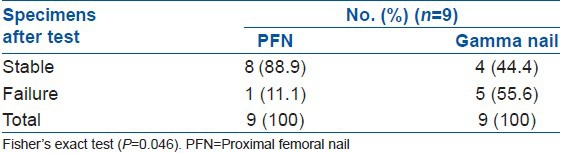
Table 8.
Correlation of bone quality and subsidence with modes of failure in Gamma nail group
DISCUSSION
Hip fractures in the elderly are frequent.12 Intertrochanteric hip fractures account for approximately half of all hip fractures in the elderly.12 Unstable fracture pattern occurs more commonly with increased age and low bone mineral density.13 The unstable fracture (fracture 31-A2 and 31-A3, AO/ASIF classification) can be difficult to manage, particularly in the noncompliant patients with implant failure.14 Because unstable fractures have a greater bony injury, greater displacement after fixation is expected. Until recently, most of these fractures were treated by a sliding hip screw system. Since this device performed less well in an unstable trochanteric fracture with a high rate of failure, intramedullary fixation devices have become increasingly popular.3 The PFN was developed to improve the rotational stability of the proximal fracture fragment, combining the features of an unreamed intramedullary femoral nail with a sliding, load bearing femoral neck screw.11 Furthermore, the tip of the nail was redesigned to decrease the risk of intra and postoperative fractures of the femoral shaft by a significant reduction in the bone stress.
Two implants the Gamma nail and the PFN have shown to provide a biomechanically stable construct allowing early weight bearing with low complication rates.4 PFN provides adequate axial and rotational stability because of the presence of two screws.15 The antirotation screw prevents rotation of the proximal fragment and the lag screw achieves compression at the fracture site. In the standard PFN, the amount of the total load carried by the hip pin varics between 8% and 39%. The nonconstrained lateral end of the hip pin reduces the bending load applied to the implant. Hip pin also allows the femur and nail to medialize. The prevalence of cutout has been reduced by this mechanism. The tip of the nail is designed in such a way that it distributes the load equally in the medullary canal. So, the incidence of fracture shaft of the femur is less. PFN achieves a valgus reduction, which is a reasonable alternative to anatomic reduction in unstable fracture patterns. The valgus reduction of the fracture decreases the bending forces on the implant by decreasing the neck shaft off set and the more vertical orientation of the neck tends to offset some of the shortening expected with an unstable fracture. Finally positioning of the fragment into valgus, reorients the fracture plane so that it is more perpendicular to the weight bearing load vector and thus more favorably positioned for interfragmentary compression.
Gamma nail has been available since 1988 and was designed specifically for the fixation of trochanteric fractures. It has the advantage of using a semi-closed technique, a dynamic femoral neck screw and early postoperative weight bearing. It has one lag screw which is along the weight bearing axis. It does not have an antirotation screw for the prevention of rotation, so cut through, migration etc., of gamma nail is relatively more common. Gamma nail does not prevent varus collapse, thus complications like proximal migration of the implant and resultant shortening is more likely. This explains the displacement at the fracture site in fractures fixed with Gamma nail. The hold and purchase of any screw in the bone is a combination of screw design and rigidity of the host bone. As such osteoporotic bone stock would theoretically has poor purchase with the same screw as compared to normal bones. So, DEXA was used to classify bone quality of the specimens used. In our study, there was no significant difference between both groups in terms of DEXA value of specimens which were nearly normal so it will not affect the outcome.
