Abstract
Objective
This study aimed to evaluate the roles of self-esteem and overvaluation of shape and weight in accounting for the internalization of weight bias among patients with binge eating disorder (BED) and obesity.
Method
Two hundred forty-five treatment-seeking individuals with BED and obesity were evaluated with diagnostic and semi-structured interviews and completed the Weight Bias Internalization Scale (WBIS) and the Rosenberg Self-Esteem Scale (RSE). Correlations and bootstrapping mediation analyses were computed to evaluate the relationships among self-esteem, overvaluation of shape/weight, and weight bias internalization. The effects of body mass index (BMI) and binge-eating frequency were also tested.
Results
Significant correlations emerged between WBIS, RSE, and overvaluation of shape and weight. BMI did not correlate with any measure, and binge-eating frequency only correlated with overvaluation. Mediation analyses provided support for the hypothesis that overvaluation of shape and weight mediates the relationship between self-esteem and weight bias internalization.
Discussion
These findings provide support to the proposed model that self-esteem and overvaluation of shape and weight contribute to weight bias internalization among patients with BED, which holds implications for clinical efforts to address weight bias and associated eating and weight-related psychopathology.
Keywords: Weight bias internalization, Overvaluation of Shape/Weight, Self-esteem, Binge eating disorder
1. Introduction
Weight-biased attitudes and resulting weight-stigmatization are prevalent in all domains of society (Puhl & Heuer, 2009), and individuals with obesity who internalize this bias apply negative stereotypes to themselves and base their self-evaluation on these stigmatizing attitudes (Durso & Latner, 2008). Weight bias internalization among individuals with obesity is associated with a host of negative mental and physical health outcomes such as low self-esteem, weight and shape concerns, body dissatisfaction, and unhealthy eating behaviors including binge eating (Durso & Latner, 2008; Roberto et al., 2012; Schvey, Roberto, & White, 2013). Indeed, weight bias internalization has been found to be high among patients with binge eating disorder (BED; Durso et al., 2012) and has been linked to poor global health functioning among these individuals (Hilbert, Braehler, Haeuser, & Zenger, 2014; Pearl, White, & Grilo, 2014).
Despite consistent evidence of links between weight bias internalization and negative health consequences, little is known about how to predict which individuals with obesity are most prone to internalizing weight bias. Except for one study demonstrating that perceived discrimination correlates with weight bias internalization (Durso, Latner, & Hayaski, 2012), we are unaware of research focused on identifying pathways that may increase vulnerability to weight bias internalization. Such knowledge could inform clinical interventions aimed at preventing and alleviating negative mental and physical health outcomes that may stem from this internalization.
In light of existing evidence of associations between weight bias internalization and eating pathology, including symptoms of BED, consideration of cognitive factors that facilitate the development of eating disorders may represent a promising starting-point for identifying risk factors for weight bias internalization. One such factor tied to eating pathology and relevant to weight-biased attitudes is overvaluation of shape and weight, or undue influence of shape and weight on one’s self-evaluation (Fairburn, 2008). Overvaluation of shape and weight is distinct from weight bias internalization, which involves applying negative weight stereotypes to oneself. Overvaluation is thought to reflect a core feature of eating disorders and is a diagnostic criterion for anorexia nervosa and bulimia nervosa (Fairburn, 2008; Grilo, 2013). Although overvaluation of shape and weight is not a feature of the DSM-5 diagnosis of BED, empirical research has found that it does not merely reflect concern with excess weight, and that it is reliably associated with greater severity of eating disorder psychopathology and distress (Grilo, 2013; Grilo et al., 2008) and with poorer treatment outcomes (Grilo, Masheb, & Crosby, 2012).
In Fairburn and colleagues’ (2003) transdiagnostic model, it is proposed that overall low self-esteem increases risk for overvaluation of shape and weight, which in turn leads to unhealthy weight-control practices that may subsequently lead to eating-related psychopathology including binge-eating. We propose that this model could also help account for understanding weight bias internalization among individuals with obesity and BED. Specifically, we hypothesize that individuals who evaluate themselves based on shape and weight may also be more vulnerable to applying negative weight stereotypes to themselves, thus exhibiting internalized weight bias.
The current study aimed to evaluate the roles of self-esteem and overvaluation of shape and weight in the internalization of weight bias among patients with BED. Consistent with Fairburn and colleagues’ (2003) theory that overvaluation of shape and weight mediates the relationship between low self-esteem and eating pathology, we predicted that overvaluation would mediate the relationship between self-esteem and weight bias internalization.
