Abstract
Androgen deprivation therapy (ADT) resulting in testosterone suppression is central to the management of prostate cancer (PC). As PC incidence increases, ADT is more frequently prescribed, and for longer periods of time as survival improves. Initial approaches to ADT included orchiectomy or oral estrogen (diethylstilbestrol [DES]). DES reduces PC-specific mortality, but causes substantial cardiovascular (CV) toxicity. Currently, luteinizing hormone-releasing hormone agonists (LHRHa) are mainly used; they produce low levels of both testosterone and estrogen (as estrogen in men results from the aromatization of testosterone), and many toxicities including osteoporosis, fractures, hot flashes, erectile dysfunction, muscle weakness, increased risk for diabetes, changes in body composition, and CV toxicity. An alternative approach is parenteral estrogen, it suppresses testosterone, appears to mitigate the CV complications of oral estrogen by avoiding first-pass hepatic metabolism, and avoids complications caused by estrogen deprivation. Recent research on the toxicity of ADT and the rationale for revisiting parenteral estrogen is discussed.
Keywords: Prostate cancer, estrogen, testosterone, LHRH agonist, PATCH trial, androgen deprivation therapy (ADT)
This review describes strategies for producing castrate levels of testosterone in men with androgen-sensitive prostate cancer (PC) and the associated toxicities, with particular focus on the re-emergence and potential benefits of parenteral estrogen. In the developed world, PC is the commonest malignancy and second commonest cause of cancer death affecting men. Its incidence is increasing with an aging population and frequent prostate-specific antigen (PSA) testing.1 Almost 240,000 new cases of PC are diagnosed each year in the US and nearly 30,000 American men die from PC annually.2
Androgen Deprivation Therapy
The androgen dependence of PC has been recognized since the 1940s and remains a major component of the strategies used to manage PC today.
Surgical Orchiectomy and Oral Estrogen
Androgen deprivation therapy (ADT) was initially achieved by surgical orchiectomy, as the testes produce nearly 95 % of circulating androgens; the remaining 5 % is produced by the adrenal glands.3 As surgical castration is invasive and can cause significant psychological trauma it became less common following the introduction of medical (also called chemical) ADT. Diethylstilbestrol (DES), a synthetic oral estrogen, was the first pharmacological agent used as ADT for PC. The primary mechanism of action of DES involves a negative feedback loop affecting the hypothalamic–pituitary–testicular axis.4,5 The pulsatile secretion of hypothalamic luteinizing hormone-releasing hormone (LHRH) stimulates the release of follicle stimulating hormone (FSH) and LH from the anterior pituitary, which then stimulates testicular Leydig cells to produce testosterone. DES remained an effective and low-cost option for ADT from the 1950s up to the 1980s, but its use was discontinued following findings of adverse cardiovascular system (CVS) outcomes from the Veterans Administrative Cooperative Urological Research Group (VACURG) trials. Initiated in the early 1960s, this series of randomized clinical trials compared DES with orchiectomy, placebo, DES plus orchiectomy, and placebo plus orchiectomy. Although DES improved PC outcomes, the DES groups were shown to have increased CVS toxicity (36 % increase in non-cancer-related deaths mostly CVS) with the highest risk in the first year of starting therapy.6
Luteinizing Hormone-releasing Hormone Agonists and Anti-androgens
Luteinizing hormone-releasing hormone agonists (LHRHa), also called gonadotrophin-releasing hormone analogs (GnRHa), were introduced in the 1980s for ADT. Unlike the pulsatile action of hypothalamic LHRH, synthetic LHRHa continually stimulate pituitary receptors, causing downregulation of the receptors and central hypogonadism. Initial exposure to LHRHa leads to a surge in androgen production, termed ‘testosterone flare’, which in some patients can exacerbate symptoms, such as bone pain from skeletal metastasis, increase the risk for aggravating nerve compression (e.g. spinal cord compression), or worsen urinary outflow obstruction. Short courses of anti-androgens that compete with androgens for receptor binding are given to avoid these complications.7,8
ADT with LHRHa is a mainstay of contemporary PC treatment. It is used alone to control PC or in the neoadjuvant/adjuvant setting with radical surgery or radiotherapy. It is also used for advanced PC, which can be incurable at presentation or as a result of disease recurrence following the failure of radical therapy. Estimates suggest that more than half of the men diagnosed with PC will be treated with ADT at some point during the course of their disease, remaining on it for a decade or even more.9
Novel Agents
Degarelix, an LHRH antagonist, is another form of ADT that binds competitively to pituitary LHRH receptors.10 It reduces LH and testosterone levels without causing testosterone flare. Other newer agents include abiraterone (an inhibitor of androgen biosynthesis) and enzalutamide (an inhibitor of nuclear translocation of the androgen receptor) that are currently reserved for use in castration-resistant PC, when the cancer no longer responds to ADT despite castrate levels of testosterone.3,7
Toxicities of Androgen Deprivation Therapy
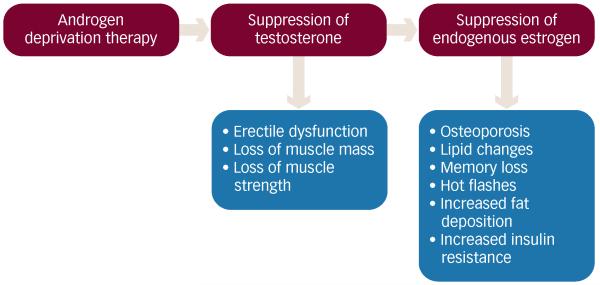
In the last decade there has been a growing recognition of the need to understand the nature and impact of the toxicities from contemporary ADT with LHRHa. This becomes more salient when considering the ever-increasing and widespread use of LHRHa, as the incidence of PC and overall survival with PC increases. LHRHa toxicity has a large impact on the health economy and overall cost of treating PC. LHRHa are associated with multiple adverse effects (see Figure 1) including osteoporosis and associated fractures, hot flashes, imbalances in lipid and glucose homeostasis, diminished libido, erectile dysfunction, depression, cognitive decline, loss of musculature, adiposity, anemia, increased susceptibility to CVS events, and decreased physical strength.11-19 Some toxicities of LHRHa can be attributed to low testosterone levels. These include loss of libido, erectile dysfunction, and low muscle mass. Others, such as osteoporosis, fracture risk, hot flashes, and dyslipidemia are thought to be due to the accompanying estrogen deficiency (80 % reduction in estrogen levels by LHRHa), as testosterone is required for synthesis of estrogen through aromatization.19-21 Collectively these toxicities are labeled as ‘castration syndrome’ or ‘androgen deprivation syndrome,’ and greatly impact upon quality of life (QoL). ADT also affects the intimate partners of those receiving ADT and studies suggest that partners often experience more distress than the patients themselves.22
Figure 1. Toxicities Associated with Androgen Deprivation Therapy Attributed to Sex Hormone Deficiency.
