Abstract
Background:
Management of canal isthmus is considered as an important factor for successful endodontic treatment. Accordingly, this study was designed to determine the prevalence, location, and types of isthmus in mesial root canals of extracted mandibular molars in a sample of Iranian population.
Materials and Methods:
In this cross-sectional descriptive study, 60 extracted molars with two mesial canals were included. The samples were initially decoronated and then, roots were sectioned horizontally at 2, 4, and 6 mm levels from the apex via a low-speed handpiece with a thin metallic disk and finally prepared and stained with Indian ink. All sections were examined using a stereomicroscope at a magnification of ×30. Prevalence, location, and types of isthmus were evaluated based on the classifications by Kim and Teixeira and all data were statistically analyzed by the chi-squared test. The statistical significance level was established at 0.05.
Results:
Eighty-three percent of extracted mandibular molars had an isthmus at the mesial root. This prevalence increased with distance from the apex, that is, 92% at 6 mm from the apex and 70% at 2 mm from the apex. A statistically significant difference was found between the sections at 2 and 6 mm from the apex (P < 0.05), but no other significant differences between other levels (P > 0.05).
Conclusion:
Isthmus is very common in the mesial roots of the mandibular permanent molars in the Iranian population, with the highest prevalence in the 6 mm distance from the root apex. Therefore, detection, cleaning, and filling of these apical 6 mm isthmuses are of great benefit in modern endodontics.
Keywords: Isthmus, mandibular molars, mesial root, root anatomy
INTRODUCTION
Root canal isthmus, a narrow ribbon-shaped communication between two root canals is an important anatomical feature because of the fact that it may contain pulp remnants, necrotic tissues, and micro-organisms and their byproducts.[1] An isthmus is also called a corridor, a lateral interconnection, and a transverse anastomosis.[2] The prevalence of isthmus varies according to the tooth type,[3] root levels,[4] and age.[5] An isthmus might be found in roots with C-shaped canals or in two adjacent canals such as mesial roots of mandibular molars, premolars, and so on.[1] The mesial root of the mandibular first molar exhibits the most number of isthmuses.[3,6] The majority of isthmuses have been reported in the apical 5 mm of root canals.[6,7] A study in a Chinese population reported that the prevalence of isthmuses decreases with age in molars due to the deposition of secondary dentin.[5]
Irregularities in root canal system, including isthmuses, are inaccessible spaces for instruments, irrigation solutions, and medicaments, and serve as reservoirs for bacteria, which finally leads to the failure of conventional root canal treatment.[8,9,10] In addition, isthmuses overlooked during periapical surgeries might lead to the failure of surgical treatment.[6] Ideally, with the present practice of advanced preparation and filling of isthmuses during root-end resection, the success rate of endodontic treatments is expected to increase in most cases.[3,11] Therefore, a thorough knowledge of this anatomic feature in the apical third of root canals in posterior teeth has a great value in increasing the success rate of surgical and nonsurgical endodontic treatments.
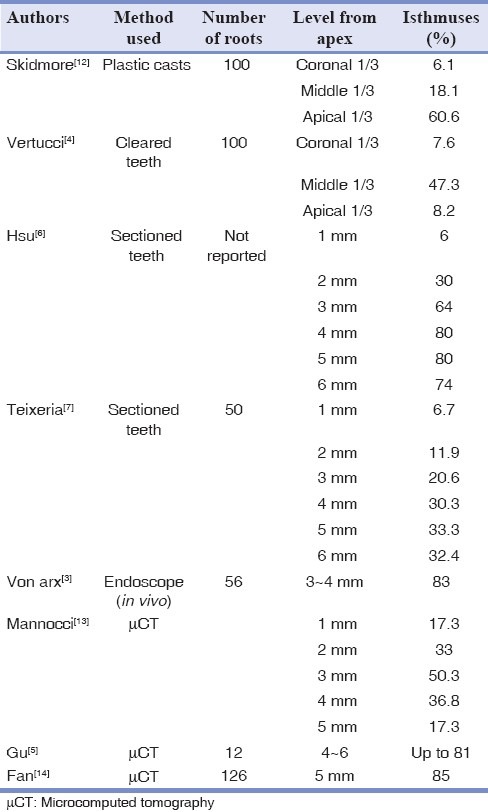
A large number of studies have been carried out in different parts of the world to determine the prevalence of isthmus in mandibular molars, ranging from 54 to 89% [Table 1].[3,4,5,6,7,12,13,14] Considering ethnical variations and inadequate published data on this anatomical feature, the aim of the present study was to evaluate the prevalence and location of isthmus in the mesial roots of extracted mandibular molars in an Iranian population.
