Abstract
Background
The purpose of this study was to compare postoperative outcomes of pediatric patients with complicated appendicitis managed with or without a peripherally inserted central catheter (PICC).
Methods
Patients ≤18 years old in the Pediatric Health Information System database with complicated appendicitis that underwent appendectomy during their index admission in 2000–2012 were grouped by whether they had a PICC placed using relevant procedure and billing codes. Rates of subsequent encounters within 30 days of discharge along with associated diagnoses and procedures were determined. A propensity score matched (PSM) analysis was performed to account for differences in baseline exposures and severity of illness.
Results
We included 33,482 patients with complicated appendicitis, of whom 6,620 (19.8%) received a PICC and 26,862 (80.2%) did not. The PICC group had a longer post-operative length of stay (median 7 vs. 5 days, p<0.001), and were more likely to undergo intra-abdominal abscess drainage during the index admission (14.4% vs. 2.1%, p<0.001), and have a re-encounter (17.5% vs. 11.4%, p<0.001) within 30 days of discharge. However, in the PSM cohort (n=4,428 in each group), outcomes did not differ between treatment groups, although the PICC group did have increased odds for development of other post-operative complications (odds ratio=3.95, 95% confidence interval: 1.45, 10.71).
Conclusions
After accounting for differences in severity of illness by propensity score matching, patients managed with PICCs had a similar risk for nearly all post-operative complications, including re-encounters. Post-operative management of pediatric complicated appendicitis with a PICC is not clearly associated with improved outcomes.
Introduction
Approximately 30% of children diagnosed with acute appendicitis will be identified as having complicated appendicitis.(1) A standard component of the management of this disease is broad-spectrum antibiotic therapy.(2, 3) Recommendations for the management of complicated appendicitis in children published in the 1980s called for a 10-day inpatient course of parenteral triple-antibiotics.(4) Since then studies have demonstrated the safety and efficacy of using shorter time courses of antibiotics, single-agent regimens, and completing intravenous (IV) antibiotics at home using a peripherally inserted central catheter (PICC) compared to continued hospitalization.(5–8) Furthermore, there is now evidence that an oral (PO) antibiotic regimen is equivalent to IV administration with respect to disease-related complications, such as intra-abdominal abscesses and wound infections, while reducing overall costs.(9–12)
PICCs do have some potential advantages in hospitalized children including providing stable intravenous access which decreases the number peripheral IV insertions throughout the hospital course and allows for blood sample collection without phlebotomy. In addition, PICCs can be used to administer parenteral nutrition to patients who have prolonged post-operative ileus. Despite these potential in-hospital benefits, PICCS are associated with increased costs and health care utilization and several PICC related complications including thrombosis, line fractures, and both superficial and bloodstream infections.(13, 14) These complications occur more commonly in patients receiving more frequent doses of medications and those who have the line in place for shorter periods of time.(14)
With studies demonstrating equivalence between prolonged home IV antibiotics with a PICC to oral antibiotics in patients with complicated appendicitis, PICC associated risks may outweigh their potential benefits in terms of improving post-operative outcomes. The objective of this study was to compare postoperative outcomes of a multi-institutional cohort of pediatric patients with complicated appendicitis managed with or without a PICC.
Methods
Cohort and Treatment Group Identification
This multi-institutional cohort study utilized the Pediatric Health Information System (PHIS), an administrative database managed by the Children’s Hospital Association (CHA). The database contains inpatient and emergency department data including demographic and payer information, International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes, and date-stamped procedure and billing codes from 44 free-standing children’s hospitals. Encrypted medical record numbers allow for longitudinal tracking of data at the same institution that spans multiple encounters.
