Abstract
The advent of effective combination antiretroviral therapy (ART) in 1996 resulted in fewer patients experiencing clinical events, so that some prognostic analyses of individual cohort studies of human immunodeficiency virus-infected individuals had low statistical power. Because of this, the Antiretroviral Therapy Cohort Collaboration (ART-CC) of HIV cohort studies in Europe and North America was established in 2000, with the aim of studying the prognosis for clinical events in acquired immune deficiency syndrome (AIDS) and the mortality of adult patients treated for HIV-1 infection. In 2002, the ART-CC collected data on more than 12,000 patients in 13 cohorts who had begun combination ART between 1995 and 2001. Subsequent updates took place in 2004, 2006, 2008, and 2010. The ART-CC data base now includes data on more than 70 000 patients participating in 19 cohorts who began treatment before the end of 2009. Data are collected on patient demographics (e.g. sex, age, assumed transmission group, race/ethnicity, geographical origin), HIV biomarkers (e.g. CD4 cell count, plasma viral load of HIV-1), ART regimen, dates and types of AIDS events, and dates and causes of death. In recent years, additional data on co-infections such as hepatitis C; risk factors such as smoking, alcohol and drug use; non-HIV biomarkers such as haemoglobin and liver enzymes; and adherence to ART have been collected whenever available. The data remain the property of the contributing cohorts, whose representatives manage the ART-CC via the steering committee of the Collaboration. External collaboration is welcomed. Details of contacts are given on the ART-CC website (www.art-cohort-collaboration.org).
Keywords: HIV, AIDS, cohort study, antiretroviral therapy, prognosis
Why was the cohort set up?
The Antiretroviral Therapy Cohort Collaboration (ART-CC) was established in 2000 to study the prognosis for adult patients treated for human immunodeficiency virus-1 (HIV-1) infection in Europe and North America. The widespread use since 1996 of combination antiretroviral therapy (ART) has substantially improved the prognosis for HIV-positive patients as compared with those treated with previously available drug regimens of nucleoside reverse transcriptase inhibitors (NRTIs), either in the form of monotherapy with zidovudine or as dual therapy with a second NRTI.1
The substantial reductions in the number of events and deaths related to acquired immune deficiency syndrome (AIDS) following the introduction of combination ART meant that modelling of prognosis among different patient groups and according to different prognostic factors often required larger numbers of patients than were available in individual cohorts at that time. Therefore, the important task of defining prognosis and prognostic factors in the era of combination ART required several cohorts to contribute data to a collaborative data base. The prognosis for patients starting treatment with combination ART, defined as a combination of at least three drugs belonging to two different classes of drugs, depends on their prior exposure to NRTI monotherapy or dual therapy, because the development of resistance to NRTI drugs as a result of incomplete viral suppression meant that ‘treatment-naive’ patients who had not previously been treated when they began triple ART had a better prognosis. Because future patients would begin treatment with triple ART rather than with NRTIs, treating physicians and their patients needed to know the prognosis for treatment-naïve patients starting combination ART according to their demographic characteristics, disease stage, and treatment options. The ART-CC was able to address this key clinical question and thereby improve care for HIV-positive patients.
The co-ordinating centre of the ART-CC was established in the Department of Social Medicine (now the School of Social and Community Medicine) of the University of Bristol, UK. An annual international workshop for researchers working with observational cohorts of HIV-positive patients had been set up in 1997, under the sponsorship of the pharmaceutical company GlaxoSmithKline. At the fourth such workshop, held in 2000 in Marbella, 16 cohorts, in Europe and North America, were approached, and 13 agreed to participate in the collaboration. The ART-CC Steering Committee consists of the Principal Investigator, a representative from each cohort, the co-ordinating team and representatives of patient groups. GlaxoSmithKline funded the first 6 months of the study, and it has since been funded by the UK Medical Research Council together with the fund providers for the contributing cohorts (see Appendix). The aim of the ART-CC, as specified in its detailed Principles of Collaboration, is ‘to examine the prognosis of HIV-infected, antiretroviral drug-naïve patients starting combination ART, with a focus on questions that cannot be fully addressed in analyses of data from individual cohorts. In particular, analyses will focus on prognosis of major clinical events (particularly AIDS, AIDS-defining conditions, and all-cause and cause-specific mortality).’
Which cohorts contribute to the collaboration?
The ART-CC is a collaboration of HIV cohort studies in Europe and North America. Table 1 lists the cohorts that have contributed data to the ART-CC. Prospective cohort studies are eligible to participate if they have enrolled at least 100 HIV-1–positive patients aged 16 years or older who have not previously received antiretroviral treatment, who began ART with a combination of at least three antiretroviral drugs after 1996, and who have been followed for a median of at least 1 year after the initiation of ART. Patients are eligible only if they have had at least one measurement of their CD4 cell count and plasma viral load of HIV-1 RNA within 3 months before starting ART. All cohorts have been approved by local ethics committees or institutional review boards, use standardised methods of data collection, and schedule follow-up visits at least once every 6 months for their patients.
Table 1.
