Abstract
Background
Aortocoronary dissection can complicate percutaneous coronary intervention (PCI) of chronic total occlusions (CTOs).
Methods
We retrospectively examined the frequency and outcomes of aortocoronary dissection among 336 consecutive CTO PCIs performed at our institution between 2005 and 2012 and performed a systematic review of the published literature.
Results
Aortocoronary dissection occurred in 6 patients (1.8%, 95% confidence intervals 0.7%, 3.8%). All aortocoronary dissections occurred in the right coronary artery (CTO target vessel in 5 patients and donor vessel in 1 patient). The baseline clinical characteristics of patients with and without aortocoronary dissection were similar. Compared to patients without, those with aortocoronary dissection were more likely to undergo crossing attempts using the retrograde approach (25% vs. 67%, P=0.036) and experience a major complication (2.4% vs. 33.3%, p=0.008). Technical and procedural success rates were similar in both groups. Of the 6 patients with aortocoronary dissection one underwent emergency coronary bypass graft surgery, 4 were treated with ostial stenting and one was treated conservatively without subsequent adverse clinical outcomes. Systematic literature review provided 107 published cases of aortocoronary dissection during PCI, that occurred mainly in the right coronary artery (74.8%) and were treated with stenting (49.5%), emergency coronary bypass graft surgery (29%) or conservatively (21.5%).
Conclusions
Aortocoronary dissection is an infrequent complication of retrograde CTO PCI and although it can be treated with stents in most patients, it may infrequently require emergency coronary artery bypass graft surgery.
Keywords: Percutaneous coronary intervention, chronic total occlusion, complications, aortocoronary dissection
Coronary chronic total occlusions (CTO) are common in patients with coronary artery disease undergoing coronary angiography (1,2), and successful CTO percutaneous coronary intervention (PCI) has been associated with clinical benefit (3,4). Currently, CTO PCI is performed infrequently in the US, in part due to concerns about procedural risks (5). However in a weighted meta-analysis of 18,061 patients from 65 studies the incidence of CTO PCI complications was low and decreased over time, in spite of an increase in procedural success rates (6).
Aortocoronary dissection is an infrequent, yet potentially serious complication of coronary angiography or PCI that can lead to emergency coronary artery bypass graft surgery (CABG) or death (7,8). To date there is limited systematic assessment of its occurrence during CTO PCI (9-12). In the present study we sought to (a) assess the frequency and outcomes of aortocoronary dissection during CTO PCI among patients treated at our institution, and (b) perform a systematic review of the literature on the occurrence and implications of aortocoronary dissection among patients undergoing cardiac catheterization.
Methods
Patient population
We reviewed the procedural and clinical records and coronary angiograms of all patients who underwent CTO PCI between May 2005 and May 2012 at our institution to determine the frequency and outcomes of aortocoronary dissection. The study was approved by our institutional review board.
Definitions
Aortocoronary dissections were identified by review of the angiograms of all study patients. Aortocoronary dissection was defined as persistent contrast staining in the aortic cusp or root.
Coronary CTOs were defined as coronary lesions with thrombolysis in myocardial infarction (TIMI) grade 0 flow for a duration of at least 3 months. Estimation of the occlusion duration was based on first onset of anginal symptoms, prior history of myocardial infarction in the target vessel territory, or comparison with a prior angiogram.
Technical success of CTO PCI was defined as successful CTO revascularization with achievement of <30% residual diameter stenosis within the treated segment and restoration of TIMI grade 3 antegrade flow. Procedural success was defined as achievement of technical success with no in-hospital major adverse cardiac events (MACE). MACE was defined as a composite of death, clinical myocardial infarction, stroke, or coronary revascularization.
Literature review: Search strategy, eligibility criteria, data extraction
We performed a comprehensive search of the Pubmed and Cochrane Library databases for manuscripts on aortocoronary dissection during coronary angiography or intervention. Human studies in English published between the years 1973-2012 were included if they reported the incidence and outcomes of aortocoronary dissection during cardiac catheterization. Review articles, letters to the editor, and studies in which procedural complications could not be accurately assessed from the published manuscript were excluded. A list of the included studies is shown in Supplemental Table 1. Data from included studies were extracted by two authors (D.S. and T.M.) and controversies were reviewed by both; in case of disagreement a third reviewer (E.B.) was used to reach consensus. Extracted data included the number of patients and lesions, age, sex, cardiac catheterization procedure type, target vessel, cause of dissection, angiographic success, and clinical outcomes.
