Abstract
Cells of the myocardium are at home in one of the most mechanically dynamic environments in the body. At the cellular level, pulsatile stimuli of chamber filling and emptying are experienced as cyclic strains (relative deformation) and stresses (force per unit area). The intrinsic characteristics of tension-generating myocytes and fibroblasts thus have a continuous mechanical interplay with their extrinsic surroundings. This review explores the ways that the micromechanics at the scale of single cardiac myocytes and fibroblasts have been measured, modeled, and recapitulated in vitro in the context of adaptation. Both types of cardiac cells respond to externally applied strain, and many of the intracellular mechanosensing pathways have been identified with the careful manipulation of experimental variables. In addition to strain, the extent of loading in myocytes and fibroblasts is also regulated by cues from the microenvironment such as substrate surface chemistry, stiffness, and topography. Combinations of these structural cues in 3D are needed to mimic the micromechanical complexity derived from the extracellular matrix of the developing, healthy, or pathophysiologic heart. An understanding of cardiac cell micromechanics can therefore inform the design and composition of tissue engineering scaffolds or stem cell niches for future applications in regenerative medicine.
Keywords: strain, stress, myocardium, hypertrophy, cell tracking, muscle model
Introduction
Cells of the myocardium are at home in one of the most mechanically dynamic environments in the body. Heart chamber filling and wall distention within diastole account for rapid changes in pressure and volume that are released by the wave of contraction that pumps blood through the body [72]. At the cellular level, these pulsatile stimuli are experienced as cyclic strains (relative deformation) and stresses (force per unit area). The heart consists predominantly of matrix-depositing fibroblasts by number and striated myocytes by volume [100]. In myocytes, contractile forces are produced through the sliding of actin and myosin filaments in sarcomeres, as triggered by action potentials and intracellular calcium signals. Actomyosin-based forces are also developed in fibroblasts from stress cables, though the structure, assembly, composition, and contractile profile of these differ from myofibers. Active tension in both cell types is also generated from microtubules, while passive tension can be established from cytoplasmic viscosity, intermediate filaments, muscle-specific titin filaments, and properties of the surrounding extracellular matrix (ECM) [52, 104]. Altogether, such mechanics determine the extent of myocardial cell loading, which for myocytes has been distinguished physiologically with clinical assessments of a preload (relating to end-diastolic volume or pressure) or afterload (left ventricular end-systolic wall stress). Though the use of these terms vary, preload and afterload are often defined at the single cell level as the strain subjected to myocytes before contraction and the resistance encountered during contraction, respectively [106].
For most of the body, the proliferative potential of cells contributes to organ growth. However, myocytes do not divide in the post-embryonic heart; instead a progenitor pool is thought to replace a limited number of dead myocytes with new ones [98]. Therefore, adaptation to meet new mechanical demands and maintain cardiac function is most readily achieved by myocyte hypertrophy, an increase in cell size and protein content due to the parallel or in-series addition of myofilaments. Such elongation or thickening of myocytes typically occurs in an attempt to normalize tissue stresses following pressure or volume overload or a segmental loss of the myocardium [119]. Apart from changes in contractile protein mass, mechanical loading can also affect cytoskeletal or sarcomeric organization to regulate cell shape and alignment [30, 51]. Collectively, these responses make up a large part of the pathological and physiological remodeling processes that exist in the heart, in which a mechanical balance is sought between cardiac cell architecture and the effective transmission of forces [31].
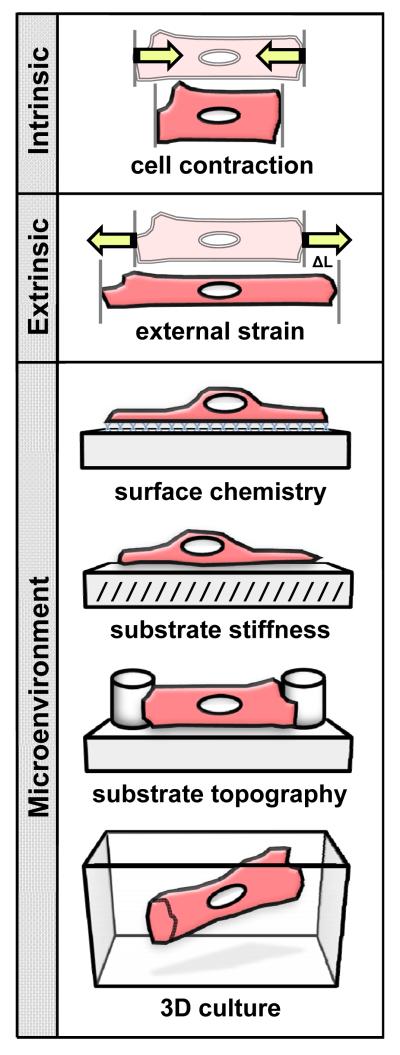
Cardiac myocyte function is governed by fundamental mechanisms of excitation, contraction, and energy consumption. For example, the Frank-Starling law describes the relationship between muscle length and active tension [2]. In the heart, as the myocardium is stretched by ventricular filling, the ability to develop pressure is altered. Such a mechanism illustrates the adaptive control built into myocytes for the recognition of mechanics-based loads [85, 117]. The intrinsic characteristics of myocytes have continuous interplay with the extrinsic dynamics and surroundings. Consequently, variables related to the tension, scale, topography, or rigidity of a cellular domain in vitro can be used to mimic a preload or afterload and explore how contractile machinery engages and remodels (see Fig. 1).
Fig. 1.
Contributions to micromechanical loading in cardiac myocytes. Contractile activity creates an intrinsic load in cardiac myocytes. Extrinsic loading may be applied through external strain (ΔL) to simulate a preload. The microenvironment influences the afterload of tension-generating cells in vitro and can be controlled through the surface chemistry, stiffness, topography, or three-dimensionality of a culture substrate
Numerous temporal and biochemical properties play a part in the mechanics of contractile cells [32]. The following review examines some of the dimensional or structural properties involved in the micromechanics within myocytes and fibroblasts to regulate cardiac cell behavior and function. The literature covered, however, is by no means complete. Rather, this work focuses on how micromechanical stimuli have been measured, sensed, and recapitulated in cardiac myocytes and fibroblasts in order to study their effect on cellular and subcellular organization. The basic approaches discussed are aimed at understanding which micromechanical aspects are important to principles of cardiac cell and tissue engineering in vitro and myocardial remodeling under various pathophysiological conditions in vivo.
Measurement of Cellular Micromechanics
Innovative methods are needed to measure contractile dynamics, given that the micromechanics of cardiac myocytes and fibroblasts can vary under certain stimuli or loads. Such techniques frequently rely on sensitive detection of motion or force, whether a direct or indirect result of muscle activity. In the intact heart, the mechanical response of functioning myocardium has been successfully measured in clinical settings through noninvasive uses of magnetic resonance imaging, echocardiography, or more specialized derivations of each [35, 99, 125, 151]. Recent advances in these techniques have permitted detailed recording of radial, longitudinal, and circumferential motions of the heart with high sampling rates to arrive at near real-time assessments of strain amplitude, strain rate, and local elasticity that approach the microscale [3, 25, 84]. The scale of these data have diagnostic implications, as regional differences in strain can be used to identify areas of ischemia, diseased tissue, or impaired contractile function [27, 127]. In all, such types of studies may guide experimental approaches in vitro, where analyses can be more precise.
The micromechanics measured at a cellular or subcellular level can act as a reasonable estimation of tissue-wide properties due to a conservation of elastic behavior. Fortunately, myocytes isolated from their native collagen-rich ECM may retain their passive stresses, as the mechanics of relaxation were reported to be similar between single and multicellular samples of a given sarcomere length [101, 152]. Yet within and around individual cells there often exist more complex distributions of stress and strain. Local nonuniformity of stress and strain has long been recognized in strips of contracting papillary muscle [65, 111]. As an analysis moves closer to the level of the sarcomere, there is a need to make meaningful measurements at or near this scale.
Micromechanics in cardiac myocytes have been studied most often in precisely-controlled conditions in vitro, but inevitably some of the actual complexity found in the whole heart is lost. The tracking of muscle cell contraction (or fractional shortening) alone serves as a simple index of cross-bridge activation and force development. However, by simplifying the structural environment and restricting contractile parameters, one can begin to separate intrinsic and extrinsic contributions of myocyte micromechanics.
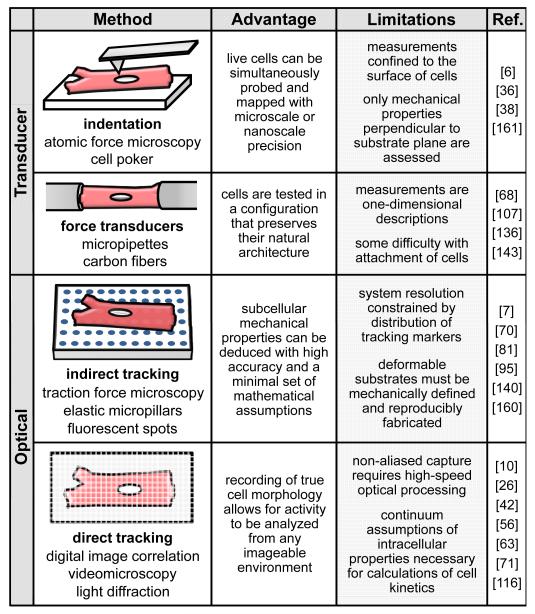
Some of the more established methods to measure the mechanical responses of single cells have involved a variety of transducer-based systems (briefly summarized in Fig. 2). Atomic force microscopy (AFM), cell poking, micropipette suction, and parallel plate devices have all been used to gauge cellular forces through various forms of translated movement or deflection [38, 107, 143]. A few of these techniques are specialized for the probing of passive cell mechanics, whereas others are well-suited for the recording of tension as a function of cell length. Nevertheless, these approaches share an inherent limitation in that their measurements require direct physical contact with isolated cells. For example, efforts to attach free ends of myocytes to transducers such as glass beams or carbon fibers have long struggled with issues of preserving the fragile sarcolemma and maintaining stress-bearing cell edges [19, 68, 136]. Recent improvements in the preparation of intact myocytes and carbon fiber transducers have, however, allowed for more precise axial relationships between sarcomere length and load to be explored [68, 73]. Conversely, nanoindentation analysis with AFM has been largely confined to the surface of cells and in non-skinned myocytes has shown poor sensitivity to micromechanics generated within the cell interior [36]. Such contact-dependent methods also tend to relegate the contractile motion of cells to the same axis of the transducer, though systematic probing has allowed for highly-localized mapping of certain submembranous characteristics [161]. To that end, experiments with spontaneously beating myocytes have shown that mechanical and spatial heterogeneity overlaps at sarcomeric structures in the cells [6].
