Abstract
Purpose of review
Both cognitive and physical function are commonly impaired in individuals with chronic kidney disease (CKD), resulting in important impacts on quality of life and overall health. This review summarizes the burden of cognitive and physical impairment in CKD, focusing on recent research that highlights a possible unifying microvascular etiology among these shared comorbid conditions
Recent findings
Multiple small studies have been published recently evaluating cognitive and physical functioning in people with CKD. These studies overall demonstrate a high burden of comorbid conditions in people with CKD, including microvascular disease, that may result in cognitive impairment. Additionally, studies demonstrate that physical function is substantially worse than expected in individuals with CKD, that decreased physical activity is associated with worse outcomes, that frailty is very common and associated with an increased risk of death, and that structured exercise programs have small but tangible short term effects of markers of physical performance.
Summary
Impaired cognitive function and physical performance are important factors impacting the lives of people with CKD. Further research is necessary to better treat this important comorbid conditions in people with CKD.
Keywords: Cognitive impairment, microvascular disease, chronic kidney disease, physical function, frailty
Introduction/Purpose of Review
Among older populations, CKD is increasingly common,1 and it is estimated that one in three US residents will have estimated glomerular filtration rate (eGFR) below 45 ml/min per 1.73m2 over the course of their lifetime.2 Given multiple associated comorbid conditions and clearly described risks to independent living,3 CKD configures well to a geriatric syndrome model, whereby treatment of modifiable factors that are important to patients is emphasized.4 Critical mediators of threatened independence in individuals with CKD likely include impairments in both cognitive and physical function. The remainder of this article summarizes key elements of cognitive and physical function in CKD, focusing on recent research that highlights a possible unifying microvascular etiology among these shared comorbid conditions.
Cognitive Function
Cognitive impairment is common at all stages of chronic kidney disease,5-9 and likely has important effects on patient well-being. Impaired cognition potentially impacts multiple areas of patient care including patient compliance with treatment plans and quality of life.10-11Although multifactorial in etiology, vascular disease - and specifically cerebrovascular disease - clearly has an important role, in particular by impacting executive cognitive function.12-14
The increased risk of cardiovascular disease in people with CKD now is widely appreciated,15 but the concept that all vascular beds in the body may be impacted, including the brain, has only recently come to the forefront. Patients with CKD are at markedly higher risk of clinically overt stroke,16.17, and are significantly more likely to have subclinical manifestations of cerebrovascular disease on brain imaging, including white matter disease (also called leukoaraiosis), silent brain infarcts and cerebral atrophy.18
The Cerebrovascular Hypothesis
In the general population, cerebrovascular disease is a leading cause of cognitive impairment and the domains most affected in vascular dementia are executive function, attention and processing speed, attributes required for successful decision making and troubleshooting. Reflecting the high prevalence of cardiovascular disease and cerebrovascular disease in individuals with CKD, the leading hypothesis to date is that cognitive impairment in the CKD population is mediated by disease of brain microvasculature. This may be superimposed on other causes of cognitive impairment, such as Alzheimer’s Disease-related pathology. Accordingly, if cerebrovascular disease is complicit in cognitive impairment seen in individuals with CKD, studies should demonstrate (1) brain structural findings consistent with cerebrovascular disease, (2) cognitive impairment patterns consistent with vascular dementia, and (3) an association among systemic vascular disease, cerebrovascular disease and cognitive function. In the past several years, significant research has explored this hypothesis.
Brain Findings and Cerebrovascular Disease
Moodalbail and colleagues recently performed a systematic review of neuroimaging in children and adults with CKD. In 43 studies, with a preponderance of Asian dialysis patients, there was a fairly consistent pattern in people with CKD of: (1) increased cerebral atrophy; and (2) increased cerebral vascular disease, including deep white matter hyperintensities, white matter lesions, cerebral microbleeds, silent cerebral infarction, and cortical infarction. More recently, within a US hemodialysis population, Drew and colleagues evaluated brain MRI results in 45 maintenance hemodialysis patients and non-CKD 67 controls with no known prior stroke. In multivariable analyses, ESRD patients had greater white matter burden, more brain atrophy, and a higher prevalence of both small- (17.8%) and large- (7.8%) vessel infarcts than controls (combined, 22% vs 0%; P <0.001).19▲ A 2007 study in Korea demonstrated similar findings in a maintenance peritoneal dialysis population.20 The key contributions of these reports are demonstration of a high prevalence of structural damage associated with microvascular cerebrovascular disease.
