Abstract
Background:
Glass and quartz fiber posts are used in restoration of structurally compromised roots. Accessory fiber posts are recently introduced to enhance the fiber post adaptation. This study evaluated the effectiveness of glass versus quartz accessory fiber posts.
Materials and Methods:
In this experimental study, 40 mandibular premolar roots with similar dimension (radius of 3.5 ± 0.2 mm and length of 13 ± 0.5 mm) were selected and their root canals were flared until 1.5 mm of dentin wall remained. They were randomly assigned to four groups (n = 10) and restored as follows: Exacto glass fiber post (EX), Exacto glass fiber post + 2 Reforpin accessories (EXR), D. T. Light quartz fiber post (DT), and D. T. Light quartz fiber post + 2 Fibercone accessories (DTF). All posts were cemented with Duo-Link resin cement and the cores were built with the particulate filler composite. Following 1-week water storage, specimens were subjected to fracture loads in a universal testing machine. The maximum loads and failure modes were recorded and analyzed with the two-way analysis of variance (ANOVA) and Fisher's exact tests (α = 0.05).
Results:
The mean fracture resistance values (N) were 402.8 (EX), 378.4 (EXR), 400.1 (DT), and 348.5 (DTF). Two-way ANOVA test showed neither reinforcing method (P = 0.094), nor post composition (P = 0.462) had statistically significant differences on fracture resistance of the structurally compromised premolar teeth. Fisher's exact test also demonstrated no statistically significant difference regarding two variables (P = 0.695). Core fracture was the most common failure mode (62.5%).
Conclusion:
Glass and quartz fiber posts with or without accessories restored the weakened premolar roots equally.
Keywords: Accessory fiber post, compromised roots, fracture resistance, glass, quartz
INTRODUCTION
Fracture resistance of the root-post-core assembly is a key factor to sustain the mechanical stability and clinical success of the restored endodontically treated teeth.[1] In some cases, roots are weakened due to the caries, trauma, pulp pathology, or iatrogenic events in endodontic treatment. Such weakened roots with a thin dentinal wall, stand at a higher risk of fracture which seriously compromise the long-term prognosis of the tooth-restoration success.[2,3,4,5]
Structurally compromised roots were conventionally restored with casting posts and cores with the advantages of post stiffness, optimum adaptation, and high retention; however, they unfortunately may experience unrestorable root fractures.[2] Therefore, fiber posts were introduced with lower elastic modulus, similar to that of dentin; and better biomechanical performance that might offer increased fracture resistance to the fragile compromised roots.[5,6,7,8] They are also compatible with Bis-GMA bonding techniques, allowing chemical and micromechanical bonding to the root dentin that leads to a more uniform stress distribution than metal posts.[9]
Recently, several methods were introduced to enhance the post adaptation in over flared canals and to compensate the remaining gaps. They included canal reinforcement with composite resins, accessory fiber posts (AFPs), woven bondable Ribbond fiber, and constructing direct or indirect anatomic fiber posts.[10,11,12,13] Some researchers showed that using AFPs resulted in comparable improvement in fracture resistance of compromised roots, close to that of composite reinforcement,[3,14] while others failed to corroborate it.[2,15,16] Li et al., concluded that adding accessories has a positive effect on stress distribution.[17] Mortazavi et al., also stated that Ribbond fiber restores most of the tooth fracture resistance.[5] On the other hand, anatomic fiber post construction is a time consuming technique and also needs canal undercut elimination, which further jeopardizes the root resistance.[2] Although, there is no evident consensus in AFPs effectiveness due to controversial results, however, this method seems time saving and offers the advantage of more favorable fracture patterns over single post placement.[14,15,17]
Glass and quartz are both silica based. Quartz is a crystalline form of silica, whereas glass is noncrystalline. Tomazinho et al., showed that the D. T. Light quartz fiber posts have higher flexural strength than the Exacto glass fiber posts,[18] and Akkayan and Gulmez found higher fracture strength in teeth restored with quartz fiber posts than those with glass fiber posts.[19] ‘Naumann et al., in their recent 10-year prospective study stated that the tooth type and number of remaining cavity walls are significant predictors for the survival of glass fiber posts supported endodontically treated teeth and the anterior teeth experience 2-fold increase in failure rate compared to the posteriors. Their study supports the use of fiber posts in premolar teeth.[20]
There have been no studies comparing the efficacy of adjoining glass versus quartz AFPs. Therefore, the purpose of this study was to evaluate the effectiveness of these two most popular post systems, glass and quartz; and also to evaluate the two methods, accessory post versus conventional single post placement, on fracture resistance and failure patterns of structurally compromised mandibular premolar root. The null hypothesis was set as neither post composition nor root reinforcing method influenced the fracture resistance, and both lead to similar fracture patterns.