Table 1.
Prevalence of isthmuses in the mesial roots of mandibular molars reported in previous studies
MATERIALS AND METHODS
In this cross-sectional descriptive study, 60 extracted mandibular first and second molars were randomly selected from dental clinics of Tehran (from the north, south, east, and west regions). The teeth were rinsed under tap water immediately after extraction and immersed in 10% neutral buffered formalin solution and prepared for two-angle radiographic examination (straight and 20° mesially). The inclusion criteria consisted of mature roots, the presence of two canals in the mesial root, absence of any calcification, internal or external root resorption, and visible cracks. The age, gender, and race of the patients were not considered.
All teeth were decoronated and two #15 K-Flexofiles (Dentsply/Maillefer, Ballaigues, Switzerland) were used to verify the two canals in the mesial roots of the teeth and a periapical X-ray was taken. A low-speed handpiece with a thin metallic disk (D and Z, Germany; length: 0.17 mm, breadth: 2.0 mm) was used to cut each root at 2, 4, and 6 mm distances from the apex perpendicular to the root long axis. Each separated root segment, which was 2 mm in thickness, was placed in 5.25% sodium hypochlorite solution for 24 hours to remove any debris or organic material remnants. Subsequently, the root samples were immersed in 17% ethylenediaminetetraacetic acid (EDTA; Ariadent, Asia Chemie Teb, Tehran, Iran) for 30 seconds, then rinsed with distilled water, and dried. Finally, the sectioned surfaces of the samples were stained with Indian ink and evaluated under a stereomicroscope (Nikon UFX-DX, Tokyo, Japan) at a magnification of ×30. Photographs were taken using a camera (Nikon FX-35 XX, Tokyo, Japan), and recorded and evaluated by two endodontists. The absence or presence of isthmuses and their types were evaluated and recorded based on the classifications of Kim[6] and Teixeira[7] at various distances from the apex. The Kim classification consists of five types [Figure 1]:
Figure 1.
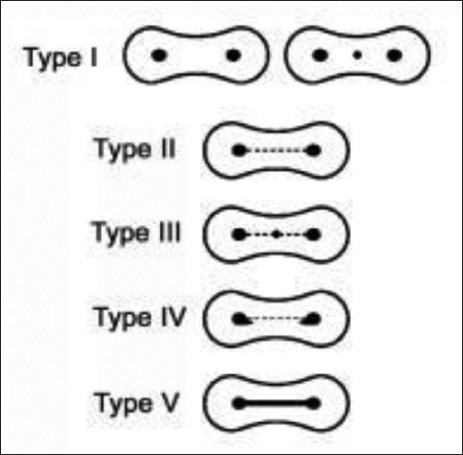
Schematic representation of isthmus classifications described by Hsu and Kim
Type I: Presence of two canals without a noticeable communication
Type II: Presence of two canals without a definite communication
Type III: Similar to type II but with three canals instead of two canals
Type IV: Extension of the main canal into the isthmus
Type V: Presence of a complete communication or corridor between the two canals
The Teixeira classification consists of no isthmus, incomplete isthmus, and complete isthmus.
A chi-squared test was used to determine the relationship between the prevalence and types of isthmuses with canal location after prevalence and confidence intervals were determined. The statistical significance level was established at 0.05.
RESULTS
The results are presented in [Tables 2 and 3] and based on the classifications of Kim and Teixeria. In the 60 mandibular first and second molars evaluated in the present study, isthmus was found in an average of 83% of the mesial roots at 2, 4, and 6 mm distances from the apex. The highest prevalence of isthmus was found at a distance of 6 mm from the apex with 92% [confidence interval (CI): 89.8-93.6]; the lowest prevalence was found at a distance of 2 mm from the apex with 70% (CI: 64.7-75.3). The prevalence of isthmus was 88% (CI: 85.7-90.92) at a distance of 4 mm from the apex.
