Abstract
A case of Malassezia pachydermatis fungemia in a preterm neonate is described. The isolate was identified by rDNA sequencing and was resistant to fluconazole and flucytosine. Since M. pachydermatis does not require lipid supplementation for growth, it can be misidentified as a Candida species. The report highlights M. pachydermatis as a cause of late onset sepsis in preterm neonates and emphasizes the need for prior antifungal susceptibility testing.
Keywords: Malassezia pachydermatis, Preterm neonate, Fungemia, Fluconazole resistance
1. Introduction
The genus Malassezia, currently comprises 14 lipophilic yeast species [1–3]. Among them, M. pachydermatis is uniquely placed, primarily being a zoopathogen with ability to grow without oil enrichment. The species forms normal microbiota of the skin and ear canal of dogs, cats, and other canines, where it causes dermatitis and otitis externa [4,5]. M. pachyderamtis has also been isolated from healthy and diseased human skin [6], whereas in neonates, it is associated with fungemia [7–9]. Here, we describe a case of M. pachydermatis fungemia in a pre-term neonate.
2. Case
At 26 weeks of gestation, a baby boy, weighing 710 g, was delivered by emergency caesarian section to a 30-year-old Egyptian female. On day 0 (day of birth), the baby had symptoms of respiratory distress syndrome, although the mother was on oral steroids. His Apgar score was 5 at one minute after birth and 9 after 5 min. The mother had previous history of multiple abortions and neonatal deaths. The baby was admitted to Neonatal Intensive Care Unit (NICU) and put on ventilator and umbilical venous catheter was inserted for giving total parenteral nutrition (TPN). Since he had abdominal distension, a vacuum-assisted closure device was also used. His cardiovascular and central nervous systems were functioning normally. Although there were no positive blood cultures, the baby was prescribed ampicillin and amikacin for 7 days to prevent sepsis due to necrotizing enterocolitis. On day 18, as the baby became febrile, the treatment was switched to Tazocin® (piperacillin and tazobactam) for 10 days. Blood culture taken on day 22, however, grew a yeast (isolate no. Kw1247/13) in BACTEC blood culture bottle after nearly 5 days of incubation. Consequently, on day 26, the baby was started on liposomal amphotericin B (Abelcet). The subsequent blood cultures taken on days 30 and 33 after birth became negative for the yeast and the patient recovered completely and was discharged.
The subculture from BACTEC blood culture bottles yielded slow-growing, cream-colored colonies on Sabouraud dextrose agar (SDA) and blood agar without lipid supplementation. On SDA at 30 °C, colonies were convex, cream-colored, 2–3 mm in diameter with entire margins. Microscopically, yeast cells were ovoid to elongated with monopolar budding, measuring 4–6 µm×2.8–4 µm in size. No hyphal forms were observed. The identity of the isolate was determined as Malassezia furfur by Vitek 2 Yeast identification system (bioMeriux, France) with 98% probability (excellent identification, bionumber 4000100002000100). Since the isolate grew without lipid enrichment, it required molecular identification. Sequencing of the ITS and D1/D2 regions of rDNA was carried out according to previously described methods [10,11] to confirm the identity of the isolate (Kw1247/13). The DNA sequencing data for the D1/D2 region showed only three nucleotide differences with reference strain M. pachydermatis CBS1879. Based on the observations that conspecific strains exhibit <1% sequence difference in the D1/D2 region of 28S rRNA, the identity of the isolate was established as M. pachydermatis [11,12]. The identity of the isolates was also confirmed by matrix-assisted laser desorption and ionization–time-of-flight mass spectrometry (MALDI–TOF MS; bioMeriuex) as M. pachydermatis with 99.9% confidence value.
Minimum inhibitory concentrations (MICs) for antifungal drugs were determined by Etest on RPMI 1640 medium supplemented with 2% glucose as described previously [10] after swabbing the surface with olive oil. The MICs read at 48 h of incubation at 35 °C and were scored as susceptible to amphotericin B, 0.19 µg/ml; voriconazole, 0.012 µg/ml and posaconazole, 0.016 µg/ml; but showed reduced susceptibility (resistance) to fluconazole, ≥256 µg/ml; flucytosine, ≥32 µg/ml; and caspofungin, ≥32 µg/ml (Table 1, Fig. 1).