Statistical Analysis
Descriptive statistics were used to report clinical characteristics, angiographic measures and in-hospital outcomes among patients with and without aortocoronary dissection. Continuous variables were presented as mean with standard deviation and compared using the t-test or Wilcoxon rank-sum test, as appropriate. Categorical variables were expressed as percentages and compared using the chi-square or the Fisher's exact test, as appropriate. All statistical analyses were performed with JMP version 9.0 (SAS Institute, Cary, North Carolina) and Stata version 12 (StataCorp, College Station, Texas).
Results
Patient characteristics
During the study period, a total of 336 consecutive patients underwent CTO PCI at our institution. Aortocoronary dissection occurred in 6 of 336 patients (1.8%, 95% confidence intervals 0.7%, 3.8%). The baseline clinical characteristics of patients with and without aortocoronary dissection were similar (Table 1). The target vessel was the right coronary artery in 5 of the 6 (83%.3%) patients with vs. 54.0% of 330 patients without aortocoronary dissection (p=0.15).
Table 1.
Baseline clinical and angiographic and procedural characteristic of the study patients, classified according to whether they developed aortocoronary dissection during CTO intervention
| Variable | Overall (n=336) | Aortocoronary dissection (n=6) | No aortocoronary dissection (n=330) | P |
|---|---|---|---|---|
| Clinical Characteristics | ||||
| Age (years)* | 63.8±8.4 | 59.7±3.7 | 63.8±8.4 | 0.229 |
| Men (%) | 98.8 | 100 | 98.7 | 0.680 |
| Hypertension (%) | 90.4 | 100 | 90.3 | 0.382 |
| Hyperlipidemia (%) | 89.0 | 83.3 | 89.1 | 0.674 |
| Diabetes (%) | 47.4 | 33.3 | 47.6 | 0.481 |
| Heart failure (%) | 37.5 | 16.7 | 37.9 | 0.258 |
| History of myocardial infarction (%) | 46.7 | 66.7 | 46.4 | 0.320 |
| History of coronary artery bypass graft surgery (%) | 25.4 | 33.3 | 25.2 | 0.660 |
| Prior percutaneous coronary intervention (%) | 37.5 | 33.3 | 37.6 | 0.831 |
| History of stroke (%) | 4.6 | 16.7 | 4.3 | 0.260 |
| Angiographic characteristics | ||||
| CTO target vessel | 0.303 | |||
| Right coronary artery (%) | 54.5 | 83.3 | 54.0 | |
| Left anterior descending artery (%) | 23.1 | 16.7 | 23.2 | |
| Circumflex (%) | 202 | 0 | 20.6 | |
| Left main/bypass graft (%) | 2.2 | 0 | 2.2 | |
| Prior failed attempt for CTO PCI (%) | 6.6 | 0 | 6.3 | 0.378 |
| Moderate/severe calcification (%) | 46.6 | 83.3 | 46.1 | 0.060 |
| Moderate/severe tortuosity (%) | 36.8 | 33.3 | 37.2 | 0.845 |
| Procedural techniques | ||||
| Antegrade wire escalation attempt (%) | 95.2 | 83.3 | 95.1 | 0.292 |
| Antegrade dissection/re-entry attempt (%) | 28.1 | 50.0 | 27.7 | 0.254 |
| Retrograde attempt (%) | 26.2 | 67.0 | 25.0 | 0.036 |
| Final successful CTO crossing Technique (n=261) | 0.017 | |||
| Antegrade wire escalation (%) | 76.6 | 25 | 76.5 | |
| Antegrade dissection/re-entry (%) | 10.6 | 0 | 10.7 | |
| Retrograde (%) | 13.8 | 75 | 12.8 | |
| Procedural outcomes | ||||
| Technical success (%) | 77.7 | 83.3 | 77.6 | 0.728 |
| Procedural success (%) | 75.9 | 66.7 | 76.0 | 0.607 |
| Retrograde attempt (%) | 26.2 | 66.7 | 25.5 | 0.036 |
| Total procedure time (min)* | 139±71 | 206±91 | 138±71 | 0.034 |