Fig. 2.
Methods for the analysis of micromechanics in isolated cardiac myocytes or fibroblasts. Techniques to study the active or passive micromechanical properties of cardiac cells rely on measurements that use either transducers or optical microscopy with image capture. Some methods have components that span multiple categories, but each comes with its own advantages and limitations
Other means to evaluate cardiac myocyte activity are optically-based measurement methods. Early work with myocytes exploited the diffraction of light by striations, in which the spacing and dynamics of sarcomeres could be revealed instantaneously as interference patterns [56, 66, 77]. Older imaging methods have taken advantage of the light scattered along the cell periphery during contraction to build semi-automated edge detection procedures; this approach has been applied to one or both ends of myocytes to assess rapid changes in cell or sarcomere length [131, 133]. Also performed with high temporal resolution are linear arrays (or line scanning), which have been used under a range of conditions to acquire the axial displacement of myocytes as they transition between their resting and contracting states [55, 132]. However, many of these one-dimensional (1D) techniques have confirmed that, depending on how they are cultured or supported, isolated myocytes can exhibit nonuniform cell geometry, irregular mechanics at cell ends, bulk lateral and rotational movement, and uneven regional periodicity of sarcomeres [34]. Consequently, the spatial compensations of 1D capture methods have fueled a steady transition towards more quantitative high-speed two-dimensional (2D) imaging as technological improvements have been made.
To reveal how micromechanics vary within an entire cell, contractile motion is analyzed with post hoc computation over an area that contains distinct particles or objects with traceable positions. Several strategies have used indirect tracking, wherein the effect of actomyosin forces can be measured through deformation of engineered landmarks on a compliant culture surface [7, 70, 95, 140]. The same concepts are in fact widely used in the broader field of traction force microscopy to map the passive tensions that develop in adherent cells [148]. For example, fluorescent spots patterned on a 2D surface have shown that focal adhesions in myocytes and fibroblasts correlated with substrate deformation and, hence, the localization of static stresses [7]. Such tracking is not restricted to flat domains, as the bending of elastomeric micropillars affected by contractile cells has been used to identify a minimum threshold size of focal adhesions (1 μm2) to correlate with substrate stresses [140]. A similar arrangement of flexible micropillars with isolated cardiac myocytes demonstrated how the transmission of active forces can vary within the cell thickness [160]. Strides have also been made with indirect tracking in full 3D, as new work has combined fibroblasts and submicron-sized fluorescent beads in 3D matrices to map the principal strains exerted along the contours of cell membranes [81].
Optical methods recently gaining popularity are those that have incorporated direct tracking, in which subcellular activity is monitored by entirely non-destructive and non-contact means through fluorescently labeled molecules or simple fiduciary particles on or within cells [10, 63, 71, 118]. These approaches (sometimes referred to as digital image correlation or videomicroscopy analysis) rely on the software-assisted correlation of captured images to track changes in position of visible cell morphology [26]. Cell displacement data can then be paired with the deformation of the culture surface to evaluate both the transfer of forces and the viscoelastic losses at cell-substrate interfaces [49, 80]. Such methods have also been used to calculate in-plane values of work, power, and strain energy density of contracting myocytes [42, 116]. Similarly, one of the most sophisticated applications of the technique to date has used direct tracking of adult myocytes to help reconstruct the time-varying stresses in beating cells down to a submicrometer resolution [115, 145]. This integrative form of analysis therefore not only permits the faithful reproduction of contractile events, but also allows for the digitized cell to provide the framework for advanced continuum mechanics models. As the interest in combining experimental data and iterative modeling takes root, an entirely new set of considerations becomes important for the study of cardiac myocyte micromechanics.
Modeling of Cardiac Myocyte Micromechanics
Cell models built from known biophysical relationships can be used to pose new physiological questions. This approach of computational biology is based on the mathematical integration of structural and molecular processes within cells, which in cardiac myocytes has included equations relating ionic currents, calcium handling, cross-bridge interactions, metabolism, neurohormonal regulation, and other signaling events [92]. The mechanical function of myocytes is controlled by the interplay of all of these systems, and therefore often requires some broad “black box” interpretations of cell processes to begin modeling. The simplest mechanical models have treated myocytes as simple circuits with four components to represent muscle properties, including analogues for a force generator (actomyosin tension), a parallel damping element (viscous resistance of cytoplasm to shortening), nonlinear springs both in series with and parallel to the generator (active and passive elastic cell characteristics, respectively) [44]. These latter components that act secondary to actomyosin forces may be tempting to overlook during modeling, and their implementation has been continuously refined over the years [22, 57]. The modeling of such components has become increasingly dynamic, given that the relative contribution of elasticity to restore resting tension in myocytes is known to be length-dependent (via the Frank-Starling law), and that the viscosity of cells can alone contribute to nearly 70% of an intrinsic load at high shortening velocities [33, 103].
Several recent attempts to model cardiac myocyte behavior have focused on ways to identify the micromechanical conditions that drive cell growth and reorganization [50, 64, 76]. Simulations have related local myofiber orientations to optimally minimized shear strains, increased stroke work density, and more homogeneous peak stresses within the modeled myocardium [76]. In addition, the mechanical response of myocardial tissue has been accurately approximated with a model defined in three orthogonal directions; this minimal framework showed conformity with myofiber direction and myocyte alignment [59]. Predictions of mechanical-induced changes in cell or tissue shape has overlapped with a large and fascinating field known as finite growth modeling [78, 94]. For cardiac muscle, such concepts have been used to represent myocytes as theoretical volumes with competing elastic and growth components, the configuration of which can ultimately account for pathological dilation and thickening of the myocardium [50].
Intrinsic Loading of Cardiac Myocytes and Fibroblasts
The oscillatory contraction of sarcomeres acts as an intrinsic mechanical load for myocytes in addition to performing external work. Indeed, electrical stimulation of myocyte contraction over several days causes increases in the size and myofibrillar organization of isolated cells [93]. Conversely, arrest of contraction in cultured myocytes results in a more rounded morphology with less alignment of Z-discs; more prolonged contractile arrest leads to widespread myofibril disassembly [128]. Further studies have verified that sustained excitation-contraction coupling alone is adequate to promote both the synthesis and addition of sarcomeric proteins in anchored myocytes – hallmarks of a hypertrophic response [21, 40, 93, 128]. However, other aspects of hypertrophy are difficult to attribute to overall beating activity, as myocyte contraction involves a number of overlapping kinetic and biochemical events. Some aspects of sarcomeric organization, gene expression, and protein accumulation and activation appear to coincide differently with actomyosin cross-bridge cycling or calcium signaling [21, 40].
The intrinsically-generated micromechanics of cardiac myocytes and fibroblasts can also have an effect on the development or behavior of neighboring cells. For example, in zebrafish embryos, cells of the mesoderm sort according to actomyosin-dependent cell tension rather than cell-cell adhesivity [75]. Such work has reinforced the biological principle that form follows function, and for the various cell types of the myocardium, contractile function is clearly the main evolutionary determinant [120]. Computations have suggested that the endogenous forces of contractile cells, when transmitted throughout the local environment, can produce a mechanical feedback that results in cell polarization [159]. However, this relatively slow-acting phenomenon is posited to be significant only in static states, and would thus be overridden with any moderate cyclic stimulus experienced within a beating heart. Experiments with fibroblasts in 3D matrices have shown that a change in neighboring cell tension corresponds less with the overall alignment of contractile stress cables than with their size and number [53]. Thus, the net micromechanics generated and experienced by a group of cells seem to be more critical than the cytoskeletal organization of individual cells.
Extrinsic Loading and Mechanosensing in Cardiac Myocytes and Fibroblasts
Application of Strain
The most thoroughly investigated micromechanical responses of cardiac myocytes and fibroblasts have been those affected by externally-applied strain, which is an imposed length change relative to a reference state (ΔL in Fig. 1). Strain is easily manipulated in vitro by the controlled stretching (tensile strain) of culture substrates or scaffolds, which can simulate a preload at the end of diastole as it relates to the resting length of myocardial cells prior to contraction [106]. While it is straightforward experimentally to introduce strains as high as 20% of initial cell length, such strains can actually be quite complex as perceived at the level of a single cell. Any stretch administered to cells in a single direction will, by conservation of Poisson’s ratio, produce a compression in an orthogonal direction [89]. Some discretion must thus be used when these stimuli are employed in vitro, especially when the layered, anisotropic strains of the native myocardium are often approximated with uniaxial or isotropic conditions [51]. Furthermore, many studies have been performed with cells on flat, relatively rigid surfaces subjected to flexing, where the resulting changes in cell orientation may have more to do with the stabilization of cell anchorage than with strain-dependent remodeling [91, 124, 141].
