Abstract
Background
Cystic fibrosis (CF) is an autosomal recessive genetic disease that affects approximately 30,000 people in the United States. Mucus in CF patients can be exceptionally viscous, leading to progressive cycles of inflammation and infection. The most widely accepted staging system used to score sinus computed tomography (CT) scans is the Lund-Mackay Score (LMS).
Methods
To determine if a significant correlation exists between LMS and the need for revision sinus surgery in a patient population with CF, we performed a retrospective review of 32 patients with CF who were referred to the Tulane Otolaryngology Clinic from 2005 to 2011 and received a CT scan of the paranasal sinuses. CT scans were graded in a blinded manner by the institution's neuroradiologist using the LMS system.
Results
We found no statistically significant difference in the raw or scaled LMSs between patients receiving revision surgery (n=9) and patients receiving a single surgery (n=23).
Conclusions
CT scans are vital for preoperative planning, but they are not a useful tool for risk stratification. More specifically, application of the LMS is not relevant in identifying which CF patients with chronic rhinosinusitis will be at risk for revision surgeries.
Keywords: Cystic fibrosis, paranasal sinuses, surgical procedures–operative, tomography–x-ray computed
INTRODUCTION
Cystic fibrosis (CF) is an autosomal recessive genetic disease that affects approximately 30,000 people in the United States.1 CF is caused by a mutation in the cystic fibrosis transmembrane conductance regulator (CFTR) glycoprotein gene that codes for a cyclic adenosine monophosphate-mediated chloride channel regulating exocrine secretion viscosity. As a result, mucus in CF patients is exceptionally viscous, making clearance by respiratory epithelium more challenging. The resulting mucus stasis leads to progressive cycles of inflammation and infection. Recurrent pneumonias are a hallmark of CF and lead to respiratory failure, but CF also affects the upper airway, specifically the nose and paranasal sinuses.2
Chronic rhinosinusitis (CRS) is almost pervasive in CF patients, and paranasal sinus disease has a radiographic prevalence on computed tomography (CT) scans approaching 100%.3 The sinus CT scan has long been considered the gold standard for evaluating the extent of sinus disease, as well as for surveying the sinonasal anatomy prior to any planned surgical intervention.
The most widely accepted staging system used to score sinus CT scans is the Lund-Mackay Score (LMS). Although this staging system was designed for and has been successfully used to guide optimal therapeutic interventions in patients with CRS but without CF, it has also been applied to the CF patient population. This study aimed to determine if a significant correlation exists between LMS and the need for revision surgery in the CF patient population as demonstrated by experience at 1 institution.
METHODS
This retrospective cohort study was approved by the Tulane University Institutional Review Board, and all data were handled in accordance with Health Insurance Portability and Accountability Act regulations. Patients with a diagnosis of CF who were surgically treated in the Otolaryngology Clinic at Tulane University since 2005 and who received a CT scan of the paranasal sinuses were included. Each CT scan was obtained preoperatively, and only the CT scan preceding the first operation was considered in revision cases.
CT scans were graded in a blinded manner by the institution's neuroradiologist using the LMS system. The LMS scale is 0 (no opacification), 1 (partial opacification), and 2 (complete opacification), while the ostiomeatal complex score is 0 (not occluded) or 2 (occluded). Each sinus is staged and scored separately. Additionally, each sinus was evaluated by the neuroradiologist and graded as normal, hypoplastic, or absent based on age-appropriate norms. Those sinuses that were undeveloped were assigned a null value. The sinus scores were summed, and the combined score was scaled up to range from 0 to 24 by the factor 24/n, where n represents the maximum potential LMS based on the number of sinuses pneumatized.4-6 Statistical analysis was undertaken utilizing the Mann-Whitney test, and results with corresponding P values <0.05 were considered statistically significant.