| Total fluoroscopy time (min)* | 39±22 | 58±31 | 39±21 | 0.034 |
| Total air kerma radiation exposure (Gray)* | 4.6±2.4 | 5.8±0.7 | 4.6±2.5 | 0.341 |
| Total contrast volume (ml)* | 356±139 | 389±260 | 355±136 | 0.555 |
| Major complications (%) | 3.0 | 33.3 | 2.4 | 0.008 |
mean ±standard deviation
CTO, chronic total occlusion; PCI, percutaneous coronary intervention
Procedural characteristics and outcomes
Patients with aortocoronary dissection were more likely to undergo crossing attempts using the retrograde approach (67% vs. 25%, p=0.036). Two of the six dissections occurred during antegrade crossing and were due to pressure dampening in the setting of ostial coronary artery disease. The other four occurred during the retrograde approach. In three cases entry of the retrograde guidewire into the proximal true lumen using the reverse controlled antegrade and retrograde tracking and dissection (reverse CART) technique was challenging, resulting in sub-aortic entry into the aorta. In the fourth retrograde case the dissection occurred in the donor vessel due to pressure dampening.
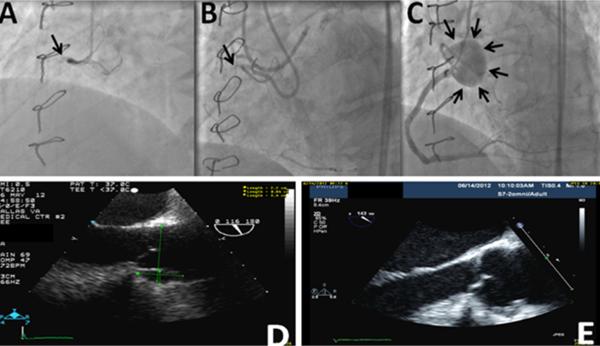
There was no significant difference in technical or procedural success rates between the two groups of patients. Of the 6 patients with aortocoronary dissection one underwent emergency coronary bypass graft surgery, 4 were treated with ostial stenting and one was treated conservatively without subsequent adverse clinical outcomes. Imaging with trans-esophageal echocardiography (TEE) was done in 2 patients – in one patient repeat TEE was repeated 1 month later, demonstrating resolution of the dissection (Figure 1).
Figure 1.
Coronary angiography demonstrating chronic total occlusion of the proximal right coronary artery using single (arrow, panel A) or dual (arrow, panel B) injection. Angiography after successful intervention of the right coronary artery chronic total occlusion demonstrating aortocoronary dissection adjacent to the right coronary artery ostium (arrows, panel C). Trans-esophageal echocardiography at the end of the chronic total occlusion intervention of the right coronary artery demonstrating a dissection in the right coronary cusp (Panel 1D). Repeat trans-esophageal echocardiography performed 1 month later demonstrated resolution of the dissection (Panel 1E).
A major periprocedural complication occurred in 10 of 336 patients (3.0%), as follows: 1 death due to cardiac arrest, 2 emergent CABG (1 for entrapped Tornus catheter, 1 for acute closure of the right coronary artery), 4 clinical myocardial infarction (3 treated conservatively, 1 required emergent PCI), 1 tamponade which required emergent pericardiocentesis, 1 transient ischemic attack, and 1 major bleeding event requiring 3 units blood transfusion without an identifiable overt bleeding source. Major periprocedural complications occurred more commonly in patients with (33.3%) compared to those without (2.4%) aortocoronary dissection (p=0.008). In patients with aortocoronary dissection, major periprocedural complications were emergent CABG for acute right coronary artery occlusion and transient ischemic attack presenting as right arm weakness, which resolved in 1 hour.