Independent variables of the direction or rate of strain can, along with the structure of the cell or tissue environment itself, influence how strain is distributed within cells. Extensive studies with fibroblasts, in particular, have shown that both cell and actomyosin filament alignment is readily controlled by such aspects of applied strain [88]. Interestingly, while externally-applied strain is known to trigger stress cable alignment and turnover, focal adhesion kinase (FAK) is required only in the alignment of whole fibroblasts, not cables [29, 61]. When strain rate is varied, fibroblasts and their stress cables are known to align parallel to the direction of strain when presented in the form of static or very low-frequency strain [138]. At higher frequencies of cyclic strain (or those more analogous to the rates experienced in the beating heart), fibroblasts adopt a perpendicular orientation; theoretically, a high rate of depolymerization of stress fibers in line with an anisotropic load results in an accumulation of all other fiber orientations away from the direction of strain [30, 150]. This dependence on strain frequency also extends to cells grown in 3D, as fibroblasts seeded in collagen matrices were reported to align parallel with a static strain vector and perpendicular to a cyclic strain vector [8, 62]. Apart from strain rate, it has been established that cells respond specifically to the direction of principal strain, identified as an axis of pure extension or contraction [15]. Yet in a 3D milieu, other seeding conditions unrelated to strain such as cell number, matrix density, or bulk architecture can affect where this principal strain exists relative to the applied strain axis [112]. In one study, the shape and aspect ratio of a 3D construct was found to alter the principal strain direction perceived by fibroblasts, as thick, cuboidal constructs yielded principal strains slightly perpendicular to the applied load but long, thin constructs confined principal strains parallel to the load [39]. Though many discrepancies remain as to which characteristics of strain dominate in the regulation of fibroblasts, it is clear that all forms of external strain can elicit changes in the cytoskeleton that guide cell orientation and morphology.
Strain of Myocytes and Related Mechanosensors
By concentrating focal adhesions at points of distortion in cells, an external mechanical stimulus can be transmitted throughout the cell for detection [147]. In muscle, externally-applied strain and internally-generated stress are summed and sensed at specific locations. Cardiac myocytes possess specialized forms of focal adhesions at the circumference of the Z-disc known as costameres, where protein complexes anchor cells by connecting filamentous proteins of the ECM to the actin-based cytoskeleton [119, 123, 129]. It is not known how many proteins are mechanically deformed to sense the mechanical input, but transmembrane integrin receptors, talin, vinculin, α-actinin, FAK, and paxillin are all part of the adaptor complex. Signaling results when these proteins themselves translocate or trigger traditional pathways like small GTPases of the Rho family [24, 60, 156]. Once signaling cascades are activated by strain stimuli, some proteins can shuttle to the nucleus to act as strain-sensitive transcription factors. Another mechanical sensor is titin, a very long, spring-like protein that links the M-line and Z-disc of half-sarcomeres [52]. Regions of varying elasticity in titin have been correlated to distinct interactions with muscle-specific LIM protein (MLP), telethonin, myopalladin, and cardiac ankyrin repeat protein upon stretching [9, 60, 74, 153]. The duration, frequency, and amplitude of strain experienced in myocytes are integral to the activation of such signals and the onset of hypertrophic responses [1, 144]. Thus, the detection of strain triggers signaling pathways, gene reprogramming, protein synthesis, and other hallmarks of hypertrophy in cardiac myocytes independent of any contractile activity or actin polymerization [119, 121].
It has long been known that the whole heart and the individual myocytes have anisotropic contributions to longitudinal or transverse strain (relative to the long axis of cells) [16, 134]. Efforts to understand the sensitivity of myocytes to strain direction has led to ways of restricting cell alignment with substrate patterning or grooved topography in order to compare distinct longitudinal and transverse regimes [51, 126]. Through these approaches, it has become evident that the mechanosensors have the ability to detect and respond to the vector of an applied strain. Longitudinal strain of myocytes is less effective on myofibrillar orientation and contractile protein turnover than transverse strain [51, 130]. The situation is complex because some mechanosensors show subcellular redistribution in response to the direction of strain. For example, applied cyclic strain of a given direction alters both MLP shuttling to the nucleus and the subsequent myofibrillar location of this mechanosensor [17]. A static strain applied longitudinally to myocytes leads to the insertion of new sarcomeres all along the cell length; this adaptive remodeling progresses steadily and is complete within 4 hours, adding one sarcomere per hour [90]. The transduction of longitudinal strain stimuli in myocytes is known to involve certain highly-expressed isoforms of the enzyme protein kinase C (PKC), which are required for such stretch-induced hypertrophy [90, 157]. The ends of the myocytes show extensive remodeling to longitudinal strain of the intercalated discs and gap junctions [41, 122, 155, 158].
Microenvironmental Factors Affecting Cardiac Myocyte and Fibroblast Loading
Regulation by Substrate Surface Chemistry
It has been established that anchorage-dependent cells on flat culture surfaces tend to strike a functional balance between cytoskeletal tension and adhesive spreading [67]. Much in vitro work has explored such spreading by constraining morphology to ECM protein-micropatterned surfaces of defined size and shape [23, 102]. This geometric control of cells has allowed for the prediction of micromechanical forces, which have been shown to correlate with the area, concentration, and orientation of adhesion sites in fibroblasts and myocytes [7, 37]. On circular micropatterned islands, fibroblasts were found to assume higher tractional stresses and a lower variance of shear moduli than cells on unpatterned substrates [135]. For myocytes, the introduction of corners within these islands (i.e. a change in micropattern shape from circles to rectangles) was reported to induce a regional formation of sarcomeres with aligned Z-discs [48, 109]. Furthermore, as the aspect ratio of rectangular islands was increased, the sarcomere formation was seen to expand throughout the myocyte to result in a more in vivo-like uniaxial anisotropy during contraction [20]. The same group also demonstrated that different micropatterned shapes of similar surface areas did not alter the overall myocyte volume, but rather the striated architecture of cells [48]. Similarly, the mechanical properties of fibroblasts have shown a biphasic dependence on relative micropattern size, an effect thought to be related to the volume fraction of polymerized actin within the cell [135]. Beyond a certain size threshold, however, there is evidence that the distribution of tension in contractile cells on a substrate surface is conserved at the tissue level [13].
Regulation by Substrate Stiffness
If an afterload is defined as the effective resistance against which a cardiac myocyte must work, perhaps the clearest link to an afterload in vitro is through modification of domain stiffness, or the resistance of a substrate to deformation. Cardiac myocytes are mechanically anisotropic, but their passive stiffness has widely been approximated with a single Young’s modulus between 10 and 50 kPa [6, 11, 19, 86]. In order to reproduce this range of native stiffnesses presented in the study of isolated cells, a number of groups have employed polymeric substrates of tunable crosslinker content. Neonatal myocytes on 10 kPa collagen-coated elastic surfaces displayed well-organized sarcomeres, while cells on 1 kPa or 50 kPa surfaces had poorly-defined or less-aligned striations, respectively [69]. Furthermore, myocytes on 50kPa surfaces were spread into irregular shapes, but on a 10kPa substrate they adopted an axially-aligned shape that corresponded with higher developed forces. A continuous tensional balance thus exists between external stiffness and internal remodeling of the contractile filaments, which determines the state of cytoskeletal “prestress” at any given time [149]. This concept can account for the general finding that both myocytes and fibroblasts exhibit more spreading with increasing substrate stiffness [42]. Likewise, individual stress fibers have been shown to contribute more to intracellular tension and overall cell shape on softer surfaces than on relatively stiffer ones [79]. For myocytes, the matching of stiffnesses between cells and their local surroundings appears to be especially crucial for maximizing the efficiency of the actomyosin power stroke [42, 69, 137]. In all, these trends have suggested that the ideal rigidity for sarcomeres to organize, mature, and optimize a mechanical capability is within the 10-50 kPa passive stiffness range of resting myocytes. However, many studies continue to culture cells on very hard surfaces (e.g. polystyrene, MPa, or glass, GPa) that are considerably stiffer than physiologic or pathophysiologic tissues.
Regulation by Substrate Topography
Cells cultured on conventional two-dimensional dishes generally display an irregular, flattened morphology. This morphology is uncharacteristic of the stellate to fusiform shape of fibroblasts or the rounded cross-sectional area (~15 μm thickness) of myocytes common in vivo [87, 114]. Given that the micromechanics of stress fibers and myofibrils are otherwise confined within a single thin plane on two dimensions, the engineered recapitulation of a cellular environment into three dimensions is more lifelike. For example, myocytes grown on elastomeric substrates containing regularly-spaced 5 μm-high topographical structures were shown to terminate with sarcomeric striations over a greater thickness than those cell ends on untextured surfaces [96, 97]. Fibroblasts seeded on similar substrates exhibited greater adhesive interactions and trailing edge lengths than cells on uniformly flat substrates [110, 142]. In these environments, the local dynamics in fibroblast contractility were linked to global changes in cell proliferation and RhoA expression. In a much larger scale, 1.5 mm-high elastomeric posts have been used to guide cell alignment and the spatial arrangement of tension in cardiac muscle tissues [12]. Cell contact with a vertically-oriented substrate therefore appears to provide conditions for optimal anchoring of tension-generating elements and the ability to transmit forces. This is likely to carry over into full 3D environments, as cell-populated collagen gels are known to develop a net mechanical stress from the collective actomyosin constituents of myocytes or fibroblasts alone [44]. In addition, cardiac fibroblasts have been shown to convert to a more contractile myofibroblast phenotype with distinct differences in ECM protein production when maintained in 3D matrices [113].
Combinations of Substrate Cues in 3D: Mimicking ECM Complexity
There have been efforts to explore how physical cues can overlap or compete to affect the micromechanics in cardiac myocytes and fibroblasts. For instance, with discontinuities of stiffness in 3D environments, fibroblasts assemble the cytoskeleton to polarize in the direction of the greatest effective stiffness, orienting perpendicular to the stiffer boundary [14]. Fibroblasts that encounter local resistance in 3D matrices change their morphology from dendritic to fusiform, indicative of resting and contractile states, respectively [139]. The cell–matrix interactions at such regions of high stiffness in 3D also mature from punctate complexes to larger clusters of focal adhesions [139]. Mechanical heterogeneity has also been introduced to fibroblasts through the use of discrete polymeric microstructures of variable stiffness suspended in pliant 3D gels [5, 105]. Even a low concentration of relatively stiff microstructures (50 kPa) causes a decrease in fibroblast proliferation and the expression of the contractility marker alpha-smooth muscle actin compared to 3D cultures containing soft (2 kPa) or no microstructures [5]. Embryological development of the heart and its contractile function are accompanied by similarly complex changes in stiffness and 3D architecture. The formation of the heart tube depends on local forces, and mechanical loads can influence gene expression patterns during development [146, 154]. Recapitulation of some of these features in tube-like 3D organoid constructs using immature, proliferative ventricular myocytes from 15-day old fetuses show a transition from the quiescent to contractile phenotype [43]. Neonatal cardiac myocytes respond to microstructures in 3D with both hypertrophic growth and spontaneous contractile activity [28]. Myocytes and fibroblasts have also been combined in a 3D matrix with underlying mesoscale topography to show that muscle tissue develops greater tension with an increased stiffness than of either scaffold component alone [82].
