Abstract
Background:
Many weight loss programmes show short-term success, but long-term data in larger studies are scarce, especially in community settings. Attrition is common and complicates the interpretation of long-term outcomes.
Objective:
To investigate 2-year outcomes and explore issues of attrition and missing data.
Subjects:
A total of 772 overweight and obese adults recruited by primary care practices in Australia, Germany and the UK and randomised to a 12-month weight loss intervention delivered in a commercial programme (CP) or in standard care (SC).
Measurement:
Weight change from 0–24 and 12–24 months including measured weights only and measured and self-reported weights, using last observation carried forward (LOCF), baseline observation carried forward (BOCF), completers-only and missing-at-random (MAR) analyses.
Results:
A total of 203 participants completed the 24-month visit. Using measured weights only, there was a trend for greater 24-month weight loss in CP than in SC, but the difference was only statistically significant in the LOCF and BOCF analyses: LOCF: −4.14 vs −1.99 kg, difference adjusted for centre −2.08 kg, P<0.001; BOCF: −1.33 vs −0.74 kg, adjusted difference −0.60 kg, P=0.032; completers: −4.76 vs −2.99 kg, adjusted difference −1.53 kg, P=0.113; missing at random: −3.00 vs −1.94 kg, adjusted difference −1.04 kg, P=0.150. Both groups gained weight from 12–24 months and weight regain was significantly (P<0.001) greater for CP than for SC in all analysis approaches. Inclusion of self-reported weights from a further 138 participants did not change the interpretation of the findings.
Conclusion:
Initial weight loss was poorly maintained during the no-intervention follow-up, but both groups did have lower weight over the 24 months. Attrition was high in both groups, and assumptions about missing data had considerable impact on the magnitude and statistical significance of treatment effects. It is vital that trials on weight loss interventions consider the plausibility of these differences in an analytical approach when interpreting research findings and comparing data between studies.
Keywords: weight loss, weight maintenance, primary care
Introduction
Obesity is a major public health problem and its prevalence is increasing in many countries, along with the ensuing burden of disease.1 Weight loss is difficult to achieve for many and challenging to maintain for most. Most trials, using various therapeutic modalities, are plagued by subsequent weight regain. A systematic review of weight maintenance after lifestyle interventions found that approximately half of the weight lost is regained within 1 year of treatment cessation.2 Even within weight loss trials of continual intervention, weight regain is prominent.3
Our understanding of weight loss and regain is complicated by high attrition rates of up to 90% in obesity treatment trials.4 High dropout rates produce difficulties in analysis and interpretation of results in all clinical trials. This issue has recently received increased attention. Little et al.5 outlined a number of suggestions for improving future research, including improved trial design, subject retention plans, long-term follow-up procedures and different methods of statistical analysis.
We previously reported on the 12-month outcome of a weight loss trial comparing primary care referral to a commercial programme (CP) and standard care (SC).6 The first aim of the present investigation is to show the 24-month outcome data from this randomised controlled weight loss trial. The second aim is to use a range of statistical approaches using both measured and self-reported data for body weight to highlight some of the issues associated with attrition in weight loss studies, and to explore how different approaches and assumptions about missing data affect the interpretation of long-term outcomes. We examine ways of mitigating these effects and make recommendations for future research.
Methods
Study design and participants
Full details of the intervention have been published previously.6 In brief, 772 participants (age ⩾18 years, body mass index of 27–35 kg m−2 plus at least one additional risk factor of an obesity-related disease) were recruited from primary care practices in Australia, Germany and the UK and randomised in a 1:1 ratio to receive CP or SC for the first 12 months. Participants were recruited between September 2007 and November 2008.
Ethical approval was received from the Royal Prince Alfred Hospital zone of the Sydney South West Area Health Service (Australia), the Faculty of Medicine of the Technische Universität München (Germany) and the Nottingham Research Ethics Committee (UK) with amendments to allow follow-up at 18 and 24 months and conduct a telephone/questionnaire survey. All patients provided written informed consent. This trial is registered under number ISRCTN85485463.