Description of cohorts in the Antiretroviral Therapy Cohort Collaborative
| Cohort | Cohort established | Joined ART-CC | Coverage and facilities | Representativeness |
|---|---|---|---|---|
| European | ||||
| AIDS Therapy Evaluation Project (ATHENA), Netherlands | 1998 | 2001 | Provides 100% of national coverage. Facilities are entirely hospital-based. | Reported to be representative of the country. |
| ANRS CO3 Aquitaine, France | 1998 | 2001 | Provides 90% of provincial coverage. Facilities are entirely hospital-based. | Reported to be representative of the south-western part of France. |
| Köln/Bonn cohort, Germany | 1997 | 2001 | Two cities: Köln and Bonn. Facilities are entirely hospital-based. | Reported to be representative of the country. |
| Cohorte de la Red de Investigación en Sida (CoRIS), Spain | 2004 | 2008 | Provides 35% of national coverage. Facilities are entirely hospital-based except for one facility. | Reported to be representative of the country. |
| EuroSIDA Study Group | 1994 | 2001 | A multi-national cohort. Because this in many cases consists of university-based clinics in the capitals of the countries involved, EuroSIDA probably reflects the gold standard of management in participating countries. | Representative for the clinics included in the study. |
| ANRS CO4 French Hospital Database on HIV (FHDH) | 1989 | 2001 | Provides 57% of national coverage. Facilities are entirely hospital-based. | Reported to be largely representative of patients under care in the country. Includes French overseas territories |
| Frankfurt, Germany | 1988 | 2001 | One city: Frankfurt. Facilities are entirely hospital-based. | Reported to be largely representative of the country, but over-representative of women. |
| Italian Cohort of Antiretroviral-Naive Patients (ICONA), Italy | 1997 | 2001 | 100% regional coverage. Facilities are entirely hospital-based. | Reported to be representative of all Italy. |
| Proyecto para la Informatización del Seguimiento Clínico-epidemiológico de la Infección por HIV y SIDA (PISCIS) Cohort, Spain | 2000 | 2006 | Provides 66% coverage of Catalonia and 80% coverage of of Balearic Islands. Facilities are entirely hospital-based. | Is not reported to be representative of the country, but aims to reach representativeness at regional level by 2013. |
| Royal Free Hospital Cohort, London, UK | 1989 | 2001 | One city hospital. Facilities are entirely hospital-based. | Is not reported to be representative of the country, but somewhat over-representative of men and people of white ethnicity. |
| Swiss HIV Cohort Study (SHCS), Switzerland | 1988 | 2001 | Provides 73% of national coverage. Facilities are entirely hospital-based. Patients are followed by hospital-based clinics and private physicians. | Is not reported to be representative of the country, but under-representative of those of sub-Saharan African ethnicity and of IDUs. |
| North American | ||||
| South Alberta Clinic Cohort, Canada | 1989 | 2001 | Provides 50% of provincial coverage. Facilities are entirely community based. | Is not representative of the country, but representative of the province and over-representative of those of African/north American aboriginal ethnicity. |
| HAART Observational Medical Evaluation and Research (HOMER), British Columbia, Canada | 1996 | 2001 | Provides 99% of provincial coverage. Facilities are hospital and community-based. | Is representative of BC since it is a census of everyone on ART, but over-representative of those of Aboriginal ethnicity and IDUs compared with Canada overall. |
| HIV Atlanta Veterans Affairs Cohort Study (HAVACS), USA | 1982 | 2008 | Veterans in one city. Facilities are entirely hospital-based. | Is not reported to be representative of the country, but over-representative of men, older patients, those of black ethnicity and those who abuse alcohol. |
| University Alabama, Birmingham (UAB), USA | 1992 | 2006 | One city hospital. Facilities are entirely hospital-based. | Reported to be largely representative of the country, but over-representative of those of black ethnicity and under-representative of Latinos and Hispanics. |
| Veterans Aging Cohort Study (VACS), USA | 1997 | 2008 | Veterans database. Facilities are hospital and community-based. | Is not reported to be representative of the country, but over-representative of men and older patients. |
| Vanderbilt-Meharry Center for AIDS Research, Nashville, Tennessee, USA | 1994 | 2008 | Regional. Facilities are entirely community based. | Is representative of HIV demographic in USA with 35-40% African- American ethnicity. |
| University of Washington HIV Cohort, Seattle, USA | 1995 | 2006 | Facilities are hospital and community based. | Is representative of the Northwestern USA. |
*Cohorts that joined ART-CC and have since dropped out: ANRS CO 8 APROCO, France, Collaborations in HIV Outcomes Research-US (CHORUS) cohort, USA and VACH, Spain. IDU Injection drug use; ANRS Agence Nationale de la Recherches sur le SIDA et les hépatites virales.
Abbreviations: AIDS, acquired immune deficiency syndrome; ATHENA, AIDS Therapy Evaluation Project Netherlands; HAART, highly active antiretroviral therapy; SIDA, síndrome de inmunodeficiencia adquirida; UAB, University of Alabama at Birmingham.
Who are the participants in the cohorts?