Table 2.
Prevalence of isthmuses, based on the Kim classification, at 2, 4, and 6 mm distances from the apex in an Iranian population
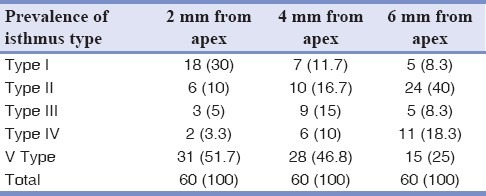
Table 3.
Prevalence of isthmuses, based on the Teixeira classification, at 2, 4, and 6 mm distances from the apex in an Iranian population
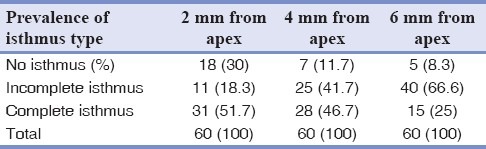
Based on the Kim classification [Figure 2], there was no significant relationship between isthmus type and canal location. The most prevalent isthmus at 2 and 4 mm from the apex was type V but at 6 mm, it was type II. However, in terms of the Teixeira classification [Figure 3], there was a significant relationship between sections at 2 and 6 mm from the apex (P = 0.039). Moreover, the incomplete type was most common in 6 mm (67%) and least in 2 mm (18.3%). Lack of isthmus was most common in 2 mm (18%) and least in 6 mm (5%). The complete type was most common in 2 mm (52%) and least in 6 mm (25%).
Figure 2.
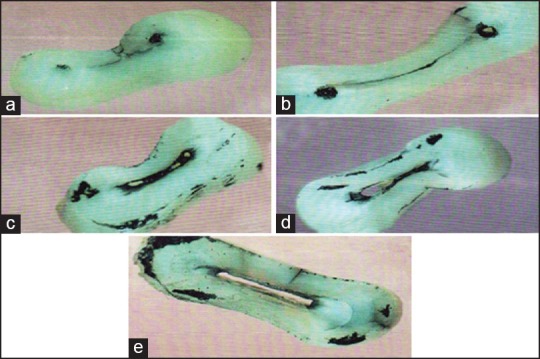
Isthmus classifications described by Hsu and Kim: Type I (a), type II (b), type III (c), type IV (d), type V (e)
Figure 3.
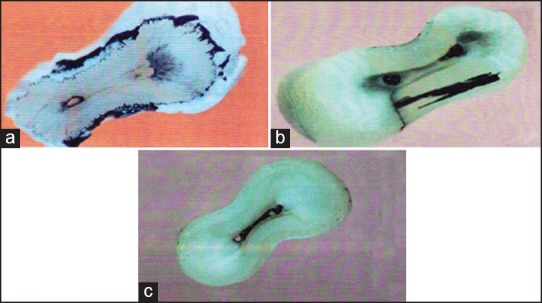
Teixeira classification: No isthmus (a), incomplete isthmus (b), and complete isthmus (c)
DISCUSSION
The management of root canal isthmus has been shown to be very essential in nonsurgical and surgical endodontic treatment.[13] Complete cleaning, shaping, and obturation of the apical third of root canals are considered as among the most important factors in achieving an excellent prognosis of root canal therapy. An unprepared isthmus in the root canal system, especially in the mandibular and maxillary molars, might contain necrotic debris and tissue remnants, which might serve as a reservoir for bacteria, leading to endodontic failure.[3,15] Therefore, initial anatomical knowledge, recognition, and proper management of an isthmus may be of great value to increase the success rate of surgical and nonsurgical endodontic treatments in posterior teeth.[16,17,18]
In the present study, isthmuses were found in 83% of the mesial roots of the mandibular first and second molars, which is consistent with the results of the studies by Fan et al.,[14] Gu et al.,[5] and also Von Arx et al.,[19] in which prevalence rates of 85, 81, and 88.5% were reported, respectively [Table 1]. Teixeira et al.[7] found an incidence of 59% two canals in the mesial root of mandibular molars. The prevalence of isthmus was greatest 3-5 mm from the apex. In these cases, 22% were complete and 37% partial in mandibular molars. Bidar et al.[18] reported an isthmus incidence of 16% in distal roots with two canals of mandibular molars in a sample of Iranian population. This lower rate of isthmus could be explained by different roots (distal versus mesial). However, the authors emphasized that even this percentage would be taken into account during the cleaning and shaping of root canals. Furthermore, the highest and lowest prevalence rates of isthmuses in the present study were found at 6 mm and 2 mm distances from the root apex, respectively. Therefore, the number of isthmuses increases from 2 to 6 mm distance beyond the apex. Previous studies, similar to our study, have shown the highest prevalence of isthmuses at 4-6 mm distances from the apex in the mesial roots of mandibular molars.[5,7,14] In addition, we found the highest and lowest prevalence rates of complete isthmuses at 2 and 6 mm distances, respectively, indicating a progressive decrease in the number of complete isthmuses from 2 to 6 mm beyond the apex. The prevalence of complete isthmus at 2 mm from the apex, in our study, was higher than that of the findings of Gu et al.[5]
Management of complete isthmus is easier with the use of microsurgical techniques, such as the usage of a dental operating microscope and microsurgical instruments; however, preparation of incomplete isthmuses is more difficult and requires the accurate use of fine ultrasonic tips.[17] In the present study, a higher rate of incomplete isthmus was found in the 6 mm apical root, indicating a challenging situation during nonsurgical preparation of mandibular molars. Additionally, following 3 mm root end resection during periapical surgery, retropreparation and retrofilling to a depth of 3 mm are suggested to clean and fill the 6 mm apically located segment of an isthmus.[5]