RESULTS
Thirty-two patients met inclusion criteria. Genotype was not available for 8 patients, 13 patients were ΔF508 homozygotes, and 11 patients were ΔF508 heterozygotes. Average age at time of surgery was 13.8 years, and average time between surgeries for patients with multiple surgeries was 15.4 months. Twenty-three patients underwent a single surgery and 9 patients required revision surgery.
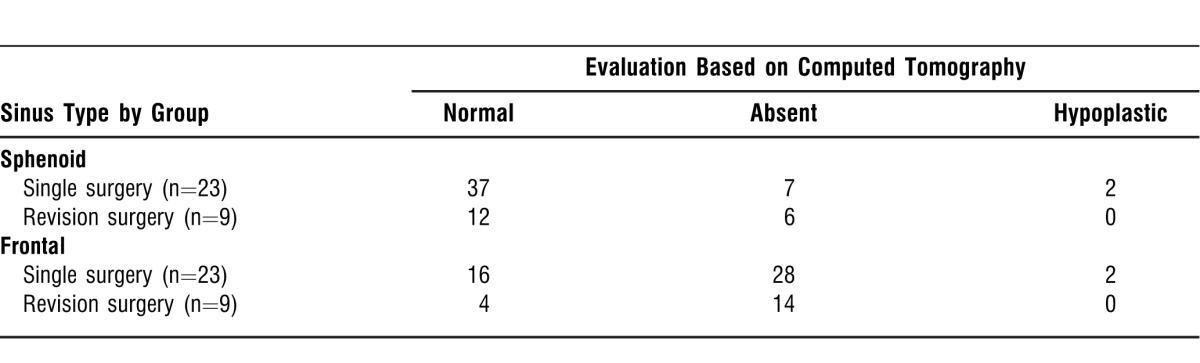
Of all patients, 21 had an absent frontal sinus (66%) and 1 (3%) had a hypoplastic sinus. Regarding the sphenoid sinus, 5 patients (16%) had an absent sinus and 1 patient (3%) had a hypoplastic sinus. The 23 patients in the single surgery group had 28 absent, 2 hypoplastic, and 16 appropriately sized frontal sinuses. The 9 patients in the revision surgery group had 14 absent, 0 hypoplastic, and 4 appropriately sized frontal sinuses. The single surgery group had 7 absent, 2 hypoplastic, and 37 appropriately sized sphenoid sinuses compared to 6 absent, 0 hypoplastic, and 12 appropriately sized sphenoid sinuses in the revision surgery group (Table 1).
Table 1.
Radiographic Evidence of Sphenoid and Frontal Sinus
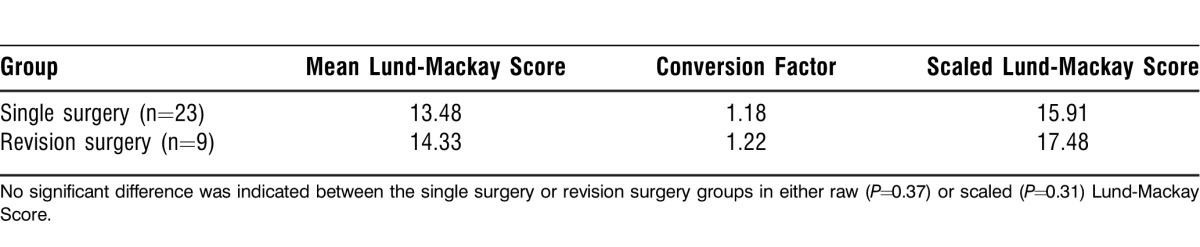
No statistically significant difference in raw LMS was demonstrated between the revision surgery (mean 14.33) and single surgery groups (mean 13.48) (P=0.37). The raw LMS was then scaled to take into account sinus hypoplasia and/or absence, which is common in the CF patient population. A conversion factor of 1.22 was applied to the 9 revision patients (28%), and a conversion factor of 1.18 was applied to the 23 single surgery patients (72%). No significant difference was found between the average LMS conversion factors (P=0.37). Utilizing the Mann-Whitney test, we found no statistically significant difference in the scaled LMS between the revision surgery (mean 17.48) and single surgery (mean 15.91) groups (P=0.31) (Table 2).