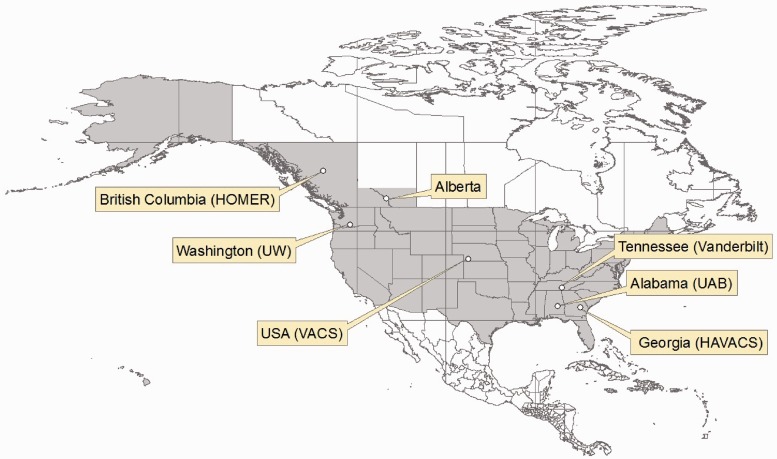
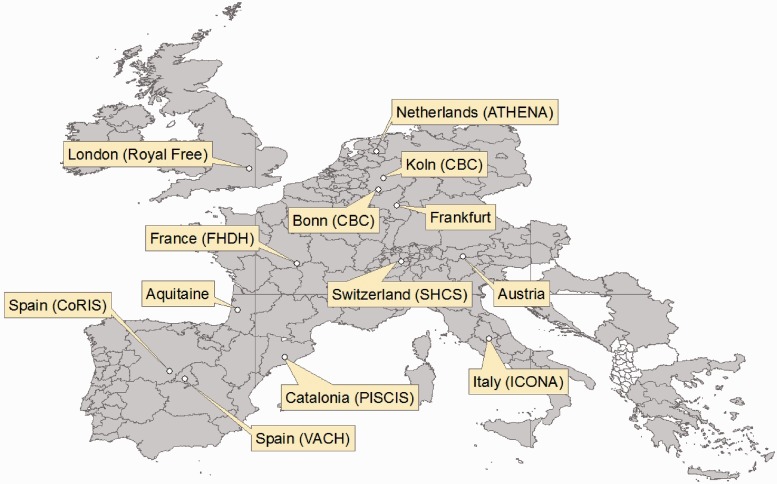
Each cohort in the ART-CC recruits patients in different ways, and the cohorts therefore differ in how representative they are of their local HIV-positive and treated populations. Only a few cohorts, such as the Swiss HIV Cohort Study (SHCS), estimate the rate of response to requests for participation. For example, the ANRS CO4 French Hospital Database on HIV (FHDH), together with the ANRS C03 Aquitaine Cohort, are likely to be fairly representative of the French HIV-positive population in whom a diagnosis has been made and who are in care. However, the Veterans Aging Cohort Study (VACS) includes only veterans of the US armed forces and is therefore not representative of the HIV-positive population of the US. Table 1 provides details of the cohorts in the ART-CC, including the ways in which their patients are recruited and whether they consider their participants to be representative of HIV positive people in their region or country. A strength of the ART-CC is that most participating cohorts recruit patients who are in usual clinical care for HIV infection in a particular geographic setting, as opposed to subjects specifically recruited for the purpose of an epidemiological study, such as a randomised controlled trial. Figures 1 and 2 show maps indicating the sites of cohorts that contribute to the ART-CC.
Figure 1.
Map of North American cohorts in the Antiretroviral Therapy Cohort Collaboration
Figure 2.
Map of European cohorts in the Antiretroviral Therapy Cohort Collaboration
EuroSIDA covers 31 European countries plus Israel and Argentina; the Infección por HIV y SIDA (PISCIS) Cohort includes two regions: Catalonia and the Balearic Islands
How often has the database been updated?
The ART-CC database is updated approximately every 2 years. A protocol is written for the data extraction for each update; it specifies names and descriptions of variables collected, eligibility criteria, and coding tables for opportunistic infections and antiretroviral drugs. The ART-CC data base has used the HIV Cohorts Data Exchange Protocol (HICDEP: www.hicdep.org) since 2008. The first ART-CC database was compiled in 2001 and included 13 cohorts that contributed information on 12 574 patients. In 2004 the update collected longer follow-up data on existing patients as well as data on new patients who had started treatment in more recent years. Table 2 provides further information about updates in 2006, 2008, and 2010, including the number of cohorts and patients in each data set. The 2012 update is currently under way.
Table 2.
Measurements collected at each data update in the Antiretroviral Therapy Cohort Collaboration
| Update | Cohorts N | Patients N | Data collected |
|---|---|---|---|
| 2001 | 13 | 12 574 | Demographic variables: age, sex, risk factors for transmission |
| Laboratory variables: CD4 cell counts and viral loads at start of ART and at 6 months | |||
| Clinical variables: ART start date, ART drug regimen at baseline, CDC disease stage at start of ART | |||
| Outcome variables: AIDS events, last visit date, death, death date | |||
| 2004 | 12 | 22 217 | As above |
| 2006 | 15 | 49 040 | As above, plus: Demographic variables: Race/ethnicity, geographical origin based on country of birth, nationality |
| Laboratory variables: CD4 cell count closest to event/death and last count during treatment, with dates. At least one 3-year measurement of each prognostic variable (CD4 cell count, HIV-1 RNA plasma viral load, haemoglobin), with dates and an indicator variable for being on/off treatment, and whether patient experienced virological failure (defined as an a viral load of > 500 during treatment) after 6 months and within 3 years of initiating treatment | |||
| Clinical variables: Total number of ART drugs and classes to which patient was exposed at 3 years, whether patient has changed treatment from initial regimen, as ascertained when available | |||
| Outcome variables: Causes of death, loss to follow-up indicator, and reason for loss to follow-up | |||
| 2008a | 18 | 59 483 | As above, plus: |
| Demographic variables: current alcohol, injection-drug use and smoking | |||
| Laboratory variables: longitudinal measurements of CD4 cells and viral load are now available, as well as other longitudinal laboratory measures (such as alanine aminotransferase, creatinine) and virology measures (such HCV/HBV status) | |||
| Clinical variables: Detailed information about start/stop dates of drugs and reasons for drug changes. | |||
| 2010 | 19 | 74 048 | As above |
aData were collected according to the HICDEP (see http://hicdep.org) format from the 2008 update onwards. This enabled collection of longitudinal data.
Abbreviations: ANRS, Agence Nationale de Recherche SIDA; ART, antiretroviral therapy; CDC, US Centers for Disease Control and Prevention; HBV, hepatitis B virus; HCV, hepatitis C virus; IDU, injection-drug user.
What has been measured?
The variables collected at each update of the ART-CC data set have become more extensive over the years and are listed in Table 2. The first data set included only basic demographic, laboratory, and clinical variables at the beginning of a patients ART and at 6 months after the beginning of ART. In contrast, the most recent update collected comprehensive longitudinal data for laboratory values (including both prognostic markers in HIV infection such as CD4 cells and viral load, and non-HIV–specific biomarkers such as haemoglobin and creatinine), start and stop dates of antiretroviral drugs used during the observation period and the reasons for changes in a drug regimen, and data on causes of death. A panel of experts has retrospectively validated causes of death in ART-CC, using the CoDe system (http://www.cphiv.dk/CoDe/tabid/55/Default.aspx).2
Table 3 shows baseline characteristics of patients in each of the 19 ART-CC cohorts that supplied data for the 2010 update. The ANRS C04 FHDH cohort, which recruits patients from most regions of France, contributes the largest number of patients. The cohorts are heterogeneous in nature and outcomes.3 Reported percentages of patients who have died vary from 1.4% in the Frankfurt cohort to 19% in the HOMER cohort, which recruited a large number of injection-drug users (IDUs). The proportion of female participants also varies greatly among cohorts, from 1.6% in HAVACS (a cohort of US military veterans) to 33% in FHDH (which has a large proportion of immigrants from sub-Saharan Africa).