Different methods have been used for the evaluation of isthmuses. In our study, the teeth were sectioned and evaluated under a stereomicroscope, similar to the technique used by Teixeria et al.[7] and Bidar et al.[18] The sectioning, staining, and clearing is a commonly used technique due to its greater accuracy in the detection of isthmus than other techniques.[6,7,20] However, microcomputed tomography is a modern technique, which is used at present for the evaluation of the morphology, location, and configuration of isthmus. The technique was first used by Mannocci et al.[13] to determine the prevalence of isthmuses in the mesial roots of mandibular first molars. One of the advantages of this technique is a thorough reconstruction of the root canal system without destroying the specimens.[20] If the isthmuses are not cleared of bacteria, there is potential for the treatment to fail, and the presence of unsuspected isthmuses may also affect the quality of the root canal filling. Therefore, complete removal of debris and micro-organisms from the apical third of the root canal is an important predicting factor for improving the long-term prognosis of endodontic treatment.[13]
A recent study found that the residual bacteria which frequently are entrapped in ramifications, isthmuses, and dentinal tubules makes it necessary to use an antibacterial irrigant and inter appointment medicament to maximize bacterial reduction before filling of the infected teeth. However, the complete eradication of bacteria could not be achieved in apical isthmus after two sessions of endodontic therapy.[21] Despite various studies on the evaluation and management of isthmuses and recent advances in nonsurgical endodontic treatment modalities such as modern sonic and ultrasonic irrigation devices, side-vented needle irrigation (SNI), and VPro EndoSafe (VPro), cleaning and shaping of isthmus areas is still difficult.[22,23] Susin et al. showed that the application of negative pressure techniques for the removal of debris from the isthmus in the mesial root of a mandibular first molar does not lead to the removal of more debris compared to the manual dynamic irrigation technique and none of the techniques completely removes debris from an isthmus.[24] Some in vitro studies have shown that none of the isthmuses in the root canals can be completely obturated with root-filling materials during conventional endodontic treatment.[25,26] It was shown that production of dentinal debris during canal instrumentation and its penetration into the isthmuses of mesial root canals of mandibular molars prevent penetration of sealers and filling materials into the isthmuses despite continuous irrigation during and after instrumentation.[26]
Therefore, proper management of isthmuses including bacterial reduction and complete filling requires future application of newer technologies and then further studies to verify their efficacies. A recent study by de Groot et al.[27] on the cleaning efficacy of laser-activated irrigation of root canals showed that the use of this technique is more efficient in removing debris from the apical third of the root canal compared to passive ultrasonic irrigation and hand irrigation techniques. In addition, the application of Er, Cr:YSGG laser (Er, Cr:YSGG: Erbium, chromium-doped:yttrium, scandium, gallium, and garnet) for the obturation of root canal system resulted in an increased rate of better obturated root canals and isthmuses.[28] Therefore, it is postulated that the use of modern technologies such as lasers, modern irrigation devices, and surgical microscopes might result in a more thorough cleaning and obturation of isthmuses during surgical and nonsurgical endodontic treatments.