2. Materials and Methods
Participants were 245 treatment-seeking adults with obesity who met DSM-5 diagnostic criteria for BED (73 men, 172 women; 80.8% White; age range 18-65, M = 48.00, SD = 9.89). Participants were recruited via newspaper advertisements to participate in a treatment research study for binge eating and obesity at a medical school-based specialty clinic. All data were collected at baseline, prior to any treatment intervention.
Doctoral-level clinicians conducted diagnostic interviews (First, Spitzer, Gibbon, & Williams, 2002) to establish the BED diagnosis and administered the Eating Disorder Examination interview (EDE; Cooper & Fairburn, 1987) to assess binge-eating frequency and overvaluation of shape and weight. The diagnostic interview (based on criteria from DSM-IV-TR) and the EDE interview were modified by the investigators to determine the specific DSM-5 criteria for BED. Body mass index (BMI) was calculated by measuring participants’ height and weight with a high capacity digital scale. Participants completed the Weight Bias Internalization Scale (WBIS) and the Rosenberg Self-esteem Scale (RSE). The WBIS contains 11 items rated on a seven-point scale (Durso & Latner, 2008) and demonstrated strong reliability in the current sample (α = .85). The RSE is a well-established measure computed by summing 10 items rated on a four-point scale, with higher scores signifying higher self-esteem (Rosenberg, 1979), α =. 91. The EDE interview (Cooper & Fairburn, 1987), a well-established investigator-based interview with demonstrated reliability (Grilo, Masheb, Lozano-Blanco, & Barry, 2004), assesses the extent to which shape and weight influence participants’ self-evaluations on a 7-point forced-choice format (0 to 6), with higher scores reflecting greater severity. Consistent with prior research (Grilo et al., 2008), the respective shape and weight overvaluation questions were asked separately and the mean score was used in analyses (item correlation r = .83, p < .001).
2.1 Analytic Plan
We first tested for correlations between WBIS, RSE, and overvaluation scores, along with BMI and binge-eating frequency (as a measure of symptom severity). Bootstrapping mediation analyses recommended by Preacher and Hayes (2008) were then conducted to test the hypothesis that overvaluation of shape and weight mediates the relationship between self-esteem and weight bias internalization. Direct and indirect effects were calculated with the SPSS macro provided by Preacher and Hayes (2008), based on 5,000 bootstrap samples and a 95% confidence interval. Analyses were conducted with and without BMI included as a covariate; due to lack of significant differences in the findings, only the results without BMI in the model are presented.
3. Results
All participants had BMIs of 30 or above, with a mean BMI of 39.49 (SD = 5.92). Participants reported an average of 19.66 (SD = 15.04) objective binge episodes in the past month. Mean WBIS score was 4.64 (SD = 1.22), mean RSE score was 29.52 (SD = 6.20), and mean overvaluation score was 3.74 (SD = 1.77).
BMI did not correlate significantly with any measure, and while binge-eating frequency significantly correlated with overvaluation scores, r(243) = .16, p = .011, it did not significantly correlate with RSE or WBIS scores. Analysis of variance revealed significant gender differences for WBIS and RSE scores but not for overvaluation scores (see Table 1).
Table 1.
Analysis of variance results: Gender differences in study measures.
| F Value | Mean Score for Women (Standard Deviation) |
Mean Score for Men (Standard Deviation) |
|
|---|---|---|---|
| Weight Bias Internalization Scale | 8.77** | 4.79 (1.20) | 4.29 (1.22) |
| Rosenberg Self-Esteem Scale | 4.97* | 28.95 (6.19) | 30.86 (6.05) |
| Overvaluation of Shape and Weight | 2.79 | 3.86 (1.75) | 3.45 (1.78) |
Note. N = 245
p < .05
p < .01
WBIS scores correlated significantly with RSE scores, r(243) = −.67, p < .001, and overvaluation, r(243) = .54, p < .001. RSE and overvaluation scores were also significantly correlated, r(243) = −.43, p < .001. Due to the aforementioned gender differences, correlations were calculated for men and women separately as well, and all correlations remained consistent across gender.