MATERIALS AND METHODS
In this experimental study, 40 freshly extracted first mandibular premolars that had similar dimensions and morphologies (radius of 3.5 ± 0.2 mm and length of 13 ± 0.5 mm) were selected from teeth that were extracted for orthodontic purposes. They were hand scaled and stored in distilled water with 0.2% thymol solution at room temperature. Radiographs were taken to ensure the presence of a single canal. The cervical area of the selected teeth, mesiodistaly and buccolingualy, had the minimums diameters of 6 and 8 mm, respectively. Also, the roots were at least 14 mm in length. All of the teeth were examined with a stereomicroscope (Motic K-500L, Motic Incorporation Ltd, Hong Kong) under ×10 magnification to verify the absence of caries and cracks.
Preparation of over-flared root canal
Clinical crowns were removed 1 mm above the buccal cementoenamel junction (CEJ) with a double-faced diamond disk (Diaswiss, Geneva, Switzerland) and subsequently, the root canals were prepared at 1, 3, and 5 mm from the apex using Gates Glidden Drills #2, 3, and 4 (Mani, Japan), respectively. Canals were irrigated with 1% sodium hypochlorite during the preparation and finally rinsed with 10 ml of distilled water to eliminate the sodium hypochlorite. Then, they were thoroughly dried with the absorbent paper points and obturated by gutta percha points (GAPADENT CO., LTD, China) and sealer (AH Plus, DENTSPLY DeTrey GmbH, Konstanz, Germany) with the lateral condensation technique. Radiographs were taken to ensure the length and quality of root fillings [Figure 1a]. To simulate the periodontal ligament, root surfaces were dipped into melted wax up to 2 mm below the CEJ, resulting in 0.2-0.3 mm thick wax layer on root surfaces. Afterward, roots were mounted in cold cure acrylic blocks (2 cm diameter and 2.5 cm height) with the flattened occlusal surfaces placed 2 mm above the acrylic top. Acrylic plane represents the bone level. Blocks were placed in cold water to dissipate the heat and prevent wax layer deformation during acryl polymerization. After polymerization, roots were removed from the blocks and wax was removed from the root surface and acrylic socket using warm water. The acrylic blocks were filled with polysiloxan impression material (Speedex, Coltene, Switzerland) using a molding syringe. The roots were reinserted into their respective acrylic sockets and excess impression material was removed with #12 scalpel blade. Therefore, the polysiloxan filled the space previously occupied by wax, so providing a standard simulated periodontal ligament with a thickness of 0.2-0.3 mm. The top 8 mm of gutta percha was removed with a Peezo Reamer #3 (Mani, Japan) [Figure 1b] and the canals were subsequently enlarged with a round end taper diamond bur 850 023 (Diaswiss, Geneva, Switzerland). Remaining dentin wall was approximately 1.5 mm thick, measured with a digital caliper accurate to 0.05 mm [Figure 1c]. Materials used in this study are presented in Table 1.
Figure 1.
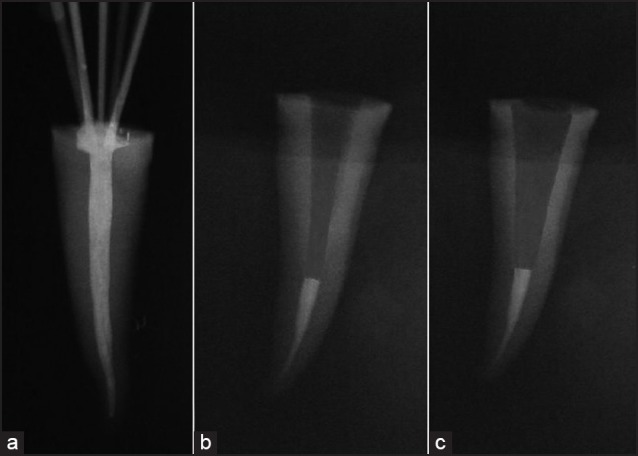
Root canal and post space preparation. (a) Radiograph obtained after obturation. (b) The canal was emptied to a depth of 8 mm. (c) The canal was flared till the remaining dentinal wall thickness reached 1.5 mm
Table 1.