Procedures
Participants attending the 12-month visit were asked to consent to follow-up at 18 and 24 months, during which time they could self-select their method of weight management independent of the interventions offered during the first 12 months. Body weight was measured according to the same standardized procedures used in the earlier assessments.6
All participants who did not complete the 24-month visit but had not formally withdrawn from the study were asked to provide self-reported weights in a telephone follow-up survey (Australia and the UK) or a postal survey (Germany). Three attempts were made to call each person or two postal surveys were sent before they were recorded as lost to follow-up.
Statistical analysis
The effect of missing data was investigated as part of a sensitivity analysis: last observation carried forward (LOCF) analysis, baseline observation carried forward (BOCF) analysis, completers-only analysis and a missing-at-random (MAR) analysis using a variance components model.
The primary outcome was change in measured weight between baseline and 24 months. Secondary outcomes were change in measured weight between 12 and 24 months and changes in measured and self-reported weights between baseline and 12 months and between 12 and 24 months. For the LOCF, BOCF and completers-only analyses, fixed effect models for continuous normal data were fitted. The fixed effects were intervention group (CP vs SC), centre (Australia, Germany, UK) and baseline measurement. For the MAR analysis, a model for multivariate normal data with the same fixed effects was fitted using measured weights at every time point (2, 4, 6, 9, 12, 18 and 24 months) using generalised least squares (GLS).
To assess the relationship between weight change over the intervention period and attendance at the 24-month clinic visit, three logistic regression models were fitted with 24-month attendance as the outcome variable and intervention period weight loss (kg), 5% weight loss and 10% weight loss as fixed effects. To assess the association between baseline weight and the 24-month attendance, a further logistic regression model was fitted with baseline weight as the fixed effect term.
In sub-analyses, weight maintenance was defined as ±2 kg of the weight recorded at 12 months.6 Weight maintenance between intervention groups was compared via a logistic regression model. The outcome variable was a binary indicator for weight maintenance, and an intervention group was included as a fixed effect. In addition, to assess the association between weight change over the intervention period and weight change during follow-up for completers, a linear model was fitted with follow-up weight gain as the outcome variable and weight loss over the intervention period as a fixed effect.
All analyses were adjusted for centre and conducted using R (version 2.4.1).
Results
Attendance at 24-month follow-up
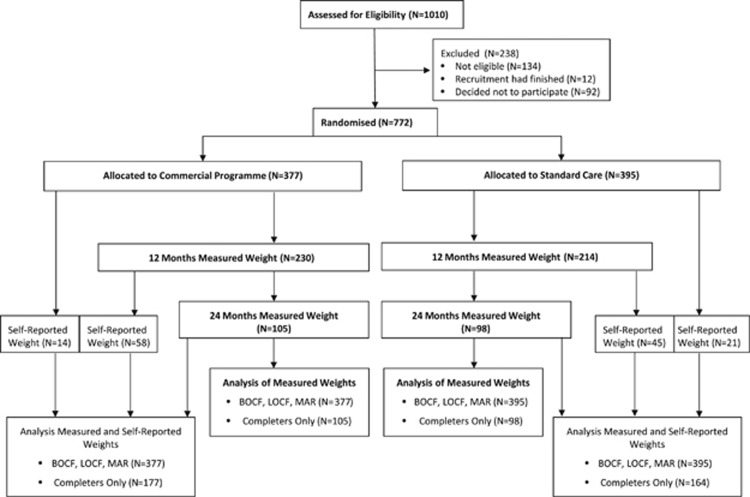
A total of 203 participants (26% of those randomised) completed the 24-month visit (Figure 1). Self-reported weight data were available from an additional 138 participants who had not attended the 24-month clinic assessment (18%), including 35 persons who had not completed the 12-month assessment.
Figure 1.
Study flow diagram from recruitment to 24 months of follow-up. BOCF, baseline observation carried forward; LOCF, last observation carried forward; MAR, missing at random.
Table 1 presents the characteristics of participants. Those who attended the 24-month visit were older than those who provided a self-reported weight and those who did not provide a final weight. More participants in Germany (113 out of 268 participants randomised; 42%) attended the final measurement appointment compared with Australia (66 out of 268 participants randomised; 25%) and UK (24 out of 236 participants randomised; 10%) participants.