3.1 Mediation Analyses
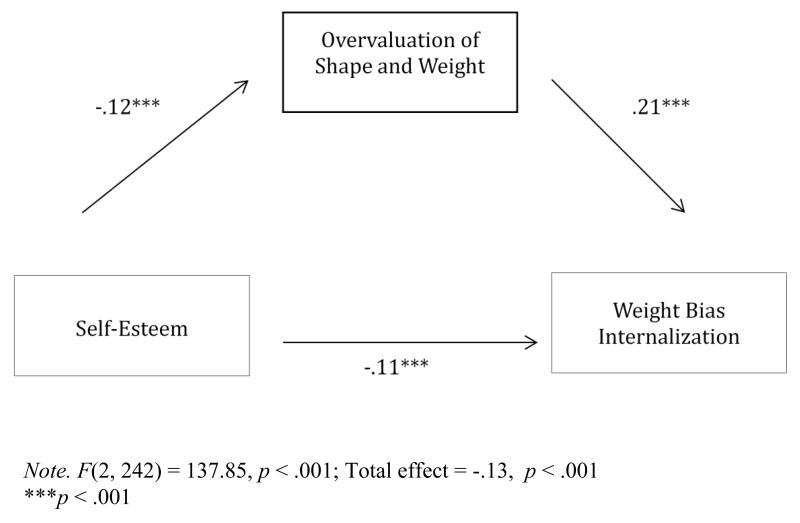
Results from bootstrap analysis supported the hypothesis that overvaluation of shape and weight mediates the relationship between self-esteem and weight bias internalization (see Figure 1). Results revealed that the 95% percent bias-corrected confidence interval for the size of the indirect effects excluded zero, indicating mediation (Preacher & Hayes, 2008); [−.04, −.02], model R2 = .53. Mediation models were constructed for men and women separately as well, and results remained consistent across gender.
Figure 1.
Mediation model of self-esteem, overvaluation of shape and weight, and weight bias internalization. Unstandardized coefficients are provided. Overvaluation of shape and weight mediates the relationship between self-esteem and weight bias internalization.
4. Discussion
The findings from this study provide evidence in support of the hypothesis that self-esteem and overvaluation of shape and weight play a role in the internalization of weight bias among binge eating disorder patients with obesity. Consistent with Fairburn and colleagues’ (2003) transdiagnostic eating disorder model, mediation analysis results suggest that low self-esteem may contribute to the internalization of weight bias through the process of basing one’s self-evaluation strongly in shape and weight. Although there was not a significant association between weight bias internalization and binge-eating frequency, this could be due to the restricted range and overall high level of symptom severity in this sample. Thus, future research could investigate these effects in a non-treatment seeking sample in order to test whether this model can be used to predict binge-eating pathology. Furthermore, given evidence that individuals who are not obese (such as underweight patients with eating disorders) may also internalize weight bias (Pearl & Puhl, 2014), it may be informative to determine if this proposed model predicts other eating pathology apart from binge-eating.
The cross-sectional nature of this study precludes conclusions about causality, and prospective longitudinal research is needed to establish the developmental course of weight bias internalization with respect to eating disorder features across different weight categories. The gender differences observed in the current research also warrant further investigation; although correlations and mediation results remained consistent across gender, future work could explore whether interventions challenging overvaluation or weight bias internalization operate differently depending on patient gender.
This study was the first to propose and test a theory accounting for the internalization of weight bias among patients with BED, which carries implications for clinical interventions. For example, cognitive techniques focusing on overvaluation, as suggested by Fairburn and colleagues (2009), may additionally prevent the incorporation of negative weight stereotypes into patients’ self-evaluations. Continuing to advance understanding of the processes that lead to weight bias internalization will be crucial to adapting current treatment strategies to reduce internalization and its associated negative health consequences.
Highlights.
We evaluated treatment-seeking individuals with binge eating disorder and obesity.
Weight bias internalization (WBI) and self-esteem were correlated.
Overvaluation of shape/weight mediated the relationship between self-esteem and WBI.
Acknowledgments
Statement 1: Role of Funding Sources
This study was funded by a grant from the National Institutes of Health (3R01 DK49587). Dr. Grilo was also supported, in part, by 2K24 DK070052. These sources of funding had no role in this specific study design, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Statement 2: Contributors
Author A was involved in the design of this specific study, the planning and execution of the data analysis and interpretation, and held primary responsibility for writing the manuscript. Authors B and C were involved in the design of the study, acquisition of the data and creation of the database, editing of drafts of the manuscript, and approval of the final manuscript.
Statement 3: Conflict of Interest
The authors have no conflict of interest to disclose.
