Abstract
Barriers to HIV testing and HIV care and treatment pose significant challenges to HIV prevention among men who have sex with men (MSM) in China. We carried out a qualitative study to identify barriers and facilitators to HIV testing and treatment among Chinese MSM. In 2012, 7 focus group discussions were conducted with 49 MSM participants in Nanjing, China. Purposive sampling was used to recruit a diverse group of MSM participants. Semi-structured interviews were conducted to collect FG data. Major barriers to testing included gay- and HIV-related stigma and discrimination, relationship type and partner characteristics, low perception of risk or threat, HIV is incurable or equals death, concerns of confidentiality, unaware that testing is offered for free, and name-based testing. Key facilitators of testing included engaging in high-risk sex, sense of responsibility for partner, collectivism, testing as a part of standard/routine medical care, MSM-friendly medical personnel, increased acceptance of gay/bisexual men by the general public, legal recognition and protection of homosexuals, and home self-testing. Barriers to treatment included negative coping, non-disclosure to families, misconceptions of domestically produced antiretroviral drugs and the benefits of treatment, and costs associated with long-term treatment. Facilitators of treatment included sense of hopefulness that a cure would be found, the cultural value of longevity, peer social support and professional psychological counseling, affordable and specialized treatment and care, and reduced HIV-related stigma and discrimination. Finally, for both testing and treatment, more educational and promotional activities within MSM communities and among the general public are needed.
Keywords: men who have sex with men, HIV, test and treat, stigma, China
Introduction
Empirical studies and modeling exercises of HIV testing and treatment have demonstrated the effectiveness of universal HIV testing and early treatment in preventing sexual transmission of HIV, lowering community viral load, and consequently reducing HIV incidence among high-risk populations such as men who have sex with men (MSM) and general populations in both concentrated and generalized epidemic settings (Cohen et al., 2011; Das et al., 2010; Granich, Gilks, Dye, DeCock, & Williams, 2009; Sorensen et al. 2012). To achieve such benefits, a cascade of linked services and strategies are needed to increase HIV testing uptake among at-risk populations, improve linkage to care among those diagnosed with HIV, initiate early treatment among HIV-positive individuals, and improve retention in care and adherence to treatment. However, in many countries and especially among stigmatized populations, unique individual, social, cultural, and structural barriers to HIV testing and access to care and treatment pose significant challenges to this cascade.
MSM in China are becoming the group most highly affected by HIV/AIDS (China Ministry of Health, 2010; H. Li et al. 2011; Zhang et al. 2012). Although an increase in HIV testing has been observed among Chinese MSM over the past decade, testing uptake is still far from optimal (Chow, Wilson, & Zhang, 2012). A meta-analysis reported that the rate of HIV testing in the past year among MSM was just 38% after the national HIV/AIDS plan called for the scale up of HIV testing services for MSM (21% prior to the scale-up) (Zhou, Hu, Xin, & Beck, 2012). A recent study also found that 86% of MSM who were HIV-positive were unaware of their infection (X. Li et al. 2011). Few data exist regarding access to HIV treatment and care among Chinese MSM and those that do exist suggest less than promising findings. A study of HIV-positive MSM in Jiangsu province found that only 33% of HIV -positive MSM were retained in care for 3 consecutive years, and compared to other high-risk groups HIV-positive MSM had faster disease progression and slower increase in CD4 counts over the course of treatment (Yan et al. 2013). These findings suggest that there may be barriers to care and treatment among Chinese MSM.