Table 1. Characteristics of participants.
| Measured final weight (N=203) | Self-reported final weight (N=138) | No recorded final weight (N=431) | P-valuea | |
|---|---|---|---|---|
| Baseline age (years) | 51.99±13.00 | 48.94±12.30 | 44.72±12.31 | 0.029 |
| Baseline weight (kg) | 85.83±11.40 | 87.59±12.47 | 86.84±11.26 | 0.188 |
| Females (N (%)) | 171 (84.24%) | 119 (86.23%) | 378 (87.70%) | 0.725 |
| Mean 12-month weight change (kg) | −5.79±5.98 (N=203) | −5.18±6.84 (N=103) | −3.75±4.99 (N=138) | 0.442 |
| Mean 24-month weight change (kg) | −3.90±6.90 | −2.81±5.93 | — | 0.119 |
Mean (± standard deviation) is given if not otherwise noted.
P-value is given for the difference between the group with measured and the group with self-reported final weight (the t-test; the chi-square test was used for comparison of the proportion of female participants).
The greater the weight loss during active intervention (baseline to 12 months), the higher the chance of attending the 24-month follow-up (odds ratio (OR)=1.06 (95% confidence interval (CI): 1.02, 1.10), P=0.001). Participants who lost ⩾5% of baseline weight during the intervention had increased odds of attending the 24-month visit (OR=1.88 (CI: 1.27, 2.82), P=0.002). Those who lost ⩾10% were more likely to attend the 24-month follow-up (OR=2.14 (CI: 1.34, 3.44), P=0.001) compared with those who lost <10%. There was also a trend for participants with higher baseline weights not to attend the 24-month follow-up (for a 10 kg difference in baseline weight OR=0.83 (CI: 0.71, 0.97), P=0.020).
Weight change from baseline to 24 months
Measured weights only
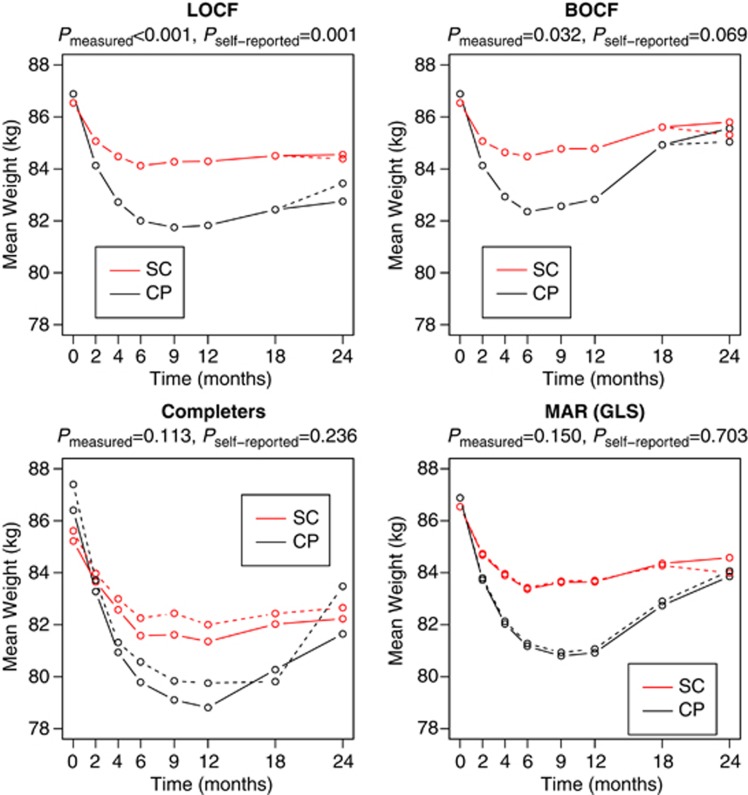
Figure 2 and Table 2A show weight change from baseline for participants who attended the 24-month visit using four different statistical analysis approaches. Participants in both groups lost weight over 24 months, and the estimates for the weight loss difference between the groups (adjusted by centre) for all analysis approaches suggest that weight loss was greater for CP than for SC. This difference was only statistically significant in the LOCF and BOCF analyses and was smaller than the difference at 12 months.