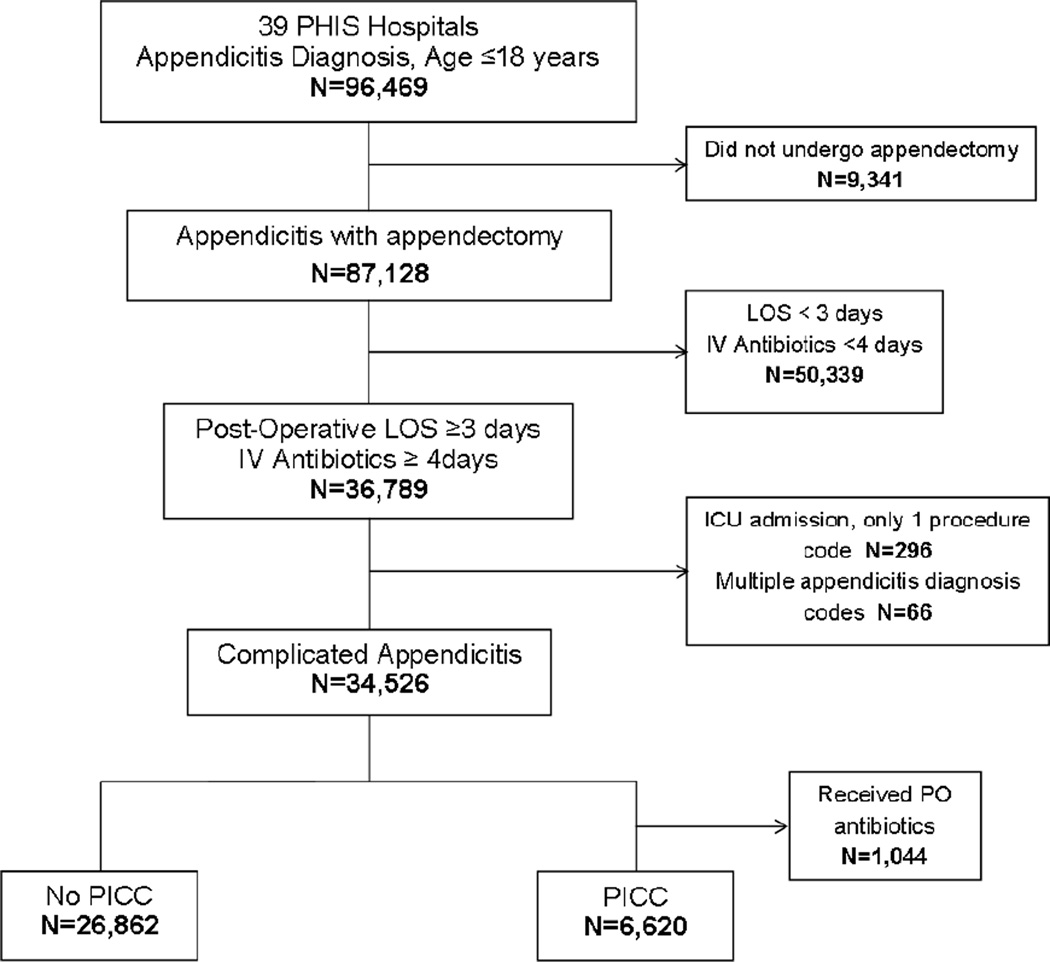
The complicated appendicitis cohort was defined by adopting previously published criteria.(15) Figure 1 displays the cohort development algorithm. Briefly, the complicated appendicitis cohort was developed by including all patients less than or equal to 18 years of age with a diagnosis code for acute appendicitis (ICD-9-CM diagnosis codes 540.0, 540.1, and 540.9). Patients initially managed non-operatively were excluded by requiring that patients also have a relevant procedure code for appendectomy (ICD-9-CM procedure codes 47.01, 47.09, 54.11, and 54.21) during the same admission. Additionally during the index admission, the postoperative length of stay (LOS) had to be at least 3 days and patients had to receive at least 4 days of IV antibiotics.
Figure 1. Identification of study cohort with complicated appendicitis.
Note: ICD-9-CM diagnosis codes for appendicitis: 540.0, 540.1, 540.9; ICD-9-CM procedure codes for appendectomy: 47.01, 47.09, 54.11, 54.21. PHIS=Pediatric Health Information System; LOS=length of stay; IV=intravenous; ICU=intensive care unit; PO=oral; PICC=peripherally inserted central catheter.
Treatment group assignment was based on a combination of billing charges, procedure codes, and if the patient was in an intensive care unit (ICU) during their index admission. In order to distinguish a PICC from a standard central venous catheter (CVC), patients who had an ICU stay were required to have both the ICD-9-CM procedure code (38.93) and a billing charge for a PICC, while those who were never in the ICU could have either the procedure code or a billing charge. This strategy was used to minimize inclusion of patients with CVCs. The patients meeting these criteria comprised the “PICC” treatment group, while all others were in the “No PICC” group. PICC placement was assumed to be a surrogate for eventual discharge with at-home IV antibiotic treatment. In order to minimize the inclusion of patents who had their PICC removed prior to discharge, we excluded all patients in the PICC group that received any post-operative doses of oral antibiotics as this would be associated with a higher likelihood of having the PICC removed and being discharged with oral antibiotic therapy.
