Abstract
Background
The purpose of this paper is to examine service use in an episode of acute and post-acute care (PAC) under alternative episode definitions and to look at geographic differences in episode payments.
Data and Methods
The data source for these analyses was a Medicare claims file for 30 percent of beneficiaries with an acute hospital initiated episode in 2008 (N = 1,705,794, of which 38.7 percent went on to use PAC). Fixed length episodes of 30, 60, and 90 days were examined. Analyses examined differences in definitions allowing any claim within the fixed length period to be part of the episode versus prorating a claim extending past the episode endpoint. Readmissions were also examined as an episode endpoint. Payments were standardized to allow for comparison of episode payments per acute hospital discharge or PAC user across states.
Results
The results of these analyses provide information on the composition of service use under different episode definitions and highlight considerations for providers and payers testing different alternatives for bundled payment.
Keywords: access, demand, utilization of services, health care costs, Medicare, payment systems, FFS, capitation, RBRVS, DRGs, risk adjusted payments, rehabilitation services
Introduction
A large proportion of Medicare services are provided following an inpatient acute hospital stay. These services include continued medical care and rehabilitation and are generally referred to as post-acute care (PAC) services. Medicare PAC providers include long-term care hospitals (LTCHs), inpatient rehabilitation facilities (IRFs), skilled nursing facilities (SNFs), and home health agencies (HHAs). While prospective payment systems were developed for each of these provider types with the intention of controlling costs, total Medicare PAC provider fee-for-service (FFS) payments increased from $26.6 billion in 2001 to $63.5 billion in 2011 (MedPAC, 2012).
The prospective payment systems for acute hospital care, LTCH, SNF, IRF, and HHA each have separate rules for payment, eligibility, coverage, and performance measurement. Given these differences, the systems are often referred to as separate silos of care. There is little incentive for providers to efficiently coordinate a beneficiary’s care across settings despite the fact that beneficiaries often transition across settings during their care. About one third of beneficiaries go on to use Medicare PAC services after acute hospital discharge and use a variety of services across a continuum of provider settings during the 30 days after acute hospital discharge (Gage, Morley, Ingber, & Smith,, 2011; Gage, Morley, Spain, & Ingber, 2009; Morley, Gage, Smith, Spain, & Ingber, 2009). Another complexity in PAC service delivery is that the supply of Medicare providers differs across the U.S.; therefore, beneficiaries with similar clinical characteristics receive services from different types of PAC providers, depending on the provider supply in a region (Buntin et al., 2005). The geographic variation in the use of PAC services is significant. According to an analysis presented in a recent Institute of Medicine report (IOM), variation in total Medicare spending would decrease by 73 percent if there was no geographic variation in spending on PAC services (IOM, 2013).
The current payment systems do not necessarily encourage care choices based on the highest quality, lowest cost, or most appropriate care setting for a beneficiary. This, coupled with the growth in Medicare PAC spending, has led to interest in testing alternative delivery system reform models. One important delivery system reform option is a bundled payment. A bundled payment is a single payment for an episode of care defined as a specified set of services over a specified period of time for a procedure or condition. The bundled payment for an episode may include multiple providers in multiple settings. This approach shifts the focus from the silos of the current Medicare PAC payment systems to an episode of care and the continuum of care across provider settings. Though the current fee-for-service payment systems provide payments for different units of service; for example, an MS-DRG payment for services during hospital stays or an HHA episode payment for all visits in a home health episode of care, the concept of a bundled payment for PAC episodes differs in that it combines payment across providers. Bundled payments incentivize improvements in patient-centered care via increased coordination and accountability across providers for an episode. Bundled payments, based on an episode definition, can be prospectively determined based on a single payment rate, or they can be retrospectively determined during a payment reconciliation period.
Section 1115A of the Social Security Act (Act) provides authority to the Center for Medicare & Medicaid Innovation (CMMI), within the Centers for Medicare & Medicaid Services (CMS), to develop, test, evaluate, and potentially scale or expand initiatives testing a variety of innovative models. In 2011, CMMI launched the Bundled Payment for Care Improvement Initiative. The first track of the Bundled Payment for Care Improvement Initiative seeks broad public participation in testing bundled payment models1. The initial models focus on Medicare services provided during the inpatient hospital stay and/or a post-discharge period.