Cerebrovascular Disease and Cognitive Function
Many studies evaluating cognitive performance in people with CKD are limited either by fairly insensitive cognitive assessments, cross-sectional design, or lack of assessment concurrent vascular disease, kidney disease, cognitive functioning and brain structure. However, viewed in sum, recent studies have established inter-relationship among systemic vascular disease markers, kidney function and cognitive function.
Albuminuria is an indicator of kidney disease and also likely serves as a marker of systemic vascular health, with even small elevations in urine albumin excretion associated with an increased risk of death.21 Accordingly, prior studies have shown an association between albuminuria and cognitive performance,5 particularly executive function.13 In 2012, Sajjad and colleagues published the results of a post hoc analysis of the Nurses’ Health Study and described an association between higher levels of albuminuria, beginning at levels within the normal range, and cognitive decline across multiple cognitive domains, a baseline ACR ≥5 mg/g versus was equivalent to the effect of approximately 5 years of aging on cognitive performance.22 Similarly, Davey and colleagues examined the longitudinal relationship between changes in kidney function and rate of decline in cognitive function among 590 community-dwelling middle-aged and older adults without dementia or prior stroke. Greater declines in eGFR over 5 years correlated with greater declines on performance of tests of global cognitive function, verbal memory, and abstract reasoning after accounting for baseline eGFR and co-morbidity.23▲ Finally, Barzilay and colleagues recently published a post hoc analysis of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) Memory in Diabetes (MIND) trial, demonstrating that persistent albuminuria and progressive albuminuria are associated with a decline in cognitive function in relatively young individuals with diabetes with unimpaired eGFR. The most notable results were seen in tests assessing processing speed, while there was no significant difference in memory or executive function performance.24▲▲ These results similarly suggest shared susceptibility of the kidneys and brain to common injury with aging, such as microvascular disease.
Several studies support the association between cerebrovascular disease and cognitive function. In the general population, a recent study from the Women’s Health Initiative Memory Study found a robust association between prevalent cardiovascular disease or cardiovascular disease risk factors and subsequent cognitive decline.25▲ This study did not evaluate specific cognitive domains. Supporting the association between microvascular disease and cognitive function in individuals with CKD, Yaffe and colleagues reported cross-sectional results from 588 participants with CKD in the Chronic Renal Insufficiency Cohort (CRIC) Study, evaluating the association between retinopathy and cognitive performance evaluated using a 6 test battery.26▲▲ Compared with those without retinopathy, participants with retinopathy had a markedly higher likelihood of impaired executive function, attention and naming in multivariable adjusted analyses. There also was a ‘dose-effect’, such that increased level of retinopathy was associated with lower executive function and attention cognitive performance. These findings suggest that retinopathy, a readily diagnosed microvascular process, is associated with a pattern of cognitive impairment in individuals with CKD that is linked to cerebrovascular disease.27
Dialysis and Cognitive Function
Two important studies were recently published exploring cognitive function in patients treated with dialysis, building on the earlier reports of Murray and colleagues.7-8 Kurella Tamura and colleagues, evaluating cognitive function in 218 participants in the Frequent Hemodialysis Network (FHN) Daily Trial and 81 participating in the FHN Nocturnal Trial, found no benefit of 1-year of frequent hemodialysis in either trial for any cognitive domains.28▲▲ This study demonstrates that higher small solute clearance with dialysis does not result in relatively short term improvements in cognitive performance, suggesting that, in well-dialyzed patients, worse cognitive performance is not a function of uremic solutes.
Sarnak and colleagues reported the results of a cross-sectional cohort of 314 US hemodialysis patients who underwent detailed neurocognitive assessment.9▲▲ Compared with population norms, patients receiving maintenance hemodialysis had significantly poorer executive function but not memory performance, a finding that persisted in the subgroup with Mini-Mental State Examination (MMSE) score of 24 or higher, a level considered consistent with normal cognitive performance. In regression models, vascular risk factors and vascular disease were associated with lower executive function, building on prior recently published findings showing an association between prevalent cardiovascular disease and worse executive functioning in this same cohort.14 In addition to revealing that the MMSE is an insufficient screening test for cognitive impairment in dialysis patients, likely because the MMSE does not evaluate executive functioning, by suggesting a vascular disease pattern of cognitive impairment, the Sarnak study is concordant with findings by Yaffe and colleagues from CRIC and the lack of a benefit seen in FHN, in as much as cerebrovascular disease is a chronic process that is unlikely to be significantly impacted over the short time span between cognitive assessments in FHN.