Data Elements and Statistical Analysis
Baseline characteristics examined included demographics and clinical characteristics of the first admission for appendicitis. The primary outcome of this study was the rate of subsequent encounters (emergency department or inpatient) within 30 days of discharge from the index admission. Additional outcomes and procedures examined during the re-encounter included superficial or intra-abdominal abscess, surgical site infection (SSI), venous thrombosis (VT), pulmonary embolism (PE), vascular access complications, gastrointestinal (GI) complications, complicated wound closures, and repeat operations. Intra-abdominal abscesses were evaluated through a combination of billing charges for abdominal imaging studies, IV antibiotics, and associated ICD-9-CM procedure codes. An abscess/phlegmon was considered present if an imaging study was performed with IV antibiotic administration alone or with a related procedure, while concern for abscess/phlegmon referred to an abdominal imaging study being performed within 30 days of discharge without antibiotics or a related procedure.
Comparisons between the treatment groups were analyzed with the Wilcoxon Rank Sum test for continuous variables and the Pearson chi square or Fisher’s Exact test for categorical variables. A propensity score matched (PSM) analysis was performed in order to compare patients in each treatment group with similar characteristics, including several severity of illness factors. Variables from the initial admission that were significantly different between the groups (p<0.05) included in the propensity score matching were: age, gender and race; post-operative LOS; the hospital-specific proportion of patients in the study cohort with a PICC; use of parenteral nutrition, mechanical ventilation, vasopressors, or transfusions; intra-abdominal abscess drainage procedures; and complications that occurred during the index admission including VT, PE, PICC complications, and post-operative infectious or gastrointestinal complications. Patients with and without a PICC were matched on the logit of their propensity score using 1:1 nearest neighbor matching within calipers of width equal to 0.25 times the standard deviation of the logit of the propensity score.(16) Propensity score matching was performed using the “gmatch” macro.(17) Patients without a match were excluded from further analyses to lessen the risk of bias to due non-exchangeability of patients between treatment groups. Balance between the PSM treatment groups in all factors included in the propensity score matching was observed by ensuring the standardized differences were less than or equal to 0.10. Odds ratios (OR) and 95% confidence intervals (CI) were estimated from logistic regression mixed effects models for the overall and PSM cohorts. These models included random intercepts for hospitals in order to adjust for variability in management between institutions.
All analyses were repeated on a subset of patients with a ICD-9-CM diagnosis code for acute appendicitis with generalized peritonitis (540.0) or with peritoneal abscess (540.1) only (excluded acute appendicitis without mention of peritonitis; 540.9). This sub-analysis was done to reduce potential variability in severity of illness between treatment groups based on diagnosis code because those with more severe illness may be more likely to have a PICC. All analyses were performed with SAS 9.3 (Carey, NC) and a p<0.05 was considered statistically significant.
Results
Overall Cohort
At the 39 included PHIS hospitals, 96,469 patients had one of the three ICD-9-CM codes for appendicitis, 87,128 (90.3%) also had a procedure code for appendectomy during the same admission, and 34,526 (35.8%) met criteria for complicated appendicitis (Figure 1). Of the patients with complicated disease, 7,664 patients had a PICC placed during the index admission but 1,044 were excluded because they received oral (PO) antibiotics post-operatively. The final cohort included 33,482 patients of which 6,620 (19.8%) had a PICC placed during the index admission and 26,862 (80.2%) did not.
Overall, there were significant differences between the groups for all baseline characteristics and factors associated with the index admission with the exception of gender (Table 1). Patients in the PICC group had a longer post-operative and total hospital LOS, were more likely to have a complex or chronic medical problem, received mechanical ventilation, TPN, vasopressors, or transfusions, or to have been in an ICU during the index admission (Table 1). Patients in the PICC group also experienced more post-operative complications during the index admission, including undergoing intra-abdominal abscess drainage procedures (Table 2).
Table 1.
Baseline characteristics and factors associated with the index admission for the overall cohort and the propensity score matched cohort. Results listed as n (%) or median (inter-quartile range).