A recent study in healthy individuals without PC has attempted to identify which short-term metabolic effects of ADT are related to testosterone insufficiency and which are related to estrogen insufficiency.23 The study enrolled 400 patients, divided into two equal cohorts (198 patients in cohort 1; 202 patients in cohort 2). Patients in both cohorts received a LHRHa (goserelin) and were then randomized to varying levels of testosterone replacement (0, 1.25 g, 2.5g, 5 g, and 10 g of testosterone gel in 24 hours). The second cohort additionally received anastrazole (which prevents the aromatization of testosterone to estrogen). Thus, in cohort 1 the varying levels of testosterone replacement were physiologically converted into estrogen, whereas in cohort 2 estrogen levels were suppressed with anastrazole, irrespective of the level of testosterone replacement. The study showed that testosterone deficiency led to a decrease in lean body mass, muscle mass, and muscle strength. The dose of testosterone to avoid these adverse effects was wide ranging among both cohorts. Estrogen deficiency seen in cohort 2 accounted for increases in percentage body fat. Increased deposition of body fat is thought to be associated with decreased insulin sensitivity and an increased risk for diabetes.24 Both groups showed a decrease in sexual desire and function.
Bone Weakness
There is extensive evidence showing the detrimental effect of ADT with LHRHa on bone health.25 LHRHa decreases bone mineral density and promotes bone turnover26 and has been shown to increase fracture risk by two to four times with the resulting fractures associated with increased mortality and decreased QoL.27 A recent study utilizing the Surveillance, Epidemiology and End Results (SEER) – Medicare database of 76,000 men with localized PC showed that men with a high baseline risk for skeletal complications had a higher probability of receiving ADT than those with a low risk (52.1 % versus 38.2 %; p<0.001). Those more likely to receive ADT in this study were older men, with higher PSAs, higher Gleason grade, more advanced staged tumors, multiple comorbidities, and those who received bisphosphonates and radiotherapy. Higher fracture risk was associated with those who were treated with ADT as a single modality compared with those who received it concomitantly with radiotherapy, or after a radical prostatectomy. The increased likelihood of receiving ADT with a higher baseline fracture risk correlates with the fact that men identified in the cohort above would be less likely to receive treatment without ADT such as a prostatectomy and were more likely to have treatment initiated because of the higher-risk nature of the cancer. More than 58 % of men with a high risk of developing a fracture and 38 % of men with a low risk had at least one fracture after ADT during the 12-year follow-up and following a fracture, the mortality risk increased by 40 %.28
Vasomotor Symptoms and Sleep Disturbance
Vasomotor symptoms, such as hot flashes and night sweats, are common, affecting almost four out of every five patients receiving ADT. They are thought to be caused by changes in sex hormone levels (particularly estrogen), which disrupt the negative feedback of hypothalamic noradrenaline production leading to a resetting of the thalamic thermoregulatory mechanism.29-32 Hot flashes appear shortly after LHRHa administration, do not appear to subside with the end of treatment, and are associated with substantial psychological distress.21 Disturbance of sleep is also a common occurrence in patients treated for PC. A recent questionnaire-based study showed higher insomnia scores in patients receiving ADT with radiotherapy compared with radiotherapy alone. Hot flashes and night sweats appear to contribute to this sleep disturbance.29,33
Cognitive Impairment
A number of studies using neuropsychological assessments have linked ADT with LHRHa to cognitive impairment.34,35 A meta-analysis by Nelson et al. including nine studies of ADT in PC showed that between 47 and 69 % of men showed decline in at least one cognitive parameter following ADT for 6 to 9 months. The most commonly affected domains included visuospatial ability and executive function.36 Some studies, however, have not shown this effect, Alibhai et al. found no consistent evidence of cognitive decline in ADT users (type of ADT not specified) over a period of 1 year.37 Functional imaging studies are being used to investigate this further. Reduced activation in the parieto-occipital lobe on a mental rotation task (a test of visuospatial memory) with ADT was seen with functional magnetic resonance imaging (fMRI).38 A similar study showed reduced pre-frontal activation on fMRI, but no cognitive deficit,39 and a further study showed decreased cortical gray matter volume in ADT users.40
Sexual Inactivity and Spousal Relations