Treatment
While research suggests a vascular disease etiology for the preponderance of cognitive impairment in CKD, few studies have evaluated treatment. Secondary analyses of large cohorts suggest that midlife control of risk factors lead to better cognition, particularly in vascular domains.29-31 In contrast, ACCORD-MIND showed no benefit of intensive glycemic control on cognitive outcomes, although total brain volume remained higher in those receiving intensive therapy, suggesting that earlier in life intervention has the potential to be beneficial.32 Specific to the CKD population, Kang and colleagues evaluated the association between sleep disordered breathing and cognitive impairment in a cohort of 169 patients with CKD stages 4-5. Participants with sleep-disordered breathing, defined by an apnea-hypopnea index >15, had significantly lower scores in tests measuring verbal memory, working memory, attention, and psychomotor speed, particularly among younger study participants. This study highlights that a potentially modifiable characteristic, sleep quality, was associated with worse function in younger patients, a population where cerebrovascular disease may be less apparent.33▲
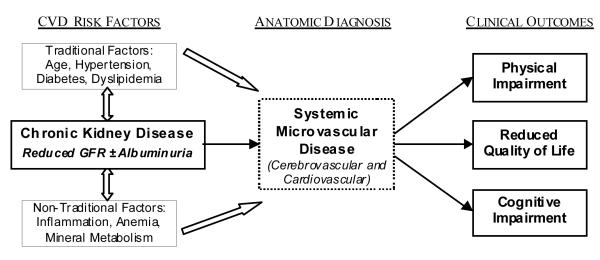
In sum, cognitive impairment is common across all stages of CKD and likely predominantly mediated by cerebrovascular disease (Figure 1). Few data exist on treatment but addressing vascular disease risk factors earlier in life may decrease the subsequent burden of cognitive impairment in this population.
Figure 1.
Concept diagram of the development of and effects of cardiovascular and cerebrovascular disease in CKD, presenting the transition from cardiovascular disease risk factors, including CKD, to clinical outcomes, including cognitive and physical impairment, mediated by microvascular disease.
Physical Function
Early studies conducted predominately in patients with ESRD demonstrate marked impairment in aerobic capacity and physical performance and lower physical activity compared to healthy populations. More recently, studies conducted in non-dialysis CKD patients and among general population cohorts demonstrate worse physical performance - especially lower extremity performance – across the spectrum of CKD, particularly in older adults. Prior small interventional trials conducted largely in ESRD patients suggest beneficial effects of structured exercise training on physical performance, cardiorespiratory fitness, and patient-reported outcomes, while a small number of trials suggest similar benefit in non-dialysis CKD patients.34
CKD and Physical Inactivity
The prognostic importance of physical inactivity in CKD patients was examined in 2 recent reports. Matsuzawa et al. directly measured physical activity using accelerometers among 202 Japanese maintenance dialysis patients who were free of severe cardiovascular disease and ambulated independently.35▲ Over up to 84 months, those who engaged in ≥50 minutes/day of at least light physical activity (characterized by at least gentle walking) had a cumulative survival of 93%, compared with 77% among those with fewer than 50 minutes/day. Following adjustment for cardiovascular disease, obesity, nutrition/inflammation, and demographics, each 10-minute/day greater activity was associated with a 22% lower risk of death. In another study, Robinson et al described the relationship between self-reported leisure-time physical activity and kidney function decline among 256 outpatients with stage 3-4 CKD.36▲ Notably, nearly 1 of 4 patients reported no leisure-time activity at all in the last 4 weeks; these patients had an adjusted annualized decline in eGFR of 9.4% per year. In contrast, those patients with at least 150 minutes of leisure-time activity (consistent with consensus guidelines for physical activity in the general population) had an adjusted annualized decline in eGFR of 6.6% per year (p=0.05). These studies suggest that maintenance of greater habitual or leisure-time physical activity may reduce mortality risk in ESRD and slow the rate of kidney function decline. Additionally, these observed associations of activity with mortality and kidney function decline are consistent with prior observational studies in the general population. However, due to the observational design these study cannot establish causality, and it is possible that physical activity in individuals with CKD is a marker of disease burden and severity rather than a readily modifiable behavioral characteristic.