Table 1.
Antifungal susceptibility of M. pachydermatis strain by Etest.
| Medium |
Minimum inhibitory concentrations (µg/ml) read at 48 h |
|||||
|---|---|---|---|---|---|---|
| AP | VO | POS | FL | FC | CS | |
| RPMI medium 1640a | 0.19 | 0.012 | 0.016 | ≥256 | ≥32 | ≥32 |
| Sabouraud dextrose Agar | 0.25 | 0.19 | 0.016 | ≥256 | ≥32 | ≥32 |
Supplemented with 2% glucose and overlaid with olive oil. Abbreviations: AP—amphotericin B, VO—voriconazole, POS—posaconazole, FL—fluconazole, FC—flucytosine, CS—caspofungin.
Fig. 1.
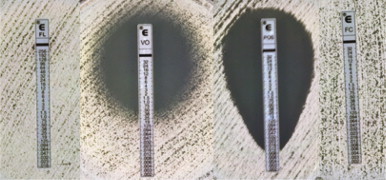
EtestS on Sabouraud dextrose agar showing minimum inhibitory concentrations for fluconazole (FL, ≥256 µg/ml), voriconazole (VO, 0.012 µg/ml), posaconazole (POS, 0.016 µg/ml) and flucytosine (FC, ≥32 µg/ml) read after 48 h of incubation at 35 °C.
3. Discussion
Malassezia spp. are known etiologic agents of pityriasis versicolor and are normally present on skin without clinical manifestations [1–3]. However, in view of their close association with human skin, M. furfur and some other species of the genus may cause systemic infection, particularly in severely ill patients receiving TPN with lipid enrichment [3]. Although, M. pachydermatis does not require lipid supplementation for growth, it is lipophilic and like other members of the genus, has the potential to cause systemic infection in preterm neonates and adults [1,8,13,14]. There are several reports of M. pachydermatis fungemia in preterm, low birth-weight neonates, who received TPN through central venous catheter [7–9]. The other risk factors associated with M. pachydermatis fungemia include increased median neonatal acute physiology score, >9 days of arterial catheterization and contact with healthcare staff harboring the organism [15].
Although M. pachydermatis is primarily a zoopathogen, there is evidence to suggest that M. pachydermatis strains may be introduced in NICU through the hands of health care staff who own dogs [15]. In a recent study, using PCR-based method, 93% of dog owners had M. pachydermatis carriage on their hands [16]. We have not investigated the source of origin of our isolate. In Kuwait, population density of dogs is low and keeping them as pets is rare, whereas domestic and stray cats are not uncommon. A recent study from north-west India (Punjab) reported that about 5% of the isolates of M. pachydermatis were obtained from the back of healthy individuals without evidence of pityriasis versicolor [17]. This observation is noteworthy as it suggests that M. pachdermatis fungemia may also have similar mode of acquisition as for candidemia.
Because of the ability of M. pachydermatis to grow without oil enrichment, it can be misidentified as a Candida species, which may lead to inappropriate antifungal therapy, particularly when Malessezia spp. are known to be intrinsically resistant to echinocandins. As observed in our isolate, most strains of M. pachydermatis exhibit reduced susceptibility to fluconazole and flucytosine [7,18–23]. However, in contrast to some other studies, where cross-resistance between azoles has been reported among veterinary strains [19,22,23], our isolate appeared susceptible to voriconazole and posaconazole (Table 1).
A limitation of the study is that we determined MICs by Etest and not by CLSI microdilution method, although both the tests have shown high categorical agreement [18]. Our isolate showed suboptimal growth on RPMI 1640 medium even with lipid supplementation, hence MIC readings were taken after 48 h [24]. Since our isolate did not grow on Mueller–Hinton medium (with or without oil supplementation), MICs were also determined on SDA for confirming results (Table 1). Optimal conditions for determining susceptibility and antifungal breakpoints for Malassezia spp. are not yet established.