The filamentous proteins of the ECM in the heart provide a common anchor for myocytes and fibroblasts, thereby stabilizing the transmission of forces parallel to the myocyte direction [18, 108]. Specifically, the network of collagen, laminin, elastin, and fibronectin serves to enmesh densely-packed myocytes in the myocardium as 50 μm-thick laminar sheets, a layout that allows for the high shear strains associated with ventricular wall shortening to be maintained with minimal shear stresses [4, 83]. The overall composition of the ECM is one suspected reason for differences in elastic anisotropy at various myocardial depths [25]. Yet many studies have focused on the mechanical contribution of fibroblast-deposited collagen alone, particularly its role in scar tissue formation to fill the physical void left by diseased or damaged myocytes. The triple-helical structure of collagen is known to be relatively stiff, and the scar-dependent increase in collagen content following a myocardial infarction can therefore cause an increase in local tissue stiffness from about 25 kPa up to 500 kPa within 2 weeks [19, 46]. The quantity, alignment, and degree of crosslinking of collagen have also been shown to alter the mechanical properties of a myocardial scar, and thus significantly influence the load of adjacent myocytes and the total heart function [45, 54, 58].
Implications for Tissue Remodeling
This review has attempted to cover the vast and rapidly growing literature concerning the micromechanical cues that guide the structure and function of fibroblasts and myocytes in vitro. Undoubtedly, the pathophysiological environment in the whole heart during remodeling is determined in part by these same micromechanical cues. The knowledge gained through the measurement, modeling, and application of micromechanical stimuli therefore provides a framework for meeting the physical requirements of cardiac myocytes and fibroblasts. With this understanding, new strategies may arise in the design of 3D tissue engineering scaffolds to employ appropriate structural cues that differentially direct cellular phenotype. Furthermore, the systematic mechanical breakdown of an artificial cell niche for stem and progenitor cell survival, engraftment, and maturation may ultimately enhance the success of cell therapy and regenerative medicine.
Abbreviations
- 1D
one dimension
- 2D
two dimensions
- 3D
three dimensions
- AFM
atomic force microscopy
- ECM
extracellular matrix
- FAK
focal adhesion kinase
- MLP
muscle LIM protein
- PKC
protein kinase C
References
- [1].Aikawa R, Komuro I, Yamazaki T, Zou Y, Kudoh S, Zhu W, Kadowaki T, Yazaki Y. Rho family small G proteins play critical roles in mechanical stress-induced hypertrophic responses in cardiac myocytes. Circ Res. 1999;84(4):458–66. doi: 10.1161/01.res.84.4.458. [DOI] [PubMed] [Google Scholar]
- [2].Allen DG, Kentish JC. The cellular basis of the length-tension relation in cardiac muscle. J Mol Cell Cardiol. 1985;17(9):821–40. doi: 10.1016/s0022-2828(85)80097-3. [DOI] [PubMed] [Google Scholar]
- [3].Amundsen BH, Crosby J, Steen PA, Torp H, Slørdahl SA, Støylen A. Regional myocardial long-axis strain and strain rate measured by different tissue Doppler and speckle tracking echocardiography methods: a comparison with tagged magnetic resonance imaging. Eur J Echocardiogr. 2009;10(2):229–37. doi: 10.1093/ejechocard/jen201. [DOI] [PubMed] [Google Scholar]
- [4].Arts T, Costa KD, Covell JW, McCulloch AD. Relating myocardial laminar architecture to shear strain and muscle fiber orientation. Am J Physiol Heart Circ Physiol. 2001;280(5):H2222–9. doi: 10.1152/ajpheart.2001.280.5.H2222. [DOI] [PubMed] [Google Scholar]
- [5].Ayala P, Lopez JI, Desai TA. Microtopographical Cues in 3D attenuate fibrotic phenotype and extracellular matrix deposition: implications for tissue regeneration. Tissue Eng Part A. 2010 doi: 10.1089/ten.tea.2009.0815. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Azeloglu EU, Costa KD. Cross-bridge cycling gives rise to spatiotemporal heterogeneity of dynamic subcellular mechanics in cardiac myocytes probed with atomic force microscopy. Am J Physiol Heart Circ Physiol. 2010;298(3):H853–60. doi: 10.1152/ajpheart.00427.2009. [DOI] [PubMed] [Google Scholar]
- [7].Balaban NQ, Schwarz US, Riveline D, Goichberg P, Tzur G, Sabanay I, Mahalu D, Safran S, Bershadsky A, Addadi L, Geiger B. Force and focal adhesion assembly: a close relationship studied using elastic micropatterned substrates. Nat Cell Biol. 2001;3(5):466–72. doi: 10.1038/35074532. [DOI] [PubMed] [Google Scholar]
- [8].Balestrini JL, Skorinko JK, Hera A, Gaudette GR, Billiar KL. Applying controlled non-uniform deformation for in vitro studies of cell mechanobiology. Biomech Model Mechanobiol. 2010;9(3):329–44. doi: 10.1007/s10237-009-0179-9. [DOI] [PubMed] [Google Scholar]
- [9].Bang ML, Mudry RE, McElhinny AS, Trombitás K, Geach AJ, Yamasaki R, Sorimachi H, Granzier H, Gregorio CC, Labeit S. Myopalladin, a novel 145-kilodalton sarcomeric protein with multiple roles in Z-disc and I-band protein assemblies. J Cell Biol. 2001;153(2):413–27. doi: 10.1083/jcb.153.2.413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Bausch AR, Ziemann F, Boulbitch AA, Jacobson K, Sackmann E. Local measurements of viscoelastic parameters of adherent cell surfaces by magnetic bead microrheometry. Biophys J. 1998;75(4):2038–49. doi: 10.1016/S0006-3495(98)77646-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Berry MF, Engler AJ, Woo YJ, Pirolli TJ, Bish LT, Jayasankar V, Morine KJ, Gardner TJ, Discher DE, Sweeney HL. Mesenchymal stem cell injection after myocardial infarction improves myocardial compliance. Am J Physiol Heart Circ Physiol. 2006;290(6):H2196–203. doi: 10.1152/ajpheart.01017.2005. [DOI] [PubMed] [Google Scholar]
- [12].Bian W, Liau B, Badie N, Bursac N. Mesoscopic hydrogel molding to control the 3D geometry of bioartificial muscle tissues. Nat Protoc. 2009;4(10):1522–34. doi: 10.1038/nprot.2009.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Bischofs IB, Klein F, Lehnert D, Bastmeyer M, Schwarz US. Filamentous network mechanics and active contractility determine cell and tissue shape. Biophys J. 2008;95(7):3488–96. doi: 10.1529/biophysj.108.134296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Bischofs IB, Schwarz US. Cell organization in soft media due to active mechanosensing. Proc Natl Acad Sci U S A. 2003;100(16):9274–9. doi: 10.1073/pnas.1233544100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Blanchard GB, Kabla AJ, Schultz NL, Butler LC, Sanson B, Gorfinkiel N, Mahadevan L, Adams RJ. Tissue tectonics: morphogenetic strain rates, cell shape change and intercalation. Nat Methods. 2009;6(6):458–64. doi: 10.1038/nmeth.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Bloch RJ, Gonzalez-Serratos H. Lateral force transmission across costameres in skeletal muscle. Exerc Sport Sci Rev. 2003;31(2):73–8. doi: 10.1097/00003677-200304000-00004. [DOI] [PubMed] [Google Scholar]
- [17].Boateng SY, Senyo SE, Qi L, Goldspink PH, Russell B. Myocyte remodeling in response to hypertrophic stimuli requires nucleocytoplasmic shuttling of muscle LIM protein. J Mol Cell Cardiol. 2009;47(4):426–35. doi: 10.1016/j.yjmcc.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Bovendeerd PH, Arts T, Huyghe JM, van Campen DH, Reneman RS. Dependence of local left ventricular wall mechanics on myocardial fiber orientation: a model study. J Biomech. 1992;25(10):1129–40. doi: 10.1016/0021-9290(92)90069-d. [DOI] [PubMed] [Google Scholar]
- [19].Brady AJ. Mechanical properties of isolated cardiac myocytes. Physiol Rev. 1991;71(2):413–28. doi: 10.1152/physrev.1991.71.2.413. [DOI] [PubMed] [Google Scholar]
- [20].Bray MA, Sheehy SP, Parker KK. Sarcomere alignment is regulated by myocyte shape. Cell Motil Cytoskeleton. 2008;65(8):641–51. doi: 10.1002/cm.20290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Byron KL, Puglisi JL, Holda JR, Eble D, Samarel AM. Myosin heavy chain turnover in cultured neonatal rat heart cells: effects of [Ca2+]i and contractile activity. Am J Physiol. 1996;271(5 Pt 1):C01447–56. doi: 10.1152/ajpcell.1996.271.5.C01447. [DOI] [PubMed] [Google Scholar]
- [22].Chapelle D, Clément F, Génot F, Tallec PL, Sorine M, Urquiza J. A physiologically-based model for the active cardiac muscle contraction. Lecture Notes in Computer Science. 2001;2230:128–133. [Google Scholar]
- [23].Chen CS, Mrksich M, Huang S, Whitesides GM, Ingber DE. Micropatterned surfaces for control of cell shape, position, and function. Biotechnol Prog. 1998;14(3):356–63. doi: 10.1021/bp980031m. [DOI] [PubMed] [Google Scholar]