Materials used in the experimental procedure
Post placement
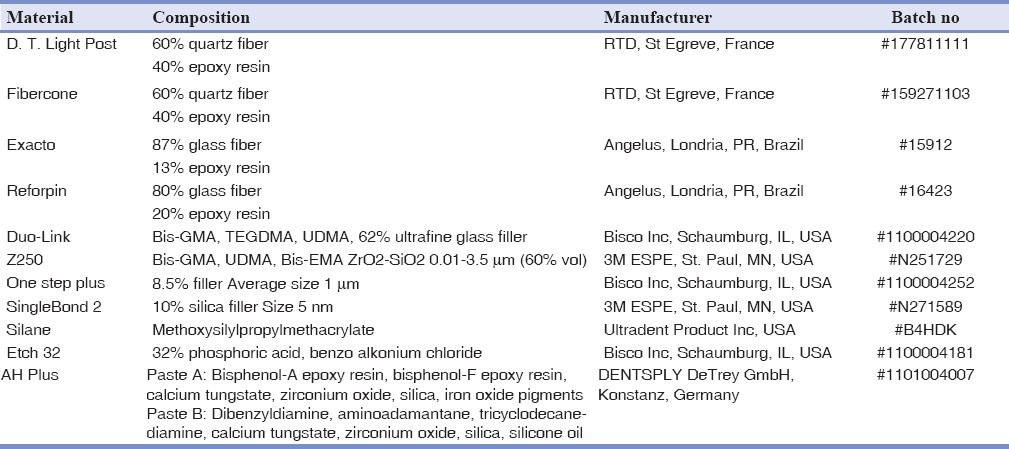
The specimens were randomly divided to four groups (n = 10). Each canal was etched with a 32% phosphoric acid gel (Etch-32, Bisco, Inc, Schaumburg, IL, USA) for 15 s, thoroughly rinsed with water for 30 s and then dried with absorbent paper points to avoid root dentin desiccation. Two consecutive coats of adhesive resin (One Step Plus, Bisco Inc., Schaumburg, IL, USA) were applied in with a microbrush (TPC, TPC Advanced Technology, China) for 15 s followed by absorbent paper point insertion to prevent adhesive pooling and then it was light cured for 20 s using a light-emitting diode (LED) curing unit with output intensity of 1,100 mW/cm2 (DEMI, Kerr, USA). Canals were filled with a dual-cured resin cement (Duo-link, Bisco, Inc, Schaumburg, IL, USA) using a needle tube provided by the manufacturer and the posts were placed as follows; In EX group, one glass fiber post #2 (Exacto, Angelus, Londria, PR, Brazil) was covered with the resin cement and inserted in the center of the canal. EXR group were restored as group EX + two accessory glass fiber posts (Reforpin, Angelus, Londria, PR, Brazil). DT group was restored with one quartz fiber post #2 (D. T. light, RTD, St Egreve, France.) and DTF group restored like DT group + two accessory quartz fiber posts (Fibercone, RTD, St Egreve, France). Before the cementation, all posts had been cleaned with 70% ethanol for 10 s, silanizated (Ultradent Silane, Ultradent product, Inc, USA) and finally coated by One Step Plus, which was light cured for 10 s. Excess cements were removed with a microbrush, and then light cured for 40 s. Experimental groups are displayed in [Figures 2a–d].
Figure 2.
Experimental groups. (a) Group EX (Exacto glass fiber post). (b) Group EXR, (Exacto glass fiber post + two Reforpin accessories). (c) Group DT (D. T. Light quartz fiber post). (d) Group DTF (D. T. Light quartz fiber post + 2 Fibercone accessories)
Core fabrication
All cemented posts were cut by diamond disk 927 104 (Diaswiss, Geneva, Switzerland), 3 mm above the flattened root surfaces. Each flattened surfaces was etched for 15 s, rinsed for 10 s and dried with tissue papers (wet bonding). Subsequently, they were covered with two consecutive coats of adhesive resin (SingleBond 2, 3M ESPE, St. Paul, MN, USA). Adhesive resin was gently air dried for 5 s then light cured for 10 s. Cores were built in three increments with the particulate filler composite resin (Z250, 3M ESPE, St. Paul, MN, USA) using 5 mm height and 4 mm width cylindrical polyethylene molds. Each layer was light cured for 20 s. The molds were removed and the occlusobuccal third of the cores were beveled at 45° angle to the root long axis, providing a bevel with 2 mm height and width. Subsequently, the specimens were stored in distilled water at 37°C for 1 week.