References
- Cooper Z, Fairburn C. The eating disorder examination: A semi-structured interview for the assessment of the specific psychopathology of eating disorders. International Journal of Eating Disorders. 1987;6(1):1–8. [Google Scholar]
- Durso LE, Latner JD. Understanding Self-directed Stigma: Development of the Weight Bias Internalization Scale. Obesity. 2008;16(S2):S80–S86. doi: 10.1038/oby.2008.448. [DOI] [PubMed] [Google Scholar]
- Durso LE, Latner JD, Hayaski K. Perceived Discrimination is Associated with Binge Eating in a Community Sample of Non-Overweight, Overweight, and Obese Adults. Obesity Facts. 2012;5:869–880. doi: 10.1159/000345931. [DOI] [PubMed] [Google Scholar]
- Durso LE, Latner JD, White MA, Masheb RM, Blomquist KK, Morgan PT, Grilo CM. Internalized Weight Bias in Obese Patients with Binge Eating Disorder: Associations with Eating Disturbances and Psychological Functioning. International Journal of Eating Disorders. 2012;45(3):423–427. doi: 10.1002/eat.20933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG. Eating disorders: The transdiagnostic view and the cognitive behavioral theory. In: Fairburn CG, editor. Cognitive Behavior Therapy and Eating Diosrders. The Guilford Press; New York: 2008. pp. 7–22. [Google Scholar]
- Fairburn CG, Cooper Z, Doll HA, O’Connor ME, Bohn K, Hawker DM, Palmer RL. Transdiagnostic Cognitive-Behavioral Therapy for Patients with Eating Disorders: A Two-Site Trial With 60-Week Follow-up. American Journal of Psychiatry. 2009;166(3):311–319. doi: 10.1176/appi.ajp.2008.08040608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z, Shafran R. Cognitive behavior therapy for eating disorders: A “transdiagnostic” theory. Behavior Research and Therapy. 2003;41(5):509–528. doi: 10.1016/s0005-7967(02)00088-8. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P) Biometrics Resarch, New York State Psychiatric Institute; New York: 2002. [Google Scholar]
- Grilo CM. Why no cognitive body image feature such as overvaluation of shape/weight in the binge eating disorder diagnosis? International Journal of Eating Disorders. 2013;46(3):208–211. doi: 10.1002/eat.22082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Hrabosky JI, White MA, Allison KC, Stunkard AJ, Masheb RM. Overvaluation of Shape and Weight in Binge Eating Disorder and Overweight Controls: Refinement of a Diagnostic Construct. Journal of Abnormal Psychology. 2008;117(2):414–419. doi: 10.1037/0021-843X.117.2.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Crosby RD. Predictors and moderators of response to cognitive behavioral therapy an dmedication for the treatment of binge eating disorder. Journal of Consulting and Clinical Psychology. 2012;80:186–195. doi: 10.1037/a0027001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grilo CM, Masheb RM, Lozano-Blanco C, Barry DT. Reliability of the Eating Disorder Examination in patients with binge eating disorder. International Journal of Eating Disorders. 2004;35:80–85. doi: 10.1002/eat.10238. [DOI] [PubMed] [Google Scholar]
- Hilbert A, Braehler E, Haeuser W, Zenger M. Weight bias internalization, core self-evaluation, and health in overweight and obese persons. Obesity. 2014;22(1):79–85. doi: 10.1002/oby.20561. [DOI] [PubMed] [Google Scholar]
- Pearl RL, Puhl RM. Measuring internalized weight attitudes across body weight categories: Validation of the Modified Weight Bias Internalization Scale. Body Image. 2014;11(1):89–92. doi: 10.1016/j.bodyim.2013.09.005. [DOI] [PubMed] [Google Scholar]
- Pearl RL, White MA, Grilo CM. Weight bias internalization, depression, and self-reported health among overweight binge eating disorder patients. Obesity. 2014;22(5):E142–E148. doi: 10.1002/oby.20617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. The Stigma of Obesity: A Review and Update. Obesity. 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Roberto CA, Sysko R, Bush J, Pearl R, Puhl RM, Schvey NA, Dovidio JF. Clinical correlatees of the weight bias internalization scale in a sample of obese adolescents seeking bariatric surgery. Obesity. 2012;20(3):533–539. doi: 10.1038/oby.2011.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M. Conceiving the Self. Basic Books; New York: 1979. [Google Scholar]
- Schvey NA, Roberto CA, White MA. Clinical correlates of the Weight Bias Internalization Scale in overweight adults with binge and purge behaviours. Advances in Eating Disorders: Theory, Research, and Practice. in press. Advance online publication. doi: 10.1080/21662630.2013.794523. [Google Scholar]