Sexual activity has been shown to decline considerably in PC patients on ADT with up to 85 % of the patients reporting sexual side effects.12,31,41,42 This sexual inactivity is a consequence of diminished libido, physical changes (decreased strength, adiposity, genital shrinkage), and erectile dysfunction.12,43 Loss of masculine traits in PC patients negatively impacts their psychosocial and sexual life.42 In one small study (n=15), nearly half the men on ADT experienced an erosion of spousal relations.44 This may be related to a degree of estrogen deficiency, as estrogen replacement appears to alleviate some of these symptoms.45
Changes in Body Composition and Physical Function
Body composition changes considerably in men undergoing ADT with LHRHa therapy, with more extensive changes seen with a longer duration of treatment. These changes include increased fat mass (adiposity), loss of lean musculature (sarcopenia), and weight gain.11,46 Smith et al. prospectively measured lean body mass at three time points following the start of ADT and compared it with baseline measurements. A significant decline in mean lean body mass was seen at 1 year (1 % decrease; p<0.01), 2 years (2.1 % decrease; p<0.001), and 3 years (2.4 % decrease; p<0.001).47 Fatigue affects nearly half of the patients on ADT and decreased muscle mass and increased adiposity may be important factors contributing to this.18 Endurance, upper extremity strength, and physical activity are affected within 3 months of starting ADT.48
Acute Kidney Injury
A recent observational study of patients with newly diagnosed non-metastatic PC has highlighted a potentially serious complication of ADT. Out of the 10,250 men studies, 232 new cases of acute kidney injury were identified. ADT included LHRHa, oral anti-androgens, combined androgen blockade (LHRHa plus anti-androgens), orchiectomy, estrogens, and combinations of these. Current ADT use was associated with an increased risk for acute kidney injury compared with no ADT use (odds ratio [OR] 2.48, 95 % confidence interval [CI] 1.61–3.82]).49
Metabolic Disturbances and Cardiovascular Risks
The relationship between CVS risk and LHRHa therapy appears complex. Treatment with LHRHa has been linked to hyperglycemia, insulin resistance, dyslipidemia, and the development of the metabolic syndrome suggesting an increased risk for diabetes and CVS disease in these patients.11,32 Observational data from Medicare databases suggest that men receiving ADT have an increased risk for coronary artery disease (hazard ratio [HR] 1.16, 95 % CI 1.10–1.21, p<0.001), myocardial infarction (HR 1.11, 95 % CI 1.01–1.21; p=0.03), and sudden death (HR 1.16, 95 % CI 1.05–1.27; p=0.004).50 In another cross-sectional study, the occurrence of type 2 diabetes and obesity was significantly greater (p<0.05) in patients receiving ADT (mean time of 15.37±2.48 months) compared with eugonadal men. Randomized data, however, have not supported these associations, for example, in a trial of 945 men, comparing prostate radiotherapy with LHRHa versus radiotherapy alone, after 9 years CV events occurred in 8.4 % in the concomitant treatment group versus 11.4 % in those receiving radiotherapy alone (p=0.17).51 Interestingly, in a recent study, a significantly higher risk for CVS events (p<0.002) was seen with LHRHa alone compared with LHRHa and Degarelix in men who had pre-existing CVS disease.52
Some of the toxicities associated with ADT are not directly attributable to either estrogen or testosterone deficiency alone. For example, gynecomastia is thought to result from a change in the ratio of estrogen to testosterone. Rates of gynecomastia differ between various forms of ADT, the highest rates are seen with estrogen (more than 50 % men affected). Rates are similar with surgical orchiectomy and LHRHa (10–15 %).11
Parenteral Estrogen as Androgen Deprivation Therapy
The route of administration of estrogen is thought to explain the CVS toxicity seen with the oral preparations. When estrogen is taken orally, entero-hepatic first pass exposes the liver to high levels of estrogen resulting in upregulation of pro-coagulant proteins (increased clotting factors I, II, VII, IX, and X) and downregulation of anti-coagulant factors (decreased plasminogen activator and anti-thrombin III). This estrogen-induced hypercoaguable state in turn increases the risk for thromboembolic and CVS events.53
Avoiding this first-pass effect through parenteral estrogen administration (intramuscular, intravenous, subcutaneous, topical) for PC treatment is a logical deduction. This was first tested in a series of studies conducted by the Scandinavian Prostate Cancer Group (SPCG) using polyestradiol phosphate (PEP) administered intramuscularly. In the earlier SPCG studies a monthly PEP dose of 160 mg was given. Rates of CVS morbidity and mortality were not different from surgical orchiectomy or LHRHa but castrate levels of testosterone were not achieved. Reduction in serum testosterone to castrate levels was achieved in subsequent studies at a dose of 240 mg PEP given monthly. No added CVS toxicity was observed with this higher dose. The largest SPCG trial randomized PC patients (n=910) to receive either combined androgen blockade (LHRHa/orchiectomy plus anti-androgen) or intramuscular estrogen (PEP 240 mg). No significant difference was observed between the groups in terms of progression-free survival, overall, or disease-specific survival, and CVS mortality.54