Compressive test
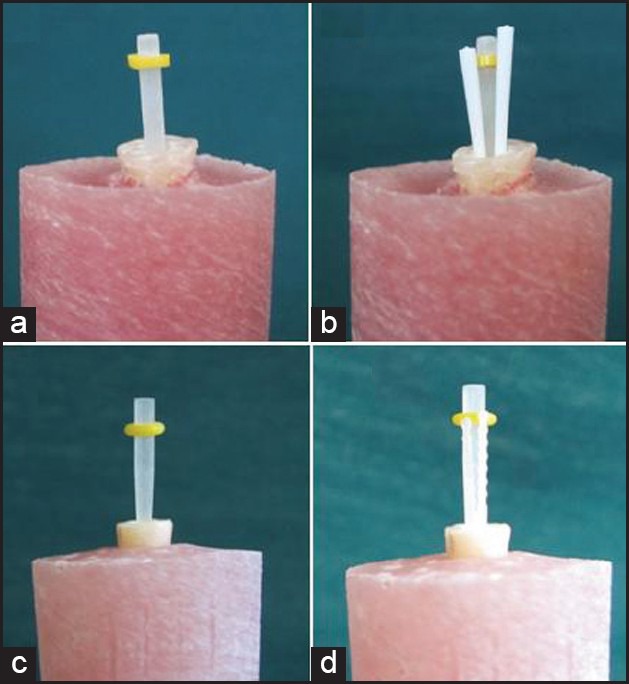
A custom made jig was fabricated with a 45° sloping surface to the horizon to standardize the position of specimens in the universal testing machine (Instron, zwick/roell Z020, Zwick, Ulm, Germany). All samples were subjected to incremental static loads at an angle of 45° to the long axis of roots. Loads were applied through a flattened end cone on core bevels with the crosshead speed of 0.5 mm/min [Figure 3]. The uppermost load to produce fracture was recorded and the failure patterns at fracture sites were also categorized as are displayed in [Figures 4a–f].
Figure 3.
45° compressive load
Figure 4.
Failure patterns. (a) Core detachment. (b) Core fracture more than one-third. (c) Complete core fracture. (d) Supracrestal root fracture. (e) Vertical root fracture. (f) Post cracking
Data were statistically analyzed with SPSS version 11.5 software (IBM, Armonk, NY, USA serial #: 30001359390). The two-way ANOVA test was performed to compare the effects of post material and reinforcing method on fracture resistance. Also, Fisher's exact test was performed to find a significant difference among failure patterns. P-values less than 0.05 were considered to be statistically significant.
RESULTS
The mean ± standard deviation (SD) of fracture resistance in experimental groups are presented in Table 2 and [Figure 5.] No interaction was found between the two variables [Figure 6]. The order of the fracture resistance was recorded as follows: EX > DT > EXR > DTF but two-way ANOVA test showed neither reinforcing method (P = 0.094), nor post composition (P = 0.462) had statistically significant differences on fracture resistance of the structurally compromised premolar teeth.
Table 2.
The mean fracture resistance value (N) of the experimental groups
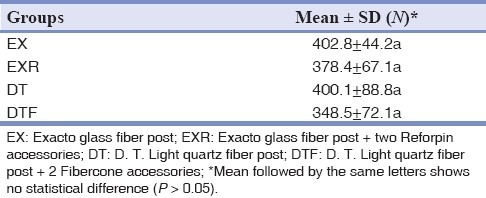
Figure 5.
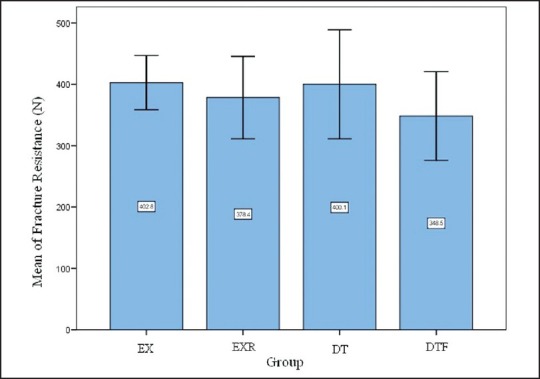
Fracture resistance mean and SD. EX: Exacto glass fiber post, EXR: Exacto glass fiber post + two Reforpin accessories, DT: D. T. Light quartz fiber post, DTF: D. T. Light quartz fiber post + 2 Fibercone accessories
Figure 6.