Exercise Training in non-Dialysis CKD
Directly testing the effects of increasing physical activity in patients with CKD requires a randomized controlled trial of a physical activity or exercise training program. Recently, Howden et al examined the effects of exercise training on cardiorespiratory fitness and function among 83 stage 3-4 CKD patients (eGFR 25-60 cc/min/1.73m2) with at least one uncontrolled cardiovascular risk factor (blood pressure, obesity, glycemic control).37▲▲ Patients were randomized to usual care or an exercise training and lifestyle intervention, which consisted of 4 weeks of group behavior/dietary modification (focused on weight loss) as well as a 12 month exercise training program. This program incorporated 150 minutes of moderate intensity aerobic and resistance training weekly, with the first 8 weeks performed in-center, followed by 10 months of unsupervised home-based training. At 12 months, aerobic capacity (VO2peak) increased moderately, by roughly 11%, in the active exercise group compared to a slight decline in the control group (p=0.01). Among echocardiographic measures, ejection fraction did not change significantly between the two groups, although several measures of diastolic function improved modestly in the exercise group. This study demonstrated the safety and feasibility of a home-based exercise training program among adults with stage 3-4 CKD at high cardiovascular risk, with the potential for significant if somewhat modest improvements in aerobic capacity and diastolic function.
Lower Extremity Function in CKD
Roshavarnan et al. recently assessed lower extremity function in 385 ambulatory stage 2-4 CKD patients.38▲ Lower extremity function, as measured by standardized physical tests, was 30%-55% worse than expected based on normative data accounting for age, sex, and body size. Furthermore, worse lower extremity function was strongly predictive of subsequent mortality, independent of co-morbidity, obesity, and kidney function. Notably, the prognostic importance of lower extremity function was much greater than that of commonly measured biochemical parameters in CKD, including estimated GFR, hemoglobin, phosphate, and bicarbonate. The results of this study suggest that simple objective measures of lower extremity physical function may be adjunctive to standard clinical and laboratory measures in risk prediction in stage 2-4 CKD.
Lower extremity function typically declines with aging. Liu et al examined the relation between CKD, defined by eGFR below <60 ml/min/1.73m2, and decline in lower extremity function among older adults in the Framingham Offspring Study.39▲▲ Among 1226 participants (mean age=68), those with CKD had significantly greater decline in usual walking speed over 6 ½ years, even after accounting for initial physical activity and co-morbidity (p=0.004). Furthermore, participants with CKD were 55% more likely to have incident mobility disability as defined by self-reported dependence in walking and/or climbing stairs (odds ratio=1.55, 95% CI: 1.05, 2.31). Among all participants, lower estimated GFR, determined using a cystatin C-based rather than creatinine-based estimating equation, was associated with greater mobility disability and gait speed decline. Results of this study demonstrate that lower GFR is a marker for subsequent physical disability and more rapid decline in physical function, independent of physical activity, highlighting the importance of potential interventions to maintain functional independence in this population.
Kidney Disease and Frailty
Three recent manuscripts examined the prevalence and significance of frailty in patients with CKD or ESRD. Frailty refers to a complex phenotype of aging characterized by a combination of objective and subjective findings: unintentional weight/muscle loss, muscle weakness, slow gait, physical inactivity, and exhaustion/fatigue. Different studies have applied different criteria to define the presence of frailty. In dialysis patients, Bao et al examined the prevalence and correlates of frailty using data from the USRDS Comprehensive Dialysis study.40▲ Frailty was defined using patient-reported questionnaires only and information on weight loss was not available to help define frailty. Frailty as defined by the authors was present among 73% of 1576 incident dialysis patients; these patients were at 57% greater risk of death and 26% greater risk of first hospitalization compared to non-frail patients. Among stage 1-4 CKD patients in the Seattle Kidney Study (SKS), Roshanravan et al reported 14% prevalence of frailty, with a monotonic increase in prevalence with more severe CKD.41▲▲ Of note, both weakness and slow gait were measured directly in this study. Frail patients were 2.5 times as likely to die or initiate dialysis during follow-up, after accounting for initial kidney function and co-morbidity. In contrast, a lower prevalence of frailty (7%) was observed among 1,111 stage 2-4 CKD patients participating in the CRIC multicenter study, with higher prevalence rates at lower eGFR levels.42▲ Frail patients had significantly worse lower extremity performance on the Short Physical Performance Battery. In both the SKS and CRIC, higher body mass index was associated with a greater prevalence of frailty. These studies suggest a direct relationship between kidney disease severity and frailty, and further that frailty in CKD has prognostic significance beyond standard comorbidity. The relationship of frailty with higher rather than lower body mass index suggests that in CKD this phenotype may occur in setting of excess adiposity, in contrast to the traditional conception of age-related frailty characterized by a normal or decreased BMI.