Topical Estrogen
Topical estrogen therapy can be applied either as a transdermal patch, gel, or cream. It has potential advantages over other forms of parenteral estrogen administration, it can be conveniently self-administered by the patient, and readily discontinued if toxicities occur.55 In a small pilot study, Ockrim et al. used transdermal estrogen (estradiol skin patches) in 20 hormone-naïve patients with advanced PC. Castrate levels of testosterone were achieved within 3 weeks of treatment initiation and effective tumor response was obtained in terms of a decrease in PSA levels. With DES, CVS toxicity occurred in up to 35 % of patients with 15 % experiencing a thromboembolic event. This study with parenteral estrogen showed no significant cardiac toxicity.56 Results from another trial of transdermal estradiol as second-line therapy showed a PSA reduction of more than 25 % in 10 of the 24 patients and no thromboembolic complications were seen.57
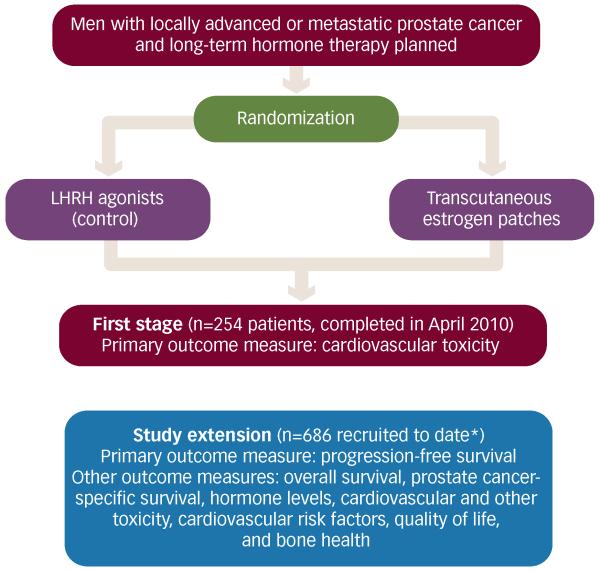
Confirmatory evidence of the potential efficacy of transdermal estrogen therapy comes from the recently published first stage of the Prostate Adenocarcinoma Trans Cutaneous Hormones (PATCH) study (see Figure 2). PATCH is a large phase II randomized clinical trial comparing transdermal estrogen patches with LHRHa in locally advanced and metastatic PC. In a cohort of 254 men (randomized 2:1 to patches or LHRHa) with a median follow-up of 19 months, the rates of CVS events (the primary outcome measure) were similar in the two trial arms (see Table 1). Testosterone suppression rates were also similar in the two groups.58 An extension to this trial is ongoing and has recruited to date nearly 700 men (excluding the first 50 randomized before the initial patch dose regime change) and will provide further efficacy and toxicity data.
Figure 2. Prostate Adenocarcinoma Trans Cutaneous Hormones Trial Schema.
*Includes patients enrolled from the first stage, apart for the first 50 patients randomized before the initial patch dose regime change. LHRH = luteinizing hormone-releasing hormone.
Table 1. Comparison of Outcomes Between Estrogen Patches and Luteinizing Hormone-releasing Hormone Agonists During the First Stage of the Prostate Adenocarcinoma Trans Cutaneous Hormones Trial (n=254).
| Outcomes | LHRHa group (n=85) | Estrogen-patch group (n=169) |
|---|---|---|
| Cardiovascular events * | ||
|
| ||
| Number of events (fatal events) | 6 (1) | 18 (5) |
|
| ||
| Number of patients with events | 6 | 17 |
|
| ||
| Proportion (95 % CI) of patients with events | 7.1 % (2.7–14.9) | 10.1 % (6.0–15.6) |
|
| ||
| Type of events (fatal events) | ||
| Heart failure | 0 | 3 (1) |
| Acute coronary syndrome | 2 (1) | 6 (1) |
| Thromboembolic stroke | 1 (0) | 4 (1) |
| Other arterial embolic event | 0 | 1 (1) |
| Venous thromboembolism | 3 (0) | 4 (1) |
|
| ||
| Testosterone levels at 3 months $ | ||
|
| ||
| Proportion (95 % CI) of patients that achieved castrate testosterone concentrations | 93 % (85–98) | 92 % (85–96) |
|
| ||
| Metabolic changes at 12 months from baseline $ | ||
|
| ||
| Fasting glucose | ||
| Mean change (range, mmol/l) | +0.33 (−2.0 to 6.9) | −0.16 (−1.9 to 2.4) |
| Percentage change | 5.5 % | −2.4 % |
| Treatment effect p value=0.004 | ||
|
| ||
| Fasting cholesterol | ||
| Mean change (range, mmol/l) | +0.20 (−2.9 to 1.9) | −0.23 (−3.1 to 1.9) |
| Percentage change | 4.1 % | −3.3 % |
| Treatment effect p value <0.0001 | ||
CI = confidence interval.
The primary cardiovascular analysis was based on a modified intention-to-treat approach: patients were included in the estrogen patch group if they had been treated with patches at any point, and were included in the luteinizing hormone-releasing hormone agonist (LHRHa) group if they had received LHRH but not patches at any point. Median follow-up was 19 months (interquartile range 12–31). The analysis was not powered to compare treatment groups.
Based on patients with data available who are still on allocated treatment without additional therapy. Reproduced from Langley et al.58
Potential Benefits of Androgen Deprivation Therapy with Parenteral Estrogen
Exogenous parenteral estrogen for ADT potentially offers two major therapeutic benefits. First, it appears to circumvent the CVS toxicity of oral estrogen by avoiding hepatic first-pass metabolism.56 Second, exogenous estrogen replaces endogenous estrogen, which would be lost through LHRHa administration.58 Thus exogenous estrogen as a single agent has the potential of being an effective and cost-effective therapy for PC, avoiding the need for further expensive treatment of conditions caused by LHRHa.