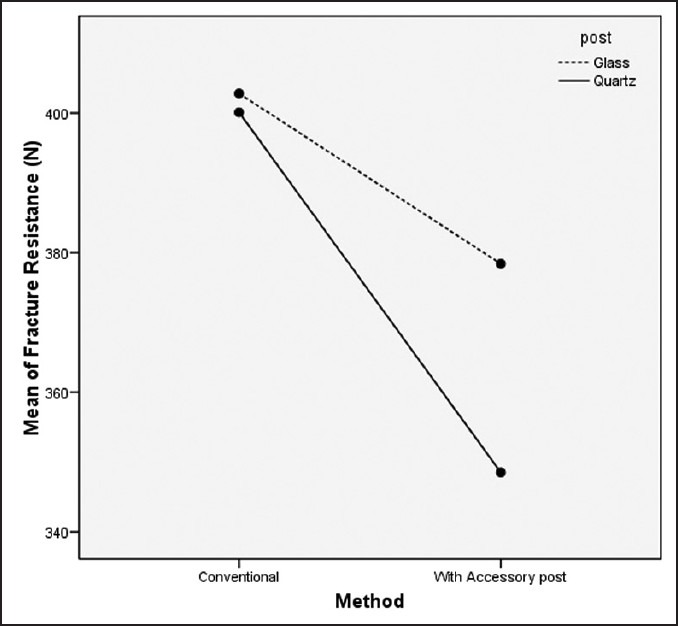
Patterns of change in the experimental groups
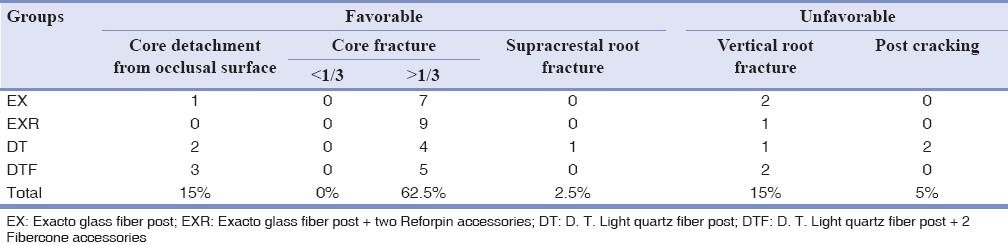
Failure pattern classification and distributions are provided in [Table 3]. The order of the favorable fracture prevalence was documented as follows: EXR > EX = DTF > DT; but Fisher's exact test demonstrated no statistically significant difference regarding two variables (P = 0.695). Core fracture was the most common failure pattern (62.5%).
Table 3.
Incidence of fractures (percent) in experimental groups
DISCUSSION
Structurally compromised roots encounters the clinicians with the challenge of selecting post composition and reinforcing method. Glass and quartz fiber posts have been evaluated in several studies and are extensively used in restoration of the endodontically treated teeth. Since these fiber posts have elastic modulus near to dentin and are capable of bonding to root dentin, they present some reinforcing effect to the structurally compromised roots.[5,6,7,8]
Although the D. T. Light posts have higher flexural strength than the Exacto post,[18] and teeth restored with quartz fiber posts have higher fracture strength than those with glass fiber posts,[19] both glass and quartz fiber posts performed the same in the present study. Maccari et al., also reported the same fracture resistance in flared roots restored with glass and quartz fiber posts,[21] which is in accordance with this study.
It has been reported that in glass and polyethylene fiber reinforced tooth colored restorations, bulk of fiber and type of bonding agent are important factors for increasing fracture load and flexural strength.[22,23,24,25] Also, post composition and bulk of post and resin cement affect stress distribution and fracture resistance in weakened roots.[14,15,16,17]
Clavijo et al., stated that although AFPs reduce the bulk of resin cements, there are still some empty spaces between fibers, which will be filled by the resin cement. This results in thicker cement layer that possibly contains more voids and bubbles, thus leading to a lower cohesive strength of the resin cements.[2] Nevertheless, in the present study, groups with AFPs showed reduced fracture resistance with respect to single post groups, but this was not statistically significant. This outcome could be related to the introduction of more filled resin cements with higher strength value that can strengthen the remaining root dentin. In single post placement technique, highly filled resin cement can strengthen the remaining root but in AFPs method, multiple spaces between AFPs weaken the resin cement. On the other hand, Mortazavi et al., showed that restoration of weakened roots with D. T. Light post in combination with Ribbond fibers restore most of the root fracture resistance.[5]
The mean occlusal load in mandibular region is about 373.8 ± 102.6 N in male and 314.7 ± 96.5 N in female,[26] which are approximately in the range of the fracture resistance we obtained in the present study. However, functional and parafunctional cyclic habits, as well as time and oral environmental factors result in fatigue and adhesive failures.[8,14]
According to Table 3, 80% of the teeth had favorable fractures. Favorable fractures imply to those such as core detachment, core fracture, and supracrestal root fracture in which tooth can be restored. Core fracture was the most common failure pattern and was more prevalent with the AFPs. This could be related to the voids and multiple spaces between fibers and the consequent reduction in cohesive strength of cores. Moosavi et al., reported that more incidence of core fracture with AFPs results from the frictional forces between multiple posts.[3] Incorporating crown as a final restoration will significantly reduce the risk of core fractures, but increase root fracture.[27] In one prospective study, Cagidiaco et al., concluded that endodontically treated premolars should be restored with fiber posts and complete crowns to obtain the highest success.[28]
In order to eliminate the ferrule effect, crown fabrication was eliminated in this study. Crown margin passes greater compression force to root cervical third, which diminishes the role of the post and core foundation in load transmission to whole root canal surface. Crown application also imparts some variables such as differences in their morphologies and additional interfacial bond surfaces, which both may lead to errors in interpreting the results.[29,30]