| Overall Cohort | Propensity Score Matched Cohort | |||||
|---|---|---|---|---|---|---|
| Variable | PICC (n=6,620) |
No PICC (n=26,862) |
P | PICC (n=4,428) |
No PICC (n=4,428) |
P |
| Age (years) | 9 (5–12) | 9 (6–12) | <0.001 | 9 (5–12) | 9.0 (5–12) | 0.596 |
| Female | 2,684 (40.5) | 10,850 (40.4) | 0.821 | 1,830 (41.3) | 1,814 (41.0) | 0.730 |
| Race | ||||||
| White | 4,413 (66.7) | 17,858 (66.5) | 3,000 (67.8) | 3,020 (68.2) | ||
| Black | 1,274 (19.2) | 2,271 (8.5) | <0.001 | 552 (12.5) | 503 (11.4) | 0.245 |
| Other/unknown | 933 (14.4) | 6,733 (25.1) | 876 (19.8) | 905 (20.4) | ||
| Acute appendicitis | ||||||
| with generalized peritonitis | 3,842 (58.0) | 16,280 (60.6) | 2,713 (61.3) | 2,750 (62.1) | ||
| with peritoneal abscess | 2,433 (36.8) | 5,134 (19.1) | <0.001 | 1,431 (32.3) | 1,404 (31.7) | 0.709 |
| without mention of peritonitis | 345 (5.2) | 5,448 (20.3) | 284 (6.4) | 274 (6.2) | ||
| Intensive care unit | 261 (3.9) | 483 (1.8) | <0.001 | 146 (3.3) | 144 (3.3) | 0.905 |
| Mechanical ventilator | 139 (2.1) | 95 (0.4) | <0.001 | 66 (1.5) | 47 (1.1) | 0.072 |
| Total parenteral nutrition | 2,635 (39.8) | 1,157 (4.3) | <0.001 | 1,116 (25.2) | 968 (21.9) | <0.001 |
| Transfusion | 141 (2.1) | 169 (0.6) | <0.001 | 58 (1.3) | 53 (1.2) | 0.633 |
| Vasopressors | 274 (4.1) | 479 (1.8) | <0.001 | 146 (3.3) | 137 (3.1) | 0.587 |
| Complex chronic condition | 302 (4.6) | 919 (3.4) | <0.001 | 195 (4.4) | 201 (4.5) | 0.758 |
| Post-operative LOS (days) | 7 (5–10) | 5 (4–6) | <0.001 | 6 (5–9) | 6 (5–8) | <0.001 |
| Total LOS (days) | 7 (5–11) | 5 (4–6) | <0.001 | 7 (5–9) | 6 (5–9) | 0.019 |
Note: PICC=peripherally inserted central catheter; LOS=length of stay.
Bold p-values indicate significant result (P<0.05)
Table 2.
Complications during the index admission for both the overall cohort and the propensity score matched cohort. Results listed as n (%) or median (inter-quartile range).
| Overall Cohort | Propensity Score Matched Cohort | |||||
|---|---|---|---|---|---|---|
| Variable | PICC (n=6,620) |
No PICC (n=26,862) |
P | PICC (n=4,428) |
No PICC (n=4,428) |
P |
| Thrombosis | 27 (0.3) | 6 (0.0) | <0.001 | 7 (0.2) | 4 (0.1) | 0.549 |
| Vascular access complication | 33 (0.5) | 9 (0.0) | <0.001 | 10 (0.2) | 7 (0.2) | 0.466 |
| Pulmonary embolism | 0 (0.0) | 2 (0.0) | 1.000 | 0 (0.0) | 2 (0.0) | 0.500 |
| Intra-abdominal abscess drainage | 955 (14.4) | 557 (2.1) | <0.001 | 446 (10.1) | 401 (9.1) | 0.104 |
| Post-operative GI complications | 1,133 (17.1) | 2,768 (10.3) | <0.001 | 640 (14.5) | 668 (15.1) | 0.402 |
| Post-operative infection | 395 (6.0) | 451 (1.7) | <0.001 | 188 (4.2) | 184 (4.2) | 0.832 |
| Other post-operative complicationsa | 137 (2.1) | 166 (0.6) | <0.001 | 58 (1.3) | 46 (1.0) | 0.237 |
| Antibiotics complications | 58 (0.9) | 129 (0.5) | <0.001 | 29 (0.7) | 36 (0.8) | 0.384 |
Note: PICC=peripherally inserted central catheter; GI=gastrointestinal.
This variable includes: bleeding, shock, accidental puncture, disruption of wound, fistula, and non-healing wound.
Bold p-values indicate significant result (P<0.05)
In the 30 days after discharge from the index admission, patients in the PICC group were more likely to have a subsequent encounter, an abscess or concern for an abscess, an additional operation, or one of several other complications (Table 3). Vascular access complications including VT, both during the initial encounter and subsequent encounters within 30 days, were rare (Table 2).
Table 3.