Systematic review of the literature
A search of Pubmed and Cochrane Library databases using the term “aortocoronary dissection” provided 99 references. Of those, 72 were excluded due to being on a different topic (n=56), printed in a foreign language (n=10), or containing insufficient data (n=6). An additional 43 references were found using manual search of the retrieved references. Hence 70 studies reporting outcomes on 107 patients with aortocoronary dissection met the inclusion criteria and were included in the final pooled analysis. A full listing of all 70 articles is provided in Supplemental Table 1.
Of the 107 cases, 23.4% occurred during diagnostic coronary angiography and 76.6% during PCI. The target vessel was reported in 60.7% of the cases and was CTO in 37% of those cases. The most common cause of dissection was guide catheter-induced trauma (n=60, 63.2%) followed by guidewire-induced trauma (n=11, 11.6%), forceful balloon inflation (n=14, 14.7%), forceful contrast injection (n=7, 7.4%), and forceful manipulation of a stent (n=1, 1.1%). Two cases were attributed to other factors (one from weakened aorta due to cystic medial necrosis, and the other from trauma from a thrombectomy system). The right coronary artery was most commonly involved (n=80, 74.8%), followed by the left main (n=17, 15.9%), aorta (n=6, 5.6%), or a saphenous vein graft (n=1, 0.9%). Three (2.8%) of the published cases included in the review did not specify the initial site of dissection. Aortocoronary dissections were most commonly treated with stenting (49.5%), followed by surgery (29%) or conservative management (21.5%). Eight patients (7.5%) died: 6 of them underwent surgery to repair the dissection and 2 were treated conservatively. Of those who went to surgery one died during surgery (could not be weaned from bypass), and 5 died during the postoperative period [one from myocardial infarction, one from uncontrollable septic shock, one from pulmonary embolism, one from multi-organ failure; the cause of death for one patient was not reported (16)]. Of the 2 patients who did not undergo surgery, one died 48 hours post PCI after developing multiple hematomas on the anterior wall of the ascending aorta and around the right coronary and another one died 15 days after catheterization.
Discussion
The major findings of our study are that aortocoronary dissection: (1) is an infrequent complication of CTO PCI; (2) occurs most commonly during retrograde CTO PCI; and (3) often can be successfully treated with stenting, although occasionally emergency CABG may be required.
In a recently published weighted meta-analysis of CTO PCI complications (6), only 3 of 65 studies reported the frequency of aortocoronary dissection (9-11). Two of these were exclusively retrograde series reporting an aortocoronary dissection frequency of 1/85 (1.2%) (11) and 1/157 (0.6%) (9). In the third study of unselected patients undergoing CTO PCI the frequency of aortocoronary dissection was 2/904 (0.2%) (10). Our study revealed higher risk of aortocoronary dissection during CTO PCI (1.8%, 95% confidence intervals 0.7%, 3.8%) that may have been due to inclusion of high risk patients (as suggested in part by the high prevalence of prior coronary artery bypass graft surgery) or due to the systematic review of angiographic and procedural data.
In our study and the published literature (9-11), aortocoronary dissection was more common among patients undergoing retrograde CTO PCI. Most aortocoronary dissection occurred in patients undergoing retrograde CTO PCI. Donor vessel dissection is one of the most feared complications of the retrograde approach, as it can lead to acute hemodynamic collapse and/or death (13). The patient who developed donor vessel dissection in our series (in the right coronary artery) remained hemodynamically stable, but required emergency coronary artery bypass graft surgery later in the day. If the donor vessel is the left main, dissection or injury can lead to rapid cardiac arrest or death and requires immediate percutaneous treatment (8,13).
Every effort should be undertaken to prevent aortocoronary dissections. This can first be achieved by paying meticulous attention to the pressure waveform. Contrast should not be injected when the pressure waveform is dampened. Moreover, guide catheters with side holes should be avoided (especially in the left main coronary artery), as they may provide a false sense of security, but can still cause dissection when contrast is injected. During retrograde CTO PCI the retrograde guidewire should not be advanced in the subaortic space; re-entry into the proximal true lumen should be best attempted distal to the CTO vessel ostium and could be facilitated by use of a guide catheter extension. Finally, if aortocoronary dissection occurs, stopping antegrade contrast injections is critical to avoid extension and enlargement of the dissection (8).
