Abstract
Background:
The aim of this study was to evaluate the response of common sized fiber-reinforced composites (FRCs) to different deflections due to bending forces and comparing it with stainless steel (SS) wires.
Materials and Methods:
In this experimental study, two FRC groups with 0.75 mm and 1.2 mm diameters (Everstick Ortho, Stick Tech, Finland) and three SS groups with 0.016 × 0.022 inch, 0.0215 × 0.028 inch and 0.7 mm diameters (3M Uniteck, Monrovia, California, USA) were tested. Each group contained 10 samples that were tested according to a three point bending test. Each group was tested at deflections of 0.5, 1 and 1.5 mm and the data was analyzed using the repeated measure ANOVA by SPSS software (Statistical Package for the Social Sciences, IBM SPSS, Inc. in Chicago, Illinois, USA). P < 0.05 was considered as significant.
Results:
The highest recorded load belonged to the 1.2 mm FRC and after that 0.7 mm SS wire, 0.75 mm FRC, 0.0215 × 0.028 inch SS wire and finally 0.016 × 0.022 inch SS wire. The 0.7 mm SS wire and 0.75 mm FRC were compared as retainers and the results showed the 0.7 mm SS wire showed significantly higher load compared with 0.75 mm FRC (P < 0.05). The 1.2 mm FRC had significantly higher load compared to 0.0215 × 0.028 inch and 0.016 × 0.022 inch SS wires (P < 0.05).
Conclusion:
The results showed that the 1.2 mm FRC group had significantly higher load compared to SS wires and other FRC groups under the 0.5, 1 and 1.5 mm deflections. Therefore, it can be suggested that FRC can be used as an esthetic replacement for SS wires for active and passive purposes in orthodontics.
Keywords: Fiber-reinforced composite, load-deflection, stainless steel wire
INTRODUCTION
Fiber-reinforcement was first introduced in dental articles in the early 1960s and has become an alternative treatment in esthetic and metal free dentistry.[1] Fiber-reinforced composites (FRCs) that incorporates long fibers such as glass or carbon are a new generation of materials with similar features to metals. To optimize the mechanical properties, fibers are wetted, oriented and the plastic matrix added under controlled manufacturing conditions. Wires or strips that are impregnated by the matrix and are unpolymerized are called “prepregs.”[2] Plasma treated polyethylene fibers are embedded inside the plastic composite resin matrix to reinforce the material features.[3] Reinforcing the properties of FRCs is affected by the type and quantity of the fibers, impregnation by the resin matrix, fiber adhesion to the matrix and fiber orientation. Theoretically, unidirectional fibers reinforce the composite 100% in one direction (anisotropic mechanical features), whereas the fiber nets need to be oriented 25-50% in two directions to reinforce the composite.[4] Overall, fiber reinforcement produces a composite structure with better biomechanical features which result in excellent tension and flexure properties.[5] FRCs are widely used in dentistry for periodontal tooth splinting,[6] post-traumatic splint,[7] fixed partial dentures[8] and post and cores.[9] Recently, FRCs have been used as implant materials in dental, orthopedic and craniofacial surgeries.[10] FRCs are used in orthodontics for forced eruption,[11] bimaxillary protrusion treatment[12] and space maintainers.[13] FRCs can also be used for orthodontic retention and can replace removable and lingual bonded wire retainer due to their esthetics, ease of use and no need for patient care.[2] Burstone and Kuhlberg introduced a new clinical application for FRC, which was connecting the teeth to form anchorage or active tooth movement units and the attachments such as brackets, hooks or tubes could be bonded to the FRC directly.[14] Freudenthaler et al.[15] and Meiers et al.[16] showed that attachment bonding to FRC is great and FRC -enamel bond strength is good. Therefore, a FRC bar or connector can be used in: (a) retention, (b) anchorage and (c) active tooth movement.[15] The major clinical application of FRC is an active appliance for teeth movement, which long-continuous fiber composites replace common stainless steel (SS) wires.[14] In orthodontics, optimizing the fiber-matrix ratio can produce FRC wires with a wide range of elastic stiffness.[17] Cacciafesta et al. carried out a study, which resulted that in patients with esthetical considerations or allergy to common wires or brackets of orthodontics, FRC can be considered as an effective alternative.[18] FRCs should have a significant clinical improvement compared with non-reinforced resins to be considered as an alternative dental material.[19] Before recommending FRC for special orthodontic appliances, their mechanical and physical properties should be evaluated.[18]