Outcomes occurring within 30 days after discharge from the index admission based on either procedure codes or diagnosis codes for the overall cohort and the propensity score matched cohort.
| Overall Cohort | Propensity Score Matched Cohort | |||||
|---|---|---|---|---|---|---|
| Variable | PICC (n=6,620) |
No PICC (n=26,862) |
Odds Ratio 95% CI |
PICC (n=4,428) |
No PICC (n=4,428) |
Odds Ratio 95% CI |
| Re-encounter | 1,159 (17.5) | 3,064 (11.4) | 1.65 (1.53–1.78) | 710 (16.0) | 663 (15.0) | 1.08 (0.97–1.22) |
| Superficial abscess | 7 (0.1) | 18 (0.1) | 1.53 (0.64–3.66) | 3 (0.1) | 8 (0.2) | 0.09 (0.01–0.62) |
| Intra-abdominal abscess | ||||||
| Concern for abscess (imaging only) | 978 (12.8) | 1,966 (7.3) | 2.14 (1.95–2.35) | 568 (12.8) | 471 (10.6) | 1.24 (1.08–1.41) |
| Abdominal imaging + antibiotics | 792 (10.3) | 1,619 (6.0) | 6.23 (5.17–7.50) | 467 (10.5) | 403 (9.1) | 1.18 (1.02–1.37) |
| Abdominal imaging + drainage | 284 (3.7) | 192 (0.7) | 2.84 (2.56–3.15) | 131 (3.0) | 120 (2.7) | 1.09 (0.85–1.41) |
| Any re-operation | 156 (2.0) | 148 (0.6) | 4.36 (3.48–5.47) | 69 (1.6) | 77 (1.7) | 0.89 (0.65–1.24) |
| Laparotomy | 37 (0.5) | 51 (0.2) | 2.91 (1.90–4.47) | 18 (0.4) | 31 (0.7) | 0.57 (0.31–1.04) |
| Lysis of adhesions | 91 (1.2) | 71 (0.3) | 5.29 (3.88–7.21) | 42 (0.9) | 27 (0.6) | 1.56 (0.96–2.54) |
| Dehiscence repair | 3 (0.0) | 0 (0.0) | -- | 1 (0.0) | 0 (0.0) | -- |
| Delayed closure | 4 (0.1) | 3 (0.0) | 5.41 (1.21–24.19) | 1 (0.0) | 3 (0.1) | 0.33 (0.03–3.21) |
| Thrombosis | 2 (0.0) | 3 (0.0) | 2.70 (0.45–16.19) | 0 (0.0) | 2 (0.0) | -- |
| Vascular access complication | 6 (0.1) | 2 (0.0) | 12.18 (2.46–60.37) | 1 (0.0) | 1 (0.0) | 1.00 (0.06–16.01) |
| Pulmonary embolism | 0 (0.0) | 2 (0.0) | -- | 0 (0.0) | 2 (0.0) | -- |
| GI complications | 223 (2.9) | 426 (1.6) | 2.15 (1.82–2.53) | 115 (2.6) | 123 (2.8) | 0.93 (0.72–1.21) |
| Post-operative infection | 79 (1.0) | 73 (0.3) | 4.41 (3.27–5.95) | 29 (0.7) | 29 (0.7) | 0.99 (0.59–1.65) |
| Other post-operative complicationsa | 28 (0.4) | 26 (0.1) | 3.20 (1.58–6.48) | 11 (0.2) | 6 (0.1) | 3.95 (1.45–10.71) |
| Antibiotics complications | 12 (0.2) | 26 (0.1) | 1.86 (0.94–3.70) | 4 (0.1) | 6 (0.1) | 0.67 (0.19–2.36) |
Note: PICC=peripherally inserted central catheter; CI=confidence interval; GI=gastrointestinal; abscess categories were not mutually exclusive; odds ratios are unadjusted and were estimated using logistic mixed effects models.
This variable includes: bleeding, shock, accidental puncture, disruption of wound, fistula, and non-healing wound.
Bold p-values indicate significant result (P<0.05).
All results were similar in the subgroup analysis of patients with diagnosis codes for acute appendicitis with generalized peritonitis (540.0) or with peritoneal abscess (540.1) only.
Propensity Score Matched Cohort
Propensity score matching produced two groups of 4,428 patients each. Baseline characteristics were similar between both groups, including the different diagnoses for acute appendicitis that indicate severity of illness (Table 1). Although some of the characteristics of the index admission, such as LOS and use of TPN, remained significantly different, the standardized differences in all pre-treatment variables between the two treatment groups were less than 10%. Complications that occurred during the index admission were also similar for both groups in the PSM cohort (Table 2). Of note, we could not match 33% of patients in the PICC group because there were insufficient numbers of patients in the No PICC group with propensity scores high enough to match these patients
There was no significant difference between the matched treatment groups in proportions of patients who had a repeat encounter within 30 days (Table 3). Furthermore, other outcomes during the subsequent encounter, such as additional operations or post-operative infections, were statistically similar between the two groups. The PICC group did have higher proportions of patients who were evaluated with imaging due to concern for intra-abdominal abscess and who were treated with antibiotics for an abscess, although the two groups were similar for the proportion who underwent abscess drainage at a subsequent encounter.