Aortocoronary dissection during CTO PCI is most often treated with stenting (in 4 of 6 patients in our series). Stenting can “seal off” the entry point into the dissection plane and minimize the risk for subintimal space expansion. Occasionally, a covered stent may be required: of the 4 published aortocoronary dissection cases in CTO PCI series (9-11) one was treated with covered stent implantation (11) and the other 3 were treated conservatively (9,10). Among 107 published cases of aortocoronary dissection during PCI most (49.5%) were treated with stenting or conservatively (21.5%) although approximately 1 in 3 patients (29%) required surgery. In our opinion emergency surgery for aortocoronary dissection is not needed in the vast majority of cases and should only be recommended for the following two clinical scenarios: (a) occlusion of the dissected vessel with cessation of antegrade flow that cannot be restored percutaneously; and (b) extension of the dissection to the descending aorta.
The outcome of aortocoronary dissection during CTO PCI is relatively favorable: 5 of the 6 patients in our series had uneventful recovery, although one patient required emergency CABG. All 4 published aortocoronary dissection cases in CTO PCI series (9-11) recovered without complications. Similarly, in the overall literature of aortocoronary dissection during PCI most patients had uneventful recovery, however 8 of 107 patients (7.5%) died. Moreover, in a recently published case of aortocoronary dissection during right coronary artery CTO PCI the dissection extended to the suprarenal abdominal level involving the aortic arch and celiac branch and required emergent surgery (14).
Our study is limited by its retrospective and observational design and the relatively small number of patients involved. As is common in veteran populations, most of the included patients were men, however men constitute the majority of patients in most CTO PCI series.
In summary, our study suggests that aortocoronary dissection is an infrequent complication of CTO PCI, occurs more commonly during use of the retrograde approach and can be successfully treated with stenting in most cases, although occasionally emergency CABG may be required. Every effort should be undertaken to prevent aortocoronary dissections by avoiding contrast injection when the pressure waveform is dampened and avoiding retrograde guidewire advancement in the subaortic space during retrograde CTO PCI.
Supplementary Material
Acknowledgments
Dr. Michael: Supported by Cardiovascular Training Grant from the National Institutes of Health Award Number T32HL007360
Abbreviations
- CABG
Coronary Artery Bypass Graft surgery
- CTO
Chronic Total Occlusion
- MACE
Major Adverse Cardiac Events
- MI
Myocardial infarction
- PCI
Percutaneous Coronary Intervention
- Reverse CART
reverse controlled antegrade and retrograde tracking and dissection
- TEE
Transesophageal Echocardiography
Footnotes
Conflict of Interest:
Ms. Shorrock: none
Dr. Patel: none
Dr. Kotsia: none
Dr. Rangan: none
Dr. Abdullah: none
Dr. Grodin: none
Ms. Banerjee: none
Dr. Brilakis: consulting fees/speaker honoraria from St Jude Medical, Boston Scientific, Asahi, Janssen, Abbott Vascular, Sanofi, and Terumo; research support from Guerbet; spouse is an employee of Medtronic.