Biocompatibility is a clinical advantage of FRC because it doesn’t contain nickel; therefore it can be used in nickel-allergic patients. Esthetics is another advantage, which is due to the translucency of the fibers. Some other advantages include ease of use and reduced need of bonded attachments and wires.[3] The polyethylene fiber materials easily adapt to the dental contours and can be manipulated during bonding. FRC has an acceptable strength due to fiber-composite integration which leads to good clinical longevity.[20] A material with high flexural strength, high elastic modulus, high fatigue strength and low deformation is needed in high-stress areas (like anchorage areas).[21] Burstone and Kuhlberg[14] showed that FRC has high flexural modulus, high flexural strength, high fracture strength and yield strength. The elastic modulus in flexure of Splint-It (Long FRC) is 70% higher than dental composites. FRC has high stiffness/weight (specific modulus) and high strength/weight (specific strength) compared with other materials, therefore can be successfully used.[22] Soares et al. have mentioned the typical features of FRC such as high strength-weight and modulus-weight, high fatigue strength and fatigue damage tolerance and anisotropic features.[23] Some other properties are non-susceptibility to corrosion, translucency, radiolucency, good bonding strength and easy repair.[24] Patients in need of partial or compromised treatment are good candidates for FRC appliances.[14] In addition to using FRC for anchorage or active tooth movement, they can also be used for post treatment retention. Sectional SS wires are commonly used as fixed retainers in the anterior lingual segment. These wires have a high stiffness, which can delay the teeth reorientation and stabilization after treatment.[25] Reinforced fiber materials have been successfully used as orthodontic retainers.[3]
Regarding the use of FRC for retention and splinting of the teeth to create anchorage or active tooth movement units, the load-deflection features of FRCs should be evaluated. The purpose of this study was to evaluate the response of normal size FRCs to different deflections caused by bending forces and comparing it with SS wires.
MATERIALS AND METHODS
In this laboratory study, three groups of straight SS wires with 0.016 × 0.022 inch, 0.0215 × 0.028 inch and 0.7 mm diameters (3 M Uniteck, Monrovia, California, USA) were tested. Each group had 10 samples. The wires were cut into 30 mm segments. The FRC had two groups of 10 samples with 0.75 mm and 1.2 mm diameters (Everstick Ortho, Stick Tech, Finland). The FRC samples were also cut into 30 mm segments. The FRCs were prepared according to manufacturing guidelines and then cured for 40 s with a halogen curing device (Dr's Light, South Korea) with 420-490 nm wavelength and 1600 mW/cm² light intensity.
Then, all FRC and SS samples underwent a three point bending test. A special fixture was designed for this test [Figure 1]. The fixture was made of two brass supports, which according to Nakano et al.[26] had a 14 mm distance (the mean distance between the labial center of a mandibular lateral incisor and mandibular first premolar). Thus, creating a 7 mm interpoint distance. Each samples was placed directly on the supports so that the center of each sample was on the center of the inter support distance. The load was applied using an Electromechanical Universal testing machine (Walter + bai company, Löhningen, Switzerland) with a crosshead speed of 1 mm/min to the center of each sample. The maximum deflection for each sample was 1.5 mm. The bending load values were recorded at 0.2 mm intervals by DION Pro+ software (Walter + bai company, Löhningen, Switzerland). The bending load values at by 0.5, 1 and 1.5 mm deflections were recorded in different groups. Data was analyzed using SPSS software (version 19) (Statistical Package for the Social Sciences, IBM SPSS, Inc. in Chicago, Illinois, USA) by the repeated measure ANOVA test. Significance was predetermined at P < 0.05.
Figure 1.

Universal testing machine
RESULTS
Table 1 show the maximum load recorded in the study groups in different deflections. It also shows the minimum, mean, standard deviations of the maximum load of different sizes of FRC and SS wires.
Table 1.