Regression analysis of the PSM cohort demonstrated that patients who had a PICC placed during the index admission had lower odds of developing a superficial abscess (OR=0.09, 95% CI: 0.01, 0.62); however, they had higher odds for concern for abscess (OR=1.24, 95% CI: 1.08, 1.41) and for abscess treated with antibiotics only (OR=1.18, 95% CI: 1.02, 1.37). They also had a higher risk for a composite group of other post-operative complications including bleeding, shock, accidental puncture, disruption of wound, fistula, and non-healing wound (OR=3.95, 95% CI: 1.45,10.71). There were no other outcomes with significantly different odds for either treatment group (Table 3). Vascular access complications were also rare in the propensity score matched groups (Table 2).
Findings were similar in the subset analysis of patients with diagnosis codes for acute appendicitis with generalized peritonitis (540.0) or with peritoneal abscess (540.1) only, except that in this sub-group analysis, patients with a PICC placed during the index admission now had a significantly higher odds of a subsequent encounter (OR=1.15, 95% CI: 1.01,1.29).
Discussion
After accounting for disparities in baseline characteristics, severity of illness, and complications that occurred during the index admission including development of intra-abdominal abscesses between the two treatment groups using propensity score matching, use of a PICC in the management of patients with complicated appendicitis was not associated with improved outcomes within 30 days after discharge. Rates of re-encounters and additional operations were similar in both groups. Patients with PICCs were less likely to develop a superficial abscess, but were more likely to develop other post-operative complications, be evaluated for concern for an intra-abdominal abscess, or be treated for an intra-abdominal abscess with antibiotics only in the 30 days after hospital discharge.
The last several decades have seen a progressive shift in management of complicated appendicitis from a prolonged course of IV antibiotics administered on an inpatient basis to expedited discharge followed by prolonged antibiotic therapy, administered either IV or PO.(4–12) Placement of a PICC for prolonged IV antibiotic administration can cause discomfort for children, is associated with higher costs, and exposes patients to the potential for catheter associated complications including thrombosis, infection, or line breakage.(13, 14) PICCs were advocated for post-operative care of patients with complicated appendicitis as a way of continuing long-term antibiotic regimens while allowing children to go home sooner and thus reducing total costs.(5) Since then, several studies in children have supported conversion to oral antibiotics for prolonged therapy. Gollin, et al. (2002) reported their successful trial of a treatment strategy utilizing early discharge with oral antibiotics, with the rate of both wound infections and intra-abdominal abscesses less than 5%.(10) Adibe, et al. (2008) retrospectively reviewed 47 patients treated with oral trimethoprim-sulfamethoxazole and metronidazole compared to 102 patients treated with IV ampicillin-sulbactam for a total 14-day course and found both groups to be similar in terms of the rate of intra-abdominal abscess formation.(11) In that study, oral antibiotic therapy was associated with a significant cost savings, although the IV group did have a significantly longer average initial hospital LOS. Rice, et al. (2001), and Fraser, et al. (2010) both carried out similarly designed randomized controlled trials (RCT) comparing a complete IV antibiotic course to a combined course of IV converted to PO antibiotics.(9, 12) The former study looked primarily at “clearance of infection” which included the possibility of complications, while the latter focused on intra-abdominal abscess formation. Both studies observed equivalence between the two groups with respect to their primary outcomes.
A large multi-institutional RCT to address the role of PICCs in complicated appendicitis would be difficult and expensive to perform. In addition, there may now be a lack of equipoise as many centers have shifted their practice towards using oral antibiotics at discharge and limiting PICC usage. Our study adds to the literature by performing a large multi-institutional cohort study comparing differences in outcomes based on utilization of a PICC line in the management of children with complicated appendicitis. Using propensity score matching to simulate the effects of randomization, we developed and compared two large groups with similar baseline characteristics and severity of illness.
The present study found that across 39 free-standing children’s hospitals, approximately 20% of patients with complicated appendicitis were managed with a PICC. These patients were more likely to have had critical interventions during their index admission including mechanical ventilation, blood transfusions, and drainage procedures for intra-abdominal abscesses. They demonstrated an increased severity of illness by having higher percentages of repeat encounters following discharge, post-operative infections and GI complications, and additional surgical procedures including exploratory laparotomy and complicated wound closures. In order to account for these baseline differences we performed a propensity score matched (PSM) analysis. Patients with one treatment (PICC) were matched to patients receiving the other treatment (No PICC) who had similar baseline exposures. This allowed us to determine if utilization of a PICC line provided any benefit in terms of post-operative complications. The results of this analysis demonstrated that the two groups were similar in almost all outcomes, including the proportion that had a repeat encounter or an additional surgical procedure. It must be pointed out that the number of complications that can be attributed to the PICC itself were very low, likely owing to the short amount of time these lines are in place. In addition, PICCs may have several benefits in selected complex patients including allowing for parenteral nutrition administration and blood draws without phlebotomy and providing stable access for intravenous medication administration throughout a prolonged hospitalization. Despite this, given the increased costs and risks, and lack of demonstrated improvement in outcomes related to appendicitis, the universal use of PICCs in the management of children with complicated appendicitis should be re-evaluated with PICC use reserved for selected complex patients..