Table 2.
Lund-Mackay Scores
DISCUSSION
As a result of advances in treatment, the median survival period for CF patients exceeds 35 years,7 and 25%8,9 of CF patients will ultimately undergo functional endoscopic sinus surgery (FESS) for treatment of their sinonasal disease after failing maximal medical therapy. Because of the increasing lifespan and the prevalence of sinonasal disease in this patient population, clinicians must understand which patients have particularly refractory disease and will be at risk for revision surgeries.
The LMS system was developed to quantify the amount of inflammation present in the sinus mucosa and to act as an inclusion criterion for research studies.10 The score is not meant to be used as a cutoff point for surgery, but rather as a tool that may be paired with physical examination findings and the patient's symptom severity to make treatment decisions. However, this tool has not been proven to have real predictive value for assessing overall disease severity and prognosis. For CF patients with CRS, the revision rate after initial FESS is highly variable (13%-89%).11 We find it helpful to be able to counsel these patients preoperatively about their chances for a successful outcome with FESS and their individual risks for revision surgery. The LMS system has been correlated with the need for revision surgery in CRS patients,10 but this distinction is less clear in CF patients.
McMurphy et al demonstrated that LMS was not a useful method for assessing surgical success, as preoperative and postoperative scores were not significantly different.12 However, they did not compare the LMSs of patients who underwent revision surgery to the scores of those who required a single sinus surgery. Similarly, Rowe-Jones and Mackay looked at 46 patients and found no correlation between LMS and revision surgery rate.13 Our study differs in that the raw LMS was scaled to account for hypoplastic and/or absent frontal and sphenoid sinuses; this scaling allows for greater equity when comparing imaging between patients with varying degrees of sinus development.4-6
One study in the literature—from Becker et al—does indicate a significant relationship between LMS and an increased number of surgeries in a CF population with CRS.11 Additionally, when LMSs were scaled to account for absent or hypoplastic sinuses, the results remained statistically significant. Despite using similar methodology, we found no statistical difference in our cohort.
The best indicator of which CF patients might require revision surgery remains clinical manifestations of their sinonasal disease. Rowe-Jones and Mackay demonstrated that nasal polyposis was a risk factor for revision surgery compared to patients presenting with mucopurulent rhinorrhea.13 Rickert et al recently examined a group of 49 CF patients who underwent endoscopic sinus surgery and found that a higher preoperative grade of nasal polyposis was associated with revision surgery.8 No patient without polyps required reoperation, while 58% of patients with extensive polyposis required revision surgery. Nasal polyposis is a disease that is prone to return. Thus, patients with more severe preoperative clinical nasal polyposis are more likely to have recurrent disease requiring revision surgery. The LMS does not reflect the difference between opacification secondary to polyps vs mucopurulence. This lack of differentiation largely explains why higher LMSs do not correlate with patients who are at increased risk for surgical revision.
CONCLUSION
CT is vital for preoperative planning but is not a useful tool for risk stratification of patients with sinus disease. More specifically, application of the LMS is not relevant in identifying which CF patients with CRS will be at risk for revision surgeries.
Footnotes
This paper was presented at the Combined Otolaryngology Spring Meeting, Chicago, IL, April 28, 2011.
The authors have no financial or proprietary interest in the subject matter of this article.
This article meets the Accreditation Council for Graduate Medical Education and the American Board of Medical Specialties Maintenance of Certification competencies for Patient Care, Medical Knowledge, Systems-Based Practice, and Practice-Based Learning and Improvement.