The Office of the Assistant Secretary for Planning and Evaluation (ASPE) funded research with RTI International to inform the larger policy discussion of Medicare PAC episodes and bundled payments. The analysis examined Medicare beneficiary-level episode transfer patterns, utilization, and payments for a variety of time-based PAC episode definitions initiating with a Medicare acute hospital stay. Acute hospital readmissions and subsequent PAC services following the acute hospital readmissions were included or excluded in the different episode definitions examined. The analysis looked at both fixed length episode definitions (i.e., 30, 60 or 90 days following a hospital discharge) and variable length episode definitions (i.e., episode end point based on a 30-, 45-, or 60-day gap in service use).
Understanding the composition of alternative PAC episode definitions is an important foundational step in the discussion of bundled payments and larger Medicare delivery system reforms. While many combinations of Medicare provider and supplier services could be envisioned in a bundled payment approach, the initial ASPE funded studies focused on Medicare acute hospital and PAC service episode definitions. This paper focuses on the services in a beneficiary’s trajectory of Medicare PAC use that are included or excluded under a variety of acute hospital plus PAC use definitions.
Methods
Using a 30 percent sample of acute hospital initiated episodes identified in 2008 fee-for-service Medicare claims, we examined several acute hospital and PAC episode definitions. For purposes of this analysis, the beginning of an episode was defined as an index acute hospital stay in 2008. We limited our sample to live discharges (all ages) from the index acute hospital stay, though beneficiaries may have died at a later point in the episode. Index acute hospitalizations were defined as an acute hospitalization preceded by a 30-day period without Medicare acute or PAC service use, defined as LTCH, IRF, SNF, and HHA. This 30-day period was used to be sure that we were identifying the start of an episode rather than ongoing service use following an earlier hospitalization. We examined both the inclusion and exclusion of acute hospital readmissions and subsequent PAC use, defined as LTCH, IRF, SNF, HHA, and outpatient therapy services, following an acute hospital readmission across the different episode definitions included in the analysis. All services were included as long as they fell within the time-based episode definitions described below. Hospice services are not included in the episode definition. Of our sample size (N = 1,705,794) index acute hospital events in 2008, 38.7 percent or (N = 659,549) went on to use Medicare PAC services.
There are many ways to define Medicare PAC episodes. Initiating events defining the start of a PAC episode may include an acute hospital stay, post-acute service, physician service, or ambulatory event. The end point of a time-based episode definition may be a fixed end point (e.g., an acute hospital stay plus Medicare PAC services for 30 days post discharge); a variable length end point (e.g., an episode ends with a gap in defined services); or another end point (e.g., acute hospital readmission, other considerations for episodes for chronic conditions).
The fixed length episode end points were defined as 30, 60, or 90 days after discharge from the initiating index acute hospitalization. The analysis included two specifications of a fixed length episode. First, the fixed length episode definition included any PAC claim starting within the defined timeframe (i.e., 30, 60 or 90 days) after the index acute hospitalization. Second, the alternative specification of a fixed length episode considered the end point as a firm period of time. In this case, services spanning the endpoint of the episode window were prorated so that only days and dollars associated with the service provided in the episode window were included. For example, in the first case, all visits on an HHA claim spanning the endpoint of the episode window would be included in the episode definition. In the second case, only visits on the portion of the HHA claim within the episode window would be included in the episode and visits outside of the episode window would not be included. The study also examined the impact of ending the two fixed length episode specifications with an acute hospital readmission. We also analyzed alternative variable length episode definitions, with end points defined by a 30-day period without acute or PAC service claims or by ending the variable length episode definitions with an acute hospital readmission (data not shown).
The four definitions of a 30, 60 or 90 day fixed length episode are summarized below.
Episode includes any acute hospital or PAC claim initiating within 30, 60, or 90 days of acute hospital discharge.