- [24].Clerk A, Sugden PH. Ras: the stress and the strain. J Mol Cell Cardiol. 2006;41(4):595–600. doi: 10.1016/j.yjmcc.2006.06.075. [DOI] [PubMed] [Google Scholar]
- [25].Couade M, Pernot M, Messas E, Bel A, Ba M, Albert H, Fink M, Tanter M. In vivo quantitative mapping of myocardial stiffening and transmural anisotropy during the cardiac cycle. IEEE Trans Med Imaging. 2010 doi: 10.1109/TMI.2010.2076829. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- [26].Cranston PG, Veldhuis JH, Narasimhan S, Brodland GW. Cinemechanometry (CMM): A method to determine the forces that drive morphogenetic movements from time-lapse images. Ann Biomed Eng. 2010;38(9):2937–47. doi: 10.1007/s10439-010-9998-1. [DOI] [PubMed] [Google Scholar]
- [27].Cupps BP, Taggar AK, Reynolds LM, Lawton JS, Pasque MK. Regional myocardial contractile function: multiparametric strain mapping. Interact Cardiovasc Thorac Surg. 2010;10(6):953–7. doi: 10.1510/icvts.2009.220384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Curtis MW, Sharma S, Desai TA, Russell B. Hypertrophy, gene expression, and beating of neonatal cardiac myocytes are affected by microdomain heterogeneity in 3D. Biomed Microdevices. 2010;12(6):1073–85. doi: 10.1007/s10544-010-9461-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Dalla Costa AP, Clemente CF, Carvalho HF, Carvalheira JB, Nadruz W, Jr, Franchini KG. FAK mediates the activation of cardiac fibroblasts induced by mechanical stress through regulation of the mTOR complex. Cardiovasc Res. 2010;86(3):421–31. doi: 10.1093/cvr/cvp416. [DOI] [PubMed] [Google Scholar]
- [30].De R, Zemel A, Safran SA. Do cells sense stress or strain? Measurement of cellular orientation can provide a clue. Biophys J. 2008;94(5):L29–31. doi: 10.1529/biophysj.107.126060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].de Simone G, de Divitiis O. Extracellular matrix and left ventricular mechanics in overload hypertrophy. Adv Clin Path. 2002;6(1):3–10. [PubMed] [Google Scholar]
- [32].de Tombe PP. Cardiac myofilaments: mechanics and regulation. J Biomech. 2003;36(5):721–30. doi: 10.1016/s0021-9290(02)00450-5. [DOI] [PubMed] [Google Scholar]
- [33].de Tombe PP, ter Keurs HE. An internal viscous element limits unloaded velocity of sarcomere shortening in rat myocardium. J Physiol. 1992;454:619–42. doi: 10.1113/jphysiol.1992.sp019283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Delbridge LM, Roos KP. Optical methods to evaluate the contractile function of unloaded isolated cardiac myocytes. J Mol Cell Cardiol. 1997;29(1):11–25. doi: 10.1006/jmcc.1996.0247. [DOI] [PubMed] [Google Scholar]
- [35].D’hooge J, Heimdal A, Jamal F, Kukulski T, Bijnens B, Rademakers F, Hatle L, Suetens P, Sutherland GR. Regional strain and strain rate measurements by cardiac ultrasound: principles, implementation and limitations. Eur J Echocardiogr. 2000;1(3):154–70. doi: 10.1053/euje.2000.0031. [DOI] [PubMed] [Google Scholar]
- [36].Domke J, Parak WJ, George M, Gaub HE, Radmacher M. Mapping the mechanical pulse of single cardiomyocytes with the atomic force microscope. Eur Biophys J. 1999;28(3):179–86. doi: 10.1007/s002490050198. [DOI] [PubMed] [Google Scholar]
- [37].Dumbauld DW, Shin H, Gallant ND, Michael KE, Radhakrishna H, García AJ. Contractility modulates cell adhesion strengthening through focal adhesion kinase and assembly of vinculin-containing focal adhesions. J Cell Physiol. 2010;223(3):746–56. doi: 10.1002/jcp.22084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Duszyk M, Schwab B, 3rd, Zahalak GI, Qian H, Elson EL. Cell poking: quantitative analysis of indentation of thick viscoelastic layers. Biophys J. 1989;55(4):683–90. doi: 10.1016/S0006-3495(89)82867-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Eastwood M, Mudera VC, McGrouther DA, Brown RA. Effect of precise mechanical loading on fibroblast populated collagen lattices: morphological changes. Cell Motil Cytoskeleton. 1998;40(1):13–21. doi: 10.1002/(SICI)1097-0169(1998)40:1<13::AID-CM2>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- [40].Eble DM, Qi M, Waldschmidt S, Lucchesi PA, Byron KL, Samarel AM. Contractile activity is required for sarcomeric assembly in phenylephrine-induced cardiac myocyte hypertrophy. Am J Physiol. 1998;274(5 Pt 1):C1226–37. doi: 10.1152/ajpcell.1998.274.5.C1226. [DOI] [PubMed] [Google Scholar]
- [41].Ehler E, Horowits R, Zuppinger C, Price RL, Perriard E, Leu M, Caroni P, Sussman M, Eppenberger HM, Perriard JC. Alterations at the intercalated disk associated with the absence of muscle LIM protein. J Cell Biol. 2001;153(4):763–72. doi: 10.1083/jcb.153.4.763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Engler AJ, Carag-Krieger C, Johnson CP, Raab M, Tang HY, Speicher DW, Sanger JW, Sanger JM, Discher DE. Embryonic cardiomyocytes beat best on a matrix with heart-like elasticity: scar-like rigidity inhibits beating. J Cell Sci. 2008;121(Pt 22):3794–802. doi: 10.1242/jcs.029678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Evans HJ, Sweet JK, Price RL, Yost M, Goodwin RL. Novel 3D culture system for study of cardiac myocyte development. Am J Physiol Heart Circ Physiol. 2003;285(2):H570–8. doi: 10.1152/ajpheart.01027.2002. [DOI] [PubMed] [Google Scholar]
- [44].Feng Z, Matsumoto T, Nakamura T. Measurements of the mechanical properties of contracted collagen gels populated with rat fibroblasts or cardiomyocytes. J Artif Organs. 2003;6(3):192–6. doi: 10.1007/s10047-003-0230-z. [DOI] [PubMed] [Google Scholar]
- [45].Fomovsky GM, Holmes JW. Evolution of scar structure, mechanics, and ventricular function after myocardial infarction in the rat. Am J Physiol Heart Circ Physiol. 2010;298(1):H221–8. doi: 10.1152/ajpheart.00495.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Fomovsky GM, Thomopoulos S, Holmes JW. Contribution of extracellular matrix to the mechanical properties of the heart. J Mol Cell Cardiol. 2010;48(3):490–6. doi: 10.1016/j.yjmcc.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Fung YC. Comparison of different models of the heart muscle. J Biomech. 1971;4(4):289–95. doi: 10.1016/0021-9290(71)90035-2. [DOI] [PubMed] [Google Scholar]
- [48].Geisse NA, Sheehy SP, Parker KK. Control of myocyte remodeling in vitro with engineered substrates. In Vitro Cell Dev Biol Anim. 2009;45(7):343–50. doi: 10.1007/s11626-009-9182-9. [DOI] [PubMed] [Google Scholar]
- [49].Ghosh K, Pan Z, Guan E, Ge S, Liu Y, Nakamura T, Ren XD, Rafailovich M, Clark RA. Cell adaptation to a physiologically relevant ECM mimic with different viscoelastic properties. Biomaterials. 2007;28(4):671–9. doi: 10.1016/j.biomaterials.2006.09.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Göktepe S, Abilez OJ, Parker KK, Kuhl E. A multiscale model for eccentric and concentric cardiac growth through sarcomerogenesis. J Theor Biol. 2010;265(3):433–42. doi: 10.1016/j.jtbi.2010.04.023. [DOI] [PubMed] [Google Scholar]
- [51].Gopalan SM, Flaim C, Bhatia SN, Hoshijima M, Knoell R, Chien KR, Omens JH, McCulloch AD. Anisotropic stretch-induced hypertrophy in neonatal ventricular myocytes micropatterned on deformable elastomers. Biotechnol Bioeng. 2003;81(5):578–87. doi: 10.1002/bit.10506. [DOI] [PubMed] [Google Scholar]
- [52].Granzier HL, Labeit S. The giant protein titin: a major player in myocardial mechanics, signaling, and disease. Circ Res. 2004;94(3):284–95. doi: 10.1161/01.RES.0000117769.88862.F8. [DOI] [PubMed] [Google Scholar]
- [53].Grinnell F. Fibroblast-collagen-matrix contraction: growth-factor signalling and mechanical loading. Trends Cell Biol. 2000;10(9):362–5. doi: 10.1016/s0962-8924(00)01802-x. [DOI] [PubMed] [Google Scholar]
- [54].Gupta KB, Ratcliffe MB, Fallert MA, Edmunds LH, Jr, Bogen DK. Changes in passive mechanical stiffness of myocardial tissue with aneurysm formation. Circulation. 1994;89(5):2315–26. doi: 10.1161/01.cir.89.5.2315. [DOI] [PubMed] [Google Scholar]
- [55].Harris PJ, Stewart D, Cullinan MC, Delbridge LM, Dally LJ, Grinwald P. Rapid measurement of isolated cardiac muscle cell length using a line-scan camera. IEEE Trans Biomed Eng. 1987;34(1):463–467. doi: 10.1109/tbme.1987.326081. [DOI] [PubMed] [Google Scholar]
- [56].Haworth RA, Griffin P, Saleh B, Goknur AB, Berkoff HA. Contractile function of isolated young and adult rat heart cells. Am J Physiol. 1987;253(1):H1484–H1491. doi: 10.1152/ajpheart.1987.253.6.H1484. [DOI] [PubMed] [Google Scholar]
- [57].Hill AV. The series elastic component of muscle. Proc R Soc Lond B Biol Sci. 1950;137(887):273–80. doi: 10.1098/rspb.1950.0035. [DOI] [PubMed] [Google Scholar]
- [58].Holmes JW, Nuñez JA, Covell JW. Functional implications of myocardial scar structure. Am J Physiol. 1997;272(5 Pt 2):H2123–30. doi: 10.1152/ajpheart.1997.272.5.H2123. [DOI] [PubMed] [Google Scholar]