CONCLUSION
Isthmuses are very common in the mesial roots of mandibular permanent molars in the Iranian population, with the highest prevalence in those at 6 mm distance from the root apex. Therefore, endodontic microscopes and newer technologies should be used for cleaning and obturation of isthmuses to achieve higher success rates in endodontic treatment.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Weller RN, Niemczyk SP, Kim S. Incidence and position of the canal isthmus. Part 1. Mesiobuccal root of the maxillary first molar. J Endod. 1995;21:380–3. doi: 10.1016/s0099-2399(06)80975-1. [DOI] [PubMed] [Google Scholar]
- 2.Pineda F. Roentgenographic investigation of the mesiobuccal root of the maxillary first molar. Oral Surg Oral Med Oral Pathol. 1973;36:253–60. doi: 10.1016/0030-4220(73)90247-8. [DOI] [PubMed] [Google Scholar]
- 3.Von Arx T. Frequency and type of canal isthmuses in first molars detected by endoscopic inspection during periradicular surgery. Int Endod J. 2005;38:160–8. doi: 10.1111/j.1365-2591.2004.00915.x. [DOI] [PubMed] [Google Scholar]
- 4.Vertucci FJ. Root canal anatomy of the human permanent teeth. Oral Surg Oral Med Oral Pathol. 1984;58:589–99. doi: 10.1016/0030-4220(84)90085-9. [DOI] [PubMed] [Google Scholar]
- 5.Gu L, Wei X, Ling J, Huang X. A microcomputed tomographic study of canal isthmuses in the mesial root of mandibular first molars in a Chinese population. J Endod. 2009;35:353–6. doi: 10.1016/j.joen.2008.11.029. [DOI] [PubMed] [Google Scholar]
- 6.Hsu YY, Kim S. The resected root surface. The issue of canal isthmuses. Dent Clin North Am. 1997;41:529–40. [PubMed] [Google Scholar]
- 7.Teixeira FB, Sano CL, Gomes BP, Zaia AA, Ferraz CC, Souza-Filho FJ. A preliminary in vitro study of the incidence and position of the root canal isthmus in maxillary and mandibular first molars. Int Endod J. 2003;36:276–80. doi: 10.1046/j.1365-2591.2003.00638.x. [DOI] [PubMed] [Google Scholar]
- 8.Burleson A, Nusstein J, Reader A, Beck M. The in vivo evaluation of hand/rotary/ultrasound instrumentation in necrotic, human mandibular molars. J Endod. 2007;33:782–7. doi: 10.1016/j.joen.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 9.Carr GB, Schwartz RS, Schaudinn C, Gorur A, Costerton JW. Ultrastructural examination of failed molar retreatment with secondary apical periodontitis: An examination of endodontic biofilms in an endodontic retreatment failure. J Endod. 2009;35:1303–9. doi: 10.1016/j.joen.2009.05.035. [DOI] [PubMed] [Google Scholar]
- 10.Nair PN, Henry S, Cano V, Vera J. Microbial status of apical root canal system of human mandibular first molars with primary apical periodontitis after “one-visit” endodontic treatment. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:231–52. doi: 10.1016/j.tripleo.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 11.Stropko JJ, Doyon GE, Gutmann JL. Root end management: Resection, cavity preparation, and material placement. Endod Top. 2005;11:131–51. [Google Scholar]
- 12.Skidmore AE, Bjorndal AM. Root canal morphology of the human mandibular first molar. Oral Surg Oral Med Oral Pathol. 1971;32:778–84. doi: 10.1016/0030-4220(71)90304-5. [DOI] [PubMed] [Google Scholar]
- 13.Mannocci F, Peru M, Sherriff M, Cook R, Pitt Ford TR. The isthmuses of the mesial root of mandibular molars: A micro-computed tomographic study. Int Endod J. 2005;38:558–63. doi: 10.1111/j.1365-2591.2005.00994.x. [DOI] [PubMed] [Google Scholar]