In conclusion, a case of M. pachydermatis fungemia is described. The identity of the isolate was confirmed by sequencing of rDNA. The isolate was resistant to fluconazole and flucytosine. The report highlights the need of species-specific identification and prior antifungal susceptibility testing for appropriate management. This appears to be the first report of M. pachydermatis fungemia from Kuwait and the Middle East.
Nucleotide sequence accession numbers
Sequences obtained for the ITS and D1/D2 regions of rDNA of our isolate were deposited in GenBank under accession numbers HG529981 and HG532009, respectively.
Conflict of interest
There are none.
Acknowledgments
The authors are thankful to Ms. Sandhya Vayalil and Rachel Chandy for excellent technical support.
References
- 1.Gaitanis G., Magiatis P., Hantschke M., Bassukas I.D., Velegraki A. The Malassezia genus in skin and systemic diseases. Clin Microbiol Rev. 2012;25:106–141. doi: 10.1128/CMR.00021-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Saunders C.W., Scheynius A., Heitman J. Malassezia fungi are specialized to live on skin and associated with dandruff, eczema, and other skin Diseases. PLoS Pathog. 2012;8:e1002701. doi: 10.1371/journal.ppat.1002701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tragiannidis A., Bisping G., Koehler G., Groll A.H. Minireview: Malassezia infections in immunocompromised patients. Mycoses. 2010;53:187–195. doi: 10.1111/j.1439-0507.2009.01814.x. [DOI] [PubMed] [Google Scholar]
- 4.Chen T.A., Hill P.B. The biology of Malassezia organisms and their ability to induce immune responses and skin disease. Vet Dermatol. 2005;16:4–26. doi: 10.1111/j.1365-3164.2005.00424.x. [DOI] [PubMed] [Google Scholar]
- 5.Nuttall T., Harvey R.G., McKeever P.J. Manson Publishing Ltd.; London: 2009. Malassezia dermatitis. A color handbook of skin diseases of the dog and cat; pp. 57–59. [Google Scholar]
- 6.Prohic A., Kasumagic-Halilovic E. Identification of Malassezia pachydermatis from healthy and diseased human skin. Med Arh. 2009;63:317–319. [PubMed] [Google Scholar]
- 7.Chryssanthou E., Broberger U., Petrini B. Malassezia pachydermatis fungaemia in a neonatal intensive care unit. Acta Paediatr. 2001;90:323–327. [PubMed] [Google Scholar]
- 8.Larocco M., Dorenbaum A., Robinson A., Pickering L.K. Recovery of Malassezia pachydermatis from eight infants in a neonatal intensive care nursery: clinical and laboratory features. Pediatr Infect Dis J. 1988;7:398–401. doi: 10.1097/00006454-198806000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Welbel S.F., McNeil M.M., Pramanik A., Silberman R., Oberle A.D., Midgley G. Nosocomial Malassezia pachydermatis bloodstream infections in a neonatal intensive care unit. Pediatr Infect Dis J. 1994;13:104–108. doi: 10.1097/00006454-199402000-00005. [DOI] [PubMed] [Google Scholar]
- 10.Al-Sweih N., Ahmad S., Khan Z.U., Khan S., Chandy R. Prevalence of Candida dubliniensis among germ tube-positive Candida isolates in a maternity hospital in Kuwait. Mycoses. 2005;48:347–351. doi: 10.1111/j.1439-0507.2005.01143.x. [DOI] [PubMed] [Google Scholar]
- 11.Khan Z.U., Ahmad S., Hagen F., Fell J.W., Kowshik T., Chandy R. Cryptococcus randhawai sp. nov., a novel anamorphic basidiomycetous yeast isolated from tree trunk hollow of Ficus religiosa (peepal tree) from New Delhi, India. Antonie Van Leeuwenhoek. 2010;97:253–259. doi: 10.1007/s10482-009-9406-8. [DOI] [PubMed] [Google Scholar]