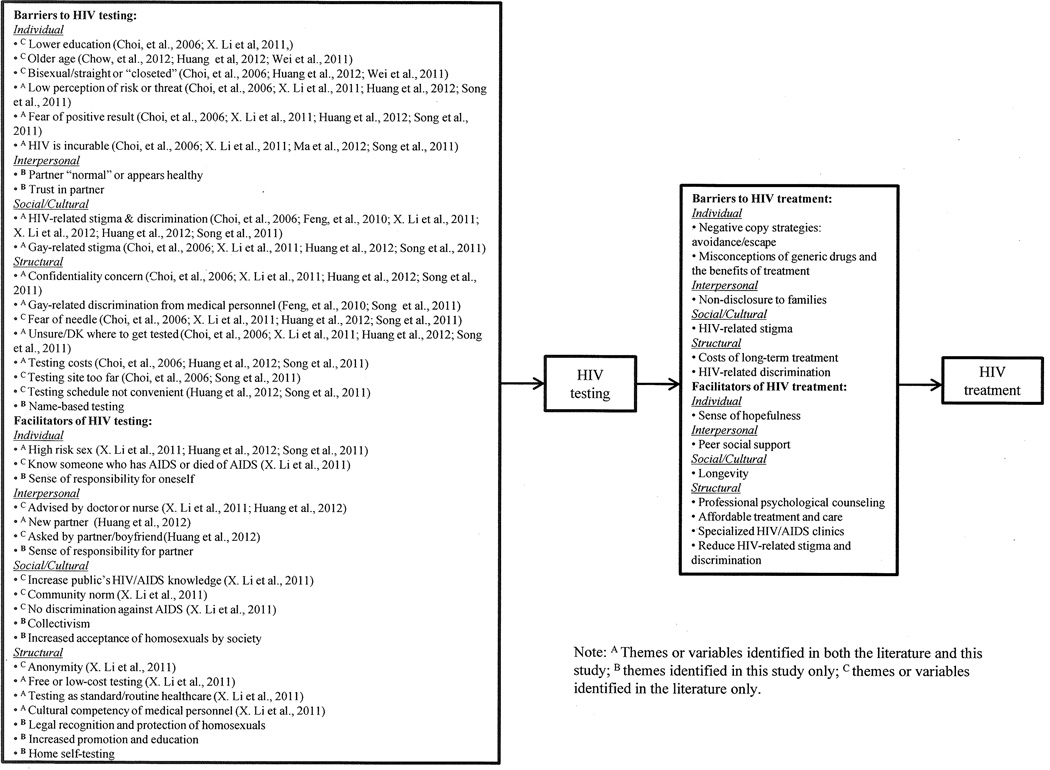
Understanding and identifying barriers and facilitators to HIV testing and treatment are critical to interventions designed to increase HIV status awareness, HIV diagnosis, access to care and treatment, improvements in health status among those HIV-infected, and subsequent viral load suppression. We carried out a qualitative study to explore barriers and facilitators to HIV testing and treatment among Chinese MSM. We also summarized the main findings from published studies of HIV testing among Chinese MSM in Figure 1 using the Ecological Model as an organizing framework (Glanz, Rimer, & Lewis, 2002). We described in detail new themes found in our study. This was one of the few studies on HIV testing behaviors among Chinese MSM and was the first to explore barriers and facilitators to treatment and care among this population in China.
Figure 1.
Barriers and facilitator to HIV testing and treatment among men who have sex with men in China
Methods
Between February and March 2012, 7 focus group (FG) discussions (6–8 participants in each group) were conducted with 49 MSM in Nanjing, China. Purposive sampling was used to recruit a diverse group of MSM participants (Table 1 presents socio-demographic characteristics of participants). Five FGs consisted of mostly younger and gay-identified participants while the other 2 FGs consisted of primarily older and bisexual-identified participants. Participants were recruited through referrals from a local community-based organization and 2 voluntary counseling and testing (VCT) sites, and peer referrals. To be eligible, participants had to be male, 18 years old or older, a resident of Nanjing, and have had sex with another male in the past 12 months. Participation in the study was anonymous and voluntary. Written informed consent was obtained from all participants. An incentive of 100RMB (~16USD) was offered to compensate for participants’ time and effort.
Table 1.
Socio-demographic characteristics of MSM participants (N = 49), Nanjing, China.
