Abstract
Objective
To determine if Instrumental Activity of Daily Living (IADL) Limitation Stages can distinguish among elderly, community-dwelling people with high likelihoods to have fallen once and more than once.
Design
Cross-sectional survey.
Setting
A nationally representative sample from the Second Longitudinal Study of Aging (LSOA II).
Participants
Included were 7,401 community-dwelling persons 70 years of age and older.
Methods
The association of falling once and more than once within the past 12 months and five stages of increasing IADL limitation was explored using a multinomial logistic regression model controlling for demographics, education, perceived lack of home accessibility features, and health conditions. Samples proportions were weighted to reflect prevalence in the US population of 1994.
Main Outcome Measures
Subjects' recall of fall history. There were three categories for this variable: no fall, falling once, and falling more than once in the past 12 months.
Results
Compared to IADL stage 0, the adjusted relative risk ratio of falling once peaked at IADL stage II at 2.0 (95% confidence interval (CI), 1.5-2.6), and those at IADL stage III had a relative risk ratio of 1.8 (95% CI, 1.3-2.6). The relative risk ratio of falling more than once was 2.1 (95% CI, 1.7-2.6), 4.0 (95% CI, 3.0-5.3), 3.7 (95% CI, 2.8-5.0), and 2.7 (95% CI, 1.5-4.9) for IADL stages I, II, III, and IV, respectively, treating IADL stage 0 as reference.
Conclusions
IADL Limitation Stages could represent a powerful and practical tool for screening patients in the US elderly population according to falls risk. Clinical implementation and prospective testing for validation as a screening tool would be necessary.
Keywords: Falls, screening tool, elderly, instrumental activities of daily living, risk assessment
Introduction
Falls amongst the elderly is a growing problem especially as the population ages. According to the US Department of Health and Human Services' Administration of Aging, 39.6 million Americans, or 12.9% of the US population, were 65 years or older in 2009; by 2030 that number is expected to increase to 72.1 million representing 19% of the population.1 Health care providers will be forced to address this problem as falls are very costly to the healthcare system, and therefore a problem that healthcare providers cannot ignore. A systematic review of peer-reviewed journals found that non-fatal and fatal falls in the US amongst people aged ≥60 years cost $23.3 billion (2008 dollars).2
Potential reasons why older adults fall are multi-dimensional. Factors associated with the natural aging process, various disease processes, and poly-pharmacy have been implicated.3-7 Therefore assessment for falls risk, i.e., which patient is more at risk to fall, can be difficult and often time consuming. Many falls risk assessment tools exist; however, we are unaware of one that has been validated based on Instrumental Activities of Daily Living (IADLs) and recommended for use in the clinical setting. History of previous falls, use of multiple medications, vision testing, and testing of strength, balance, and reaction time have been analyzed as items to be assessed in falls risk assessment tools.8-14 Asking about a patient's ability to complete their Activities of Daily Living (ADLs) and/or IADLs, however; may be a simpler way of assessing falls risk as it takes into consideration an individual's physical and cognitive abilities. While ADLs are defined as everyday routines generally involving functional mobility and personal care such as bathing, dressing, toileting, and meal preparation, IADLs are the six daily tasks of using the telephone, managing money, preparing meals, doing light housework, shopping, and doing heavy housework that require higher, intact cognitive abilities that enable a patient to live independently in the community. Another systematic literature review of articles looked at the socio-demographic characteristics in the elderly who are at risk for falls and found that difficulties in at least one ADL or IADL double the risk of falling.15
The concept of staging IADLs stemmed from a simple principle first expressed by Katz et al. who looked at ADLs: “loss of function would begin with those activities which are most complex and least basic, while those functions which are most basic and least complex could be retained to the last.”18 In the 1960's, Lawton and Brody were amongst the first to assess IADLs and its impact on the ability of older people to live in the community independently.19 Since then, other researchers have looked at both ADLs and IADLs and have demonstrated a hierarchy of functional loss. Njegovan et al. most notably looked at cognitive decline and loss of independence for ADL and IADL tasks and confirmed that there is a tendency for IADLs to be lost at higher cognitive levels compared with ADLs.21 Stineman et al., building on these previous studies along with the recognition that typical global measures of activity limitation obscure the types of activities limited, created a two-dimensional Activity Limitation Staging system with both ADL and IADL stages that expresses the severity and types of activities limited across the broad self-care and domestic life domains.22
Our study mirrors that of Henry-Sánchez et al. who utilized the Activity Limitation Staging system22 and found a strong association with history of falling.20 Given this known association, our study will utilize the Instrumental Activity Limitation Staging system22 to determine if similar associations exists with IADLs, and if not, how those patterns of association differ for IADL stages. Based on findings of ADL association, we hypothesized that as stages of IADL limitation increase, the probability of having a history of one fall and of more than one fall will also increase. This hypothesis recognizes that elderly people's cognitive and physical impairments, as they interact with their environments, are associated with IADL limitations and that these limitations combined with their need to manage their lives generate falling risks.