Various authors had compared Gamma nail to other extra medullary and intramedullary devices in cadaveric studies.16,17,18,19 Mahomed et al. compared Gamma nail and sliding hip screw in trochanteric fractures fixation and reported insignificant difference in structural stiffness for stable intertrochanteric fractures.16 Both implants effectively unloaded the proximal medial cortex. The Gamma nail does not appear to offer any distinct biomechanical advantage over the sliding hip screw system in the treatment of stable and unstable intertrochanteric fractures. Curtis et al. studied the rigidity and strength of fixation provided by intramedullary and extra medullary devices for proximal femoral fractures.17 Stable and unstable intertrochanteric fractures were studied in paired femora after internal fixation with the Gamma nail and Richards 135° classic hip-screw implants. There was no significant difference in the strength of fixation of stable and unstable intertrochanteric fractures between the Gamma nail and the hip screw, although the Gamma nail provided more rigid fixation. Haynes et al. in their study investigated the resistance to failure of the femoral head, with lag screws used in two types of sliding hip screws, the Gamma nail and DHS.18 The investigation consisted of biomechanical tests under static loading conditions on 12 pairs of cadaveric femoral heads, to establish the failure loads due to screw cut-out for the two implant lag screws. The Gamma nail appeared to reduce the tendency to cut-out in the osteoporotic bone. In high density bone (hard) the Gamma lag screw also appeared to be stronger, because the DHS showed a tendency to bend. The larger diameter of the Gamma nail lag screw resists bending and appears to reduce the risk of cut-out compared with the DHS.
This study aims to combine all the factors namely subsidence, osteoporosis and loading the construct to stimulate physiological weight bearing and study the modes of failure and stability after 50,000 cycles. This experiment did not demonstrate any significant difference in the bone density of the specimens in the two groups studied. Out of 9 PFN specimens, 1 failed before completing 50,000 cycles while the remaining 8 were stable. Out of 9 Gamma nail specimens, 5 failed before completing 50,000 cycles. The cause of failure varied in different specimens from loosening of the screws to fracture at the nail tip.
The limitations to our experiment lie in study design and are: The cadaveric nature of this study is a limitation. There is no accounting for the soft-tissue envelope or bone healing (2). All the implant bone construct were tested with axial compression for stiffness measurement and displacement across the fracture site as well as for cyclic fatigue. Other modes of loading such as stair ascent and descent and the torsional loading were not tested as those kinds of loading and movement are not expected during the early postoperative period.8
Our study comparing the fixation of the PFN to the Gamma nail in a cadaveric model of a femur did demonstrate a significant difference in postcycling subsidence between the 2 constructs. It is universally found that higher subsidence leads to early failure of implant bone construct. PFN showed a mean of 1.02 mm subsidence while the Gamma nail showed a mean of 2.367 mm after cycling and this difference was statistically significant. In this study, the average subsidence was about 56% higher in Gamma nail group in comparison to PFN group, as a result, only 4 Gamma nail construct remained stable and completed 50,000 cycles.
Footnotes
Source of Support: Nil.
Conflict of Interest: None.
REFERENCES
- 1.Friedl W, Clausen J. Experimental examination for optimized stabilisation of trochanteric femur fractures, intra or extra medullary implant localisation and influence of femur neck component profile on cut-out risk. Chirurg. 2001;72:1344–52. doi: 10.1007/s001040170041. [DOI] [PubMed] [Google Scholar]
- 2.Baumgaertner MR, Curtin SL, Lindskog DM. Intramedullary versus extra medullary fixation for the treatment of intertrochanteric hip fractures. Clin Orthop Relat Res. 1998;348:87–94. [PubMed] [Google Scholar]