In sum, the cumulative data to date demonstrate that patients with CKD have lower than expected physical function and activity, and that these impairments have strong prognostic importance. Additionally, there is evidence that a program of structured aerobic and resistance exercise training can result in modest improvements in cardiorespiratory fitness and cardiac function.
Summary
Impaired cognitive function and physical performance are important factors impacting the lives of people with CKD. While vascular disease is likely an important mediator, particularly of cognitive impairment, many of the mechanisms which contribute to impaired physical function and increased frailty in CKD remain to be elucidated. While prevention through control of cardiovascular disease risk factors and lifestyle interventions seems prudent, the optimal management of cognitive and physical impairments in CKD remains uncertain. It is likely that exercise interventions, which address both microvascular health as well as frailty, may have substantial benefits for both cognitive and physical performance in this vulnerable population.
Key Points.
Vascular disease, and specifically microvascular disease, is common in all stages of CKD and associated with important comorbid conditions, including impairments in cognitive and physical functioning.
Cognitive impairment is common at all stages of CKD, associated with cerebrovascular disease, and manifests more often with deficits in executive functioning, attention and processing speed.
Physical impairments and frailty are common in individuals with CKD and are associated with increased risk of death.
Exercise training programs appear effective and safe, even in individuals with advanced CKD, based on findings from relatively brief clinical trials
Acknowledgements
Dr. Weiner and Dr. Seliger’s research in this field is funded by NIH R01 DK090401 (Exercise training and cognitive and physical function in CKD). Neither author has any conflicts of interest related to the content of this manuscript.
REFERENCES AND RECOMMENDED READING
Papers of particular interest, published within the annual period of review, have been highlighted as:
▲ of special interest
▲▲ of outstanding interest
- 1.Bowling CB, Sharma P, Fox CS, O’Hare AM, Muntner P. Prevalence of reduced estimated glomerular filtration rate among the oldest old from 1988-1994 through 2005-2010. JAMA. 2013;310:1284–6. doi: 10.1001/jama.2013.252441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grams ME, Chow EK, Segev DL, Coresh J. Lifetime incidence of CKD stages 3-5 in the United States. Am J Kidney Dis. 2013;62:245–52. doi: 10.1053/j.ajkd.2013.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bowling CB, Muntner P, Sawyer P, et al. Community Mobility Among Older Adults With Reduced Kidney Function: A Study of Life-Space. Am J Kidney Dis. 2013 doi: 10.1053/j.ajkd.2013.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bowling CB, O’Hare AM. Managing older adults with CKD: individualized versus disease-based approaches. Am J Kidney Dis. 2012;59:293–302. doi: 10.1053/j.ajkd.2011.08.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kurella Tamura M, Muntner P, Wadley V, et al. Albuminuria, kidney function, and the incidence of cognitive impairment among adults in the United States. Am J Kidney Dis. 2011;58:756–63. doi: 10.1053/j.ajkd.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yaffe K, Ackerson L, Kurella Tamura M, et al. Chronic kidney disease and cognitive function in older adults: findings from the chronic renal insufficiency cohort cognitive study. J Am Geriatr Soc. 2010;58:338–45. doi: 10.1111/j.1532-5415.2009.02670.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kalirao P, Pederson S, Foley RN, et al. Cognitive impairment in peritoneal dialysis patients. Am J Kidney Dis. 2011;57:612–20. doi: 10.1053/j.ajkd.2010.11.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murray AM, Tupper DE, Knopman DS, et al. Cognitive impairment in hemodialysis patients is common. Neurology. 2006;67:216–23. doi: 10.1212/01.wnl.0000225182.15532.40. [DOI] [PubMed] [Google Scholar]
- ▲▲ 9.Sarnak MJ, Tighiouart H, Scott TM, et al. Frequency of and risk factors for poor cognitive performance in hemodialysis patients. Neurology. 2013;80:471–80. doi: 10.1212/WNL.0b013e31827f0f7f. Cohort study of 314 US hemodialysis patients demonstrating that poor cognitive performance is very common and is associated with vascular disease risk factors. Additionally, this study demonstarted that screening for cognitive impairment in dialysis patients with the Mini-Mental State Examination is ineffective.