One of the concerns in reinforcing procedures is the establishment of efficient bonds between components such as dentin, resin cement, resin composite, and the fiber post. Although numerous researchers affirmed that loss of post retention was the most prevalent failure mode,[9,31] none of the specimen in this study showed this failure type. This event could be related to the intentional enlargement of root canals. The surface available for bonding has much more desirable condition and improved bond surface due to decreased tubular diameter and increased intertubular dentin. Also, this could be contributed to silanization. Many authors have reported an increase in resin-fiber post bond after silanization.[32] Clavijo et al., reported that silanization created a monoblock as a result of chemical bond between resin cements and the epoxy resin in fiber posts,[2] while others have different concepts. They believe that the chemical bond may be achieved only between the exposed glass or quartz fibers on the post and resin composite or cement, because the epoxy resin in fiber post has a high degree of conversion and is highly cross linked.[32] Silanization of the exposed glass and quartz fibers on the post play an important role especially in the case of non self-adhesive resin cements such as the one we used in this study.[33] Moreover, application of an eugenol-free sealer such as AH-Plus in root canal obturation reduces the probability of eugenol-resin interaction.[34]
Core detachment from the occlusal surface represents a stable adhesion between composite core and fiber posts that prohibits core fracture. According to [Table 3], they have mostly happened in the quartz fiber posts (12.5% of 15% total). This revealed a better adhesion between composite cores and quartz fibers. Aksornmuang et al., have also reported the same result in their research and concluded that this is due to the differences in the fiber's composition.[35] Qualtrough et al., similarly declared that quartz fibers have higher retentive values with respect to glass ones,[36] which is again in accordance with our finding.
Supracrestal fracture is defined as when the fracture line passes above the acrylic surface. One of the roots in the DT group was fractured supracrestaly that might be resulted from the stronger adhesion between quartz fiber, composite core, and occlusal dentin; which transferred the load, essentially, to the root cervical third.
Post fracture and root fracture are considered as unfavorable fractures that cannot be repaired. According to [Table 3], 15% of the roots were failed because of the vertical root fractures. They were distributed nearly equal in glass and quartz fiber posts and also in both post placement techniques.
Two posts were cracked in DT group, which may have resulted from more stress concentration in quartz fibers because of its crystalline and harder nature. Adding AFPs reduce the number of unfavorable fracture in both post compositions. This might be due to better stress distribution as a consequence of increase in the final post diameter. Clavijo et al., reported that roots with AFPs experience less unfavorable fractures.[2] Mortazavi et al., also declared that Ribbond fibers result in more desirable fracture patterns.[5]
The null hypotheses were strongly accepted and this study showed that glass and quartz fiber posts, with or without accessories; were equally effective in structurally compromised roots. Assuredly, in clinical situations, several factors such as oral cavity conditions and masticatory force may affect these in vitro results. Further studies with more aging period are recommended.
CONCLUSION
Based on the findings and within the limitations of this in vitro study, it could be concluded that in the structurally compromised roots, glass and quartz fiber posts with or without accessories, were equally effective in improving the fracture resistance and failure patterns.
ACKNOWLEDGEMENTS
This article was prepared based on a postgraduate thesis and a research project (#3789) approved by the Medical Ethics and Research Office at the Shiraz University of Medical Sciences. The authors would like to thank the office of vice chancellor for research of Shiraz University of Medical Sciences for their financial support. The authors also acknowledge the biomaterial research center in Dental Faculty of Shiraz University of Medical Sciences. The authors deny any conflict of interest.