Descriptive data of load values in different sizes of FRC and stainless steel wires under 0.5, 1 and 1.5 mm deflections
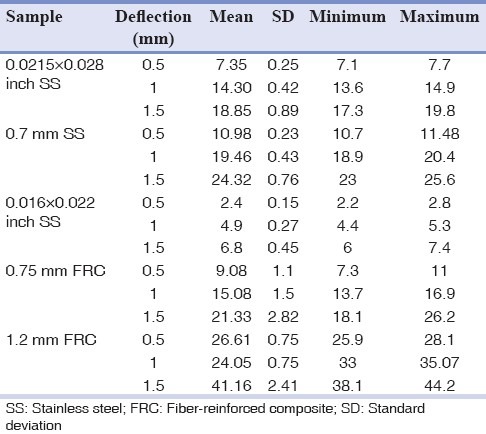
The highest load belonged to 1.2 mm FRC and after that 0.7 mm SS wire, 0.75 mm FRC, 0.0215 × 0.028 inch SS wire and 0.016 × 0.022 inch SS wire. Comparing the 0.7 mm SS wire and 0.75 mm FRC, which are used as retainers in clinic, the SS wire showed significantly higher maximum load in 0.5, 1 and 1.5 mm deflections than the FRC (P < 0.05).
In the role of an active tooth movement or anchorage unit, 1.2 mm FRC was compared with 0.0215 × 0.028 inch and 0.016 × 0.022 inch SS wires. The 1.2 mm FRC showed significantly higher load at the tested deflections (P < 0.05).
Analysis showed that the highest maximum loads were observed in 1.5 mm deflections (P < 0.05).
Comparing all the SS wires with each other and all the FRCs with each other and with SS wires showed significant difference (P < 0.05).
DISCUSSION
FRCs are regarded as the last great frontier of orthodontic materials. Due to their esthetics and strength and the ability to customize their properties according to the orthodontist's needs, it can be expected that FRCs replace metals in orthodontics just like the replacement of Aluminum by composites in the aircraft industry. No doubt, FRCs promise exciting new abilities in biomechanics and might revolutionize the practice of orthodontics.[17]
The fibers in this study were round section, unidirectional E-glass embedded in poly methyl metacrylate and Bis-GMA. E-glass fiber is made of alumino-borosilicate glass with less than 1 wt% alkali oxides.[5] These fibers were oriented correctly inside the composite and after polymerization formed a great coupling with the matrix. Freudenthaler et al.[15] reported that the initial polymerization makes the matrix modifiable so it can easily adapt to the tooth contour and the final curing stabilizes the final form and generates favorable mechanical features. Recently, the introduction of pre-impregnated commercial fiber has increased their desire for clinical application.[27]
In this study 1.2 mm FRC had significantly higher load compared with 0.75 mm FRC in different deflections. Cacciafesta et al.[22] reported that 1.2 mm FRC had a higher load value than 0.6 mm FRC. Similar results are reported by Cacciafesta et al.[18] on FRCs and SS wires, Vallittu[28] on wrought-steel wire and Park[29] on FRCs. The highest load in different deflections belonged the 1.2 mm FRC and after that 0.7 mm SS wire, while the lowest strength belonged to 0.016 × 0.022 inch SS wire.
The load values of FRC in different deflections suggest that reinforcement of polymers with long, continuous fibers is effective for many applications.[18] Therefore, it can be used as an esthetic alternative for SS wires, which can splint the teeth as a rigid unit and be used for active or passive purposes in orthodontics.[30] This finding agrees with previous studies evaluating the bond strength[15] and clinical applications of FRCs.[14,30]
Favorable features such as high stiffness/weight and strength/weight,[22] good bonding strength, easy repair, no corrosion[24] and high biocompatibility, ease of use, decreased need for bonded attachments and wire,[3] easy adaptation to tooth contours,[20] high flexural strength and elastic modulus, low deformation and high fatigue strength makes FRCs appropriate for areas in need of maximum anchorage.[21] However, to date FRCs have higher costs than SS orthodontic wires.[18]
In this study, higher deflections on FRCs and SS wires resulted in higher load values. The same results were observed in the studies of Taneja et al.[31] on multistrand SS wires, Gurgel et al.[32] on beta-titanium wires, Wilkinson et al.[33] on nickel titanium wires and Cacciafesta et al.[18] on FRCs and SS wires.