- 10.Sorensen EP, Sarnak MJ, Tighiouart H, et al. The kidney disease quality of life cognitive function subscale and cognitive performance in maintenance hemodialysis patients. American Journal of Kidney Diseases. 2012;60:417–26. doi: 10.1053/j.ajkd.2011.12.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sehgal AR, Grey SF, DeOreo PB, Whitehouse PJ. Prevalence, recognition, and implications of mental impairment among hemodialysis patients. American Journal of Kidney Diseases. 1997;30:41–9. doi: 10.1016/s0272-6386(97)90563-1. [DOI] [PubMed] [Google Scholar]
- 12.Kurella Tamura M, Xie D, Yaffe K, et al. Vascular risk factors and cognitive impairment in chronic kidney disease: the Chronic Renal Insufficiency Cohort (CRIC) study. Clin J Am Soc Nephrol. 2011;6:248–56. doi: 10.2215/CJN.02660310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Weiner DE, Bartolomei K, Scott T, et al. Albuminuria, cognitive functioning, and white matter hyperintensities in homebound elders. Am J Kidney Dis. 2009;53:438–47. doi: 10.1053/j.ajkd.2008.08.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Weiner DE, Scott TM, Giang LM, et al. Cardiovascular disease and cognitive function in maintenance hemodialysis patients. Am J Kidney Dis. 2011;58:773–81. doi: 10.1053/j.ajkd.2011.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weiner DE, Sarnak MJ. A decade after the KDOQI CKD guidelines: impact on the cardiovascular disease-CKD paradigm. Am J Kidney Dis. 2012;60:710–2. doi: 10.1053/j.ajkd.2012.08.017. [DOI] [PubMed] [Google Scholar]
- 16.Lee M, Saver JL, Chang KH, Liao HW, Chang SC, Ovbiagele B. Low glomerular filtration rate and risk of stroke: meta-analysis. BMJ. 2010;341:c4249. doi: 10.1136/bmj.c4249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang HH, Hung SY, Sung JM, Hung KY, Wang JD. Risk of Stroke in Long-term Dialysis Patients Compared With the General Population. Am J Kidney Dis. 2013 doi: 10.1053/j.ajkd.2013.10.013. [DOI] [PubMed] [Google Scholar]
- 18.Vogels SC, Emmelot-Vonk MH, Verhaar HJ, Koek HL. The association of chronic kidney disease with brain lesions on MRI or CT: a systematic review. Maturitas. 2012;71:331–6. doi: 10.1016/j.maturitas.2012.01.008. [DOI] [PubMed] [Google Scholar]
- ▲ 19.Drew DA, Bhadelia R, Tighiouart H, et al. Anatomic brain disease in hemodialysis patients: a cross-sectional study. Am J Kidney Dis. 2013;61:271–8. doi: 10.1053/j.ajkd.2012.08.035. Cross-sectional hemodialysis cohort with healthy controls that showed a high prevalence of brain atrophy, white matter disease and silent infarcts in otherwise healthy hemodialysis patients.