Table 3.
Antiretroviral Therapy Cohort Collaborative data on numbers of patients, follow-up time, patient demographics, median CD4 cell count, and logarithm of viral load at start of antiretroviral therapy by cohort and overall: 2010 update
| Risk transmission group |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cohorta | Number of patients (%) | Person-years of follow up | Median age (years) | Female (%) | AIDS at start of ART (%) | IDU (%) | MSM (%) | Hetero- sexual sex (%) | Blood products (%) | Other or unknown (%) | Median CD4+ cell count (cells/ml) | Median log Viral load (Log copies/ml) |
| ATHENA | 6742 (9.1) | 36 578 | 37 | 24 | 25 | 3 | 51 | 38 | 1.2 | 7 | 190 | 4.9 |
| Alberta | 706 (1.0) | 3158 | 37 | 20 | 44 | 21 | 44 | 34 | 1.1 | 0.7 | 193 | 4.8 |
| Aquitaine | 1298 (1.8) | 7029 | 36 | 25 | 12 | 15 | 43 | 34 | 2 | 6 | 273 | 4.8 |
| HOMER | 2839 (3.8) | 13 931 | 39 | 18 | 16 | 30 | 16 | 5 | 0.4 | 49 | 180 | 5 |
| Köln/Bonn | 1078 (1.5) | 4486 | 37 | 22 | 45 | 5 | 49 | 19 | 2.1 | 25 | 170 | 5 |
| CoRIS | 994 (1.3) | 1828 | 37 | 26 | 26 | 18 | 33 | 45 | 0 | 4 | 181 | 5 |
| EuroSIDA | 1736 (2.3) | 7725 | 36 | 24 | 20 | 15 | 46 | 33 | 0.5 | 6 | 211 | 5 |
| FHDH | 29 464 (40) | 1 49 780 | 37 | 33 | 22 | 10 | 30 | 50 | 1.3 | 9 | 233 | 4.7 |
| Frankfurt | 146 (0.2) | 258 | 38 | 23 | 19 | 10 | 49 | 31 | 0.7 | 9 | 186 | 5.2 |
| HAVACS | 386 (0.5) | 1881 | 43 | 2 | 26 | 13 | 47 | 7 | 0 | 33 | 182 | 5 |
| ICONA | 3227 (4.4) | 16 997 | 36 | 28 | 18 | 32 | 23 | 39 | 0.6 | 6 | 252 | 4.9 |
| PISCIS | 2970 (4.0) | 11 841 | 36 | 23 | 22 | 29 | 30 | 37 | 0.7 | 4 | 210 | 5 |
| Royal Free | 1385 (1.9) | 6156 | 36 | 27 | 26 | 2 | 53 | 43 | 0 | 2 | 194 | 5.1 |
| SHCS | 4538 (6.1) | 25 403 | 36 | 31 | 21 | 20 | 34 | 42 | 0.8 | 3 | 204 | 4.9 |
| UAB | 502 (0.7) | 1745 | 37 | 24 | 47 | 7 | 38 | 31 | 0 | 28 | 142 | 4.9 |
| VACH | 7038 (9.5) | 39 037 | 35 | 23 | 20 | 34 | 27 | 34 | 0.5 | 5 | 210 | 5 |
| VACS | 7371 (10) | 43 079 | 46 | 2 | 29 | 7 | 0 | 0 | 0 | 73 | 197 | 4.8 |
| Vanderbilt | 1005 (1.4) | 3488 | 37 | 24 | 10 | 10 | 39 | 28 | 0 | 22 | 190 | 4.9 |
| Washington | 623 (0.8) | 2730 | 37 | 16 | 28 | 25 | 49 | 24 | 0 | 1 | 180 | 5 |
| All | 74 048 (100) | 3 77 129 | 38 | 26 | 23 | 17 | 30 | 37 | 0.9 | 16 | 215 | 4.9 |
aSee Table 1 for full names of cohorts.
Abbreviations: AIDS, acquired immune deficiency syndrome; ART, antiretroviral therapy; IDU, injection drug use; MSM, men who have sex with men.
What is the extent of attrition?
Overall rates of loss to follow-up in the different AST-CC cohorts has ranged from 2%–18%, depending on opportunities for access to care outside the contributing centres, and cohorts’ ability to track patient transfers and pursue patients who miss appointments. Thus, for example, losses to follow-up in the Royal Free cohort are partly due to patients’ attending alternative clinics in London. In France, IDUs and immigrants, and patients with lower CD4 cell counts and higher viral loads, were more likely to be lost to follow-up. In contrast, patients in Switzerland with higher CD4 cell counts were more likely to be lost to follow up.
What are the major findings to date?
Prognosis from the beginning of antiretroviral therapy and after accounting for response to therapy
Our first paper on the prognosis for HIV-1–infected patients from beginning of ART was published in 2002.4 This and several other papers from the ART-CC have been cited in treatment guidelines.5–7 We showed that the CD4 cell count at which individuals began ART strongly predicted disease progression. A higher viral load, older age, infection via injection-drug use, and a diagnosis of AIDS before the initiation of treatment were also predictors of poorer outcome. The probability of death within 3 years after the beginning of treatment ranged from 0.8%–43%, depending on these risk factors. The prognostic modelling methodology8 has been used by several other collaborations,9.10 and the ART-CC prognostic model has been validated with data from the CASCADE collaboration.11 Further work examined the way in which prognosis depends on the initial response to ART.12 Viral load and CD4 cell count at 6 months strongly predicted subsequent survival, whereas the values measured at the beginning of treatment no longer predicted survival after accounting for the 6 month measurements.