References
- 1.Christofferson RD, Lehmann KG, Martin GV, Every N, Caldwell JH, Kapadia SR. Effect of chronic total coronary occlusion on treatment strategy. Am J Cardiol. 2005;95:1088–91. doi: 10.1016/j.amjcard.2004.12.065. [DOI] [PubMed] [Google Scholar]
- 2.Fefer P, Knudtson ML, Cheema AN, Galbraith PD, Osherov AB, Yalonetsky S, Gannot S, Samuel M, Weisbrod M, Bierstone D. Current perspectives on coronary chronic total occlusions: the Canadian Multicenter Chronic Total Occlusions Registry. J Am Coll Cardiol. 2012;59:991–7. doi: 10.1016/j.jacc.2011.12.007. others. [DOI] [PubMed] [Google Scholar]
- 3.Joyal D, Afilalo J, Rinfret S. Effectiveness of recanalization of chronic total occlusions: a systematic review and meta-analysis. Am Heart J. 2010;160:179–87. doi: 10.1016/j.ahj.2010.04.015. [DOI] [PubMed] [Google Scholar]
- 4.Grantham JA, Jones PG, Cannon L, Spertus JA. Quantifying the early health status benefits of successful chronic total occlusion recanalization: Results from the FlowCardia's Approach to Chronic Total Occlusion Recanalization (FACTOR) Trial. Circ Cardiovasc Qual Outcomes. 2010;3:284–90. doi: 10.1161/CIRCOUTCOMES.108.825760. [DOI] [PubMed] [Google Scholar]
- 5.Grantham JA, Marso SP, Spertus J, House J, Holmes DR, Jr., Rutherford BD. Chronic total occlusion angioplasty in the United States. JACC Cardiovasc Interv. 2009;2:479–86. doi: 10.1016/j.jcin.2009.02.008. [DOI] [PubMed] [Google Scholar]
- 6.Patel VG, Brayton KM, Tamayo A, Mogabgab O, Michael TT, Lo N, Alomar M, Shorrock D, Cipher D, Abdullah S. Angiographic success and procedural complications in patients undergoing percutaneous coronary chronic total occlusion interventions: a weighted meta-analysis of 18,061 patients from 65 studies. JACC Cardiovasc Interv. 2013;6:128–36. doi: 10.1016/j.jcin.2012.10.011. others. [DOI] [PubMed] [Google Scholar]
- 7.Carstensen S, Ward MR. Iatrogenic aortocoronary dissection: the case for immediate aortoostial stenting. Heart Lung Circ. 2008;17:325–9. doi: 10.1016/j.hlc.2007.11.140. [DOI] [PubMed] [Google Scholar]
- 8.Brilakis ES, editor. A Step-By-Step Approach. Elsevier; Waltham, MA: 2013. Manual of Coronary Chronic Total Occlusion Interventions. [Google Scholar]
- 9.Rathore S, Katoh O, Matsuo H, Terashima M, Tanaka N, Kinoshita Y, Kimura M, Tsuchikane E, Nasu K, Ehara M. Retrograde percutaneous recanalization of chronic total occlusion of the coronary arteries: procedural outcomes and predictors of success in contemporary practice. Circ Cardiovasc Interv. 2009;2:124–32. doi: 10.1161/CIRCINTERVENTIONS.108.838862. others. [DOI] [PubMed] [Google Scholar]
- 10.Rathore S, Matsuo H, Terashima M, Kinoshita Y, Kimura M, Tsuchikane E, Nasu K, Ehara M, Asakura Y, Katoh O. Procedural and in-hospital outcomes after percutaneous coronary intervention for chronic total occlusions of coronary arteries 2002 to 2008: impact of novel guidewire techniques. JACC Cardiovasc Interv. 2009;2:489–97. doi: 10.1016/j.jcin.2009.04.008. others. [DOI] [PubMed] [Google Scholar]
- 11.Wu CJ, Fang HY, Cheng CI, Hussein H, Abdou SM, Youssef AA, Bhasin A, Yang CH, Chen CJ, Hsieh YK. The safety and feasibility of bilateral radial approach in chronic total occlusion percutaneous coronary intervention. Int Heart J. 2011;52:131–8. doi: 10.1536/ihj.52.131. others. [DOI] [PubMed] [Google Scholar]
- 12.Abdou SM, Wu CJ. Treatment of aortocoronary dissection complicating anomalous origin right coronary artery and chronic total intervention with intravascular ultrasound guided stenting. Catheter Cardiovasc Interv. 2011;78:914–9. doi: 10.1002/ccd.23021. [DOI] [PubMed] [Google Scholar]
- 13.Brilakis ES, Karmpaliotis D, Patel V, Banerjee S. Complications of chronic total occlusion angioplasty. Interventional Cardiology Clinics. 2012;1:373–389. doi: 10.1016/j.iccl.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 14.Liao MT, Liu SC, Lee JK, Chiang FT, Wu CK. Aortocoronary dissection with extension to the suprarenal abdominal aorta: a rare complication after percutaneous coronary intervention. JACC Cardiovasc Interv. 2012;5:1292–3. doi: 10.1016/j.jcin.2012.06.027. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.