Episode includes any PAC claim initiating within 30, 60, or 90 days of acute hospital discharge. However, the presence of a readmission ends an episode.
Episode includes acute hospital or PAC services provided in the 30, 60, or 90 days following acute hospital discharge. Claims for services that span the 30, 60 or 90 day endpoint are prorated.
Episode includes PAC services provided in the 30, 60, or 90 days following acute hospital discharge. Claims for services that span the 30, 60 or 90 day endpoint are prorated. However, the presence of a readmission ends an episode.
To examine differences in episode payments by geography, we standardized payments to remove the effects of geographical payment differences using the approach from earlier ASPE studies on PAC episodes. Acute hospital, IRF, LTCH, HHA, and SNF payments were standardized using the base rate multiplied by the case mix weight. Therapy payments were standardized using the physician fee schedule amount multiplied by the units on the claim.
The analyses presented here focus on PAC use overall and by MS-DRG to look at differences in use for medical versus surgical acute hospitalizations likely to require more rehabilitation services. PAC episode payments and length were also examined by episode definition to demonstrate the effect of their differences. PAC episode payments were calculated per hospital discharge versus per PAC user for each episode definition, and payments were decomposed by service type to illustrate the effects of different service use on overall episode payments per hospital discharge versus per PAC user. Finally, PAC episode payments were examined by state to demonstrate the geographic differences in per discharge and per PAC user.
Results
Across all MS-DRGs, 38.7 percent of beneficiaries were discharged to a PAC setting. Exhibit 1 includes the top five MS-DRGs by volume of discharges to PAC. The top five by volume of discharges to PAC includes a mix of medical and rehabilitation MS-DRGs. Overall, the most common MS-DRG among PAC users in our sample is MS-DRG 470, Major Joint Replacement of Lower Extremity without MCC, with 94.2 percent of beneficiaries in this MS-DRG discharged to PAC. The second most frequent MS-DRG among PAC users is MS-DRG 65 Intracranial Hemorrhage with 75.0 percent of beneficiaries discharged to PAC. While these two MS-DRGs have very high proportions of beneficiaries going on to use PAC, a smaller proportion of beneficiaries are discharged to PAC in medical MS-DRGs, such as MS-DRG 194 Simple Pneumonia (36.3 percent).
Exhibit 1. Number of PAC Users and Percent of Beneficiaries Discharged to PAC Overall and by MS-DRG for the Top Five MS-DRGs By Volume of Discharges to PAC, 2008.
| Number of PAC Users | Percent of BeneficiariesDischarged to PAC (PAC Users) | ||
|---|---|---|---|
| All MS-DRGs | 659,549 | 38.7 | |
| MS-DRG 470 Major joint replacement of lower extremity without MCC | 90,434 | 94.2 | |
| MS-DRG 65 Intracranial hemorrhage or cerebral infarction with CC | 13,992 | 75.0 | |
| MS-DRG481 Hip& femur procedures except major joint with CC | 13,704 | 95.4 | |
| MS-DRG 194 Simple Pneumonia & pleurisy with CC | 13,604 | 36.3 | |
| MS-DRG690 Kidney & urinary tract infections without MCC | 12,954 | 43.9 | |
SOURCE: Medicare claims 2008.
Exhibit 2 shows differences in mean PAC payments and mean PAC episode lengths by PAC episode definition. Definition 1a allows any claim initiating within the 30 days after discharge to be included in the episode definition. Mean PAC payments per PAC user are $10,651 and mean PAC episode length is 40.6 days. In comparison, Definition 1b, which is identical to the 1a, but excludes acute hospital readmissions and subsequent PAC, mean PAC payments per PAC user are $8,165 and mean PAC episode length is 37.4 days. Acute readmissions comprise a significant proportion of episode payments leading to variation in payment levels.