Bone Health
Estrogen preserves bone mass through its anti-resorptive actions mediated by estrogen receptors. It is known to inhibit osteoclastogenesis and increase osteoclast apoptosis. The life span of bone-resorptive osteoclasts is prolonged in estrogen deficiency, and the resultant imbalance between the bone-forming osteoblasts and osteoclasts increases the rate of bone thinning and heightens the risk for fracture. The protective effects of estrogen in bone health have been studied extensively in the context of the female menopause.59 In PC, two studies have reported the benefit of parenteral estrogen in preventing the skeletal side effects of ADT. In the pilot study of men treated with transdermal patches for newly diagnosed locally advanced or metastatic PC, of 12 baseline osteoporotic/osteopenic regions (in five patients), four showed improvement based on the World Health Organization grading after a year of therapy and bone mineral density increased at all measured sites over time.60 In the larger SPCG trial (n=910) with a follow-up of approximately 9 years, none of the patients on intramuscular PEP developed serious skeletal complications compared with 18 on combined androgen blockade (anti-androgen with either LHRHa or bilateral orchiectomy).59
Cognition
Estrogen receptors are present throughout the brain, including the cerebral cortex, hippocampus, and amygdala. These regions mediate memory and other cognitive functions, which are impaired in sex hormone deficiency state such as the menopause. Studies in menopausal women suggest that women who use hormone replacement therapy (HRT), with estrogen alone or in combination, have better cognitive skills and memory compared with age-matched non-users.61,62 The data on cognitive effects of parenteral estrogen in PC treatment are limited. In a small study, Beer et al. suggested potential beneficial effects of transdermal estradiol on specific cognitive aspects (verbal memory) in patients with castration-resistant PC.57
Metabolic Profile
It has been suggested that estrogen has a role in the protection from atherosclerosis as rates of CVS disease in premenopausal women are lower compared with men of the same age. Data from the nurses health study including over 29,000 women, also suggested early menopause increases the risk for CVS disease.63 In post-menopausal women CVS disease rates increase to attain similar rates as men of the same age. However, randomized data have not confirmed this association and HRT in post-menopausal women is not recommended for this indication.64 Beneficial arterial effects of estrogen may be mediated through an improved lipid profile as there is evidence that estrogen reduces low-density lipoprotein (LDL) and increases high-density lipoprotein (HDL).65 Similar favorable lipid changes have been observed with the use of parenteral estrogen as ADT for PC (see Table 1).21 Results from the PATCH trial showed that at 6 and 12 months, mean fasting cholesterol increased in the LHRHa arm but decreased in the estrogen arm, whereas HDL increased in both. Mean fasting glucose increased in the LHRHa group at 6 months and again further at 12 months but showed a decrease in the estrogen group at 6 months, which was maintained unchanged at 12 months. Whether these effects on exogenous hormones impact directly on cardiac risk is unclear, both for HRT and ADT.
Hot Flashes
Several studies have highlighted the role of estrogen in preventing and treating hot flashes.21 In one such study, a significant decline in hot flashes (77 % reduction; p<0.02) after 8 weeks in men receiving transdermal estradiol as second-line therapy for castration-resistant PC was observed.66
Conclusion
Long-term ADT is becoming increasingly common as men live longer with a diagnosis of PC. By creating both testosterone and estrogen deficiency, contemporary ADT with LHRHa causes a range of significant side effects. The large number of patients receiving LHRHa greatly amplifies the impact of this toxicity and have been under-estimated in the literature.67 The wide-ranging nature of these effects complicates discussion in clinical practice68 particularly if patients are older with multiple comorbidities.69 Understanding and preventing the consequences of contemporary ADT is vital to improve the QoL of these men. There are also significant financial implications for healthcare systems the world over. The re-emergence of estrogens, in parenteral form, offers an effective and inexpensive alternative to LHRHa. Parenteral estrogen avoids the thromboembolic and CVS toxicities associated with its oral counterpart. As a monotherapy, it has the potential to reduce or eliminate some of the serious complications of LHRHa, (osteoporosis, cognitive impairment, and hot flashes), which result in significant morbidity and mortality. Results from trials such as PATCH may establish parenteral estrogen as an important alternative to LHRHa in the management of PC. Until definitive results are available, effective monitoring is required so that timely prophylactic and/or therapeutic interventions can be instituted to mitigate the toxicities associated with LHRHa.
Footnotes
Disclosure: Paul Abel, MB ChB, FRCS, and Ruth E Langley, MBBS, MRCP, are co-chief investigators of the PATCH trial, which is an academic study funded by Cancer Research UK sponsored by the MRC Clinical Trials Unit at UCL. Iain Phillips, MBBS, MRCP, Syed I A Shah, MBBS, and Trinh Duong, MSc, have no conflicts of interest to declare.