Methods
This study was approved by the institutional review board at the University of Pennsylvania.
Description of Data
Data were originally collected under the Second Longitudinal Study of Aging (LSOA II),24 a prospective study of a complex multistage cohort representative US sample of 9,447 community-dwelling persons aged 70 and older. Respondents were drawn from all sample persons (SPs) interviewed during the 1994 National Health Interview Survey (NHIS) core and were 70 at the time of the LSOA II baseline interview. The NHIS core was linked to the disability supplement follow-back survey (NHIS-D) that re-interviewed people with impairments or disabilities between 6 months and 1.5 years after the core. Many government agencies worked together to develop the NHIS-D follow-back survey after passage of the Americans with Disabilities Act (ADA) in 1990 when it was recognized that there was little information available to help guide national disability policy. The NHIS-D included questionnaires that addressed the administrative, social, and medical aspects of disability and the problems and environmental barriers individuals faced. The data used for this manuscript were primarily from the baseline LSOA II, with additional context-rich information about disability drawn from the NHIS-D follow-back survey occurring at the same time. The LSOA II was intended to provide information on the causes and correlations of changes in health and functioning. Although attempts were made to interview the SP, close proxy respondents (living in the same household) provided information when the SP could not be interviewed.
Study Population
Of the 9,447 community-dwelling persons in the LSOA II baseline, 1,999 (21.2%) did not answer one or more IADL questions thus IADL stages were derived from 7,448 (78.8%) of people. Of these individuals, 47 did not respond to the question about falls and were excluded. Thus, 7,401 persons were included in the study. The majority of the sample reported for themselves (84.9% weighted percent) whereas 15.1% (weighted percent) used proxies. Reasons for proxy use included illness (23.3%), hearing and speech issues (24.1%), dementia or mental illness (25.7%), communication issues (12.2%), or other (42.2%).
Exposure
IADL stages represented the primary exposure of interest and were assigned based on the answers to a series of questions about the SP's experienced difficulty in using the telephone, managing money, preparing meals, doing light housework, shopping, and doing heavy housework. SPs or proxies were asked if they had no difficulty (rated as 0), some difficulty (rated as 1), a lot of difficulty (rated as 2), or were unable (rated as 3) to do each activity. There are five IADL stages that are assigned from 0 to IV, with higher numbers indicating greater limitations. Methods for stage development were empirically based on observed profiles in the data as adopted from the approach used to develop a staging system for functional independence.22,25,26 In addition, the five IADL stages were developed and labeled in accordance with the International Classification of Functioning, Disability and Health performance qualifiers27 to include no difficulty (IADL-0), mild difficulty (IADL-I), moderate difficulty (IADL-II), severe difficulty (IADL-III), and complete difficulty (IADL-IV) performing IADLs. Each IADL stage specifies the maximum difficulty that a person can have for each activity and still be assigned to the stage yielding a functional threshold across the 6 activities (Table 1).
Table 1. IADL stage threshold definitions.
|
Other Variables
Demographics included gender, race (white, black, and other), and age (70-74, 75-79, 80-84, and ≥85). Education was dichotomized as high school graduate or not. Living situation (lives alone, yes or no) was also included.
Perceived lack of home accessibility features was reported by the individual or proxy according to their belief that they needed one or more accessibility feature in the home, including ramps, kitchen modifications, widened doorways, elevators or stair glides, easy open doors, railings, alerting devices, accessible parking or drop-off sites, or other special features. Need for one or more feature was counted as yes.