Retention is a stage of orthodontic treatment, which maintains the teeth in their new corrected positions.[8] Orthodontic achievements are potentially unstable, and retention is needed with a fixed retainer. The major indications for a fixed retainer are: Maintaining the mandibular incisors position during late growth, maintaining space closures, either after extractions or after the closure of diastemas and maintaining the space where it will be filled by prosthetic restoration.[3]
An excellent retainer for holding of the mandibular incisors is a fixed lingual bar bonded only to the canines (or to canines and first premolars). Severe rotations before treatment, when derotated, need to be retained with a multi-strand wire retainer.[34] However, new material such as FRCs should be compared with this standard procedures and their reliability proved in vitro and in vivo. Glass fibers are translucent, therefore even if bonded on the labial side is difficult to notice, so they can replace lingual retainers.[14]
There are several reasons for FRC retainer failure. It is best that teeth not be retained very rigidly.[3] Bearn[35] reported that reinforced fibers have the disadvantage of rigid splint, which limit the physiologic movement of teeth and lead to higher clinical failure rate. However, Bolla et al.[36] reported that the use of glass fiber reinforced (GFR) retainers as a retention strategy should not be discouraged and could be considered as a viable esthetic alternative to SS wire retainers.
In this study, the 0.75 mm FRC was compared with 0.7 mm SS wire as retainers. The 0.7 mm SS wire showed significantly higher load in different deflections (P < 0.05). Tacken et al.[37] demonstrated significantly lower success rates for GFR retainers compared with SS retainers. Similar finding have been described for ribbon-reinforced retainers when compared with SS retainers.[3] Clinically, a canine to canine fixed retainer prevents from lingual movement of the incisors and is also reasonably effective in maintaining correction of rotations in the incisor area. This retainer is made of a heavy wire to resist distortion induced by large inter-canine distance.[34] The reliability of any retainer is limited by the care taken during processing, production, handling and bonding, regardless of the material applied.
CONCLUSION
1.2 mm FRC showed significantly higher load than 0.75 mm FRC in 0.5, 1 and 1.5 mm deflections (P < 0.05).
In 0.5, 1 and 1.5 mm deflections, the highest load belonged to 1.2 mm FRC and after that 0.7 mm SS wire, 0.75 mm FRC, 0.0215 × 0.028 inch SS wire and 0.016 × 0.022 inch SS wire.
In the role of retainers, 0.7 mm SS wire showed significantly higher maximum load compared with 0.75 mm FRC in 0.5, 1 and 1.5 mm deflections (P < 0.05).
FRC can be used as an esthetic replacement for SS wires, which can splint the teeth as a rigid unit and be used for active and passive purpose in orthodontics.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Raju PS, Gupta A, Grag J, Bhattacharya P, Agarwal A. Evaluation of the shear bond strength of fiber reinforced composite using different adhesive systems. J Dr NTR Univ Health Sci. 2012;1:249–52. [Google Scholar]
- 2.Graber LW, Vanarsdall RL, Vig KW. 5th ed. USA: Mosby Co; 2012. Orthodontics Current Principles and Techniques; p. 376. [Google Scholar]
- 3.Rose E, Frucht S, Jonas IE. Clinical comparison of a multistranded wire and a direct-bonded polyethylene ribbon-reinforced resin composite used for lingual retention. Quintessence Int. 2002;33:579–83. [PubMed] [Google Scholar]