Exhibit 2. Mean PAC Payment Per PAC User and Mean PAC Episode Length by Episode Definition, 2008.
| Episode Definitions | Mean PAC Payment Per PAC User (Standard Deviation) N = 659,549 | Mean PAC Episode Length in Days (StandardDeviation) N = 659,549 | ||||
|---|---|---|---|---|---|---|
| Definition 1a—Any Claim Starting Within 30 Days of Discharge | $10,651 | 40.6 | ||||
| ($12,604) | (27.1) | |||||
| Definition 1b—Any Claim Starting within 30 Days of Discharge Excluding Acute Hospital Readmissions and Subsequent PAC Services | $8,165 | 37.4 | ||||
| ($10,099) | (27.0) | |||||
| Definition 1c—30 Day Fixed Period Following Hospital Discharge (Prorated) | $7,564 | 25.0 | ||||
| ($8,622) | (8.4) | |||||
| Definition 1d—30 Day Fixed Period Following Hospital Discharge (Prorated) Excluding Acute Hospital Readmissions and Subsequent PAC Services | $5,745 | 22.7 | ||||
| ($6,988) | (9.7) | |||||
| Definition 2a—Any Claim Starting Within 60 Days of Discharge | $12,825 | 50.5 | ||||
| ($15,574) | (30.7) | |||||
| Definition 2b—Any Claim Starting within 60 Days of Discharge Excluding Acute Hospital Readmissions and Subsequent PAC Services | $8,521 | 43.6 | ||||
| ($10,634) | (29.7) | |||||
| Definition 2c—60 Day Fixed Period Following Hospital Discharge (Prorated) | $11,241 | 43.2 | ||||
| ($12,835) | (18.7) | |||||
| Definition 2d—60 Day Fixed Period Following Hospital Discharge (Prorated) Excluding Acute Hospital Readmissions and Subsequent PAC Services | $7,487 | 36.4 | ||||
| ($9,075) | (20.4) | |||||
| Definition 3a—Any Claim Starting Within 90 Days of Discharge | $14,542 | 62.4 | ||||
| ($17,757) | (39.4) | |||||
| Definition 3b—Any Claim Starting within 90 Days of Discharge Excluding Acute Hospital Readmissions and Subsequent PAC Services | $8,781 | 50.1 | ||||
| ($10,865) | (36.4) | |||||
| Definition 3c—90 Day Fixed Period Following Hospital Discharge (Prorated) | $13,623 | 56.3 | ||||
| ($15,993) | (29.2) | |||||
| Definition 3d—90 Day Fixed Period Following Hospital Discharge (Prorated) Excluding Acute Hospital Readmissions and Subsequent PAC Services | $8,252 | 44.2 | ||||
| ($10,241) | (29.5) | |||||
SOURCE: Medicare claims 2008.
Under Definition 1c, which uses a prorated or firm 30 day period, mean PAC payments per PAC user are lower at $7,564 with a shorter 25 day mean PAC episode length. Definition 1d is the most restrictive, because it uses a prorated approach to define the end period and excludes acute readmissions and subsequent PAC. As expected, under Definition 1d, mean PAC payment per PAC user is much lower at $5,745 and mean PAC episode length decreases to 22.7 days. Similar patterns of PAC payment and PAC episode length are observed within 60 day and 90 day fixed length episodes, though payments and episode length are higher under each of these compared to the 30 day episodes.
Exhibit 3 compares mean index acute hospital payments and mean PAC payments for acute hospital discharges and PAC users. As expected, across the four 30-day episode definitions there is a higher mean index acute hospital payment per PAC user given the type of hospital services typically provided to PAC users. For Definition 1a, mean PAC payment per acute hospital discharge is $5,252 compared to the higher $10,651 mean PAC payment per PAC user. We see similar results across the episode definitions.