Figure 2.
Change in weight for participants randomised to a CP or SC for each analysis approach. In all plots, the solid lines denote that only clinically measured weights are included; that is, weight treated as missing at 24 months for participants who self-reported. In contrast, the dashed lines denote that self-reported weights are included; that is, self-reported weights are considered the same as measured weights. The LOCF and BOCF plots show the weight trajectories for participants when missing weight data are replaced by the last measured value or baseline value, respectively. The completers plot shows the weight trajectories for only those participants with a non-missing 24-month weight. The MAR (GLS) estimates plot shows the estimated weight trajectories based upon the models fitted under the MAR assumption. P-values indicate the significance of the difference between CP and SC at 24 months. CP, commercial programme; SC, standard care; LOCF, last observation carried forward; BOCF, baseline observation carried forward; MAR, missing at random; GLS, generalised least squares.
Table 2. Weight change between baseline and 24 months using measured weights only (A) or using both measured and self-reported weights (B).
| Analysis | N |
Mean weight change (s.d.) in kg |
Adjusted difference (CI) in kg | P-value | |
|---|---|---|---|---|---|
| CP | SC | ||||
| A) Measured weights only | |||||
| LOCF | 772 | −4.14 (6.07) | −1.99 (4.56) | −2.08 (−2.83, −1.33) | <0.001 |
| BOCF | 772 | −1.33 (4.53) | −0.74 (3.23) | −0.60 (−1.16, −0.05) | 0.032 |
| Completersa | 203 | −4.76 (7.60) | −2.99 (5.97) | −1.53 (−3.43, 0.37) | 0.113 |
| MAR (GLS) | 772 | −3.00 | −1.94 | −1.04 (−2.44, 0.37) | 0.150 |
| B) Measured and self-reported weights | |||||
| LOCF | 772 | −3.44 (5.97) | −2.15 (4.78) | −1.25 (−2.02, −0.49) | 0.001 |
| BOCF | 772 | −1.84 (5.26) | −1.23 (4.02) | −0.61 (−1.27, 0.05) | 0.069 |
| Completersb | 341 | −3.92 (7.13) | −2.96 (5.82) | −0.84 (−2.24, 0.56) | 0.236 |
| MAR (GLS) | 772 | −2.81 | −2.55 | −0.24 (−1.46, 0.98) | 0.703 |
Abbreviations: BOCF, baseline observation carried forward; CI, 95% confidence interval; CP, commercial programme; kg, kilogram; LOCF, last observation carried forward; MAR, missing at random; GLS, generalised least squares; SC, standard care; s.d., standard deviation.
P-value is given for the treatment difference.
completers are defined as those participants who provided a measured weight at 24 months.
completers are defined as those participants who provided either a measured or self-reported weight at 24 months.
In the CP group 48% (50/105) lost ⩾5% and 24% (25/105) lost ⩾10% of their body weight over the 24-month period compared with 36% (35/98) and 13% (13/98), respectively, in the SC group. By 24 months, 29% (58/203) of all completers (27% (28/105) in CP vs 31% (30/98) in the SC group) were heavier than at baseline by a mean of 2.3 kg (for the groups combined).
Measured and self-reported weights
Self-reported weight data were collected over a broad time range; the median number of days from baseline for measured weights was 755 days compared with 955 days for self-reported weights. However, for the purposes of this analysis, we assume that the data were collected at 24 months. The mean self-reported weight loss was 2.81 kg (s.d. 5.93 kg) and the mean objectively measured weight loss was 3.90 kg (s.d. 6.90 kg) for the intervention groups combined. It is hard to compare these observational results because of bias due to different measurement times, different instruments of measurement and treatment imbalance. Figure 2 and Table 2B show the 24-month weight change when self-reported weights were included for each analysis approach. Estimates for all analysis approaches still suggest a greater weight loss in CP than in SC, but this difference is only significant in the LOCF analysis.