- 4.Antonopoulou A, Papadopoulos T, Hatzikyriakos A. In vitro evaluation of shear bond strength and mode of failure of the interface between an indirect composite bonded to fiber-reinforced composite substructures. J Prosthodont. 2012;21:451–9. doi: 10.1111/j.1532-849X.2012.00851.x. [DOI] [PubMed] [Google Scholar]
- 5.Zhang M, Matinlinna JP. E-glass fiber-reinforced composites in dental applications. Silicon. 2012;4:73–8. [Google Scholar]
- 6.Strassler HE, Serio CL. Esthetic considerations when splinting with fiber-reinforced composites. Dent Clin North Am. 2007;51:507–24. doi: 10.1016/j.cden.2006.12.004. [DOI] [PubMed] [Google Scholar]
- 7.Strassler HE. Aesthetic management of traumatized anterior teeth. Dent Clin North Am. 1995;39:353–66. [PubMed] [Google Scholar]
- 8.Kumbuloglu O, Saracoglu A, Cura C, User A. Bonded orthodontic retainer and fixed partial denture made with fiber reinforced composite resin. Eur J Dent. 2011;5:237–40. [PMC free article] [PubMed] [Google Scholar]
- 9.Kathuria A, Kavitha M, Khetarpal S. Ex vivo fracture resistance of endodontically treated maxillary central incisors restored with fiber-reinforced composite posts and experimental dentin posts. J Conserv Dent. 2011;14:401–5. doi: 10.4103/0972-0707.87211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Abdulmajeed AA, Närhi TO, Vallittu PK, Lassila LV. The effect of high fiber fraction on some mechanical properties of unidirectional glass fiber-reinforced composite. Dent Mater. 2011;27:313–21. doi: 10.1016/j.dental.2010.11.007. [DOI] [PubMed] [Google Scholar]
- 11.Oshagh M, Sadeghi AR, Sharafeddin F, Alavi AA, Amid R, Derafshi R. Forced eruption by fiber-reinforced composite. Dent Today. 2009;28:66. 68, 70-1. [PubMed] [Google Scholar]
- 12.Uribe F, Nanda R. Treatment of bimaxillary protrusion using fiber-reinforced composite. J Clin Orthod. 2007;41:27–32. [PubMed] [Google Scholar]
- 13.Nidhi C, Jain RL, Neeraj M, Harsimrat K, Samriti B, Anuj C. Evaluation of the clinical efficacy of glass fiber reinforced composite resin as a space maintainer and its comparison with the conventional band and loop space maintainer. An in vivo study. Minerva Stomatol. 2012;61:21–30. [PubMed] [Google Scholar]
- 14.Burstone CJ, Kuhlberg AJ. Fiber-reinforced composite in orthodontics. J Clin Orthod. 2000;34:271–9. [Google Scholar]
- 15.Freudenthaler JW, Tischler GK, Burstone CJ. Bond strength of fiber-reinforced composite bars for orthodontic attachment. Am J Orthod Dentofacial Orthop. 2001;120:648–53. doi: 10.1067/mod.2001.118779. [DOI] [PubMed] [Google Scholar]
- 16.Meiers JC, Kazemi RB, Donadio M. The influence of fiber reinforcement of composites on shear bond strengths to enamel. J Prosthet Dent. 2003;89:388–93. doi: 10.1067/mpr.2003.87. [DOI] [PubMed] [Google Scholar]
- 17.Valiathan A, Dhar S. Fiber-reinforced composite archwires in orthodontics: Function meets esthetics. Trends Biomater Artif Organs. 2006;20:16–9. [Google Scholar]
- 18.Cacciafesta V, Sfondrini MF, Lena A, Scribante A, Vallittu PK, Lassila LV. Force levels of fiber-reinforced composites and orthodontic stainless steel wires: A 3-point bending test. Am J Orthod Dentofacial Orthop. 2008;133:410–3. doi: 10.1016/j.ajodo.2006.01.047. [DOI] [PubMed] [Google Scholar]
- 19.Goldberg AJ, Burstone CJ. The use of continuous fiber reinforcement in dentistry. Dent Mater. 1992;8:197–202. doi: 10.1016/0109-5641(92)90083-o. [DOI] [PubMed] [Google Scholar]
- 20.Karaman AI, Kir N, Belli S. Four applications of reinforced polyethylene fiber material in orthodontic practice. Am J Orthod Dentofacial Orthop. 2002;121:650–4. doi: 10.1067/mod.2002.123818. [DOI] [PubMed] [Google Scholar]