Exhibit 3. Mean Acute Hospital and PAC Episode Payments Per Acute Hospital Discharge Versus Per PAC User, By Episode Definition, 2008.
| Episode Definitions | Mean Index Acute Hospital Payment Per Discharge (Standard Deviation) | Mean PAC Payment Per Acute Hospital Discharge (Standard Deviation) | Mean Index Acute Hospital Payment Per PAC User (Standard Deviation) | Mean PAC Payment PerPAC User (Standard Deviation) | |||
|---|---|---|---|---|---|---|---|
| Definition 1a—Any Claim Starting Within 30 Days of Discharge | $8,531 | $5,252 | $10,572 | $10,651 | |||
| ($9,798) | ($10,730) | ($12,413) | ($12,604) | ||||
| Definition 1b—Any Claim Starting within 30 Days of Discharge Excluding Acute Hospital Readmissions and Subsequent PAC Services | $8,531 | $3,157 | $10,572 | $8,165 | |||
| ($9,798) | ($7,433) | ($12,413) | ($10,099) | ||||
| Definition 1c—30 Day Fixed Period Following Hospital Discharge (Prorated) | $8,531 | $3,845 | $10,572 | $7,564 | |||
| ($9,798) | ($7,523) | ($12,413) | ($8,622) | ||||
| Definition 1d—30 Day Fixed Period Following Hospital Discharge (Prorated) Excluding Acute Hospital Readmissions and Subsequent PAC Services | $8,531 | $2,221 | $10,572 | $5,745 | |||
| ($9,798) | ($5,168) | ($12,413) | ($6,988) | ||||
SOURCE: Medicare claims 2008.
Additional analyses of specific PAC service use within PAC episodes for Definition 1a are shown in Exhibit 4. These results indicate that 52.2% of PAC episodes had at least one HHA claim as compared to 2% with at least one LTCH claim. Mean LTCH payment per LTCH service user is about $35,200. Averaging across all PAC users, the mean LTCH component decreases to $691 as compared to $283 averaging across all hospital discharges. Mean HHA payment per HHA service user is about $2,786 as compared to $1,455 per PAC user and $590 per hospital discharge. Similar results were found across episode definitions (data not shown).
Exhibit 4. Mean PAC Episode Payments, By PAC Service, 2008.
| Episode Definition | Definition 1a- Any Claim Starting Within 30 Days of Discharge |
|---|---|
| HHA | |
| Percent with Claim | 52.2 |
| Mean Payment Per Service User | $2,786 |
| Mean Payment Per PAC User | $1,455 |
| Mean Payment Per Hospital Discharge | $590 |
| SNF | |
| Percent with Claim | 45.3 |
| Mean Payment Per Service User | $11,476 |
| Mean Payment Per PAC User | $5,204 |
| Mean Payment Per Hospital Discharge | $2,085 |
| IRF | |
| Percent with Claim | 9.0 |
| Mean Payment Per Se rvice User | $16,504 |
| Mean Payment Per PAC User | $1,489 |
| Mean Payment Per Hospital Discharge | $601 |
| LTCH | |
| Percent with Claim | 2.0 |
| Mean Payment Per Service User | $35,203 |
| Mean Payment Per PAC User | $691 |
| Mean Payment Per Hospital Discharge | $283 |
| Acute Hospital Readmission | |
| Percent with Claim | 14.8 |
| Mean Payment Per Service User | $11,594 |
| Mean Payment Per PAC User | $1,718 |
| Mean Payment Per Hospital Discharge | $1,655 |
SOURCE: Medicare claims 2008.
The results demonstrate the differential impact of averaging high and low volume PAC services in a mean episode payment across service users, all PAC users, or all acute hospital discharges. Though the per hospital discharge payments for LTCH are quite small, the payments for those who use LTCHs are much higher. The differences in these payments decrease for lower cost services, such as HHA, that are used by a higher proportion of beneficiaries. The differential impact may vary in areas of the country with a limited number of Medicare PAC providers versus a variety of Medicare PAC provider settings.