Weight change between 12 and 24 months
Measured weights only
Table 3A shows changes in measured weight from 12–24 months among participants who were weighed at 24 months. On average, both groups gained weight, but weight regain was significantly greater for the CP group than for the SC group in all analyses. Weight loss over the intervention period was not significantly associated with weight change over the follow-up period (coefficient estimate 0.06 (CI:−0.03, 0.15); P=0.208).
Table 3. Weight change between 12 and 24 months using measured weights only (A) or using both measured and self-reported weights (B).
| Analysis | N | Mean weight change (s.d.) in kg | Adjusted difference (CI) in kg | P-value | |
|---|---|---|---|---|---|
| |
|
CP |
SC |
|
|
| A) Measured weights only | |||||
| LOCF | 772 | 0.92 (2.42) | 0.26 (2.20) | 0.69 (0.36, 1.01) | <0.001 |
| BOCF | 772 | 2.73 (4.82) | 1.02 (3.50) | 1.68 (1.09, 2.28) | <0.001 |
| Completersa | 203 | 2.83 (3.58) | 0.88 (4.14) | 1.97 (0.89, 3.05) | <0.001 |
| MAR (GLS) | 772 | 2.94 | 0.93 | 2.01 (0.98, 3.03) | <0.001 |
| B) Measured and self-reported weights | |||||
| LOCF | 772 | 1.62 (4.03) | 0.10 (3.04) | 1.51 (1.01, 2.02) | <0.001 |
| BOCF | 772 | 2.21 (4.57) | 0.53 (3.87) | 1.68 (1.08, 2.27) | <0.001 |
| Completersb | 306 | 3.27 (5.01) | 0.46 (4.30) | 2.71 (1.63, 3.79) | <0.001 |
| MAR (GLS) | 772 | 3.00 | 0.29 | 2.72 (1.70, 3.73) | <0.001 |
Abbreviations: BOCF, baseline observation carried forward; CI, 95% confidence interval; CP, commercial programme; kg, kilogram; LOCF, last observation carried forward; MAR, missing at random; GLS, generalised least squares; SC, standard care; s.d., standard deviation.
P-value is given for the treatment difference.
completers are defined as those participants who provided measured weight data at baseline, after 12 and 24 months.
completers are defined as those participants who provided a measured weight at baseline and at 12 months and either a measured or self-reported weight at 24 months. Those who did not attend the 12-month visit but provided self-reported 24-month weight data (n=35) are not included.
Most participants in both intervention groups (83% in CP and 62% in SC) regained weight. Of the 200 participants who attended both their 18- and 24-month visits, 57 participants (29%) remained within ±2 kg of their 12-month weight at both visits. There was no significant difference between treatment groups in the proportion of participants whose weight stayed within this range (OR=0.64 (CI: 0.34, 1.20), P=0.17).
Measured and self-reported weights
Table 3B shows the changes in weight from 12–24 months using data from both measured and self-reported weights. Again, both groups regained weight and this was significantly greater for CP than for SC in all analyses. The difference in weight regain between groups was greater than in the analysis for measured weights only.
Discussion
This trial presents a clear example of the high rates of attrition that can occur in trials on obesity treatment, with only 26% of those randomised providing a measured weight at 24 months and a further 18% providing a self-reported final weight. In this particular trial, the loss to follow-up may have been exacerbated by the community setting and lack of planned post-intervention follow-up at initial enrolment.
High rates of attrition are very common in weight loss trials,4 where lack of return to follow-up could be because the outcome is self-evident to participants and does not require any clinical interpretation. Those who fail to achieve their weight loss goal might be less motivated to return to the clinic or respond to requests, as they might perceive the follow-up as part of the failed treatment or feel embarrassed to show the investigator they have been unable to achieve or sustain weight loss. This is a particular issue for a dietary programme in which lack of success may be more likely to be perceived as a personal failure than a pharmacological intervention that might be more likely viewed as lack of efficacy of the drug.