- 3.Buciuto R, Hammer R. RAB-plate versus sliding hip screw for unstable trochanteric hip fractures: Stability of the fixation and modes of failure: Radiographic analysis of 218 fractures. J Trauma. 2001;50:545–50. doi: 10.1097/00005373-200103000-00022. [DOI] [PubMed] [Google Scholar]
- 4.Xu Y, Geng D, Yang H, Wang X, Zhu G. Treatment of unstable proximal femoral fractures: Comparison of the proximal femoral nail antirotation and Gamma nail 3. Orthopedics. 2010;33:473. doi: 10.3928/01477447-20100526-03. [DOI] [PubMed] [Google Scholar]
- 5.Adams CI, Robinson CM, Court-Brown CM, McQueen MM. Prospective randomized controlled trial of an intramedullary nail versus dynamic screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma. 2001;15:394–400. doi: 10.1097/00005131-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Albareda J, Laderiga A, Palanca D, Paniagua L, Seral F. Complications and technical problems with the Gamma nail. Int Orthop. 1996;20:47–50. doi: 10.1007/s002640050026. [DOI] [PubMed] [Google Scholar]
- 7.Gaebler C, Stanzl-Tschegg S, Tschegg EK, Kukla C, Menth-Chiari WA, Wozasek GE, et al. Implant failure of the Gamma nail. Injury. 1999;30:91–9. doi: 10.1016/s0020-1383(98)00215-0. [DOI] [PubMed] [Google Scholar]
- 8.Koval KJ, Hoehl JJ, Kummer FJ, Simon JA. Distal femoral fixation: A biomechanical comparison of the standard condylar buttress plate, a locked buttress plate, and the 95-degree blade plate. J Orthop Trauma. 1997;11:521–4. doi: 10.1097/00005131-199710000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Heiney JP, Barnett MD, Vrabec GA, Schoenfeld AJ, Baji A, Njus GO. Distal femoral fixation: A biomechanical comparison of trigen retrograde intramedullary (i.m) nail, dynamic condylar screw (DCS), and locking compression plate (LCP) condylar plate (LCP) condylar plate. J Trauma. 2009;66:443–9. doi: 10.1097/TA.0b013e31815edeb8. [DOI] [PubMed] [Google Scholar]
- 10.Strauss EJ, Kummer FJ, Koval KJ, Egol KA. The “Z-effect” phenomenon defined: A laboratory study. J Orthop Res. 2007;25:1568–73. doi: 10.1002/jor.20457. [DOI] [PubMed] [Google Scholar]
- 11.Cheema GS, Rastogi A, Singh V, Goel SC, Mishra D, Arora S. Comparison of cutout resistance of dynamic condylar screw and proximal femoral nail in reverse oblique trochanteric fractures: A biomechanical study. Indian J Orthop. 2012;46:259–65. doi: 10.4103/0019-5413.96369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Thorngren KG, Norrman PO, Hommel A, Cedervall M, Thorngren J, Wingstrand H. Influence of age, sex, fracture type and prefracture living on rehabilitation pattern after hip fracture in the elderly. Disabil Rehabil. 2005;27:1091–7. doi: 10.1080/09638280500056402. [DOI] [PubMed] [Google Scholar]
- 13.Zain Elabdien BS, Olerud S, Karlström G. The influence of age on the morphology of trochanteric fracture. Arch Orthop Trauma Surg. 1984;103:156–61. doi: 10.1007/BF00435546. [DOI] [PubMed] [Google Scholar]
- 14.Medoff RJ, Maes K. A new device for the fixation of unstable pertrochanteric fractures of the hip. J Bone Joint Surg Am. 1991;73:1192–9. [PubMed] [Google Scholar]
- 15.Al-yassari G, Langstaff RJ, Jones JW, Al-Lami M. The AO/ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fracture. Injury. 2002;33:395–9. doi: 10.1016/s0020-1383(02)00008-6. [DOI] [PubMed] [Google Scholar]
- 16.Mahomed N, Harrington I, Kellam J, Maistrelli G, Hearn T, Vroemen J. Biomechanical analysis of the Gamma nail and sliding hip screw. Clin Orthop Relat Res. 1994;304:280–8. [PubMed] [Google Scholar]
- 17.Curtis MJ, Jinnah RH, Wilson V, Cunningham BW. Proximal femoral fractures: A biomechanical study to compare intramedullary and extra medullary fixation. Injury. 1994;25:99–104. doi: 10.1016/0020-1383(94)90111-2. [DOI] [PubMed] [Google Scholar]
- 18.Haynes RC, Pöll RG, Miles AW, Weston RB. Failure of femoral head fixation: A cadaveric analysis of lag screw cut-out with the Gamma locking nail and AO dynamic hip screw. Injury. 1997;28:337–41. doi: 10.1016/s0020-1383(97)00035-1. [DOI] [PubMed] [Google Scholar]
- 19.Rosenblum SF, Zuckerman JD, Kummer FJ, Tam BS. A biomechanical evaluation of the Gamma nail. J Bone Joint Surg Br. 1992;74:352–7. doi: 10.1302/0301-620X.74B3.1587875. [DOI] [PubMed] [Google Scholar]