Footnotes
Source of Support: The office of vice chancellor for research of Shiraz University of Medical Sciences
Conflict of Interest: None declared
REFERENCES
- 1.Ozcan M, Valandro LF. Fracture strength of endodontically treated teeth restored with post and cores and composite cores only. Oper Dent. 2009;34:429–36. doi: 10.2341/08-110. [DOI] [PubMed] [Google Scholar]
- 2.Clavijo VG, Reis JM, Kabbach W, Silva AL, Oliveira OB, Junior, Andrade MF. Fracture strength of flared bovine roots restored with different intra radicular posts. J Appl Oral Sci. 2009;17:574–8. doi: 10.1590/S1678-77572009000600007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moosavi H, Maleknejad F, Kimyai S. Fracture resistance of endodontically treated teeth restored using three root-reinforcement methods. J Contemp Dent Pract. 2008;9:30–7. [PubMed] [Google Scholar]
- 4.Ayad MF, Bahannan SA, Rosenstiel SF. Morphological characteristics of the interface between resin composite and glass-ionomer cement to thin-walled roots: A microscopic investigation. Am J Dent. 2010;23:103–7. [PubMed] [Google Scholar]
- 5.Mortazavi V, Fathi M, Katiraei N, Shahnaseri S, Badrian H, Khalighinejad N. Fracture resistance of structurally compromised and normal endodontically treated teeth restored with different post systems: An in vitro study. Dent Res J (Isfahan) 2012;9:185–91. doi: 10.4103/1735-3327.95234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Spazzin AO, Galafassi D, de Meira-Júnior AD, Braz R, Garbin CA. Influence of post and resin cement on stress distribution of maxillary central incisors restored with direct resin composite. Oper Dent. 2009;34:223–9. doi: 10.2341/08-73. [DOI] [PubMed] [Google Scholar]
- 7.Schmoldt SJ, Kirkpatrick TC, Rutledge RE, Yaccino JM. Reinforcement of simulated immature roots restored with composite resin, mineral trioxide aggregate, gutta-percha, or a fiber post after thermocycling. J Endod. 2011;37:1390–3. doi: 10.1016/j.joen.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 8.Schwartz RS, Robbins JW. Post placement and restoration of endodontically treated teeth: A literature review. J Endod. 2004;30:289–301. doi: 10.1097/00004770-200405000-00001. Review. [DOI] [PubMed] [Google Scholar]
- 9.Jongsma LA, Bolhuis PB, Pallav P, Feilzer AJ, Kleverlaan CJ. Benefits of a two-step cementation procedure for prefabricated fiber posts. J Adhes Dent. 2010;12:55–62. doi: 10.3290/j.jad.a17534. [DOI] [PubMed] [Google Scholar]
- 10.Lui JL. Composite resin reinforcement of flared canals using light-transmitting plastic posts. Quintessence Int. 1994;25:313–9. [PubMed] [Google Scholar]
- 11.Erkut S, Eminkahyagil N, Imirzalioglu P, Tunga U. A technique for restoring an over flared root canal in an anterior tooth. J Prosthet Dent. 2004;92:581–3. doi: 10.1016/j.prosdent.2004.08.016. [DOI] [PubMed] [Google Scholar]
- 12.Grandini S, Sapio S, Simonetti M. Use of anatomic post and core for reconstructing an endodontically treated tooth: A case report. J Adhes Dent. 2003;5:243–7. [PubMed] [Google Scholar]
- 13.Fokkinga WA, Kreulen CM, Le Bell-Rönnlöf AM, Lassila LV, Vallittu PK, Creugers NH. Fracture behavior of structurally compromised non-vital maxillary premolars restored using experimental fiber reinforced composite crowns. Am J Dent. 2006;19:326–32. [PubMed] [Google Scholar]
- 14.Silva GR, Santos-Filho PC, Simamoto-Júnior PC, Martins LR, Mota AS, Soares CJ. Effect of post type and restorative techniques on the strain and fracture resistance of flared incisor roots. Braz Dent J. 2011;22:230–7. doi: 10.1590/s0103-64402011000300009. [DOI] [PubMed] [Google Scholar]
- 15.Martelli H, Jr, Pellizzer EP, Rosa BT, Lopes MB, Gonini A., Jr Fracture resistance of structurally compromised root filled bovine teeth restored with accessory glass fiber posts. Int Endod J. 2008;41:685–92. doi: 10.1111/j.1365-2591.2008.01424.x. [DOI] [PubMed] [Google Scholar]
- 16.Zogheib LV, Saavedra Gde S, Cardoso PE, Valera MC, Araújo MA. Resistance to compression of weakened roots subjected to different root reconstruction protocols. J Appl Oral Sci. 2011;19:648–54. doi: 10.1590/S1678-77572011000600018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li Q, Xu B, Wang Y, Cai Y. Effects of auxiliary fiber posts on endodontically treated teeth with flared canals. Oper Dent. 2011;36:380–9. doi: 10.2341/10-283-L. [DOI] [PubMed] [Google Scholar]