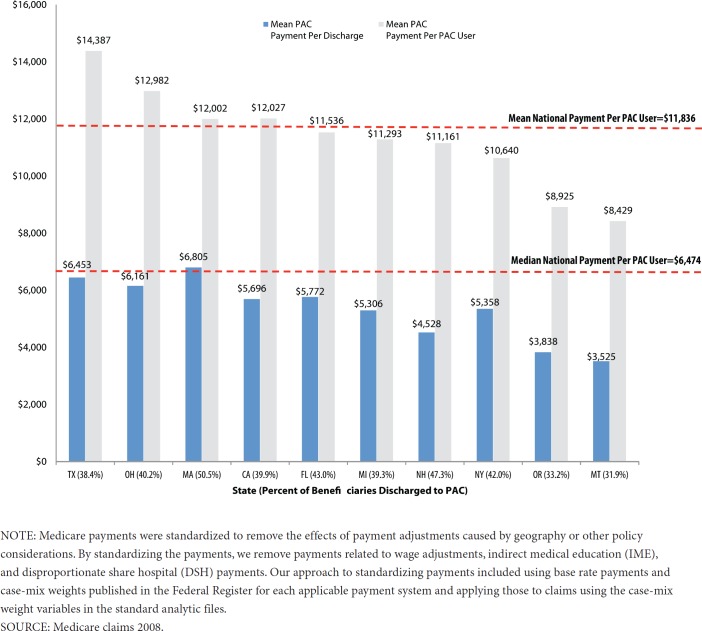
Exhibit 5 shows differences in standardized mean PAC episode payment per PAC user versus per acute hospital discharge across several states that vary in terms of the supply of PAC providers and in total episode payments. The figure includes a subset of states that are in the top 5, middle 10, and bottom 5 levels of mean payment per PAC user. This work highlights the importance of understanding the differences in geographic areas.
Exhibit 5. Standardized Mean PAC Episode Payment Per PAC User, and Per Discharge, By State, Episode Definition 30-day Fixed-Length Episode with Any Claim Starting Within 30 Days, 2008.
The percentage of beneficiaries discharged to PAC varies by state ranging from 50.5% in Massachusetts to 31.9% in Montana. This may be due to variation in geographic supply of PAC providers or practice patterns in a given area. In 2008, the standardized mean national payment per PAC user was $11,836 as compared to the median at $6,476. For all states in Exhibit 5 except Texas, Ohio, Massachusetts, and California, the standardized mean PAC payment per PAC user is less than the mean national payment per PAC user.
Discussion
This paper is intended to provide an overview of the exploratory research results looking at a beneficiary’s trajectory of Medicare PAC use and the services that are included or excluded under a variety of acute hospital plus PAC use definitions. The results of these analyses on Medicare beneficiary PAC use vary based on: (1) the denominator used to calculate an average payment level for all hospital discharges or solely PAC users; (2) the mix and volume of PAC services including decisions to include or exclude an acute hospital readmission; and (3) the definition of the end point of an episode.
This study explored a variety of PAC episodes initiating with an index acute hospital stay, which introduces options of whether an episode definition applies to all hospital discharges versus solely PAC users. As shown in Exhibit 3, mean PAC payments per acute hospital discharge are approximately half of the per PAC user payment across the episode definitions. While this is the result when calculating across all MS-DRGs, the per hospital discharge payment versus the per PAC user payment differ by MS-DRG depending on the proportion of discharges in an MS-DRG going on to PAC services. For example, the difference between these payments will be less in MS-DRGs with a high proportion of beneficiaries going on to PAC, such as those in MS-DRGs for joint replacement, hip and femur procedures, and stroke.
If an episode payment includes an index hospitalization and PAC, there may be several different behavioral responses. For example, providers may have an incentive to keep patients in acute care slightly longer to reduce the need for subsequent service use and minimize total episode payments. In addition, there may be a shift toward the use of lower cost PAC settings. Alternatively, if episode payments are for PAC services only, there may be an incentive to discharge more patients to PAC services in order to initiate the episode payment, though there may be a shift toward the use of lower cost PAC services. The mix and volume of PAC services included in the episode definition impacts mean episode payment levels. This exploratory analysis defines an episode using Medicare SNF, LTCH, HHA, IRF and hospital outpatient therapy services. A broader episode definition including additional Medicare services, such as physician visits and other services, may yield different results. The approach also examined the payment impact of inclusion or exclusion of an acute hospital readmission occurring during the timeframe of the episode definition. Acute readmissions reflect a significant proportion of episode payments leading to variation in payment levels. The variation in episode payments also differs across MS-DRGs, depending on the number of readmissions for beneficiaries with a particular MS-DRG. Depending upon the parameters of the episode definition, excluding acute hospital readmissions may introduce incentives to generate new episode payments. Including readmissions may incentivize the management of care within an episode, such as increasing collaboration and the introduction of other efforts to decrease the likelihood of a readmission. Analysis decomposing PAC episodes by service type highlights the potential differential impact of averaging high and low volume services across episode payment calculations and the effect of the denominator over which the payments are averaged (i.e., per acute hospital discharge, per PAC user, or per user of a particular service).