REFERENCES
- 1.Cystic Fibrosis Foundation. Patient Registry 2007 Annual Report. http://www.cff.org/research/ClinicalResearch/PatientRegistryReport. Accessed January 11, 2010. [Google Scholar]
- 2.Tandon R, Derkay C. Contemporary management of rhinosinusitis and cystic fibrosis. Curr Opin Otolaryngol Head Neck Surg. 2003 Feb;11(1):41–44. doi: 10.1097/00020840-200302000-00009. [DOI] [PubMed] [Google Scholar]
- 3.Eggesbø HB, Søvik S, Dølvik S, Kolmannskog F. CT characterization of inflammatory paranasal sinus disease in cystic fibrosis. Acta Radiol. 2002 Jan;43(1):21–28. doi: 10.1080/028418502127347592. [DOI] [PubMed] [Google Scholar]
- 4.Ashraf N, Bhattacharyya N. Determination of the “incidental” Lund score for the staging of chronic rhinosinusitis. Otolaryngol Head Surg. 2001 Nov;125(5):483–486. doi: 10.1067/mhn.2001.119324. [DOI] [PubMed] [Google Scholar]
- 5.Hill M, Bhattacharyya N, Hall TR, Lufkin R, Shapiro NL. Incidental paranasal sinus imaging abnormalities and the normal Lund score in children. Otolaryngol Head Neck Surg. 2004 Feb;130(2):171–175. doi: 10.1016/j.otohns.2003.11.006. [DOI] [PubMed] [Google Scholar]
- 6.Lund VJ, Kennedy DW. Staging for rhinosinusitis. Otolaryngol Head Neck Surg. 1997 Sep;117((3 Pt 2)):S35–S40. doi: 10.1016/S0194-59989770005-6. [DOI] [PubMed] [Google Scholar]
- 7.Boyle MP. Adult cystic fibrosis. JAMA. 2007 Oct 17;298(15):1787–1793. doi: 10.1001/jama.298.15.1787. [DOI] [PubMed] [Google Scholar]
- 8.Rickert S, Banuchi VE, Germana JD, Stewart MG, April MM. Cystic fibrosis and endoscopic sinus surgery: Relationship between nasal polyposis and likelihood of revision endoscopic sinus surgery in patients with cystic fibrosis. Arch Otolaryngol Head Neck Surg. 2010 Oct;136(10):988–992. doi: 10.1001/archoto.2010.162. [DOI] [PubMed] [Google Scholar]
- 9.Jorissen MB, De Boeck K, Cuppens H. Genotype-phenotype correlations for the paranasal sinuses in cystic fibrosis. Am J Respir Crit Care Med. 1999 May;159((5 Pt 1)):1412–1416. doi: 10.1164/ajrccm.159.5.9712056. [DOI] [PubMed] [Google Scholar]
- 10.Hopkins C, Browne JP, Slack R, Lund V, Brown P. The Lund-Mackay staging system for chronic rhinosinusitis: how is it used and what does it predict? Otolaryngol Head Neck Surg. 2007 Oct;137(4):555–561. doi: 10.1016/j.otohns.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 11.Becker SS, de Alarcon A, Bomeli SR, Han JK, Gross CW. Risk factors for recurrent sinus surgery in cystic fibrosis: review of a decade of experience. Am J Rhinol. 2007 Jul-Aug;21(4):478–482. doi: 10.2500/ajr.2007.21.3056. [DOI] [PubMed] [Google Scholar]
- 12.McMurphy AB, Moriss C, Roberts DB, Friedman EM. The usefulness of computed tomography scans in cystic fibrosis patients with chronic sinusitis. Am J Rhinol Allergy. 2007 Nov-Dec;21(6):706–710. doi: 10.2500/ajr.2007.21.3104. [DOI] [PubMed] [Google Scholar]
- 13.Rowe-Jones JM, Mackay IS. Endoscopic sinus surgery in the treatment of cystic fibrosis with nasal polyposis. Laryngoscope. 1996 Dec;106((12 Pt 1)):1540–1544. doi: 10.1097/00005537-199612000-00019. [DOI] [PubMed] [Google Scholar]