It is noteworthy that attrition was highest in the UK, where participants had no contact with specialist research facilities and the follow-up was conducted entirely within the primary care setting.6 As well as the general practitioners, the study team in Germany had close contact with the study participants, as the bio-impedance analysis was performed at the study centre.6 The dedicated research staff were able to spend more time with participants and adapt a more flexible schedule for appointments. From this, it was learned that close contact with study participants is important to retain participants and reduce the attrition rate. Furthermore, in the German study arm, participants were given a small monetary incentive for undergoing bio-impedance measurement.
Loss to follow-up has significant implications for the analysis and interpretation of data in all weight loss trials, as analytical methods make different assumptions about the values of missing data. The completers-only analysis might be biased if there is a difference in the weight trajectory between those who complete the follow-up assessment and those who do not. Our observation of greater weight loss from baseline among those attending the 24-month visit relative to those self-reporting data might indicate a difference. Analyses based on an intention-to-treat basis are often favoured in clinical trials. The assumption that would justify the use of LOCF analysis is that participants do not change weight after they drop out, but this does not concur with the known difficulties of weight loss maintenance and the marked weight regain evident in this and other studies. The assumption that would justify the use of BOCF analysis is that participants who dropped out of the study returned to their baseline weight and, implicitly, that the same amount of weight is regained regardless of the length of follow-up after the last measured weight. These imputation methods also lead to smaller treatment effect variances, as there is no measurement error in an imputed weight. MAR analysis is appealing, as all observed weight data from all visits are included in the analysis. However, the assumption here is that the chance an individual drops out of the study depends only on the observed data, such as participants' characteristics, and we must consider the possibility that participants who drop out of the study differ from completers in ways that are not captured by the observed data.
At 12 months we demonstrated that the CP was associated with significantly greater weight loss compared with the SC, and this was robust to each of the three assumptions tested (BOCF, LOCF and completers-only), as well as to MAR and to further sensitivity analyses that tested departures from these assumptions.6, 7 In contrast, this analysis of data at 24 months shows that the method of statistical analysis does have an impact on the interpretation of the efficacy of treatment, both in terms of the magnitude of weight change and statistical significance of the difference between groups.7 Here, in the completers analysis an estimated weight loss difference between CP and SC of −1.53 kg is not significant, whereas in the LOCF and BOCF analyses differences of −2.08 and −0.60 kg are significant. In these analyses, the imputation of missing data artificially boosts the sample size and increases the power of the analysis, such that even the smaller difference between treatments in the BOCF analysis reaches statistical significance. This challenges a common assertion that BOCF is the most conservative analysis approach. We might infer that there is greater weight loss at 24 months in CP than in SC, but this difference is clinically small (−0.60 to −2.08 kg) and the finding is not statistically robust.
Comparing multiple methods of missing data imputation is one way of examining the robustness of trial findings, but it is clear that none of these methods can represent the true weight change of participants lost to follow-up. Researchers should be alert to continued improvements in statistical modelling techniques. It might be possible to improve estimates by incorporating data on other variables that influence adherence and/or weight trajectories in the model. Further, principled sensitivity analyses to assess the effect of departures from analysis assumptions should be considered.8
Limiting the burden of data collection can help increase retention, and we attempted to compensate for the extent of missing data at 24 months by obtaining self-reported data for weight (primary outcome) from all those who had been lost to follow-up but we were able to trace. This yielded an additional 138 participants, boosting the sample to 44% of those randomised and giving a fuller picture of the weight trajectory of the wider sample. However, these self-reported weights alter the size and statistical significance of weight differences and must be interpreted with caution. Recent data on self-reported vs measured weight from a national representative population in the UK showed that, on average, women underestimated their weight by 2.4 kg and men by 1.4 kg.9 However, this may not adequately reflect the experience of those recently attempting to lose weight. We attempted to make self-reported weights more accurate by asking participants to weigh themselves at home before the survey. However, with the delay incurred through applying for further ethical approval to contact these individuals and the time taken to elicit responses, these measures were on average 200 days later than the measured weight data at visits, and we could surmise that additional weight could have been regained during this extended time, reducing the observed weight loss. Further explorations of the data did not suggest an association between self-reported weight and time measurement (data not shown). Moreover, those giving a self-reported weight were characteristically different from those who attended the 24-month visit, having lost less weight during the active intervention, and might be expected to have a different subsequent weight trajectory, so it would be preferable to reduce uncertainty by eliciting self-reported weights from a subsample of participants for whom body weight is subsequently measured.10, 11
As recently highlighted, it is not only weight loss trials that suffer from issues of missing data, and a number of practical suggestions have been made for maximising follow-up data.5 Researchers should design trials to include methods including self-report where necessary to obtain a final measurement of the primary outcome even if participants have dropped out of the intervention or are unwilling to complete all planned measures.