- 21.van Heumen CC, Kreulen CM, Bronkhorst EM, Lesaffre E, Creugers NH. Fiber-reinforced dental composites in beam testing. Dent Mater. 2008;24:1435–43. doi: 10.1016/j.dental.2008.06.006. [DOI] [PubMed] [Google Scholar]
- 22.Cacciafesta V, Sfondrini MF, Lena A, Scribante A, Vallittu PK, Lassila LV. Flexural strengths of fiber-reinforced composites polymerized with conventional light-curing and additional postcuring. Am J Orthod Dentofacial Orthop. 2007;132:524–7. doi: 10.1016/j.ajodo.2005.09.036. [DOI] [PubMed] [Google Scholar]
- 23.Soares CA, Soares CM, Freitas MJ. 3rd ed. Netherlands: Kluwer Academic Publishers; 1999. Mechanics of Composite Materials and Structures; pp. 1–79. [Google Scholar]
- 24.Freilich MA, Meiers JC, Duncan JP, Goldberg AJ. 4th ed. Chicago: Quintessence Publishing Co; 2000. Fiber-Reinforced Composite in Clinical Dentistry; p. 13. [Google Scholar]
- 25.Silvestrini-Biavati A, Angiero F, Gibelli F, Signore A, Benedicenti S. In vitro determination of the mechanical and chemical properties of a fibre orthodontic retainer. Eur J Orthod. 2012;34:693–7. doi: 10.1093/ejo/cjr083. [DOI] [PubMed] [Google Scholar]
- 26.Nakano H, Satoh K, Norris R, Jin T, Kamegai T, Ishikawa F, et al. Mechanical properties of several nickel-titanium alloy wires in three-point bending tests. Am J Orthod Dentofacial Orthop. 1999;115:390–5. doi: 10.1016/s0889-5406(99)70257-x. [DOI] [PubMed] [Google Scholar]
- 27.Freilich MA, Karmaker AC, Burstone CJ, Goldberg AJ. Development and clinical applications of a light-polymerized fiber-reinforced composite. J Prosthet Dent. 1998;80:311–8. doi: 10.1016/s0022-3913(98)70131-3. [DOI] [PubMed] [Google Scholar]
- 28.Vallittu PK. Fatigue resistance and stress of wrought-steel wire clasps. J Prosthodont. 1996;5:186–92. doi: 10.1111/j.1532-849x.1996.tb00295.x. [DOI] [PubMed] [Google Scholar]
- 29.Park SH. Comparison of degree of conversion for light-cured and additionally heat-cured composites. J Prosthet Dent. 1996;76:613–8. doi: 10.1016/s0022-3913(96)90439-4. [DOI] [PubMed] [Google Scholar]
- 30.Cacciafesta V, Sfondrini MF, Norcini A, Macchi A. Fiber-reinforced composites in lingual orthodontics. J Clin Orthod. 2005;39:710–4. [PubMed] [Google Scholar]
- 31.Taneja P, Duncanson MG, Jr, Khajotia SS, Nanda RS. Deactivation force-deflection behavior of multistranded stainless steel wires. Am J Orthod Dentofacial Orthop. 2003;124:61–8. doi: 10.1016/s0889-5406(03)00309-3. [DOI] [PubMed] [Google Scholar]
- 32.Gurgel JA, Pinzan-Vercelino CR, Powers JM. Mechanical properties of beta-titanium wires. Angle Orthod. 2011;81:478–83. doi: 10.2319/070510-379.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilkinson PD, Dysart PS, Hood JA, Herbison GP. Load-deflection characteristics of superelastic nickel-titanium orthodontic wires. Am J Orthod Dentofacial Orthop. 2002;121:483–95. doi: 10.1067/mod.2002.121819. [DOI] [PubMed] [Google Scholar]
- 34.Proffit WR, Fields HW, Sarver DM. 5th ed. Canada: Mosby Co; 2013. Contemporary Orthodontics; p. 626. [Google Scholar]
- 35.Bearn DR. Bonded orthodontic retainers: A review. Am J Orthod Dentofacial Orthop. 1995;108:207–13. doi: 10.1016/s0889-5406(95)70085-4. [DOI] [PubMed] [Google Scholar]
- 36.Bolla E, Cozzani M, Doldo T, Fontana M. Failure evaluation after a 6-year retention period: A comparison between glass fiber-reinforced (GFR) and multistranded bonded retainers. Int Orthod. 2012;10:16–28. doi: 10.1016/j.ortho.2011.12.005. [DOI] [PubMed] [Google Scholar]
- 37.Tacken MP, Cosyn J, De Wilde P, Aerts J, Govaerts E, Vannet BV. Glass fibre reinforced versus multistranded bonded orthodontic retainers: A 2 year prospective multi-centre study. Eur J Orthod. 2010;32:117–23. doi: 10.1093/ejo/cjp100. [DOI] [PubMed] [Google Scholar]