Individuals or their proxies were asked about the presence of 13 health conditions grouped into 7 categories as reported by their doctor. These included the following conditions: stroke, cardiopulmonary disorder (heart attack, myocardial infarction, angina, other heart disease, bronchitis, emphysema, or asthma), diabetes, hypertension, cancer, arthritis, or osteoporosis. If the survey information was reported by a proxy because of poor memory or Alzheimer's disease, the individual was considered to have cognitive impairment. If during the past 12 months the individual had schizophrenia, paranoid disorder, bipolar disorder, or major depression lasting two or more weeks, they were considered as having a major psychiatric disorder.
Outcome Measure
The outcome of this study was history of falling in the previous year. SPs or proxies were asked if, during the prior 12 months, they had fallen. If the answer was yes, they were then asked whether they had fallen more than once.
Statistical Analyses
The LSOA II data was structured applying a multi-stage non-equal probability complex sample design. In our analysis, we used the Final Annual SOA II Weight provided in the LSOA II public-use data files which accounts for the unequal probability of sampling, adjustment for non-response, and a post-stratification adjustment. After weighting, the sample is distributed similar to the population control counts from July 1, 1994 in age, gender, and race.
The prevalence of demographics, health status, and IADL stage were calculated as weighted proportions from the LSOA II data reflecting expected prevalence in the population. We looked at the unadjusted associations between demographics, health status, and IADL stage according to a history of falling in the previous year. We reported un-weighted sample sizes and weighted proportions of these estimates.
An ordinal logistic regression assuming proportional odds was first attempted since the outcome, history of falling in the previous year, has multiple ordered levels, i.e., no falls, one fall, or multiple falls. We used the Brant test to validate the proportional odds assumption. We got a significant test which provided evidence that the proportional odds assumption was violated 34. Thus, we then fit a multinomial logistic regression model. The selection of the covariates in the model was hypothesis driven. IADL stage was the primary exposure in the model. The other variables as described above were entered into the model in which the relative risk of falling once (and falling multiple times) was modeled, with relative risk of falling once (and falling multiple times) defined as the probability of falling once divided by the probability of having no falls. The multinomial logistic regression model reports relative risk ratios (RRRs) and 95% confidence intervals (CIs). The p-values are two-tailed where p<0.05 was considered statistically significant.
To obtain the correct point and variance for population estimates, all analyses took into account clustering, survey weights, and stratification. Statistical analyses were performed with Stata/MP version 11.0 (StataCorp, College Station, TX) using the proper statements to account for the complex sampling design. For example, svyset command in STATA can specify variables for clustering, weight, and stratification. Svy:mlogic was then used to do multinomial logistic regression35.
Results
Among the 7,401 community-dwelling persons included in this study, the majority were female (63.0%), white (88.8%), and between the ages of 70 to 74 years old (49.6%). Approximately one-third lived alone with the remaining respondents stating that they lived with others (Table 2). The majority of the respondents were at IADL- 0 (69.9%, N=5,151); the remainder was distributed among the IADL stages as follows: 1,238 (16.7%) at IADL- I; 462 (6.1%) at IADL- II; 437 (5.8%) at IADL- III; and 113 (1.5%) at IADL- IV. There were 5,925 (80.0%) respondents who reported not falling within the 12 months prior to the time they were interviewed. A total of 814 (11.0%) respondents reported fallen once while 662 (9.0%) reported multiple falls.
Table 2. History of falling in the past 12 months in community-dwelling persons 70 years or oldera.