This study has several limitations. First, errors and misclassifications of data within an administrative dataset can occur. However, administrative databases with rigorous quality control measures to minimize errors and misclassifications, such as PHIS, are being increasingly utilized to perform large comparative effectiveness studies, similar to this one, which have affected changes in practice.(18–21) Second, the temporal relationship between PICC placement and certain factors/outcomes (e.g. SSI) within the same encounter cannot be determined. This was accounted for in our study by considering these variables as outcomes only if they occurred at a subsequent hospital encounter. Third, longitudinal tracking of individual patients can only be done if a patient returns to the hospital of their index admission; therefore, any patient that returned to a different hospital will not be included in this analysis. The effect of this on our analysis is difficult to measure; however, when evaluating short-term outcomes 30-days) following a severe surgical illness, such as complicated appendicitis, we believe that the effect will be minimal because most patients are likely to return to the same children’s hospital where their initial care had taken place in the event of a subsequent problem. Fourth, to account for differences in severity of illness of patients managed with and without a PICC, we performed a PSM analysis to compare groups with similar baseline characteristics. The presence of unmeasured or unaccounted-for factors that contribute to treatment choice may confound the interpretation of these analyses; to minimize this possibility, we included as many known markers of severity illness that could be derived from the PHIS as possible including the use of post-operative length of stay and complications (e.g. abscess) during the index admission.
In conclusion, after matched analysis, management of complicated appendicitis with a PICC was not clearly associated with improved outcomes. These findings, in combination with other recent studies, suggest that, although PICCs may have potential benefits in the management of selected complex patients, treatment protocols that include universal PICC placement for complicated appendicitis in children should be reconsidered.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errorsmaybe discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions: JP Sulkowski: conception and design, analysis and interpretation, writing the article; L Asti: conception and design, analysis and interpretation, data collection, writing the article; JN Cooper: conception and design, analysis and interpretation, critical revision; BD Kenney: conception and design, critical revision; MV Raval: conception and design, critical revision; SJ Rangel: conception and design, critical revision; KJ Deans: conception and design, critical revision; PC Minneci: conception and design, analysis and interpretation, critical revision, obtaining funding.
References
- 1.Ponsky TA, Huang ZJ, Kittle K, Eichelberger MR, Gilbert JC, Brody F, et al. Hospital- and patient-level characteristics and the risk of appendiceal rupture and negative appendectomy in children. JAMA. 2004;292(16):1977–1982. doi: 10.1001/jama.292.16.1977. [DOI] [PubMed] [Google Scholar]
- 2.Solomkin JS, Mazuski JE, Bradley JS, Rodvold KA, Goldstein EJ, Baron EJ, et al. Diagnosis and management of complicated intra-abdominal infection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society of America. Surg Infect. 2010;11(1):79–109. doi: 10.1089/sur.2009.9930. [DOI] [PubMed] [Google Scholar]
- 3.Lee SL, Islam S, Cassidy LD, Abdullah F, Arca MJ. Antibiotics and appendicitis in the pediatric population: an American Pediatric Surgical Association Outcomes and Clinical Trials Committee systematic review. J Pediatr Surg. 2010;45(11):2181–2185. doi: 10.1016/j.jpedsurg.2010.06.038. [DOI] [PubMed] [Google Scholar]
- 4.Schwartz MZ, Tapper D, Solenberger RI. Management of perforated appendicitis in children. The controversy continues. Ann Surg. 1983;197(4):407–411. doi: 10.1097/00000658-198304000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stovroff MC, Totten M, Glick PL. PIC lines save money and hasten discharge in the care of children with ruptured appendicitis. J Pediatr Surg. 1994;29(2):245–247. doi: 10.1016/0022-3468(94)90327-1. [DOI] [PubMed] [Google Scholar]