| N (%) | |
|---|---|
| Age: Mean/Range (SD) | 31.3/18 – 63 (10.6) |
| Recruitment source | |
| CBO | 20 (40.8%) |
| VCT sites | 18 (36.7%) |
| Peer referral | 11 (22.5%) |
| Marital status | |
| Single | 38 (77.5%) |
| Married/divorced | 11 (22.5%) |
| Hukou | |
| Nanjing | 26 (53.1%) |
| Jiangsu Province | 11 (22.4%) |
| Other | 12 (24.5%) |
| Education | |
| Middle school or lower | 5 (10.2%) |
| High school | 10 (20.4%) |
| Some college | 6 (12.2%) |
| College or above | 28 (57.1%) |
| Employment | |
| Full-time | 30 (61.2%) |
| Part-time | 6 (12.2%) |
| Student | 11 (22.4%) |
| Unemployed/retired | 2 (4.1%) |
| Have a steady male (sex) partner Sexual orientation | 32 (65.3%) |
| Gay | 40 (81.6%) |
| Bisexual/unsure | 9 (18.4%) |
| Ever tested for HIV | 42 (85.7%) |
Semi-structured interviews, which lasted between 1.5 to 2 hours and were facilitated by the Principal Investigator (PI), were conducted to collect FG data. The Ecological Model and the Health Belief Model were used to guide the development of the interview guide (Glanz et al., 2002). Interview questions were structured into several major domains: 1) perceived risk and threat of HIV and its impact; 2) homophobia and gay-related discrimination; 3) reasons for obtaining or not obtaining an HIV test; 4) strategies to encourage testing; 5) barriers to treatment and care if tested HIV-positive; 6) types of services needed for HIV-positive individuals. The interviews were audio-taped and transcribed verbatim in Chinese. Two coders independently coded the data under the categories of barriers and facilitators to testing and treatment. These initial codes were then reviewed and recoded into major themes for each category. The PI and a bilingual research assistant performed translation and back-translation. The study was approved by the University of Pittsburgh and Jiangsu Provincial CDC’s Institutional Review Boards.
Results
Barriers to HIV Testing
Major barriers documented in the literature were also identified by FG participants: 1) Gay-related stigma and discrimination; 2) HIV-related stigma and discrimination; 3) low perception of risk or threat; 4) fear of being tested positive; 5) HIV is incurable or equals death; 6) concerns of confidentiality; 7) unsure or don’t know where to get tested; and 8) costs of testing or unaware that testing is offered free. FG participants identified the following additional barriers:
Partner and relationship characteristics
Relationship type and partner characteristics appeared to affect participants’ decision-making. Some participants said they did not seek (routine) testing because they were in a long-term relationship or because they and their partner trusted each other. Participants said that their emotional connection to a partner would affect their decision about testing with that partner (i.e., testing was a denial of the emotional bond that they held with their partner). As one participant put it:
“If you trust the other person completely, or the other person also trusts you, then getting tested is just a matter of formality. If you don’t trust him, even if he doesn’t have the disease, you will still think that he may have it. If you do trust him, it doesn’t matter even if he’s not tested. Right?”
Some also based their decisions on sexual partners’ appearances or behaviors. If a potential partner appeared to have a higher socio-economic status (e.g., college-educated or well-dressed), then he was believed to be non-promiscuous. One participant said:
“By looking at his clothes and other aspects of him, he doesn’t seem to be a promiscuous person. You can really tell by just looking.”
Name-based testing
Participants’ reaction to the implementation of name-based testing in Guangxi Zhuang Autonomous Region was overwhelmingly negative. Because of gay-related stigma and concerns of confidentiality, almost all participants said they definitely would not seek testing if this policy was implemented in their province.
Facilitators of HIV Testing
Some common facilitators that were documented in the literature and identified by FG participants include: 1) Engaging in high-risk sex; 2) having a new partner; 3) free or low-cost testing; 4) normalizing HIV testing by implementing as it a part of standard/routine medical care; 5) MSM-friendly and culturally competent medical personnel. FG participants identified other facilitators:
Sense of responsibility for oneself and one’s partner
Among participants who tested at least annually, they said that they were being health conscious because condoms do not provide 100% protection, and that knowing one’s HIV status was being responsible for oneself and others. This sense of responsibility for others came from participants’ intentions to protect their partners and to show respect for each other. In response to being asked why he got tested annually, a participant said:
“I’m afraid to infect my friend. I think the purpose of testing is to control, to end it with you, so you don’t pass it on to others. This is a virus. You never know who could catch it, or when you could have it. Getting tested is being responsible for others as well as for yourself. It’s best to get tested when you are uncertain.”
Collectivism
The decision-making process of obtaining an HIV test appeared to be related to a collective culture in China. Rather than going alone, some participants had their first testing experience with close friends. This group-based behavior could be a strategy that these men employ to cope with stress and deal with stigma. One participant remembered:
“Five or six years ago, I heard about it [HIV testing] for the first time because I was a member in a very large online group, about 400 members in it. Then they said there was testing, so several of us went together because we were close friends. I was too embarrassed to go at the very beginning, but I wanted to, so I asked them and 3 or 5 of us went together.”