Analyses were updated in 2007 to include new patients who began ART up to 2003 and a longer follow-up of existing patients in the ART-CC database.13 Cumulative probabilities of AIDS and death at up to 5 years from the beginning of ART were provided in the paper that described the update13 and as an interactive risk calculator on the ART-CC website (www.bris.ac.uk/art-cc/research/calculator/). We investigated, in patients treated for at least 3 years, the prognostic importance, for AIDS and death, of the CD4 cell count and HIV-1 viral load measured at the beginning of ART and at 6 and 36 months later.14 Although the most recent values of the CD4 cell count and viral load are the most important prognostic factors, changes in the CD4 cell count from 6 to 36 months after the beginning of ART, and the value of the viral load at 6 months, were also prognostic for AIDS.
We showed that the incidence of all AIDS-defining events decreased substantially after the beginning of ART, and that the decline was most pronounced for events with a viral aetiology.15 We found that some patient groups, such as men who have sex with men, experience a greater benefit from ART than do other groups,16 and that AIDS-related events differed in their importance for subsequent prognosis.17 In later updates data were collected on non-HIV biomarkers, for example, haemoglobin, liver enzymes and creatinine, and were incorporated into prognostic models.18
Trends in mortality over time, life expectancy and cause-specific mortality
In 2006, after a decade of availability of combination ART, we reported on trends over time in the response to treatment for HIV and the prognosis for treated patients.19 Standardised mortality rates in HIV-positive individuals were compared with those in country-matched background populations.20 Estimates of life expectancy were shown to have increased by some 13 years for patients in whom ART was begun from 2003–2005 as compared with 1996–1999, with an accompanying decline in mortality of nearly 40% in the same period.21 However, life expectancy in these patients remained well short of that of the general population, and patients treated later in the course of their infection had a shorter life expectancy.
From 2006 onward, we collected and classified information about causes of death. Overall, almost 50% of deaths were caused by AIDS.2 Because rates of death from AIDS declined with the duration of ART, rates of non-AIDS–related death exceeded those of death from AIDS after 4 years of ART. Lifestyle-related causes of death such as suicide, drug overdose, and liver diseases (mainly hepatitis) were the most frequent causes of non-AIDS–related deaths, with the most common non-AIDS–related cancer being lung cancer. Deaths from causes associated with ageing, such as cancers other than lung cancer and cardiovascular disease, will be of increasing importance in treated HIV-positive people over the next decade, and the ART-CC will have the capacity to explore these trends.
When to begin antiretroviral therapy
The CD4 cell count below which ART should be begun remains a central issue in the care of HIV-positive individuals. In 2009 we attempted to address this question by combining data from observational cohort studies conducted before and after the era of combination ART,22 and concluded that deferring treatment until the CD4 cell count was under 350 cells/µl was associated with increased rates of AIDS. International treatment guidelines were amended later in 2009 to account for our own and others’ findings, mainly in cohort studies. However only a randomised controlled trial will definitively show whether deferring treatment on the basis of the CD4 cell count will increase the rates of AIDS. Results of the Strategic Timing of Antiretroviral therapy (START) trial23 are awaited with interest in this regard.
Prognosis for patients infected through injection-drug use
Patients infected with HIV-1 through injection-drug use have worse outcomes after treatment than do those infected sexually.24 We found that mortality rates of IDUs were twice as high as those of non-IDUs, and that IDUs experienced higher rates than did non-users of infection drugs of almost all causes of death, particularly liver-related deaths and deaths from direct effects of substance abuse. The CD4 cell count predicted death more strongly for non-users of injection drugs than for IDUs, indicating that excess mortality in IDUs was related to factors other than HIV. Excess mortality in IDUs may also relate to suboptimal management of HIV disease in these individuals.
Estimated effects of different antiretroviral drugs on the basis of observational studies and clinical trials
We found evidence that rates of AIDS and death varied according to the drugs included in the initial ART regimen,19 and that between-regimen differences in rates of short-term virological failure (the outcome most commonly used in clinical trials) do not necessarily translate to longer-term differences in rates of various clinical outcomes.25 We compared the results of two randomized trials done by the AIDS Clinical Trial Group (ACTG 5095 and ACTG 5142) with those estimated in ART-CC cohorts, which follow patients in routine care.26 Results for the ART-CC cohorts were comparable with those of the trials conducted in similar settings, and we concluded that the results of clinical trials appear ro be generalisable to routine-care settings in resource-rich countries.
Other topics covered by the Antiretroviral Therapy Cohort Collaborative
Collaborative analyses have compared mortality during the first year of ART in resource-limited and high income settings.9 In the past, similar comparisons of the incidence of tuberculosis were reported.27,28 Other questions addressed by the ART-CC include the way in which the effect of prognostic factors at the beginning of ART varies with the duration of treatment,29 and the effect of baseline CD4 cell counts on the clinical significance of short-term immunologic responses to ART in individuals with virologic suppression.30
Current work
We have recently examined the effect of sex,31 race/ethnicity, and geographical origin32,33 on the prognosis in HIV infection and investigated the heterogeneity in mortality rates among cohorts.3 Ongoing analyses are addressing the durability of first-line ART and the cumulative incidence of and risk factors for different types of changes in regimen and of the interruption of ART. This work will be extended to use methods for causal inference34 to examine the implications for subsequent mortality of different strategies for switching ART regimens after virological failure. As longer follow-up data become available, we will estimate the prognosis for patients treated for up to 10 years, investigate whether the prognosis in HIV-1 infection becomes stable after an initial response to ART, and investigate the effect of cumulative viral load on specific causes of death. We are also now investigating measures and effects of adherence to ART. The ART-CC is working increasingly closely with other collaborations of HIV cohort studies, in particular the Collaboration of Observational HIV Epidemiological Research Europe (COHERE), which now merges the data for European cohorts participating in the ART-CC, as well as the HIV-Cohorts Analyzed Using Structural Approaches to Longitudinal Data (HIV-CAUSAL) Collaboration, and the International epidemiologic Databases to Evaluate AIDS (IeDEA) Southern Africa Collaboration. The ART-CC also works with the North American AIDS Cohort Collaboration on Research and Design (NA-ACCORD), IeDEA West Africa, and the Concerted Action on SeroConversion to AIDS and Death in Europe (CASCADE) collaboration.