References
- 1.Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29. doi: 10.3322/caac.20138. [DOI] [PubMed] [Google Scholar]
- 2.Silberstein J, Pal SK, Lewis B, Sartor O. Current clinical challenges in prostate cancer. Transl Androl Urol. 2013;2:122–36. doi: 10.3978/j.issn.2223-4683.2013.09.03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rehman Y, Rosenberg JE. Abiraterone acetate: oral androgen biosynthesis inhibitor for treatment of castration-resistant prostate cancer. Drug Des Devel Ther. 2012;6:13–8. doi: 10.2147/DDDT.S15850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Turo R, Smolski M, Esler R, et al. Diethylstilboestrol for the treatment of prostate cancer: past, present and future. Scand J Urol. 2013 Oct;32:1–11. doi: 10.3109/21681805.2013.861508. [DOI] [PubMed] [Google Scholar]
- 5.Bosset P-O, Albiges L, Seisen T, et al. Current role of diethylstilbestrol in the management of advanced prostate cancer. BJU Int. 2012;110(11 Pt C):E826–9. doi: 10.1111/j.1464-410X.2012.11206.x. [DOI] [PubMed] [Google Scholar]
- 6.Byar DP. The Veterans Administration Cooperative Urological Research Groups Studies of cancer of the prostate. Cancer. 1973;32:1126–30. doi: 10.1002/1097-0142(197311)32:5<1126::aid-cncr2820320518>3.0.co;2-c. [DOI] [PubMed] [Google Scholar]
- 7.Thomas BC, Neal DE. Androgen deprivation treatment in prostate cancer. BMJ. 2013;346:e8555. doi: 10.1136/bmj.e8555. [DOI] [PubMed] [Google Scholar]
- 8.Gomella LG. Effective testosterone suppression for prostate cancer: is there a best castration therapy? Rev Urol. 2009;11:52–60. [PMC free article] [PubMed] [Google Scholar]
- 9.Bourke L, Kirkbride P, Hooper R, et al. Endocrine therapy in prostate cancer: time for reappraisal of risks, benefits and cost-effectiveness? Br J Cancer. 2013;108:9–13. doi: 10.1038/bjc.2012.523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Oudard S. Progress in emerging therapies for advanced prostate cancer. Cancer Treat Rev. 2013;39:275–89. doi: 10.1016/j.ctrv.2012.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Sharifi N, Gulley JL, Dahut WL. An update on androgen deprivation therapy for prostate cancer. Endocr Relat Cancer. 2010;17:R305–15. doi: 10.1677/ERC-10-0187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mazzola CR, Mulhall JP. Impact of androgen deprivation therapy on sexual function. Asian J Androl. 2012;14:198–203. doi: 10.1038/aja.2011.106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ockrim JL, Abel PD. Long term androgen deprivation therapy in prostate cancer. BMJ. 2008;337:a1361. doi: 10.1136/bmj.a1361. [DOI] [PubMed] [Google Scholar]
- 14.Beebe-Dimmer JL, Freedland SJ. Androgen deprivation therapy: further confirmation of known harms. BJU Int. 2013;111:690–1. doi: 10.1111/j.1464-410X.2013.11797.x. [DOI] [PubMed] [Google Scholar]
- 15.Walker LM, Tran S, Robinson JW. Luteinizing hormone-releasing hormone agonists: a quick reference for prevalence rates of potential adverse effects. Clin Genitourin Cancer. 2013;11:375–84. doi: 10.1016/j.clgc.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 16.Trost LW, Serefoglu E, Gokce A, et al. Androgen deprivation therapy impact on quality of life and cardiovascular health, monitoring therapeutic replacement. J Sex Med. 2013;10(Suppl. 1):84–101. doi: 10.1111/jsm.12036. [DOI] [PubMed] [Google Scholar]
- 17.Saylor PJ, Smith MR. Adverse effects of androgen deprivation therapy: defining the problem and promoting health among men with prostate cancer. J Natl Compr Canc Netw. 2010;8:211–23. doi: 10.6004/jnccn.2010.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ahmadi H, Daneshmand S. Androgen deprivation therapy: evidence-based management of side effects. BJU Int. 2013;111:543–8. doi: 10.1111/j.1464-410X.2012.11774.x. [DOI] [PubMed] [Google Scholar]
- 19.The Leuprolide Study Group Leuprolide versus diethylstilbestrol for metastatic prostate cancer. N Engl J Med. 1984;311:1281–6. doi: 10.1056/NEJM198411153112004. [DOI] [PubMed] [Google Scholar]
- 20.Garnick MB. Leuprolide versus diethylstilbestrol for previously untreated stage D2 prostate cancer. Results of a prospectively randomized trial. Urology. 1986;27(Suppl. 1):21–8. [PubMed] [Google Scholar]
- 21.Freedland SJ, Eastham J, Shore N. Androgen deprivation therapy and estrogen deficiency induced adverse effects in the treatment of prostate cancer. Prostate Cancer Prostatic Dis. 2009;12:333–8. doi: 10.1038/pcan.2009.35. [DOI] [PubMed] [Google Scholar]
- 22.Elliott S, Latini DM, Walker LM, et al. Androgen deprivation therapy for prostate cancer: recommendations to improve patient and partner quality of life. J Sex Med. 2010;7:2996–3010. doi: 10.1111/j.1743-6109.2010.01902.x. [DOI] [PubMed] [Google Scholar]
- 23.Finkelstein JS, Lee H, Burnett-Bowie S-AM, et al. Gonadal steroids and body composition, strength, and sexual function in men. N Engl J Med. 2013;369:1011–22. doi: 10.1056/NEJMoa1206168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Raji A, Seely EW, Arky RA, Simonson DC. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab. 2001;86:5366–71. doi: 10.1210/jcem.86.11.7992. [DOI] [PubMed] [Google Scholar]