Increased promotion and education
Participants complained that there has been very limited education on HIV/AIDS. Some said they only saw this type of education once a year on World AIDS Day. Furthermore, they felt that the existing education was non-specific to MSM, superficial, and did not resonate with them. They suggested that more educational and promotional activities, specifically prioritizing MSM populations, are needed.
“If I see HIV-related education more often I would pay more attention to it, which may encourage me to get tested. This could have a herd effect, maybe everyone will get tested then.”
“Promotion needs to be strengthened. For example, organize some promotion activities at popular [gay] venues. This will raise awareness, then you will go [get tested].”
Increased acceptance of homosexuals by society and legal protection
Participants acknowledged that there has been increased awareness of gay-related issues, however, acceptance of homosexuality was still low. Increased acceptance by society and legal recognition and protection were seen as a potential buffer against the negative effects of stigma. A participant said:
“Actually the reason why many [MSM] don’t get tested is that they would feel embarrassed if their [gay] identity is exposed. So if the society accepts it, and the relationship [between society and gay] isn’t so tense, then I would go get tested. I won’t be afraid because you won’t discriminate against me when I get a test.”
Home self-testing
When asked what would be the ideal testing method, participants universally endorsed self-testing at home. They gave two reasons for their choice: protection of privacy and convenience. At present, HIV self-testing kits are not approved for sale in China, however, one participant reported that he purchased an unauthorized kit from the Internet.
Barriers to HIV Treatment
Negative coping and non-disclosure
Instead of seeking treatment, a majority of younger and college-educated participants said they would move away if they tested positive. They would go travel and enjoy themselves, and try to avoid people in fear of discrimination. Some also said they would choose to leave Nanjing and go live in another city and wait to die. Dealing with a positive status appeared to be extremely difficult, one participant said:
“I’ll go travel, have fun, and try to be happy. Didn’t you hear that it [HIV] disappeared in someone after 16 years?”
In addition to negative coping and avoidance, participants said they would only disclose a positive status to few people such as partners and close friends. They would not disclose it to parents or family members because it would bring shame to the family. One participant summarized these barriers:
“I dare not even think about it. I really think that having AIDS is like a death sentence. If I get it, I will move to another city alone. I also won’t want my parents to know about it, maybe just letting a few good friends know because I think they will still care for me. …then wait to die slowly”
Misconceptions of treatment
Misconceptions regarding antiretroviral drugs (ARVs) produced domestically and the benefits of treatment were prevalent among participants. Reflecting a sense of distrust in the medical care system, participants believed that domestically produced ARVs were inferior to imported ARVs. One participant said:
“From what I know, at present, perhaps many domestically produced ARVs have a lot of bad side effects. So, only taking imported drugs is good for you…”
Some also were not familiar with the benefits of treatment. They believed that one could not live long after having HIV. Since HIV is not a curable disease, treatment might not be necessary or useful. As one participant put it:
“If you have this disease, there’s no cure for it, so just let it be.”
Treatment costs
Most participants were concerned with the high costs associated with long-term treatment, yet few were aware that first-line ARVs were provided free in China. Some felt that it might not be worth it to spend most of their income and savings on ARVs because it could take several more decades to find a cure. One participant said:
“You don’t know when it [cure] will come out, what if it doesn’t for decades? …Unless you can live that long, otherwise, like what he just said, you work really hard for it [paying for ARVs], but at the end you die nonetheless.”
Facilitators of HIV Treatment
Sense of hopefulness
A motivating factor for seeking treatment among some participants was a sense of hopefulness that HIV can be cured someday within their lifetime. They said they would remain optimistic and strong while on treatment, and there is always hope if one can remain in treatment. As one participant put it:
“[I will] definitely seek treatment because I myself believe that this disease can be cured sooner or later…Moreover, I think the possibility of curing it is definitely greater than curing cancer…”
Prolong life
Longevity is recognized as one of the most important fortunes or blessings in Chinese culture. The desire for long life is embodied in many Chinese traditions as well as practices including medicine and health. Thus, a reason for treatment among participants was to prolong life. This participant said:
“[I would] take ARVs. I will be very proactive in terms of treatment, and pay very close attention to it. By that I mean I want to maintain my life, to prolong it.”