What are the main strengths and weaknesses?
The generosity and collaborative spirit of researchers in the contributing cohort studies has been a key strength of ART-CC, which has brought together researchers with clinical, epidemiological and statistical expertise. The ART-CC data base includes large numbers of patients enrolled in diverse cohorts from two continents, so that the results for different cohorts are likely to be generalisable to patients in clinical care in this broad setting. All patients in the ART-CC were ART-naïve when they began treatment, and the results for the Collaboration are therefore relevant to new patients starting combination ART. However, prognostic models are fitted on historic data, and therefore provide trailing indicators of prognosis for new patients starting ART with improved drugs and co-formulations. The large data set of the ART-CC permits examination of prognoses for specific causes of death, but these data are incomplete. So far, it has been possible to classify only 85% of deaths, and there will have been some misclassification because of limitations of available data. There is likely to be some under-ascertainment of deaths, which may result in estimates of mortality rates and life expectancy being over-optimistic. Nevertheless, most of the cohorts in the ART-CC link to death registries, but at intervals that vary from monthly to tri-annually.3 Because the data are mainly collected as part of routine clinical care, there are issues with the standardisation of definitions and completeness of data. Moreover, not all laboratory, demographic and lifestyle measures are available from all cohorts. Data on important life-style risk factors, such as smoking and substance abuse, which affect mortality and may be highly prevalent in some HIV-positive populations, have not yet been sufficiently widely available for inclusion in prognostic models. Data on adherence to ART are now being collected, but not data on patient physical and psychological symptoms or quality of life measures.
Can I get the data gathered by the Antiretroviral Therapy Collaboration?
The data collected by the ART-CC remain the property of the contributing cohorts, and all analyses of these data must be approved by the ART-CC steering committee. Each cohort has a representative on the steering committee, which also includes patient representatives who provide guidance by asking research questions that are important and relevant to patients. Interested investigators should contact the co-ordinating centre and will be asked to fill in a concept sheet which gives brief details of the proposed study. All concept sheets are discussed by the steering committee, and projects must also be approved by contributing cohorts. We welcome the addition of collaborating cohorts to the ART-CC; eight cohorts have joined since the Collaboration was established in 2000. More information, including details of collaborating centres, is available on the ART-CC website (www.art-cohort-collaboration.org).
Author Contributions
M.T.M. and S.M.I. wrote the first draft of the paper and compiled the tables. S.M.I. contributed the figures. All authors contributed to the study design and the writing of the manuscript, and approved the final version of the paper.
Funding
This work was funded by the UK Medical Research Council grant MR/J002380/1.
Antiretroviral Therapy Cohort Collaboration Steering Group
Andrew Boulle (IeDEA Southern Africa), Hans-Reinhard Brodt (Frankfurt), Jordi Casabona (PISCIS), Matthias Cavassini (SHCS), Geneviève Chêne (Aquitaine), Dominique Costagliola (FHDH), François Dabis (Aquitaine), Antonella D’Arminio Monforte (ICONA), Julia del Amo (CoRIS), Frank de Wolf (ATHENA), Gerd Fätkenheuer (Köln/Bonn), John Gill (South Alberta Clinic), Jodie Guest (HAVACS), David Hans-Ulrich Haerry (EATG), Robert Hogg (HOMER), Amy Justice (VACS), Amanda Mocroft (EuroSIDA), Mari Kitahata (Washington), Fiona Lampe (Royal Free), Peter Reiss (ATHENA), Michael Saag (Alabama), Timothy Sterling (Vanderbilt-Meharry), Matthew Williams (UK-CAB), Robert Zangerle (Austria)
Co-ordinating team
Jonathan Sterne and Margaret May (Principal Investigators), Suzanne Ingle (statistician).
Acknowledgements
We thank all patients, doctors, and study nurses associated with the participating cohort studies. We gratefully acknowledge GSK for initially funding the study. Since 2002, the ART-CC has been supported by the UK Medical Research Council (grants G0100221, G0700820, and MR/J002380/1). Sources of funding of individual cohorts include the Agence Nationale de Recherches sur le SIDA et les hépatites virales (ANRS), the Institut National de la Santé et de la Recherche Médicale (INSERM), the French, Italian, and Spanish Ministries of Health, the Swiss National Science Foundation (grant 33CS30-134277), the Ministry of Science and Innovation and the Spanish Network for AIDS Research (RIS; ISCIII-RETIC RD06/006), the Stichting HIV Monitoring, the European Commission (EuroCoord grant 260694), the British Columbia and Alberta Governments, the National Institutes of Health (NIH) [UW Center for AIDS Research (CFAR) (NIH grant P30 AI027757), UAB CFAR (NIH grant P30-AI027767), The Vanderbilt-Meharry CFAR (NIH grant P30 AI54999), the National Institute on Alcohol Abuse and Alcoholism (U10-AA13566, U24-AA020794), the US Department of Veterans Affairs, the Michael Smith Foundation for Health Research, the Canadian Institutes of Health Research, the VHA Office of Research and Development, and unrestricted grants from Abbott, Gilead, Tibotec-Upjohn, ViiV Healthcare, MSD, GlaxoSmithKline, Pfizer, Bristol Myers Squibb, Roche, and Boehringer-Ingelheim.
Conflict of interest: None declared.
KEY MESSAGES.