The definition of the end point of an episode can be set at various timeframes. In this study, we defined a fixed end point in two ways: (1) allowing any claim initiating during the time frame to be included in the episode definition and (2) proration of the last claim in the time frame of the episode. The first approach provides a broader episode time frame. The second approach provides a clean fixed period of time, though it presents additional considerations regarding payment for services following the episode endpoint and the initiation of subsequent episodes. While the first approach may capture the majority of care associated with an episode, it may provide an incentive to delay some service initiation outside of the episode window.
The supply of Medicare PAC providers differs significantly across different geographic areas of the U.S. While HHAs and SNFs are available in every state, there are fewer IRF providers overall, and LTCHs are not located in every state. Medicare beneficiaries with similar clinical characteristics may receive services depending on the supply of PAC providers in their local area. This study examined differences in payments by geographic area using standardized payments at the national and state level, and the results illustrate the geographic variation in the percent of beneficiaries discharged to PAC and the state variation in mean payment per PAC user. These differences are important to consider in thinking about an episode based payment.
The results of these analyses provide information on the composition of service use under different episode definitions and highlight considerations for providers and payers testing different alternatives for bundled payment.
Disclaimer
The work was funded by Department of Health and Human Services, Office of the Assistant Secretary for Planning and Evaluation (ASPE) under contract with RTI International (Contract 100-03-0018, HHSP233200700001T). None of the authors have financial or other interests related to the research or policy implications. The views in the article are those of the authors and do not reflect the views of the Department of Health and Human Services.
Acknowledgment
The authors would like to acknowledge the programming support of John Potelle of RTI International.
Footnotes
Request for Applications—Bundled Payment for Care Improvement Initiative: http://www.innovations.cms.gov/initiatives/Bundled-Payments/Model-2/index.html
References
- Buntin MB, Garten AD, Paddock S, Saliba D, Totten M, Escarce JJ. How much is postacute care use affected by its availability? Health Services Research. 2005 Apr;40(2):413–434. doi: 10.1111/j.1475-6773.2005.0i366.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gage B, Morley M, Spain P, Ingber I. Examining Post Acute Care Relationships in an Integrated Hospital System. Waltham, MA: RTI International; 2009. Feb, Prepared for the Office of the Assistant Secretary for Planning and Evaluation. Project Officer Susan Bogasky. Retrieved from http://aspe.hhs.gov/health/reports/09/pacihs/index.shtml. [Google Scholar]
- Gage B, Morley M, Ingber M, Smith L. Expanded Post Acute Episodes File. Waltham, MA: RTI International; 2011. Apr, Prepared for the Office of the Assistant Secretary for Planning and Evaluation. Project Officer Susan Bogasky. Retrieved from http://www.aspe.hhs.gov/health/reports/2011/PACexpanded/index.shtml. [Google Scholar]
- IOM (Institute of Medicine) Variation in Health Care Spending: Target Decision Making, Not Geography. 2013 Retrieved from http://www.nap.edu/catalog.php?record_id=18393. [PubMed]
- MedPAC (Medicare Payment Advisory Commission) A Data Book: Healthcare Spending and the Medicare Program. Washington DC: 2012. [Google Scholar]
- Morley M, Gage B, Smith L, Spain P, Ingber M. Post Acute Care Episodes. Waltham, MA: RTI International; 2009. Nov, Prepared for the Office of the Assistant Secretary for Planning and Evaluation. Project Officer Susan Bogasky. Retrieved from http://aspe.hhs.gov/health/reports/09/pacepifinal/index.shtml. [Google Scholar]