Peer social support and professional psychological counseling
Participants thought that communicating with other people living with HIV/AIDS (PLWHA) would be an important source of support. Through such peer support groups, either in-person or online, they could share their treatment experiences and care for each other without being discriminated against. In addition, participants thought professional psychological counseling would also be very helpful. One participant summarized these two points:
“I think it’s very necessary to communicate with other HIV-positive individuals. Everybody get together, just like Friends of Cancer Patients, they encourage each other…. Second, although patients can provide counseling among themselves, they are not professional psychologists. Theirs [counseling] is not as professional as psychologists’. So, both are needed.”
Affordable, specialized, and systematic treatment and care
Participants made a few suggestions regarding the overall treatment and care system. First, related to their concerns with costs of ARVs, participants said free and affordable ARVs should be provided for life and should not be restricted to just first-line ARVs. One participant said:
“I heard from others that ARVs were free now, perhaps. If it’s free, I’m willing to take it.”
Second, more HIV clinics are needed to provide patients with specialized care, where medical personnel have adequate expertise in HIV-related diseases and complications and are non-discriminatory. Third, a system should be implemented that links and coordinates treatment and care activities. This participant said:
“I head this story about an AIDS patient, from our [gay] circle. He already had AIDS, then there was a tumor grown in his waist, it wasn’t a malignant one…because he was HIV-positive, no one hospital was willing to admit him, even in a big city like Guangzhou…they took him to Ditan Hospital in Beijing, an HIV hospital…I think the government or even some international organization should implement a system in China. For example, guarantee drug supply at early stage…then have care organizations like this [Ditan Hospital] at later stage, like a line of services.”
Reduce HIV-related stigma and discrimination
Probably most importantly, participants hoped that society would be more accepting of PLWHA. They suggested that anti-stigma/discrimination campaigns or education should not be limited to slogans, but should describe the disease in an objective manner and create positive images of PLWHA. As one participant put it:
“[Show] interviews or documentaries of PLWHA. Let us know that there are healthy and optimistic HIV-positive individuals around us…. Because sometimes we feel the current education is too far away from us, you say don’t discriminate against AIDS, but where are these people in the advertisements? …The power of role models!”
Discussion
This study explored barriers and facilitators to HIV testing and treatment among MSM in China. Overall, participants were not well aware of the importance of HIV testing, acknowledged that many MSM in the community were not seeking routine testing, and had minimal knowledge of treatment and its benefits. For HIV testing, we identified themes that were consistent with existing literature and some that were new. Gay-related stigma and discrimination were identified as major barriers to HIV testing among Chinese MSM. Most men were reluctant to obtain an HIV test in fear that their gay identity would be exposed, and sometimes they encountered direct discrimination from medical personnel.
Several facilitators identified by participants were to counter such stigma and discrimination. These include implementing HIV testing as a part of standard healthcare, training culturally competent medical personnel, increased acceptance of homosexuals among the public, providing legal recognition and protection of homosexuals, and making home self-testing available. Although it will require long-term cultural and political shifts to reduce gay-related stigma and discrimination in China, some of these facilitators could be transformed into policies or interventions in short-term. In particular, since participants universally endorsed home self-testing, this strategy is likely to increase HIV testing uptake among Chinese MSM. Offering low-cost home self-testing will not only protect MSM’s identity and privacy, but will also resolve transportation and inconvenience issues of traveling to VCT sites during scheduled operating hours. A recent systematic review found that HIV self-testing was highly feasible and acceptable among high-risk populations, including MSM, in different settings (Pai et al., 2013). In addition, this testing method can reach sub-groups of MSM who do not or cannot access facility-based testing, such as non-gay identified and rural MSM. The Chinese collective culture appeared to influence participants’ testing behavior (i.e., testing with close friends in order to cope with gay-related stigma and stress). Within this unique cultural context, group-based testing could be a viable intervention strategy. Such interventions can specifically prioritize young MSM who have never been tested or encourage routine testers to bring their friends for testing.
Trust in partner and decision-making based on partner’s appearance were identified as barriers to testing. While trust is important for building a healthy relationship, trust is also a potential threat considering rising HIV infection rates and low rates of HIV testing among Chinese MSM. Educational campaigns and behavioral interventions should address these misconceptions and incorporate components that emphasizing sense of responsibility for one’s partners, which was identified as a facilitator to HIV testing. Furthermore, couples-based testing could be an effective strategy to encourage testing among those who are in a stable relationship.