- [59].Holzapfel GA, Ogden RW. Constitutive modelling of passive myocardium: a structurally based framework for material characterization. Philos Transact A Math Phys Eng Sci. 2009;367(1902):3445–75. doi: 10.1098/rsta.2009.0091. [DOI] [PubMed] [Google Scholar]
- [60].Hoshijima M. Mechanical stress-strain sensors embedded in cardiac cytoskeleton: Z disk, titin, and associated structures. Am J Physiol Heart Circ Physiol. 2006;290(4):H1313–25. doi: 10.1152/ajpheart.00816.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Hsu HJ, Lee CF, Locke A, Vanderzyl SQ, Kaunas R. Stretch-induced stress fiber remodeling and the activations of JNK and ERK depend on mechanical strain rate, but not FAK. PLoS One. 2010;5(8):e12470. doi: 10.1371/journal.pone.0012470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [62].Huang D, Chang TR, Aggarwal A, Lee RC, Ehrlich HP. Mechanisms and dynamics of mechanical strengthening in ligament-equivalent fibroblast-populated collagen matrices. Ann Biomed Eng. 1993;21(3):289–305. doi: 10.1007/BF02368184. [DOI] [PubMed] [Google Scholar]
- [63].Huang J, Peng X, Qin L, Zhu T, Xiong C, Zhang Y, Fang J. Determination of cellular tractions on elastic substrate based on an integral Boussinesq solution. J Biomech Eng. 2009;131(6):061009. doi: 10.1115/1.3118767. [DOI] [PubMed] [Google Scholar]
- [64].Hunter PJ, McCulloch AD, ter Keurs HE. Modelling the mechanical properties of cardiac muscle. Prog Biophys Mol Biol. 1998;69(2-3):289–331. doi: 10.1016/s0079-6107(98)00013-3. [DOI] [PubMed] [Google Scholar]
- [65].Huntsman LL, Day SR, Stewart DK. Nonuniform contraction in the isolated cat papillary muscle. Am J Physiol. 1977;233(5):H613–6. doi: 10.1152/ajpheart.1977.233.5.H613. [DOI] [PubMed] [Google Scholar]
- [66].Huxley AF, Niedergerke R. Structural changes in muscle during contraction; interference microscopy of living muscle fibres. Nature. 1954;173(4412):971–3. doi: 10.1038/173971a0. [DOI] [PubMed] [Google Scholar]
- [67].Ingber DE. Tensegrity: the architectural basis of cellular mechanotransduction. Annu Rev Physiol. 1997;59:575–99. doi: 10.1146/annurev.physiol.59.1.575. [DOI] [PubMed] [Google Scholar]
- [68].Iribe G, Helmes M, Kohl P. Force-length relations in isolated intact cardiomyocytes subjected to dynamic changes in mechanical load. Am J Physiol Heart Circ Physiol. 2007;292(3):H1487–97. doi: 10.1152/ajpheart.00909.2006. [DOI] [PubMed] [Google Scholar]
- [69].Jacot JG, McCulloch AD, Omens JH. Substrate stiffness affects the functional maturation of neonatal rat ventricular myocytes. Biophys J. 2008;95(7):3479–87. doi: 10.1529/biophysj.107.124545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Kajzar A, Cesa CM, Kirchgessner N, Hoffmann B, Merkel R. Toward physiological conditions for cell analyses: forces of heart muscle cells suspended between elastic micropillars. Biophys J. 2008;94(5):1854–66. doi: 10.1529/biophysj.107.115766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Kamgoué A, Ohayon J, Usson Y, Riou L, Tracqui P. Quantification of cardiomyocyte contraction based on image correlation analysis. Cytometry A. 2009;75(4):298–308. doi: 10.1002/cyto.a.20700. [DOI] [PubMed] [Google Scholar]
- [72].Katz AM. Physiology of the heart. Lippincott Williams & Wilkins; Philadelphia: 2010. [Google Scholar]
- [73].King NM, Methawasin M, Nedrud J, Harrell N, Chung CS, Helmes M, Granzier H. Mouse intact cardiac myocyte mechanics: cross-bridge and titin-based stress in unactivated cells. J Gen Physiol. 2011;137(1):81–91. doi: 10.1085/jgp.201010499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Knöll R, Hoshijima M, Hoffman HM, Person V, Lorenzen-Schmidt I, Bang ML, Hayashi T, Shiga N, Yasukawa H, Schaper W, McKenna W, Yokoyama M, Schork NJ, Omens JH, McCulloch AD, Kimura A, Gregorio CC, Poller W, Schaper J, Schultheiss HP, Chien KR. The cardiac mechanical stretch sensor machinery involves a Z disc complex that is defective in a subset of human dilated cardiomyopathy. Cell. 2002;111(7):943–55. doi: 10.1016/s0092-8674(02)01226-6. [DOI] [PubMed] [Google Scholar]
- [75].Krieg M, Arboleda-Estudillo Y, Puech PH, Käfer J, Graner F, Müller DJ, Heisenberg CP. Tensile forces govern germ-layer organization in zebrafish. Nat Cell Biol. 2008;10(4):429–36. doi: 10.1038/ncb1705. [DOI] [PubMed] [Google Scholar]
- [76].Kroon W, Delhaas T, Bovendeerd P, Arts T. Computational analysis of the myocardial structure: adaptation of cardiac myofiber orientations through deformation. Med Image Anal. 2009;13(2):346–53. doi: 10.1016/j.media.2008.06.015. [DOI] [PubMed] [Google Scholar]
- [77].Krueger JW, Forletti D, Wittenberg BA. Uniform sarcomere shortening behavior in isolated cardiac muscle cells. J Gen Physiol. 1980;76(1):587–607. doi: 10.1085/jgp.76.5.587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Kuhl E, Garikipati K, Arruda EM, Grosh K. Remodeling of biological tissue: Mechanically induced reorientation of a transversely isotropic chain network. Journal of the Mechanics and Physics of Solids. 2005;53(1):1552–73. [Google Scholar]
- [79].Kumar S, Maxwell IZ, Heisterkamp A, Polte TR, Lele TP, Salanga M, Mazur E, Ingber DE. Viscoelastic retraction of single living stress fibers and its impact on cell shape, cytoskeletal organization, and extracellular matrix mechanics. Biophys J. 2006;90(10):3762–73. doi: 10.1529/biophysj.105.071506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Lee CH, Guo CL, Wang J. Optical measurement of the viscoelastic and biochemical responses of living cells to mechanical perturbation. Opt Lett. 1998;23(4):307–9. doi: 10.1364/ol.23.000307. [DOI] [PubMed] [Google Scholar]
- [81].Legant WR, Miller JS, Blakely BL, Cohen DM, Genin GM, Chen CS. Measurement of mechanical tractions exerted by cells in three-dimensional matrices. Nat Methods. 2010;7(12):969–71. doi: 10.1038/nmeth.1531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Legant WR, Pathak A, Yang MT, Deshpande VS, McMeeking RM, Chen CS. Microfabricated tissue gauges to measure and manipulate forces from 3D microtissues. Proc Natl Acad Sci U S A. 2009;106(25):10097–102. doi: 10.1073/pnas.0900174106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [83].LeGrice IJ, Takayama Y, Covell JW. Transverse shear along myocardial cleavage planes provides a mechanism for normal systolic wall thickening. Circ Res. 1995;77(1):182–93. doi: 10.1161/01.res.77.1.182. [DOI] [PubMed] [Google Scholar]
- [84].Leitman M, Lysyansky P, Sidenko S, Shir V, Peleg E, Binenbaum M, Kaluski E, Krakover R, Vered Z. Two-dimensional strain-a novel software for real-time quantitative echocardiographic assessment of myocardial function. J Am Soc Echocardiogr. 2004;17(10):1021–9. doi: 10.1016/j.echo.2004.06.019. [DOI] [PubMed] [Google Scholar]
- [85].Levy C, Ter Keurs HE, Yaniv Y, Landesberg A. The sarcomeric control of energy conversion. Ann N Y Acad Sci. 2005;1047:219–31. doi: 10.1196/annals.1341.020. [DOI] [PubMed] [Google Scholar]
- [86].Lieber SC, Aubry N, Pain J, Diaz G, Kim SJ, Vatner SF. Aging increases stiffness of cardiac myocytes measured by atomic force microscopy nanoindentation. Am J Physiol Heart Circ Physiol. 2004;287(2):H645–51. doi: 10.1152/ajpheart.00564.2003. [DOI] [PubMed] [Google Scholar]
- [87].Liu Z, Hilbelink DR, Crockett WB, Gerdes AM. Regional changes in hemodynamics and cardiac myocyte size in rats with aortocaval fistulas. 1. Developing and established hypertrophy. Circ Res. 1991;69(1):52–8. doi: 10.1161/01.res.69.1.52. [DOI] [PubMed] [Google Scholar]
- [88].MacKenna D, Summerour SR, Villarreal FJ. Role of mechanical factors in modulating cardiac fibroblast function and extracellular matrix synthesis. Cardiovasc Res. 2000;46(2):257–63. doi: 10.1016/s0008-6363(00)00030-4. [DOI] [PubMed] [Google Scholar]
- [89].Mahaffy RE, Park S, Gerde E, Käs J, Shih CK. Quantitative analysis of the viscoelastic properties of thin regions of fibroblasts using atomic force microscopy. Biophys J. 2004;86(3):1777–93. doi: 10.1016/S0006-3495(04)74245-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [90].Mansour H, de Tombe PP, Samarel AM, Russell B. Restoration of resting sarcomere length after uniaxial static strain is regulated by protein kinase Cepsilon and focal adhesion kinase. Circ Res. 2004;94(5):642–9. doi: 10.1161/01.RES.0000121101.32286.C8. [DOI] [PubMed] [Google Scholar]
- [91].Matsuda T, Takahashi K, Nariai T, Ito T, Takatani T, Fujio Y, Azuma J. N-cadherin-mediated cell adhesion determines the plasticity for cell alignment in response to mechanical stretch in cultured cardiomyocytes. Biochem Biophys Res Commun. 2005;326(1):228–32. doi: 10.1016/j.bbrc.2004.11.019. [DOI] [PubMed] [Google Scholar]