Patients starting ART later in the course of their infection had worse prognosis, as did those infected via injection drug use.
Life expectancy of HIV positive individuals increased by 13 years for those initiating ART in 2003–05 compared with 1996-99.
Overall, almost 50% of deaths were from AIDS, but rates of non-AIDS death exceeded rates of AIDS death after four years of ART.
Deferring treatment until CD4 count is less than 350 cells/μL was associated with increased rates of AIDS.
References
- 1.Mocroft A, Vella S, Benfield TL, Chiesi A, Miller V, Gargalianos P, et al. Changing patterns of mortality across Europe in patients infected with HIV-1. EuroSIDA Study Group. Lancet. 1998;352:1725–30. doi: 10.1016/s0140-6736(98)03201-2. [DOI] [PubMed] [Google Scholar]
- 2.Gill MJ, May M, Lewden C, Saag M, Mugavero MJ, Reiss P, et al. and the Antiretroviral Therapy Cohort Collaboration Causes of death in HIV-1 infected patients treated with antiretroviral therapy 1996–2006: collaborative analysis of 13 HIV cohorts. Clin Infect Dis. 2010;50:1387–96. doi: 10.1086/652283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.May M, Hogg RS, Justice AC, Shepherd B, Costagliola D, Ledergerber B, et al. Heterogeneity in outcomes of treated HIV-positive patients in Europe and North America: relation with patient and cohort characteristics. Int J Epidemiol. 2012;41:1807–20. doi: 10.1093/ije/dys164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Egger M, May M, Chene G, Phillips AN, Ledergerber B, Dabis F, et al. Prognosis of HIV-1-infected patients starting highly active antiretroviral therapy: a collaborative analysis of prospective studies. Lancet. 2002;360:119–29. doi: 10.1016/s0140-6736(02)09411-4. [DOI] [PubMed] [Google Scholar]
- 5.Pozniak A, Gazzard B, Anderson J, Babiker A, Churchill D, Collins S, et al. British HIV Association (BHIVA) guidelines for the treatment of HIV-infected adults with antiretroviral therapy. HIV Med. 2003;4(Suppl 1):1–41. [PubMed] [Google Scholar]
- 6.British HIV Association (BHIVA) guidelines for the treatment of HIV-1-positive adults with antiretroviral therapy 2012. HIV Med. 2012;13(Suppl 2):1–85. doi: 10.1111/j.1468-1293.2012.01029.x. available at: http://www.bhiva.org/documents/Guidelines/Treatment/2012/hiv1029_2.pdf (24 September 2012, date last accessed) [DOI] [PubMed] [Google Scholar]
- 7.Panel on Antiretroviral Guidelines for adults and adolescents. Guidelines for the Use of Antiretroviral Agents in HIV-1 Infected Adults and Adolescents. Washington, DC: Department of Health and Human Services; pp. 1–167. Available at: http://aidsinfo.nih.gov/contentfiles/AdultandAdolescentGL002534.pdf (24 September 2012, date last accessed) [Google Scholar]
- 8.May M, Royston P, Egger M, Justice AC, Sterne JA. Development and validation of a prognostic model for survival time data: application to prognosis of HIV positive patients treated with antiretroviral therapy. Stat Med. 2004;23:2375–98. doi: 10.1002/sim.1825. [DOI] [PubMed] [Google Scholar]
- 9.Braitstein P, Brinkhof MW, Dabis F, Schechter M, Boulle A, Miotti P, et al. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: comparison between low-income and high-income countries. Lancet. 2006;367:817–24. doi: 10.1016/S0140-6736(06)68337-2. [DOI] [PubMed] [Google Scholar]
- 10.May M, Boulle A, Phiri S, Messou E, Myer L, Wood R, et al. Prognosis of patients with HIV-1 infection starting antiretroviral therapy in sub-Saharan Africa: a collaborative analysis of scale-up programmes. Lancet. 2010;376:449–57. doi: 10.1016/S0140-6736(10)60666-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.May M, Porter K, Sterne JA, Royston P, Egger M. Prognostic model for HIV-1 disease progression in patients starting antiretroviral therapy was validated using independent data. J Clin Epidemiol. 2005;58:1033–41. doi: 10.1016/j.jclinepi.2005.02.015. [DOI] [PubMed] [Google Scholar]
- 12.Chene G, Sterne JA, May M, Costagliola D, Ledergerber B, Phillips AN, et al. Prognostic importance of initial response in HIV-1 infected patients starting potent antiretroviral therapy: analysis of prospective studies. Lancet. 2003;362:679–86. doi: 10.1016/s0140-6736(03)14229-8. [DOI] [PubMed] [Google Scholar]
- 13.May M, Sterne JA, Sabin C, Costagliola D, Justice AC, Thiebaut R, et al. Prognosis of HIV-1-infected patients up to 5 years after initiation of HAART: collaborative analysis of prospective studies. AIDS. 2007;21:1185–97. doi: 10.1097/QAD.0b013e328133f285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lanoy E, May M, Mocroft A, Phillip A, Justice A, Chene G, et al. Prognosis of patients treated with cART from 36 months after initiation, according to current and previous CD4 cell count and plasma HIV-1 RNA measurements. AIDS. 2009;23:2199–208. doi: 10.1097/QAD.0b013e3283305a00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.D'Arminio MA, Sabin CA, Phillips A, Sterne J, May M, Justice A, et al. The changing incidence of AIDS events in patients receiving highly active antiretroviral therapy. Arch Intern Med. 2005;165:416–23. doi: 10.1001/archinte.165.4.416. [DOI] [PubMed] [Google Scholar]
- 16.Sabin CA, Phillips AN, Hogg RS, Dabis F, Gill MJ, Reiss P, et al. on behalf of the Antiretroviral Therapy (ART) Cohort Collaboration. AIDS events among individuals initiating HAART: do some patients experience a greater benefit from HAART than others? AIDS. 2005;19:1995–2000. doi: 10.1097/01.aids.0000189858.59559.d2. [DOI] [PubMed] [Google Scholar]