- 20.Kim CD, Lee HJ, Kim DJ, et al. High prevalence of leukoaraiosis in cerebral magnetic resonance images of patients on peritoneal dialysis. Am J Kidney Dis. 2007;50:98–107. doi: 10.1053/j.ajkd.2007.03.019. [DOI] [PubMed] [Google Scholar]
- 21.Hallan SI, Matsushita K, Sang Y, et al. Age and association of kidney measures with mortality and end-stage renal disease. JAMA. 2012;308:2349–60. doi: 10.1001/jama.2012.16817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sajjad I, Grodstein F, Kang JH, Curhan GC, Lin J. Kidney dysfunction and cognitive decline in women. Clin J Am Soc Nephrol. 2012;7:437–43. doi: 10.2215/CJN.05330611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ▲ 23.Davey A, Elias MF, Robbins MA, Seliger SL, Dore GA. Decline in renal functioning is associated with longitudinal decline in global cognitive functioning, abstract reasoning and verbal memory. Nephrol Dial Transplant. 2013;28:1810–9. doi: 10.1093/ndt/gfs470. General population study demonstrating that greater declines in eGFR over 5 years were correlated with greater declines in cognitive performance over that same time period
- ▲▲ 24.Barzilay JI, Lovato JF, Murray AM, et al. Albuminuria and cognitive decline in people with diabetes and normal renal function. Clin J Am Soc Nephrol. 2013;8:1907–14. doi: 10.2215/CJN.11321112. Post hoc analysis of the ACCORD clinical trial of blood pressure and glycemic control in diabetes that showed an association between albuminuria and cognitive decline in participants with preserved kidney function.
- ▲ 25.Haring B, Leng X, Robinson J, et al. Cardiovascular Disease and Cognitive Decline in Postmenopausal Women: Results From the Women’s Health Initiative Memory Study. J Am Heart Assoc. 2013;2:e000369. doi: 10.1161/JAHA.113.000369. Prospective follow-up of 6455 cognitively intact, postmenopausal women aged 65 to 79 years old enrolled in the Women’s Health Initiative Memory Study which demonstrated that prevalent cardiovascular disease, hypertension and diabetes were associated with cognitive decline.
- ▲▲ 26.Yaffe K, Ackerson L, Hoang TD, et al. Retinopathy and cognitive impairment in adults with CKD. Am J Kidney Dis. 2013;61:219–27. doi: 10.1053/j.ajkd.2012.10.006. Post-hoc analysis of CRIC demonstating an association between the presence microvascular disease defined by retinopathy and worse executive functioning in people with advanced CKD, suggesting that small vessel cerebrovascular disease may be a causative factor for the high prevalence of coognitive impairment in people with CKD.
- 27.Seliger SL, Weiner DE. Cognitive impairment in dialysis patients: focus on the blood vessels? Am J Kidney Dis. 2013;61:187–90. doi: 10.1053/j.ajkd.2012.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ▲▲ 28.Kurella Tamura M, Unruh ML, Nissenson AR, et al. Effect of more frequent hemodialysis on cognitive function in the frequent hemodialysis network trials. Am J Kidney Dis. 2013;61:228–37. doi: 10.1053/j.ajkd.2012.09.009. Post hoc analysis of the FHN revelaing that there was no difference in cognitive performance asscoaied with more frequent dialysis. This suggests that, in an era where sunstantial small solute clearance is universal in hemodialysis patients, uremic solutes are not the cause of cognitive impairment.
- 29.Launer LJ, Hughes T, Yu B, et al. Lowering midlife levels of systolic blood pressure as a public health strategy to reduce late-life dementia: perspective from the Honolulu Heart Program/Honolulu Asia Aging Study. Hypertension. 2010;55:1352–9. doi: 10.1161/HYPERTENSIONAHA.109.147389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ninomiya T, Ohara T, Hirakawa Y, et al. Midlife and late-life blood pressure and dementia in Japanese elderly: the Hisayama study. Hypertension. 2011;58:22–8. doi: 10.1161/HYPERTENSIONAHA.110.163055. [DOI] [PubMed] [Google Scholar]
- 31.Forette F, Seux ML, Staessen JA, et al. The prevention of dementia with antihypertensive treatment: new evidence from the Systolic Hypertension in Europe (Syst-Eur) study. Arch Intern Med. 2002;162:2046–52. doi: 10.1001/archinte.162.18.2046. [DOI] [PubMed] [Google Scholar]
- 32.Launer LJ, Miller ME, Williamson JD, et al. Effects of intensive glucose lowering on brain structure and function in people with type 2 diabetes (ACCORD MIND): a randomised open-label substudy. Lancet Neurol. 2011;10:969–77. doi: 10.1016/S1474-4422(11)70188-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ▲ 33.Kang EW, Abdel-Kader K, Yabes J, Glover K, Unruh M. Association of sleep-disordered breathing with cognitive dysfunction in CKD stages 4-5. Am J Kidney Dis. 2012;60:949–58. doi: 10.1053/j.ajkd.2012.08.033. In a cohort of 169 patients with CKD stages 4-5, sleep-disordered breathing was associated with cognitive impairment, particularly in older participants.