- 6.Hoelzer DJ, Zabel DD, Zern JT. Determining duration of antibiotic use in children with complicated appendicitis. Pediatr Infect Dis J. 1999;18(11):979–982. doi: 10.1097/00006454-199911000-00009. [DOI] [PubMed] [Google Scholar]
- 7.Nadler EP, Reblock KK, Ford HR, Gaines BA. Monotherapy versus multi-drug therapy for the treatment of perforated appendicitis in children. Surg Infect. 2003;4(4):327–333. doi: 10.1089/109629603322761382. [DOI] [PubMed] [Google Scholar]
- 8.Alamili M, Gogenur I, Rosenberg J. Oral antibiotics for perforated appendicitis is not recommended. Dan Med Bull. 2010;57(9):A4177. [PubMed] [Google Scholar]
- 9.Rice HE, Brown RL, Gollin G, Caty MG, Gilbert J, Skinner MA, et al. Results of a pilot trial comparing prolonged intravenous antibiotics with sequential intravenous/oral antibiotics for children with perforated appendicitis. Arch Surg. 2001;136(12):1391–1395. doi: 10.1001/archsurg.136.12.1391. [DOI] [PubMed] [Google Scholar]
- 10.Gollin G, Abarbanell A, Moores D. Oral antibiotics in the management of perforated appendicitis in children. Am Surg. 2002;68(12):1072–1074. [PubMed] [Google Scholar]
- 11.Adibe OO, Barnaby K, Dobies J, Comerford M, Drill A, Walker N, et al. Postoperative antibiotic therapy for children with perforated appendicitis: long course of intravenous antibiotics versus early conversion to an oral regimen. Am J Surg. 2008;195(2):141–143. doi: 10.1016/j.amjsurg.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 12.Fraser JD, Aguayo P, Leys CM, Keckler SJ, Newland JG, Sharp SW, et al. A complete course of intravenous antibiotics vs a combination of intravenous and oral antibiotics for perforated appendicitis in children: a prospective, randomized trial. J Pediatr Surg. 2010;45(6):1198–1202. doi: 10.1016/j.jpedsurg.2010.02.090. [DOI] [PubMed] [Google Scholar]
- 13.Thiagarajan RR, Ramamoorthy C, Gettmann T, Bratton SL. Survey of the use of peripherally inserted central venous catheters in children. Pediatrics. 1997;99(2):E4. doi: 10.1542/peds.99.2.e4. [DOI] [PubMed] [Google Scholar]
- 14.Barrier A, Williams DJ, Connelly M, Creech CB. Frequency of peripherally inserted central catheter complications in children. Pediatr Infect Dis J. 2012;31(5):519–521. doi: 10.1097/INF.0b013e31824571b0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rice-Townsend S, Hall M, Barnes JN, Lipsitz S, Rangel SJ. Variation in Risk-Adjusted Hospital Readmission After Treatment of Appendicitis at 38 Children's Hospitals: An Opportunity for Collaborative Quality Improvement. Ann Surg. 2012;257(4):758–765. doi: 10.1097/SLA.0b013e318268a663. [DOI] [PubMed] [Google Scholar]
- 16.Faries DE, Leon AC, Haro JM, Obenchain RL. Analysis of Observational Health Care Data Using SAS. Cary, NC: SAS Institute; 2010. [Google Scholar]
- 17.Kosanke J, Bergstralh E. GMATCH. Mayo Clinic Division of Biomedical Statistics and Informatics. 2004 [Google Scholar]
- 18.Goldin AB, Sawin RS, Garrison MM, Zerr DM, Christakis DA. Aminoglycoside-based triple-antibiotic therapy versus monotherapy for children with ruptured appendicitis. Pediatrics. 2007;119(5):905–911. doi: 10.1542/peds.2006-2040. [DOI] [PubMed] [Google Scholar]
- 19.Tanaka ST, Grantham JA, Thomas JC, Adams MC, Brock JW, 3rd, Pope JCt. A comparison of open vs laparoscopic pediatric pyeloplasty using the pediatric health information system database--do benefits of laparoscopic approach recede at younger ages? J Urol. 2008;180(4):1479–1485. doi: 10.1016/j.juro.2008.06.044. [DOI] [PubMed] [Google Scholar]
- 20.Coffin SE, Leckerman K, Keren R, Hall M, Localio R, Zaoutis TE. Oseltamivir shortens hospital stays of critically ill children hospitalized with seasonal influenza: a retrospective cohort study. The Pediatr Infect Dis J. 2011;30(11):962–966. doi: 10.1097/INF.0b013e318232ede9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zaoutis T, Localio AR, Leckerman K, Saddlemire S, Bertoch D, Keren R. Prolonged intravenous therapy versus early transition to oral antimicrobial therapy for acute osteomyelitis in children. Pediatrics. 2009;123(2):636–642. doi: 10.1542/peds.2008-0596. [DOI] [PMC free article] [PubMed] [Google Scholar]