It seems reasonable to conclude that initial weight loss is poorly maintained during a subsequent year in which no further intervention was provided. Differences between initial treatment allocation groups still show a tendency to favour CP over SC but the differences are much smaller after 1 year of follow-up (24 months) than observed after 12 months of active intervention, with participants in the CP group experiencing on average greater weight regain from 12 to 24 months. Even among participants who completed the study, who appear to be more successful than the average participant, almost a third of those in both CP and SC groups were heavier at 24 months than at baseline. More research is needed to uncover the strategies used that facilitate weight loss maintenance.
Post-treatment weight regain is seen even within research-centre-based trials on more intensive psychological therapies and in trials with continual intervention.12, 13 For example, in a recent trial on continuous 24-month interventions, participants receiving brief lifestyle counselling (monthly counselling sessions) lost 2.9 kg at 24 months, similar to the CP group in the present investigation, although those receiving enhanced lifestyle counselling, with additional pharmacotherapy or use of meal replacement products, lost 4.6 kg.14 In the Look Ahead Study with intensive lifestyle intervention in the first year and continued but less frequent contact during years 2–4, considerable weight regain was also seen.3 However, the fact that weight regain is common should not mean it is viewed as inevitable. In any treatment programme, a proportion of participants successfully lose weight and keep it off. Further research is needed to understand this inter-individual variability. Our study is limited in the fact that we have no data about the weight management strategies utilised during the second set of 12 months. The seeming inevitability of weight regain in the majority should neither make us complacent nor deter us from endeavouring to find interventions that can help sustain weight loss maintenance. We posit that novel interventions may be required to develop the skills for weight maintenance, rather than simply a continuation or reinforcement of those developed for weight loss.
In relation to attrition, missing data and the 24-month weight outcome, our data show results similar to those of other 2-year weight loss studies, but with active intervention in the second year. The different statistical approaches for dealing with high attrition rates in weight loss studies as well as the imputation of data (self-reported data in our study) demonstrate similar results, and it appears that this method is a reasonable approach for use with the inevitable attrition in weight loss trials.
Acknowledgments
We thank participants and the staff of participating primary care practices for their contribution to the trial. The authors had full access to all the data in the study, and the corresponding author had the final responsibility for the decision to submit for publication. Weight Watchers International, through a grant to the UK Medical Research Council. The CP intervention was delivered by an employee of the sponsor, but the sponsor had no role in the study design, data collection, data analysis, data interpretation or writing of the report.
Author contribution
APM, IDC, SAJ and HH contributed to the study conception and design. APM, IDC, SAJ and HH obtained funding. CH, ALA, ME, NRF, JS, IDC, SAJ and HH contributed to the acquisition of data. CH, LC, ALA, APM, IDC, SAJ and HH analysed and interpreted the data. CH, LC, ALA, APM, IDC, SAJ and HH drafted the report, and all authors contributed to revision of the report.
All authors declare financial support to their institutions for the submitted work from Weight Watchers. LC has received payment from LighterLife Ltd. for consultancy services. SAJ has received research grants for other clinical trials from Sanofi-Aventis and Coca Cola. IDC and NRF have received research grants for other clinical trials funded by Sanofi-Aventis, Allergan, Roche Products, MSD, Novo Nordisk and GlaxoSmithKline. NRF has received conference travel expenses from Allergan. HH has received a travel grant from Roche. SAJ is a member of the Tanita Medical Advisory Board and has received payment for nutrition articles and lectures for Rosemary Conley Enterprises. HH is on the Advisory Board for Weight Watchers International and has received payment for lectures from Sara Lee, Lilly, Novartis, Sanofi-Aventis and Bristol-Myers Squibb. IDC was a board member for the SCOUT trial and has received payment for lectures from iNova Pharmaceuticals, Eisai Pharmaceuticals, Pfizer Australia and Servier Laboratories (Australia).