- 12.Khan Z.U., Ahmad S., Mokaddas E., Chandy R., Cano J., Guarro J. Actinomucor elegans var. kuwaitiensis isolated from the wound of a diabetic patient. Antonie Van Leeuwenhoek. 2008;94:343–352. doi: 10.1007/s10482-008-9251-1. [DOI] [PubMed] [Google Scholar]
- 13.Lautenbach E., Nachamkin I., Schuster M.G. Malassezia pachydermatis infections. N Engl J Med. 1998;339:270. doi: 10.1056/NEJM199807233390414. [DOI] [PubMed] [Google Scholar]
- 14.Mickelsen P.A., Viano-Paulson M.C., Stevens D.A., Diaz P.S. Clinical and microbiological features of infection with Malassezia pachydermatis in high-risk infants. J Infect Dis. 1988;157:1163–1168. doi: 10.1093/infdis/157.6.1163. [DOI] [PubMed] [Google Scholar]
- 15.Chang H.J., Miller H.L., Watkins N., Arduino M.J., Ashford D.A., Midgley G. An epidemic of Malassezia pachydermatis in an intensive care nursery associated with colonization of health care workers’ pet dogs. N Engl J Med. 1998;338:706–711. doi: 10.1056/NEJM199803123381102. [DOI] [PubMed] [Google Scholar]
- 16.Morris D.O., O’Shea K., Shofer F.S., Rankin S. Malassezia pachydermatis carriage in dog owners. Emerg Infect Dis. 2005;11:83–88. doi: 10.3201/eid1101.040882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaur M., Narang T., Bala M., Gupte S., Aggarwal P., Manhas A. Study of the distribution of Malassezia species in patients with pityriasis versicolor and healthy individuals in Tertiary Care Hospital, Punjab. Indian J Med Microbiol. 2013;31:270–274. doi: 10.4103/0255-0857.115636. [DOI] [PubMed] [Google Scholar]
- 18.Cafarchia C., Figueredo L.A., Iatta R., Colao V., Montagna M.T., Otranto D. in vitro evaluation of Malassezia pachydermatis susceptibility to azole compounds using E-test and CLSI microdilution methods. Med Mycol. 2012;50:795–801. doi: 10.3109/13693786.2012.674219. [DOI] [PubMed] [Google Scholar]
- 19.Cafarchia C., Figueredo L.A., Iatta R., Montagna M.T., Otranto D. in vitro antifungal susceptibility of Malassezia pachydermatis from dogs with and without skin lesions. Vet Microbiol. 2012;155:395–398. doi: 10.1016/j.vetmic.2011.09.008. [DOI] [PubMed] [Google Scholar]
- 20.Carrillo-Muñoz A.J., Rojas F., Tur-Tur C., de Los Ángeles Sosa M., Diez G.O., Espada C.M. in vitro antifungal activity of topical and systemic antifungal drugs against Malassezia species. Mycoses. 2013;56:571–575. doi: 10.1111/myc.12076. [DOI] [PubMed] [Google Scholar]
- 21.Garau M., Pereiro M., Jr., del Palacio A.m. in vitro susceptibilities of Malassezia species to a new triazole, albaconazole (UR-9825), and other antifungal compounds. Antimicrob Agents Chemother. 2003;47:2342–2344. doi: 10.1128/AAC.47.7.2342-2344.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jesus F.P., Lautert C., Zanette R.A., Mahl D.L., Azevedo M.I., Machado M.L. in vitro susceptibility of fluconazole-susceptible and -resistant isolates of Malassezia pachydermatis against azoles. Vet Microbiol. 2011;152:161–164. doi: 10.1016/j.vetmic.2011.04.027. [DOI] [PubMed] [Google Scholar]
- 23.Nijima M., Kano R., Nagata M., Hasegawa A., Kamata H. An azole-resistant isolate of Malassezia pachydermatis. Vet Microbiol. 2011;149:288–290. doi: 10.1016/j.vetmic.2010.10.010. [DOI] [PubMed] [Google Scholar]
- 24.Cafarchia C., Figueredo L.A., Favuzzi V., Surico M.R., Colao V., Iatta R. Assessment of the antifungal susceptibility of Malassezia pachydermatis in various media using a CLSI protocol. Vet Microbiol. 2012;159:536–540. doi: 10.1016/j.vetmic.2012.04.034. [DOI] [PubMed] [Google Scholar]