- 34.Heiwe S, Jacobson SH. Exercise training for adults with chronic kidney disease. Cochrane Database Syst Rev. 2011:CD003236. doi: 10.1002/14651858.CD003236.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- ▲ 35.Matsuzawa R, Matsunaga A, Wang G, et al. Habitual physical activity measured by accelerometer and survival in maintenance hemodialysis patients. Clin J Am Soc Nephrol. 2012;7:2010–6. doi: 10.2215/CJN.03660412. Among a population of 202 maintenance hemodialysis patients in Japan, those engaging in regular physical activity had lower risk of death.
- ▲ 36.Robinson-Cohen C, Littman AJ, Duncan GE, et al. Physical Activity and Change in Estimated GFR among Persons with CKD. J Am Soc Nephrol. 2013 doi: 10.1681/ASN.2013040392. [epub ahead of print] Among 256 participants in the Seattle Kidney Study cohort, those who engaged in more physical activity had a small but significantly slower decline in eGFR.
- ▲▲ 37.Howden EJ, Leano R, Petchey W, Coombes JS, Isbel NM, Marwick TH. Effects of exercise and lifestyle intervention on cardiovascular function in CKD. Clin J Am Soc Nephrol. 2013;8:1494–501. doi: 10.2215/CJN.10141012. Parallel-group randomized clinical trial indicating modest but significant improvements in cardiorespiratory fitness after 12 months of structured exercise training in stage 3-4 CKD, suggesting that the diminished fitness in non-dialysis CKD patients can be at least partially reversed with exercise training.
- ▲ 38.Roshanravan B, Robinson-Cohen C, Patel KV, et al. Association between physical performance and all-cause mortality in CKD. J Am Soc Nephrol. 2013;24:822–30. doi: 10.1681/ASN.2012070702. Among 385 ambulatory, stroke-free participants with stage 2-4 CKD enrolled in clinic-based cohorts at the University of Washington and University of Maryland and Veterans Affairs Maryland Healthcare systems, slower gait speed and worse performance on the timed get-up-and-go test were associated with higher risk of death.
- ▲▲ 39.Liu CK, Lyass A, Massaro JM, D’Agostino RB, Sr., Fox CS, Murabito JM. Chronic Kidney Disease Defined by Cystatin C Predicts Mobility Disability and Changes in Gait Speed: The Framingham Offspring Study. J Gerontol A Biol Sci Med Sci. 2013 doi: 10.1093/gerona/glt096. Longitudinal cohort study of middle-aged and older adults indicating a greater risk of incident walking disability and greater declines in gait speed associated with CKD. One of the few longitudinal studies to examine the relationship between CKD and physical performance, suggesting that older adults with CKD should be considered an at-risk group for walking disability.
- ▲ 40.Bao Y, Dalrymple L, Chertow GM, Kaysen GA, Johansen KL. Frailty, dialysis initiation, and mortality in end-stage renal disease. Arch Intern Med. 2012;172:1071–7. doi: 10.1001/archinternmed.2012.3020. Frailty, present among 73% of incident hemodialysis patients, is more common among those intiating dialysis at higher eGFR levels and is independently associated with mortality and time to first hospitalization.
- ▲▲ 41.Roshanravan B, Khatri M, Robinson-Cohen C, et al. A prospective study of frailty in nephrology-referred patients with CKD. Am J Kidney Dis. 2012;60:912–21. doi: 10.1053/j.ajkd.2012.05.017. Prospective study indicating a direct relationship between CKD severity and frailty, and identifying frailty in CKD as an independent risk marker for mortality. This study also suggests that frailty in CKD is associated more strongly with markers of obesity and adiposity rather than underweight or weight loss.
- ▲ 42.Reese PP, Cappola AR, Shults J, et al. Physical performance and frailty in chronic kidney disease. Am J Nephrol. 2013;38:307–15. doi: 10.1159/000355568. Among 1,111 participants in CRIC, in cross-sectional analyses lower eGFR was associated with poor physical performance and frailty in a graded fashion.