- [92].McCulloch AD. Functionally and structurally integrated computational modeling of ventricular physiology. Jpn J Physiol. 2004;54(6):531–9. doi: 10.2170/jjphysiol.54.531. [DOI] [PubMed] [Google Scholar]
- [93].McDonough PM, Glembotski CC. Induction of atrial natriuretic factor and myosin light chain-2 gene expression in cultured ventricular myocytes by electrical stimulation of contraction. J Biol Chem. 1992;267(17):11665–8. [PubMed] [Google Scholar]
- [94].Menzel A. Modelling of anisotropic growth in biological tissues. A new approach and computational aspects. Biomech Model Mechanobiol. 2005;3(3):147–71. doi: 10.1007/s10237-004-0047-6. [DOI] [PubMed] [Google Scholar]
- [95].Merkel R, Kirchgessner N, Cesa CM, Hoffmann B. Cell force microscopy on elastic layers of finite thickness. Biophys J. 2007;93(9):3314–23. doi: 10.1529/biophysj.107.111328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Motlagh D, Hartman TJ, Desai TA, Russell B. Microfabricated grooves recapitulate neonatal myocyte connexin43 and N-cadherin expression and localization. J Biomed Mater Res A. 2003;67(1):148–57. doi: 10.1002/jbm.a.10083. [DOI] [PubMed] [Google Scholar]
- [97].Motlagh D, Senyo SE, Desai TA, Russell B. Microtextured substrata alter gene expression, protein localization and the shape of cardiac myocytes. Biomaterials. 2003;24(14):2463–76. doi: 10.1016/s0142-9612(02)00644-0. [DOI] [PubMed] [Google Scholar]
- [98].Murry CE, Field LJ, Menasché P. Cell-based cardiac repair: reflections at the 10-year point. Circulation. 2005;112(20):3174–83. doi: 10.1161/CIRCULATIONAHA.105.546218. [DOI] [PubMed] [Google Scholar]
- [99].Muthupillai R, Lomas DJ, Rossman PJ, Greenleaf JF, Manduca A, Ehman RL. Magnetic resonance elastography by direct visualization of propagating acoustic strain waves. Science. 1995;269(5232):1854–7. doi: 10.1126/science.7569924. [DOI] [PubMed] [Google Scholar]
- [100].Nag AC. Study of non-muscle cells of the adult mammalian heart: a fine structural analysis and distribution. Cytobios. 1980;28(109):41–61. [PubMed] [Google Scholar]
- [101].Nassar RM, Reedy MC, Anderson PAW. Developmental changes in the ultrastructural and sarcomere shortening of the isolated rabbit ventricular myocyte. Circ Res. 1987;61(1):465–483. doi: 10.1161/01.res.61.3.465. [DOI] [PubMed] [Google Scholar]
- [102].Nelson CM, Jean RP, Tan JL, Liu WF, Sniadecki NJ, Spector AA, Chen CS. Emergent patterns of growth controlled by multicellular form and mechanics. Proc Natl Acad Sci U S A. 2005;102(33):11594–9. doi: 10.1073/pnas.0502575102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [103].Niggli E, Lederer WJ. Restoring forces in cardiac myocytes. Insight from relaxations induced by photolysis of caged ATP. Biophys J. 1991;59(5):1123–35. doi: 10.1016/S0006-3495(91)82327-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [104].Nishimura S, Nagai S, Katoh M, Yamashita H, Saeki Y, Okada J, Hisada T, Nagai R, Sugiura S. Microtubules modulate the stiffness of cardiomyocytes against shear stress. Circ Res. 2006;98(1):81–7. doi: 10.1161/01.RES.0000197785.51819.e8. [DOI] [PubMed] [Google Scholar]
- [105].Norman JJ, Collins JM, Sharma S, Russell B, Desai TA. Microstructures in 3D biological gels affect cell proliferation. Tissue Eng Part A. 2008;14(3):379–90. doi: 10.1089/tea.2007.0077. [DOI] [PubMed] [Google Scholar]
- [106].Norton JM. Toward consistent definitions for preload and afterload. Adv Physiol Educ. 2001;25(1-4):53–61. doi: 10.1152/advances.2001.25.1.53. [DOI] [PubMed] [Google Scholar]
- [107].Palmer RE, Brady AJ, Roos KP. Mechanical measurements from isolated cardiac myocytes using a pipette attachment system. Am J Physiol. 1996;270(2 Pt 1):C697–704. doi: 10.1152/ajpcell.1996.270.2.C697. [DOI] [PubMed] [Google Scholar]
- [108].Parker KK, Ingber DE. Extracellular matrix, mechanotransduction and structural hierarchies in heart tissue engineering. Philos Trans R Soc Lond B Biol Sci. 2007;362(1484):1267–79. doi: 10.1098/rstb.2007.2114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [109].Parker KK, Tan J, Chen CS, Tung L. Myofibrillar architecture in engineered cardiac myocytes. Circ Res. 2008;103(4):340–2. doi: 10.1161/CIRCRESAHA.108.182469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Patel AA, Thakar RG, Chown M, Ayala P, Desai TA, Kumar S. Biophysical mechanisms of single-cell interactions with microtopographical cues. Biomed Microdevices. 2010;12(2):287–96. doi: 10.1007/s10544-009-9384-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [111].Pinto JG, Win R. Non-uniform strain distribution in papillary muscles. Am J Physiol. 1977;233(3):H410–6. doi: 10.1152/ajpheart.1977.233.3.H410. [DOI] [PubMed] [Google Scholar]
- [112].Pizzo AM, Kokini K, Vaughn LC, Waisner BZ, Voytik-Harbin SL. Extracellular matrix (ECM) microstructural composition regulates local cell-ECM biomechanics and fundamental fibroblast behavior: a multidimensional perspective. J Appl Physiol. 2005;98(5):1909–21. doi: 10.1152/japplphysiol.01137.2004. [DOI] [PubMed] [Google Scholar]
- [113].Poobalarahi F, Baicu CF, Bradshaw AD. Cardiac myofibroblasts differentiated in 3D culture exhibit distinct changes in collagen I production, processing, and matrix deposition. Am J Physiol Heart Circ Physiol. 2006;291(6):H2924–32. doi: 10.1152/ajpheart.00153.2006. [DOI] [PubMed] [Google Scholar]
- [114].Porter KE, Turner NA. Cardiac fibroblasts: at the heart of myocardial remodeling. Pharmacol Ther. 2009;123(2):255–78. doi: 10.1016/j.pharmthera.2009.05.002. [DOI] [PubMed] [Google Scholar]
- [115].Pustoc’h A, Ohayon J, Usson Y, Kamgoue A, Tracqui P. An integrative model of the self-sustained oscillating contractions of cardiac myocytes. Acta Biotheor. 2005;53(4):277–93. doi: 10.1007/s10441-005-4880-5. [DOI] [PubMed] [Google Scholar]
- [116].Qin L, Huang J, Xiong C, Zhang Y, Fang J. Dynamical stress characterization and energy evaluation of single cardiac myocyte actuating on flexible substrate. Biochem Biophys Res Commun. 2007;360(2):352–6. doi: 10.1016/j.bbrc.2007.06.060. [DOI] [PubMed] [Google Scholar]
- [117].Rall JA. Sense and nonsense about the Fenn effect. Am J Physiol. 1982;242(1):H1–6. doi: 10.1152/ajpheart.1982.242.1.H1. [DOI] [PubMed] [Google Scholar]
- [118].Roeder BA, Kokini K, Robinson JP, Voytik-Harbin SL. Local, three-dimensional strain measurements within largely deformed extracellular matrix constructs. J Biomech Eng. 2004;126(6):699–708. doi: 10.1115/1.1824127. [DOI] [PubMed] [Google Scholar]
- [119].Russell B, Curtis MW, Koshman YE, Samarel AM. Mechanical stress-induced sarcomere assembly for cardiac muscle growth in length and width. J Mol Cell Cardiol. 2010;48(5):817–23. doi: 10.1016/j.yjmcc.2010.02.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [120].Russell B, Motlagh D, Ashley WW. Form follows function: how muscle shape is regulated by work. J Appl Physiol. 2000;88(3):1127–32. doi: 10.1152/jappl.2000.88.3.1127. [DOI] [PubMed] [Google Scholar]
- [121].Sadoshima J, Izumo S. Mechanotransduction in stretch-induced hypertrophy of cardiac myocytes. J Recept Res. 1993;13(1-4):777–94. doi: 10.3109/10799899309073692. [DOI] [PubMed] [Google Scholar]
- [122].Salameh A, Wustmann A, Karl S, Blanke K, Apel D, Rojas-Gomez D, Franke H, Mohr FW, Janousek J, Dhein S. Cyclic mechanical stretch induces cardiomyocyte orientation and polarization of the gap junction protein connexin43. Circ Res. 2010;106(10):1592–602. doi: 10.1161/CIRCRESAHA.109.214429. [DOI] [PubMed] [Google Scholar]
- [123].Samarel AM. Costameres, focal adhesions, and cardiomyocyte mechanotransduction. Am J Physiol Heart Circ Physiol. 2005;289(6):H2291–301. doi: 10.1152/ajpheart.00749.2005. [DOI] [PubMed] [Google Scholar]
- [124].Samuel JL, Vandenburgh HH. Mechanically induced orientation of adult rat cardiac myocytes in vitro. In Vitro Cell Dev Biol. 1990;26(9):905–14. doi: 10.1007/BF02624616. [DOI] [PubMed] [Google Scholar]
- [125].Sarvazyan AP, Rudenko OV, Swanson SD, Fowlkes JB, Emelianov SY. Shear wave elasticity imaging: a new ultrasonic technology of medical diagnostics. Ultrasound Med Biol. 1998;24(9):1419–35. doi: 10.1016/s0301-5629(98)00110-0. [DOI] [PubMed] [Google Scholar]
- [126].Senyo SE, Koshman YE, Russell B. Stimulus interval, rate and direction differentially regulate phosphorylation for mechanotransduction in neonatal cardiac myocytes. FEBS Lett. 2007;581(22):4241–7. doi: 10.1016/j.febslet.2007.07.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Serri K, Reant P, Lafitte M, Berhouet M, Le Bouffos V, Roudaut R, Lafitte S. Global and regional myocardial function quantification by two-dimensional strain: application in hypertrophic cardiomyopathy. J Am Coll Cardiol. 2006;47(6):1175–81. doi: 10.1016/j.jacc.2005.10.061. [DOI] [PubMed] [Google Scholar]