- 14.Fan B, Pan Y, Gao Y, Fang F, Wu Q, Gutmann JL. Three-dimensional morphologic analysis of isthmuses in the mesial roots of mandibular molars. J Endod. 2010;36:1866–9. doi: 10.1016/j.joen.2010.08.030. [DOI] [PubMed] [Google Scholar]
- 15.Kim S, Pecora G, Rubinstein RA. Color Atlas of Microsurgery in Endodontics. Philadelphia: W.B. Saunders Company; 2001. The resected root surface and isthmus; pp. 98–104. [Google Scholar]
- 16.Rubinstein RA, Kim S. Long-term follow-up of cases considered healed one year after apical microsurgery. J Endod. 2002;28:378–83. doi: 10.1097/00004770-200205000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Kim S, Kratchman S. Modern endodontic surgery concepts and practice: A review. J Endod. 2006;32:601–23. doi: 10.1016/j.joen.2005.12.010. [DOI] [PubMed] [Google Scholar]
- 18.Bidar M, Sheikhnezmi M, Moradi S. In vitro evaluation of the presence of second canal in distal root of first and second mandibular molars. J Dent. 2006;30:177–82. [Google Scholar]
- 19.Von Arx, Steiner RG, Tay FR. Apical surgery: Endoscopic findings at the resection level of 168consecutively treated roots. Int Endod J. 2003;44:290–30. doi: 10.1111/j.1365-2591.2010.01811.x. [DOI] [PubMed] [Google Scholar]
- 20.Neelakantan P, Subbarao C, Subbarao CV, Ravindranath M. Root and canal morphology of mandibular second molars in an Indian population. J Endod. 2010;36:1319–22. doi: 10.1016/j.joen.2010.04.001. [DOI] [PubMed] [Google Scholar]
- 21.Vera J, Siqueira JF, Jr, Ricucci D, Loghin S, Fernandez N, Flores B, et al. One- versus two-visit endodontic treatment of teeth with apical periodontitis: A histobacteriologic study. J Endod. 2012;38:1040–52. doi: 10.1016/j.joen.2012.04.010. [DOI] [PubMed] [Google Scholar]
- 22.Johnson M, Sidow SJ, Looney SW, Lindsey K, Niu LN, Tay FR. Canal and Isthmus Debridement Efficacy Using a Sonic Irrigation Technique in a Closed-canal System. J Endod. 2012;38:1265–8. doi: 10.1016/j.joen.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 23.Sarno MU, Sidow SJ, Looney SW, Lindsey KW, Niu LN, Tay FR. Canal and Isthmus Debridement Efficacy of the VPro Endo Safe Negative-pressure Irrigation Technique. J Endod. 2012;38:1631–4. doi: 10.1016/j.joen.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 24.Susin L, Liu Y, Yoon JC, Parente JM, Loushine RJ, Ricucci D, et al. Canal and isthmus debridement efficacies of two irrigant agitation techniques in a closed system. Int Endod J. 2010;43:1077–90. doi: 10.1111/j.1365-2591.2010.01778.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jung IY, Seo MA, Fouad AF, Spangberg LS, Lee SJ, Kim HJ, et al. Apical anatomy in mesial and mesiobuccal roots of permanent first molars. J Endod. 2005;31:364–8. doi: 10.1097/01.don.0000145425.73364.91. [DOI] [PubMed] [Google Scholar]
- 26.Endal U, Shen Y, Knut A, Gao Y, Haapasalo M. A high-resolution computed tomographic study of changes in root canal isthmus area by instrumentation and root filling. J Endod. 2011;37:223–7. doi: 10.1016/j.joen.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 27.de Groot SD, Verhaagen B, Versluis M, Wu MK, Wesselink PR, van der Sluis LW. Laser activated irrigation within root canals: Cleaning efficacy and flow visualization. Int Endodc J. 2009;42:1077–83. doi: 10.1111/j.1365-2591.2009.01634.x. [DOI] [PubMed] [Google Scholar]
- 28.Varella CH, Pileggi R. Obturation of root canal system treated by Cr, Er: YSGG laser irradiation. J Endod. 2007;33:1091–3. doi: 10.1016/j.joen.2007.05.012. [DOI] [PubMed] [Google Scholar]