In terms of treatment, a major barrier discussed was negative coping methods including avoidance and “escape” among younger men. This could create significant problems for linking newly diagnosed men to care and retaining them in care. Non-disclosure to families could also be a significant barrier to receiving long-term treatment. Chinese families have always played an important role in providing instrumental support to each other, non-disclosure could lead to financial stress among these men as they have to bear all the costs associated with treatment and care. Intensive psychological counseling, identified as a facilitator of treatment by participants, should be in place to help these men develop positive coping strategies and facilitate disclosure. Healthcare providers should also refer newly diagnosed men to peer support groups so that they can receive continued social support. Another major barrier to treatment was misconceptions and lack of knowledge of treatment and ARVs. Post-test counseling could include a brief educational session or provide educational materials to address these misconceptions, emphasizing that domestically produced ARVs are just as effective and of as high quality as imported ARVs and the benefits of early treatment. In addition, since longevity is greatly valued in Chinese culture, education should also emphasize that HIV is a manageable chronic disease and provide a sense of hopefulness for individuals’ future.
A facilitator of treatment identified by participants – affordable, specialized, and systematic treatment and care – will require long-term structural changes. Foremost, the government needs to increase its spending on drug assistance programs. In the long run, this is a cost-effective approach to controlling the HIV epidemic. Specialized HIV treatment and care hospital units, with properly trained and culturally competent medical personnel, should be established in areas where MSM constitutes the largest HIV/AIDS affected group.
This study has several limitations. First, this was an exploratory qualitative study with a convenience sample of MSM participants. Our findings are not generalizable, although participants were diverse in terms of socio-demographic characteristics. Second, we did not ask participants’ HIV status due to the focus group methodology (i.e., asking serostatus would have breached individual’s privacy) and all interview questions related to treatment were asked hypothetically. Thus, findings should be interpreted with caution. Additional qualitative studies with HIV-positive MSM should be conducted and explore issues of access to care, retention in care, and adherence to treatment.
Finally, for both testing and treatment, more educational and promotional activities within MSM communities and among the public are needed. While HIV testing and first-line ARVs are offered for free in China, many of our participants were not aware of this fact. As suggested by participants, promotional activities should be MSM-specific and be conducted at both physical and virtual MSM venues. Anti-HIV stigma campaigns should promote relatable and positive images of PLWHA.
Acknowledgement
This study was funded by a grant from NIH/NIMH (grant number: K99MH093201). We thank Dr. Erin Wilson for providing guidance on the analysis.
Footnotes
There are no conflicts of interest
References
- China Ministry of Health, UNAIDS, World Health Organization. 2009 estimates for the HIV/AIDS epidemic in China. Beijing, China: China Ministry of Health; 2010. [May 31, 2010. Accessed 12 Dec 2010]. http://www.unaids.org.cn/download/2009%20China%20Estimation%20Report-En.pdf. [Google Scholar]
- Choi KH, Lui H, Guo Y, Han L, Mandel JS. Lack of HIV testing and awareness of HIV infection among men who have sex with men, Beijing, China. AIDS Education and Prevention. 2006;18:33–43. doi: 10.1521/aeap.2006.18.1.33. [DOI] [PubMed] [Google Scholar]
- Chow EPF, Wilson DP, Zhang L. The rate of HIV testing is increasing among men who have sex with men in China. HIV Medicine. 2012;13:255–263. doi: 10.1111/j.1468-1293.2011.00974.x. [DOI] [PubMed] [Google Scholar]