- [128].Sharp WW, Terracio L, Borg TK, Samarel AM. Contractile activity modulates actin synthesis and turnover in cultured neonatal rat heart cells. Circ Res. 1993;73(1):172–83. doi: 10.1161/01.res.73.1.172. [DOI] [PubMed] [Google Scholar]
- [129].Sharp WW, Simpson DG, Borg TK, Samarel AM, Terracio L. Mechanical forces regulate focal adhesion and costamere assembly in cardiac myocytes. J Physiol. 1997;273(2 Pt 2):H546–56. doi: 10.1152/ajpheart.1997.273.2.H546. [DOI] [PubMed] [Google Scholar]
- [130].Simpson DG, Majeski M, Borg TK, Terracio L. Regulation of cardiac myocyte protein turnover and myofibrillar structure in vitro by specific directions of stretch. Circ Res. 1999;85(10):e59–69. doi: 10.1161/01.res.85.10.e59. [DOI] [PubMed] [Google Scholar]
- [131].Sollott SJ, Lakatta EG. Novel method to alter length and load in isolated mammalian cardiac myocytes. Am J Physiol. 1994;267(4 Pt 2):H1619–29. doi: 10.1152/ajpheart.1994.267.4.H1619. [DOI] [PubMed] [Google Scholar]
- [132].Spurgeon HA, Stern MD, Baartz G, Raffaeli S, Hansford RG, Talo A, Lakatta EG, Capogrossi MC. Simultaneous measurement of Ca++, contraction, and potential in cardiac myocytes. Am J Physiol. 1990;258(1):H574–H586. doi: 10.1152/ajpheart.1990.258.2.H574. [DOI] [PubMed] [Google Scholar]
- [133].Steadman BW, Moore KB, Spitzer KW, Bridge JHB. A video system for measuring motion in contracting heart cells. IEEE Trans Biomed Eng. 1988;35(1):264–272. doi: 10.1109/10.1375. [DOI] [PubMed] [Google Scholar]
- [134].Street SF. Lateral transmission of tension in frog myofibers: a myofibrillar network and transverse cytoskeletal connections are possible transmitters. J Cell Physiol. 1983;114(3):346–64. doi: 10.1002/jcp.1041140314. [DOI] [PubMed] [Google Scholar]
- [135].Su J, Jiang X, Welsch R, Whitesides GM, So PT. Geometric confinement influences cellular mechanical properties I -- adhesion area dependence. Mol Cell Biomech. 2007;4(2):87–104. [PubMed] [Google Scholar]
- [136].Sugiura S, Nishimura S, Yasuda S, Hosoya Y, Katoh K. Carbon fiber technique for the investigation of single-cell mechanics in intact cardiac myocytes. Nat Protoc. 2006;1(3):1453–7. doi: 10.1038/nprot.2006.241. [DOI] [PubMed] [Google Scholar]
- [137].Takagi Y, Homsher EE, Goldman YE, Shuman H. Force generation in single conventional actomyosin complexes under high dynamic load. Biophys J. 2006;90(4):1295–307. doi: 10.1529/biophysj.105.068429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [138].Takakuda K, Miyairi H. Tensile behaviour of fibroblasts cultured in collagen gel. Biomaterials. 1996;17(14):1393–7. doi: 10.1016/0142-9612(96)87280-2. [DOI] [PubMed] [Google Scholar]
- [139].Tamariz E, Grinnell F. Modulation of fibroblast morphology and adhesion during collagen matrix remodeling. Mol Biol Cell. 2002;13(11):3915–29. doi: 10.1091/mbc.E02-05-0291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [140].Tan JL, Tien J, Pirone DM, Gray DS, Bhadriraju K, Chen CS. Cells lying on a bed of microneedles: an approach to isolate mechanical force. Proc Natl Acad Sci U S A. 2003;100(4):1484–9. doi: 10.1073/pnas.0235407100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [141].Terracio L, Miller B, Borg TK. Effects of cyclic mechanical stimulation of the cellular components of the heart: in vitro. In Vitro Cell Dev Biol. 1988;24(1):53–8. doi: 10.1007/BF02623815. [DOI] [PubMed] [Google Scholar]
- [142].Thakar RG, Chown MG, Patel A, Peng L, Kumar S, Desai TA. Contractility-dependent modulation of cell proliferation and adhesion by microscale topographical cues. Small. 2008;4(9):1416–24. doi: 10.1002/smll.200701302. [DOI] [PubMed] [Google Scholar]
- [143].Thoumine O, Ott A. Time scale dependent viscoelastic and contractile regimes in fibroblasts probed by microplate manipulation. J Cell Sci. 1997;110(Pt 17):2109–16. doi: 10.1242/jcs.110.17.2109. [DOI] [PubMed] [Google Scholar]
- [144].Torsoni AS, Constancio SS, Nadruz W, Jr, Hanks SK, Franchini KG. Focal adhesion kinase is activated and mediates the early hypertrophic response to stretch in cardiac myocytes. Circ Res. 2003;93(2):140–7. doi: 10.1161/01.RES.0000081595.25297.1B. [DOI] [PubMed] [Google Scholar]
- [145].Tracqui P, Ohayon J, Boudou T. Theoretical analysis of the adaptive contractile behaviour of a single cardiomyocyte cultured on elastic substrates with varying stiffness. J Theor Biol. 2008;255(1):92–105. doi: 10.1016/j.jtbi.2008.07.036. [DOI] [PubMed] [Google Scholar]
- [146].Varner VD, Voronov DA, Taber LA. Mechanics of head fold formation: investigating tissue-level forces during early development. Development. 2010;137(22):3801–11. doi: 10.1242/dev.054387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].Wang N, Butler JP, Ingber DE. Mechanotransduction across the cell surface and through the cytoskeleton. Science. 1993;260(5111):1124–7. doi: 10.1126/science.7684161. [DOI] [PubMed] [Google Scholar]
- [148].Wang JH, Lin JS. Cell traction force and measurement methods. Biomech Model Mechanobiol. 2007;6(6):361–71. doi: 10.1007/s10237-006-0068-4. [DOI] [PubMed] [Google Scholar]
- [149].Wang N, Tolić-Nørrelykke IM, Chen J, Mijailovich SM, Butler JP, Fredberg JJ, Stamenović D. Cell prestress. I. Stiffness and prestress are closely associated in adherent contractile cells. Am J Physiol Cell Physiol. 2002;282(3):C606–16. doi: 10.1152/ajpcell.00269.2001. [DOI] [PubMed] [Google Scholar]
- [150].Wei Z, Deshpande VS, McMeeking RM, Evans AG. Analysis and interpretation of stress fiber organization in cells subject to cyclic stretch. J Biomech Eng. 2008;130(3):031009. doi: 10.1115/1.2907745. [DOI] [PubMed] [Google Scholar]
- [151].Wen H, Bennett E, Epstein N, Plehn J. Magnetic resonance imaging assessment of myocardial elastic modulus and viscosity using displacement imaging and phase-contrast velocity mapping. Magn Reson Med. 2005;54(3):538–48. doi: 10.1002/mrm.20589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [152].White E, Boyett MR, Orchard CH. The effects of mechanical loading and changes of length on single guinea-pig ventricular myocytes. J Physiol. 1995;482(Pt 1):93–107. doi: 10.1113/jphysiol.1995.sp020502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [153].Witt SH, Labeit D, Granzier H, Labeit S, Witt CC. Dimerization of the cardiac ankyrin protein CARP: implications for MARP titin-based signaling. J Muscle Res Cell Motil. 2005;26(6-8):401–8. doi: 10.1007/s10974-005-9022-9. [DOI] [PubMed] [Google Scholar]
- [154].Wozniak MA, Chen CS. Mechanotransduction in development: a growing role for contractility. Nat Rev Mol Cell Biol. 2009;10(1):34–43. doi: 10.1038/nrm2592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [155].Yamada K, Green KG, Samarel AM, Saffitz JE. Distinct pathways regulate expression of cardiac electrical and mechanical junction proteins in response to stretch. Circ Res. 2005;97(4):346–53. doi: 10.1161/01.RES.0000178788.76568.8a. [DOI] [PubMed] [Google Scholar]
- [156].Yamane M, Matsuda T, Ito T, Fujio Y, Takahashi K, Azuma J. Rac1 activity is required for cardiac myocyte alignment in response to mechanical stress. Biochem Biophys Res Commun. 2007;353(4):1023–7. doi: 10.1016/j.bbrc.2006.12.144. [DOI] [PubMed] [Google Scholar]
- [157].Yamazaki T, Komuro I, Kudoh S, Zou Y, Shiojima I, Mizuno T, Takano H, Hiroi Y, Ueki K, Tobe K. Mechanical stress activates protein kinase cascade of phosphorylation in neonatal rat cardiac myocytes. J Clin Invest. 1995;96(1):438–46. doi: 10.1172/JCI118054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [158].Yu JG, Russell B. Cardiomyocyte remodeling and sarcomere addition after uniaxial static strain in vitro. J Histochem Cytochem. 2005;53(7):839–44. doi: 10.1369/jhc.4A6608.2005. [DOI] [PubMed] [Google Scholar]
- [159].Zemel A, Safran SA. Active self-polarization of contractile cells in asymmetrically shaped domains. Phys Rev E Stat Nonlin Soft Matter Phys. 2007;76(2 Pt 1):021905. doi: 10.1103/PhysRevE.76.021905. [DOI] [PubMed] [Google Scholar]
- [160].Zhao Y, Lim CC, Sawyer DB, Liao R, Zhang X. Simultaneous orientation and cellular force measurements in adult cardiac myocytes using three-dimensional polymeric microstructures. Cell Motil Cytoskeleton. 2007;64(9):718–25. doi: 10.1002/cm.20218. [DOI] [PubMed] [Google Scholar]
- [161].Zhu J, Sabharwal T, Kalyanasundaram A, Guo L, Wang G. Topographic mapping and compression elasticity analysis of skinned cardiac muscle fibers in vitro with atomic force microscopy and nanoindentation. J Biomech. 2009;42(13):2143–50. doi: 10.1016/j.jbiomech.2009.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]