- 25.Smith MR. Androgen deprivation therapy for prostate cancer: new concepts and concerns. Curr Opin Endocrinol Diabetes Obes. 2007;14:247–54. doi: 10.1097/MED.0b013e32814db88c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morrison BF, Burrowes IE, Aiken WD, et al. Bone mineral density in Jamaican men on androgen deprivation therapy for prostate cancer. Infect Agent Cancer. 2011;6(Suppl. 2):S7. doi: 10.1186/1750-9378-6-S2-S7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Greenspan SL, Wagner J, Nelson JB, et al. Vertebral fractures and trabecular microstructure in men with prostate cancer on androgen deprivation therapy. J Bone Miner Res. 2013;28:325–32. doi: 10.1002/jbmr.1771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Shao Y-H, Moore DF, Shih W, et al. Fracture after androgen deprivation therapy among men with a high baseline risk of skeletal complications. BJU Int. 2013;111:745–52. doi: 10.1111/j.1464-410X.2012.11758.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nishimura K, Yamaguchi Y, Yamanaka M, et al. Climacteric-like disorders in prostate cancer patients treated with LHRH agonists. Arch Androl. 2005;51:41–8. doi: 10.1080/014850190513003. [DOI] [PubMed] [Google Scholar]
- 30.Yamaguchi N, Okajima Y, Fujii T, et al. The efficacy of nonestrogenic therapy to hot flashes in cancer patients under hormone manipulation therapy: a systematic review and meta-analysis. J Cancer Res Clin Oncol. 2013;139:1701–7. doi: 10.1007/s00432-013-1491-4. [DOI] [PubMed] [Google Scholar]
- 31.Grunfeld EA, Halliday A, Martin P, Drudge-Coates L. Andropause syndrome in men treated for metastatic prostate cancer: a qualitative study of the impact of symptoms. Cancer Nurs. 2002;35:63–9. doi: 10.1097/NCC.0b013e318211fa92. [DOI] [PubMed] [Google Scholar]
- 32.Bagrodia A, Diblasio CJ, Wake RW, Derweesh IH. Adverse effects of androgen deprivation therapy in prostate cancer: Current management issues. Indian J Urol. 2009;25:169–76. doi: 10.4103/0970-1591.52907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Savard J, Hervouet S, Ivers H. Prostate cancer treatments and their side effects are associated with increased insomnia. Psychooncology. 2013;22:1381–8. doi: 10.1002/pon.3150. [DOI] [PubMed] [Google Scholar]
- 34.Janowsky JS. The role of androgens in cognition and brain aging in men. Neuroscience. 2006;138:1015–20. doi: 10.1016/j.neuroscience.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 35.Jamadar RJ, Winters MJ, Maki PM. Cognitive changes associated with ADT: a review of the literature. Asian J Androl. 2012;14:232–8. doi: 10.1038/aja.2011.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nelson CJ, Lee JS, Gamboa MC, Roth AJ. Cognitive effects of hormone therapy in men with prostate cancer: a review. Cancer. 2008;113:1097–106. doi: 10.1002/cncr.23658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Alibhai SMH, Breunis H, Timilshina N, et al. Impact of androgen-deprivation therapy on cognitive function in men with nonmetastatic prostate cancer. J Clin Oncol. 2010;28:5030–7. doi: 10.1200/JCO.2010.30.8742. [DOI] [PubMed] [Google Scholar]
- 38.Cherrier MM, Borghesani PR, Shelton AL, Higano CS. Changes in neuronal activation patterns in response to androgen deprivation therapy: a pilot study. BMC Cancer. 2010;10:1. doi: 10.1186/1471-2407-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chao HH, Uchio E, Zhang S, et al. Effects of androgen deprivation on brain function in prostate cancer patients – a prospective observational cohort analysis. BMC Cancer. 2012;12:371. doi: 10.1186/1471-2407-12-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chao HH, Hu S, Ide JS, et al. Effects of androgen deprivation on cerebral morphometry in prostate cancer patients – an exploratory study. PLoS One. 2013;8:e72032. doi: 10.1371/journal.pone.0072032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Corona G, Gacci M, Baldi E, et al. Androgen deprivation therapy in prostate cancer: focusing on sexual side effects. J Sex Med. 2012;9:887–902. doi: 10.1111/j.1743-6109.2011.02590.x. [DOI] [PubMed] [Google Scholar]
- 42.Casey RG, Corcoran NM, Goldenberg SL. Quality of life issues in men undergoing androgen deprivation therapy: a review. Asian J Androl. 2012;14:226–31. doi: 10.1038/aja.2011.108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Higano CS. Sexuality and intimacy after definitive treatment and subsequent androgen deprivation therapy for prostate cancer. J Clin Oncol. 2012;30:3720–5. doi: 10.1200/JCO.2012.41.8509. [DOI] [PubMed] [Google Scholar]
- 44.Navon L, Morag A. Advanced prostate cancer patients’ relationships with their spouses following hormonal therapy. Eur J Oncol Nurs. 2003;7:73–80. doi: 10.1016/s1462-3889(03)00022-x. discussion 81-2. [DOI] [PubMed] [Google Scholar]
- 45.Wibowo E, Wassersug R, Warkentin K, et al. Impact of androgen deprivation therapy on sexual function: a response. Asian J Androl. 2012;14:793–4. doi: 10.1038/aja.2012.60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cleffi S, Neto AS, Reis LO, et al. Androgen deprivation therapy and morbid obesity: do they share cardiovascular risk through metabolic syndrome? Actas Urol Españolas. 2011;35:259–65. doi: 10.1016/j.acuro.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 47.Smith MR, Saad F, Egerdie B, et al. Sarcopenia during androgen-deprivation therapy for prostate cancer. J Clin Oncol. 2012;30:3271–6. doi: 10.1200/JCO.2011.38.8850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alibhai SMH, Breunis H, Timilshina N, et al. Impact of androgen-deprivation therapy on physical function and quality of life in men with nonmetastatic prostate cancer. J Clin Oncol. 2010;28:5038–45. doi: 10.1200/JCO.2010.29.8091. [DOI] [PubMed] [Google Scholar]