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hoseinipour MC, Kumarasamy N HPTN 052 Study Team. Prevention of HIV-1 infection with early antiretroviral therapy. New England Journal of Medicine. 2011;365:493–505. doi: 10.1056/NEJMoa1105243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Das M, Chu PL, Santos G, Scheer S, Vittinghoff E, McFarland W, Colfax GN. Decreases in community viral load are accompanied by reductions in new HIV infections in San Francisco. PLoS One. 2010;5:e11068. doi: 10.1371/journal.pone.0011068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y, Wu Z, Detels R. Evolution of MSM community and experienced stigma among MSM in Chengdu, China. Journal of Acquired Immune Deficiency Syndromes. 2010;53(Suppl 1):S98–S103. doi: 10.1097/QAI.0b013e3181c7df71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Rimer BK, Lewis FM. Health behavior and health education: Theory, research, and practice. 3rd Edition. San Francisco, Calif.: Jossey-Bass; 2002. [Google Scholar]
- Granich RM, Gilks CF, Dye C, De Cock KM, Williams BG. Universal voluntary HIV testing with immediate antiretroviral therapy as a strategy for elimination of HIV transmission: a mathematical model. Lancet. 2009;373(9657):48–57. doi: 10.1016/S0140-6736(08)61697-9. [DOI] [PubMed] [Google Scholar]
- Huang ZJ, He N, Nehl EJ, Zheng T, Smith BD, Zhang J, Wong FY. Social network and other correlates of HIV testing: Findings from male sex workers and other MSM in Shanghai, China. AIDS & Behavior. 2012;16:858–871. doi: 10.1007/s10461-011-0119-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li H, Peng R, Li J, Yin Y, Wang B, Cohen MS, Chen XS. HIV incidence among men who have sex with men in China: A meta-analysis of published studies. PLoS One. 2011;6:e23431. doi: 10.1371/journal.pone.0023431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Lu H, Raymond HF, Sun Y, Jia Y, He X, Ruan Y. Untested and undiagnosed: barriers to HIV testing among men who have sex with men, Beijing, China. Sexually Transmitted Infections. 2011;88:187–193. doi: 10.1136/sextrans-2011-050248. [DOI] [PubMed] [Google Scholar]
- Li X, Lu H, Ma X, Sun Y, He X, Li C, Jia Y. HIV/AIDS-related stigmatizing and discriminatory attitudes and recent HIV testing among men who have sex with men in Beijing. AIDS & Behavior. 2012;16:499–507. doi: 10.1007/s10461-012-0161-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma W, Ding X, Lu H, Ma X, Xia D, Lu R, Ruan Y. HIV risk perception among men who have sex with men in two municipalities of China – implications for education and intervention. AIDS Care. 2012 doi: 10.1080/09540121.2012.701727. [DOI] [PubMed] [Google Scholar]
- Pai NP, Sharma J, Shivkumar S, Pillay S, Vadnais C, Joseph L, Peeling RW. Supervised and unsupervised self-testing for HIV in high- and low-risk populations: A systematic review. PLoS One. 2013;10:e1001414. doi: 10.1371/journal.pmed.1001414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Song Y, Li X, Zhang L, Fang X, Lin X, Liu Y, Stanton B. HIV-testing behavior among young migrant men who have sex with men (MSM) in Beijing, China. AIDS Care. 2011;23:179–186. doi: 10.1080/09540121.2010.487088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sorensen SW, Sansom SL, Brooks JT, Marks G, Begier EM, Buchacz K, Kilmarx PH. A mathematical model of comprehensive test-and-treat services and HIV incidence among men who have sex with men in the United States. PLoS One. 2012;7:e29098. doi: 10.1371/journal.pone.0029098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wei C, Ruan S, Zhao J, Yang H, Zhu Y, Raymond HF. Which Chinese men who have sex with men missing out on HIV testing? Sexually Transmitted Infections. 2011;87:225–228. doi: 10.1136/sti.2010.047407. [DOI] [PubMed] [Google Scholar]
- Yan H, Yang H, Li J, Wei C, Liu X, Xu X, McFarland W. Emerging disparity in HIV/AIDS disease progression and mortality for men who have sex with men, Jiangsu province, China. AIDS and Behavior. 2013 doi: 10.1007/s10461-013-0520-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Chen P, Lu R, Liu L, Wu Y, Liu X, Yi D. Prevalence of HIV among men who have sex with men in Chongqing, China, 2006–2009: cross-sectional biological and behavioral surveys. Sexually Transmitted Infections. 2012;88:444–450. doi: 10.1136/sextrans-2011-050295. [DOI] [PubMed] [Google Scholar]
- Zhou H, Hu N, Xin Q, Beck J. HIV testing among men who have sex with men in China: A systematic review and meta-analysis. AIDS & Behavior. 2012;16:1717–1728. doi: 10.1007/s10461-012-0225-y. [DOI] [PubMed] [Google Scholar]