References
- WHO . Global Health Risks: Mortality and Burden of Disease Attributable to Selected Major Risks. World Health Organization; 2009. [Google Scholar]
- Barte JC, ter Bogt NC, Bogers RP, Teixeira PJ, Blissmer B, Mori TA, et al. Maintenance of weight loss after lifestyle interventions for overweight and obesity, a systematic review. Obes Rev. 2010;11:899–906. doi: 10.1111/j.1467-789X.2010.00740.x. [DOI] [PubMed] [Google Scholar]
- Wadden TA, Neiberg RH, Wing RR, Clark JM, Delahanty LM, Hill JO, et al. Four-year weight losses in the Look AHEAD study: factors associated with long-term success. Obesity. 2011;19:1987–1998. doi: 10.1038/oby.2011.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moroshko I, Brennan L, ÒBrien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obes Rev. 2011;12:912–934. doi: 10.1111/j.1467-789X.2011.00915.x. [DOI] [PubMed] [Google Scholar]
- Little RJ, D'Agostino R, Cohen ML, Dickersin K, Emerson SS, Farrar JT, et al. The prevention and treatment of missing data in clinical trials. N Engl J Med. 2012;367:1355–1360. doi: 10.1056/NEJMsr1203730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jebb SA, Ahern AL, Olson AD, Aston LM, Holzapfel C, Stoll J, et al. Primary care referral to a commercial provider for weight loss treatment versus standard care: a randomised controlled trial. Lancet. 2011;378:1485–1492. doi: 10.1016/S0140-6736(11)61344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mander AP, Ahern AL, Caterson ID, Hauner H, Jebb SA. Weight loss in a commercial setting. Lancet. 2012;379:1003. doi: 10.1016/S0140-6736(12)60424-3. [DOI] [PubMed] [Google Scholar]
- White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ. 2011;342:d40. doi: 10.1136/bmj.d40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Survey for England 2011: Health, Social Care and Lifestyles. Health and Social Care Information Centre: Leeds; 2012. [Google Scholar]
- Wolf AM, Finer N, Allshouse AA, Pendergast KB, Sherrill BH, Caterson I, et al. PROCEED: Prospective Obesity Cohort of Economic Evaluation and Determinants: baseline health and healthcare utilization of the US sample. Diabetes Obes Metab. 2008;10:1248–1260. doi: 10.1111/j.1463-1326.2008.00895.x. [DOI] [PubMed] [Google Scholar]
- Lowe MR, Miller-Kovach K, Phelan S. Weight-loss maintenance in overweight individuals one to five years following successful completion of a commercial weight loss program. Int J Obes Relat Metab Disord. 2001;25:325–331. doi: 10.1038/sj.ijo.0801521. [DOI] [PubMed] [Google Scholar]
- Cooper Z, Doll HA, Hawker DM, Byrne S, Bonner G, Eeley E, et al. Testing a new cognitive behavioural treatment for obesity: a randomized controlled trial with three-year follow-up. Beh Res Ther. 2010;48:706–713. doi: 10.1016/j.brat.2010.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Appel LJ, Clark JM, Yeh HC, Wang NY, Coughlin JW, Daumit G, et al. Comparative effectiveness of weight-loss interventions in clinical practice. N Engl J Med. 2011;365:1959–1968. doi: 10.1056/NEJMoa1108660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wadden TA, Volger S, Sarwer DB, Vetter ML, Tsai AG, Berkowitz RI, et al. A two-year randomized trial of obesity treatment in primary care practice. N Engl J Med. 2011;365:1969–1979. doi: 10.1056/NEJMoa1109220. [DOI] [PMC free article] [PubMed] [Google Scholar]