- 49.Lapi F, Azoulay L, Niazi MT, et al. Androgen deprivation therapy and risk of acute kidney injury in patients with prostate cancer. JAMA. 2013;310:289–96. doi: 10.1001/jama.2013.8638. [DOI] [PubMed] [Google Scholar]
- 50.Keating NL, O’Malley AJ, Smith MR. Diabetes and cardiovascular disease during androgen deprivation therapy for prostate cancer. J Clin Oncol. 2006;24:4448–56. doi: 10.1200/JCO.2006.06.2497. [DOI] [PubMed] [Google Scholar]
- 51.Efstathiou JA, Bae K, Shipley WU, et al. Cardiovascular mortality after androgen deprivation therapy for locally advanced prostate cancer: RTOG 85-31. J Clin Oncol. 2009;27:92–9. doi: 10.1200/JCO.2007.12.3752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Albertsen PC, Klotz L, Tombal B, et al. Cardiovascular morbidity associated with gonadotropin releasing hormone agonists and an antagonist. Eur Urol. 2014;65:565–73. doi: 10.1016/j.eururo.2013.10.032. [DOI] [PubMed] [Google Scholar]
- 53.Von Schoultz B, Carlström K, Collste L, et al. Estrogen therapy and liver function—metabolic effects of oral and parenteral administration. Prostate. 1989;14:389–95. doi: 10.1002/pros.2990140410. [DOI] [PubMed] [Google Scholar]
- 54.Hedlund PO, Damber J-E, Hagerman I, et al. Parenteral estrogen versus combined androgen deprivation in the treatment of metastatic prostatic cancer: part 2. Final evaluation of the Scandinavian Prostatic Cancer Group (SPCG) Study No. 5. Scand J Urol Nephrol. 2008;42:220–9. doi: 10.1080/00365590801943274. [DOI] [PubMed] [Google Scholar]
- 55.Wassersug RJ. Extending the case for oestradiol in androgen-sensitive prostate cancer. Lancet Oncol. 2013;14:e252–3. doi: 10.1016/S1470-2045(13)70120-7. [DOI] [PubMed] [Google Scholar]
- 56.Ockrim JL, Lalani E-N, Kakkar AK, Abel PD. Transdermal estradiol therapy for prostate cancer reduces thrombophilic activation and protects against thromboembolism. J Urol. 2005;174:527–33. doi: 10.1097/01.ju.0000165567.99142.1f. discussion 532-3. [DOI] [PubMed] [Google Scholar]
- 57.Beer TM, Bland LB, Bussiere JR, et al. Testosterone loss and estradiol administration modify memory in men. J Urol. 2006;175:130–5. doi: 10.1016/S0022-5347(05)00049-2. [DOI] [PubMed] [Google Scholar]
- 58.Langley RE, Cafferty FH, Alhasso AA, et al. Cardiovascular outcomes in patients with locally advancedand metastatic prostate cancer treated with luteinising hormone-releasing-hormone agonists or transdermal oestrogen: the randomised, phase 2 MRC PATCH trial (PR09) Lancet Oncol. 2013;14:306–16. doi: 10.1016/S1470-2045(13)70025-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Frenkel B, Hong A, Baniwal SK, et al. Regulation of adult bone turnover by sex steroids. J Cell Physiol. 2010;224:305–10. doi: 10.1002/jcp.22159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ockrim JL, Lalani EN, Banks LM, et al. Transdermal estradiol improves bone density when used as single agent therapy for prostate cancer. J Urol. 2004;172(6 Pt 1):2203–7. doi: 10.1097/01.ju.0000145511.56476.00. [DOI] [PubMed] [Google Scholar]
- 61.Genazzani AR, Pluchino N, Luisi S, Luisi M. Estrogen, cognition and female ageing. Hum Reprod Update. 2007;13:175–87. doi: 10.1093/humupd/dml042. [DOI] [PubMed] [Google Scholar]
- 62.LeBlanc ES, Janowsky J, Chan BK, Nelson HD. Hormone replacement therapy and cognition: systematic review and meta-analysis. JAMA. 2001;285:1489–99. doi: 10.1001/jama.285.11.1489. [DOI] [PubMed] [Google Scholar]
- 63.Parker WH, Broder MS, Chang E, et al. Ovarian conservation at the time of hysterectomy and long-term health outcomes in the nurses’ health study. Obstet Gynecol. 2009;113:1027–37. doi: 10.1097/AOG.0b013e3181a11c64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Yang X-P, Reckelhoff J. Estrogen, hormone replacement therapy and cardiovascular disease. Curr Opin Nephrol Hypertens. 2011;20:133–8. doi: 10.1097/MNH.0b013e3283431921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bracamonte MP, Miller VM. Vascular effects of estrogens: arterial protection versus venous thrombotic risk. Trends Endocrinol Metab. 2001;12:204–9. doi: 10.1016/s1043-2760(01)00406-4. [DOI] [PubMed] [Google Scholar]
- 66.Bland LB, Garzotto M, DeLoughery TG, et al. Phase II study of transdermal estradiol in androgen-independent prostate carcinoma. Cancer. 2005;103:717–23. doi: 10.1002/cncr.20857. [DOI] [PubMed] [Google Scholar]
- 67.Phillips JL, Wassersug RJ, McLeod DL. Systemic bias in the medical literature on androgen deprivation therapy and its implication to clinical practice. Int J Clin Pract. 2012;66:1189–96. doi: 10.1111/ijcp.12025. [DOI] [PubMed] [Google Scholar]
- 68.Tran S, Walker LM, Wassersug RJ, et al. What do Canadian uro-oncologists believe patients should know about androgen deprivation therapy? J Oncol Pharm Pract. 2013 doi: 10.1177/1078155213495285. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 69.Cheung AS, Pattison D, Bretherton I, et al. Cardiovascular risk and bone loss in men undergoing androgen deprivation therapy for non-metastatic prostate cancer: implementation of standardized management guidelines. Andrology. 2013;1:583–9. doi: 10.1111/j.2047-2927.2013.00093.x. [DOI] [PubMed] [Google Scholar]