- 17.Mocroft A, Sterne JA, Egger M, May M, Grabar S, Furrer H, et al. Variable impact on mortality of AIDS-defining events diagnosed during combination antiretroviral therapy: not all AIDS-defining conditions are created equal. Clin Infect Dis. 2009;48:1138–51. doi: 10.1086/597468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris RJ, Sterne JA, Abgrall S, Dabis F, Reiss P, Saag M, et al. Prognostic importance of anaemia in HIV type-1-infected patients starting antiretroviral therapy: collaborative analysis of prospective cohort studies. Antivir Ther. 2008;13:959–67. [PMC free article] [PubMed] [Google Scholar]
- 19.May MT, Sterne JA, Costagliola D, Sabin CA, Phillips AN, Justice AC, et al. HIV treatment response and prognosis in Europe and North America in the first decade of highly active antiretroviral therapy: a collaborative analysis. Lancet. 2006;368:451–58. doi: 10.1016/S0140-6736(06)69152-6. [DOI] [PubMed] [Google Scholar]
- 20.Zwahlen M, Harris RJ, Hogg R, Costagliola D, May M, de WF, et al. Mortality of HIV-infected patients starting potent antiretroviral therapy: comparison with the general population in eight industrialized countries. Int J Epidemiol. 2009;38:1624–33. doi: 10.1093/ije/dyp306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hogg R, Lima V, Sterne JAC, Grabar S, Battegay M, Bonarek M, et al. Life expectancy of individuals on combination antiretroviral therapy in high-income countries: a collaborative analysis of 14 cohort studies 1. Lancet. 2008;372:293–99. doi: 10.1016/S0140-6736(08)61113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sterne JA, May M, Costagliola D, de Wolf F, Phillips AN, Harris R, et al. Timing of initiation of antiretroviral therapy in AIDS-free HIV-1-infected patients: a collaborative analysis of 18 HIV cohort studies. Lancet. 2009;373:1352–1363. doi: 10.1016/S0140-6736(09)60612-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Babiker AG, Emery S, Fatkenheuer G, Gordin FM, Grund B, Lundgren JD, et al. Considerations in the rationale, design and methods of the Strategic Timing of AntiRetroviral Treatment (START) study. Clin Trials. 2012 doi: 10.1177/1740774512440342. doi:10.1177/1740774512440342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Murray M, Hogg RS, Lima VD, May MT, Moore DM, Abgrall S, et al. The effect of injecting drug use history on disease progression and death among HIV-positive individuals initiating combination antiretroviral therapy: collaborative cohort analysis. HIV Med. 2012;13:89–97. doi: 10.1111/j.1468-1293.2011.00940.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mugavero MJ, May M, Harris R, Saag MS, Costagliola D, Egger M, et al. Does short-term virologic failure translate to clinical events in antiretroviral-naive patients initiating antiretroviral therapy in clinical practice? AIDS. 2008;22:2481–92. doi: 10.1097/QAD.0b013e328318f130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mugavero MJ, May M, Ribaudo HJ, Gulick RM, Riddler SA, Haubrich R, et al. Comparative effectiveness of initial antiretroviral therapy regimens: ACTG 5095 and 5142 clinical trials relative to ART-CC cohort study. J Acquir Immune Defic Syndr. 2011;58:253–60. doi: 10.1097/QAI.0b013e318230372e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Girardi E, Sabin CA, D'Arminio MA, Hogg B, Phillips AN, Gill MJ, et al. Incidence of Tuberculosis among HIV-infected patients receiving highly active antiretroviral therapy in Europe and North America. Clin Infect Dis. 2005;41:1772–82. doi: 10.1086/498315. [DOI] [PubMed] [Google Scholar]
- 28.Brinkhof MW, Egger M, Boulle A, May M, Hosseinipour M, Sprinz E, et al. Tuberculosis after initiation of antiretroviral therapy in low-income and high-income countries. Clin Infect Dis. 2007;45:1518–21. doi: 10.1086/522986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sterne JAC, May M, Sabin C, Phillips A, Costagliola D, Chene G, et al. Importance of baseline prognostic factors with increasing time since initiation of highly active antiretroviral therapy—Collaborative analysis of cohorts of HIV-1-Infected patients. J Acquir Immune Defic Syndr. 2007;46:607–15. doi: 10.1097/QAI.0b013e31815b7dba. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Moore DM, Harris R, Lima V, Hogg B, May M, Yip B, et al. Effect of baseline CD4 cell counts on the clinical significance of short-term immunologic response to antiretroviral therapy in individuals with virologic suppression. J Acquir Immune Defic Syndr. 2009;52:357–63. doi: 10.1097/QAI.0b013e3181b62933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jarrin I. Sex differences in mortality rates among HIV-positive patients: The Antiretroviral Therapy Cohort Collaboration. Presented at the International AIDS Society Conference (IAS) in July 2011; Rome, Italy. [Google Scholar]
- 32.Jarrin I, Del Amo J, the Antiretroviral Therapy Cohort Collaboration (ART-CC) Differences in mortality rates among treated patients according to geographical origin and ethnicity/race. 18th Conference on Retroviruses and Opportunistic Infections; February 2011; Boston, MA, USA. [Google Scholar]
- 33.Shepherd BE, Jenkins CA, Parrish DD, Glass TR, Cescon A, Masbeu A, et al. Higher rates of AIDS during the first year of antiretroviral therapy among migrants: the importance of tuberculosis. AIDS. 2012 doi: 10.1097/QAD.0b013e32835faa95. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Cain LE, Robins JM, Lanoy E, Logan R, Costagliola D, Hernan MA. When to start treatment? A systematic approach to the comparison of dynamic regimes using observational data. Int J Biostat. 2010 doi: 10.2202/1557-4679.1212. doi:10.2202/1557-4679.1212. [DOI] [PMC free article] [PubMed] [Google Scholar]