- 18.Tomazinho FS, Zaitter FS, Silva SR, Alfredo E, Silva-Sousa YT. Flexural properties of fiber reinforced root canal posts. [Last accessed on: November 21 2012];J Dent Res. 2010 89(Spec. Iss. B) #3115. Available from: www.dentalresearch.org . [Google Scholar]
- 19.Akkayan B, Gülmez T. Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent. 2002;87:431–7. doi: 10.1067/mpr.2002.123227. [DOI] [PubMed] [Google Scholar]
- 20.Naumann M, Koelpin M, Beuer F, Meyer-Lueckel H. 10-year survival evaluation for glass-fiber-supported postendodontic restoration: A prospective observational clinical study. J Endod. 2012;38:432–5. doi: 10.1016/j.joen.2012.01.003. [DOI] [PubMed] [Google Scholar]
- 21.Maccari PC, Cosme DC, Oshima HM, Burnett LH, Jr, Shinkai RS. Fracture strength of endodontically treated teeth with flared root canals and restored with different post systems. J Esthet Restor Dent. 2007;19:30–6. doi: 10.1111/j.1708-8240.2006.00060.x. [DOI] [PubMed] [Google Scholar]
- 22.Sharafeddin F, Bahrani S. Load bearing capacity of fragmented incisal edge restored with two different positions of fiber reinforced composite restorations. J Dent Shiraz Univ Med Scien. 2011;11:23–8. [Google Scholar]
- 23.Sharafeddin F, Alavi AA, Farzinfar M. Effect of fiber orientation and position on fracture resistance and failure mode of cuspal coverage composite restorations. J Dent Shiraz Univ Med Scien. 2007;8:1–10. [Google Scholar]
- 24.Tavakkol M, Mortazavi MV, Sharafeddin F, Alavi AA. Effect of glass fiber length on flexural strength of fiber-reinforced composite resin. World J Dent. 2012;3:131–35. [Google Scholar]
- 25.Sharafeddin F, Alavi AA, Moshref Javadi F. The impact of bonding agent composision on flextural strength of fiber-reinforced composite. J Dent Shiraz Univ Med Scien. 2011;12:261–70. [Google Scholar]
- 26.Lepley CR, Throckmorton GS, Ceen RF, Buschang PH. Relative contributions of occlusion, maximum bite force, and chewing cycle kinematics to masticatory performance. Am J Orthod Dentofacial Orthop. 2011;139:606–13. doi: 10.1016/j.ajodo.2009.07.025. [DOI] [PubMed] [Google Scholar]
- 27.Kim YH, Lee JH. Influence of modification in core building procedure on fracture strength and failure patterns of premolars restored with fiber post and composite core. J Adv Prosthodont. 2012;4:37–42. doi: 10.4047/jap.2012.4.1.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cagidiaco MC, García-Godoy F, Vichi A, Grandini S, Goracci C, Ferrari M. Placement of fiber prefabricated or custom made posts affects the 3-year survival of endodontically treated premolars. Am J Dent. 2008;21:179–84. [PubMed] [Google Scholar]
- 29.Chuang SF, Yaman P, Herrero A, Dennison JB, Chang CH. Influence of post material and length on endodontically treated incisors: An in vitro and finite element study. J Prosthet Dent. 2010;104:379–88. doi: 10.1016/S0022-3913(10)60171-0. [DOI] [PubMed] [Google Scholar]
- 30.Al-Omiri MK, Mahmoud AA, Rayyan MR, Abu-Hammad O. Fracture resistance of teeth restored with post-retained restorations: An overview. J Endod. 2010;36:1439–49. doi: 10.1016/j.joen.2010.06.005. [DOI] [PubMed] [Google Scholar]
- 31.Cagidiaco MC, Goracci C, Garcia-Godoy F, Ferrari M. Clinical studies of fiber posts: A literature review. Int J Prosthodont. 2008;21:328–36. [PubMed] [Google Scholar]
- 32.Monticelli F, Osorio R, Sadek FT, Radovic I, Toledano M, Ferrari M. Surface treatments for improving bond strength to prefabricated fiber posts: A literature review. Oper Dent. 2008;33:346–55. doi: 10.2341/07-86. [DOI] [PubMed] [Google Scholar]
- 33.Jongsma LA, Kleverlaan CJ, Feilzer AJ. Influence of surface pretreatment of fiber posts on cement delamination. Dent Mater. 2010;26:901–7. doi: 10.1016/j.dental.2010.05.005. [DOI] [PubMed] [Google Scholar]
- 34.Tang W, Wu Y, Smales RJ. Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod. 2010;36:609–17. doi: 10.1016/j.joen.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 35.Aksornmuang J, Foxton RM, Nakajima M, Tagami J. Microtensile bond strength of a dual-cure resin core material to glass and quartz fibre posts. J Dent. 2004;32:443–50. doi: 10.1016/j.jdent.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 36.Qualtrough AJ, Chandler NP, Purton DG. A comparison of the retention of tooth-colored posts. Quintessence Int. 2003;34:199–201. [PubMed] [Google Scholar]