| Number of Falls | |||||
|---|---|---|---|---|---|
|
| |||||
| Predictor Variables | N (%) (N=7,401) | None (N=5,925, 80.0%) | 1 (N=814, 11.0%) | >1 (N=662, 9.0%) | p-value |
|
| |||||
| IADL stage | |||||
| 0: No difficulty | 5151 (69.9) | 4415 (85.6) | 482 (9.4) | 254 (5.0) | <0.001 |
| I: Mild difficulty | 1238 (16.7) | 901 (72.9) | 170 (13.9) | 167 (13.3) | |
| II: Moderate difficulty | 462 (6.1) | 270 (57.9) | 83 (18.5) | 109 (23.6) | |
| III: Severe difficulty | 437 (5.8) | 262 (58.2) | 71 (17.5) | 104 (24.3) | |
| IV: Complete difficulty | 113 (1.5) | 77 (68.3) | 8 (5.9) | 28 (25.8) | |
|
| |||||
| Gender | |||||
| Male | 2705 (37.0) | 2261 (84.0) | 224 (8.1) | 220 (8.0) | <0.001 |
| Female | 4696 (63.0) | 3664 (77.6) | 590 (12.9) | 442 (9.5) | |
|
| |||||
| Race | |||||
| White | 6365 (88.8) | 5072 (79.8) | 726 (11.4) | 567 (8.9) | 0.225 |
| Black | 762 (7.3) | 627 (80.4) | 67 (9.4) | 68 (10.2) | |
| Other | 274 (3.9) | 226 (83.6) | 21 (7.6) | 27 (8.8) | |
|
| |||||
| Age, yrs | |||||
| 70-74 | 3630 (49.6) | 3024 (82.9) | 355 (9.9) | 251 (7.1) | <0.001 |
| 75-79 | 2021 (27.4) | 1623 (80.3) | 236 (11.5) | 162 (8.1) | |
| 80-84 | 1146 (15.1) | 866 (75.6) | 137 (12.2) | 143 (12.2) | |
| >85 | 604 (7.9) | 412 (68.0) | 86 (14.9) | 106 (17.1) | |
|
| |||||
| High school graduate | |||||
| Yes | 4364 (60.0) | 3519 (80.9) | 492 (11.2) | 353 (7.9) | 0.002 |
| No | 3037 (40.0) | 2406 (78.6) | 322 (10.9) | 309 (10.5) | |
|
| |||||
| Lives alone | |||||
| Yes | 2728 (36.7) | 2077 (75.9) | 350 (13.0) | 301 (11.1) | <0.001 |
| No | 4673 (63.3) | 3848 (82.3) | 464 (10.0) | 361 (7.7) | |
|
| |||||
| Lack of home accessibility features | |||||
| Yes | 436 (5.8) | 262 (60.2) | 68 (16.0) | 106 (23.8) | <0.001 |
| No | 6965 (94.2) | 5663 (81.2) | 746 (10.8) | 556 (8.0) | |
|
| |||||
| Stroke | |||||
| Yes | 553 (7.4) | 353 (63.6) | 83 (15.0) | 117 (21.4) | <0.001 |
| No | 6848 (92.6) | 5572 (81.3) | 731 (10.8) | 545 (8.0) | |
|
| |||||
| Cardiopulmonary | |||||
| Yes | 2387 (32.4) | 1796 (75.1) | 299 (12.9) | 292 (12.1) | <0.001 |
| No | 5014 (67.6) | 4129 (82.3) | 515 (10.2) | 370 (7.5) | |
|
| |||||
| Diabetes | |||||
| Yes | 870 (11.5) | 634 (72.1) | 109 (12.7) | 127 (15.2) | <0.001 |
| No | 6531 (88.5) | 5291 (18.0) | 705 (10.9) | 535 (8.1) | |
|
| |||||
| Hypertension | |||||
| Yes | 3215 (42.8) | 2486 (76.9) | 392 (12.4) | 337 (10.7) | <0.001 |
| No | 4186 (57.2) | 3439 (82.2) | 422 (10.1) | 325 (7.7) | |
|
| |||||
| Cancer | |||||
| Yes | 1201 (16.6) | 921 (77.4) | 134 (11.0) | 146 (11.6) | 0.002 |
| No | 6200 (83.4) | 5004 (80.5) | 680 (11.1) | 516 (8.4) | |
|
| |||||
| Arthritis | |||||
| Yes | 3375 (45.5) | 2511 (74.0) | 454 (13.7) | 410 (12.2) | <0.001 |
| No | 4026 (54.5) | 3414 (84.9) | 360 (8.9) | 252 (6.2) | |
|
| |||||
| Osteoporosis | |||||
| Yes | 541 (7.7) | 367 (68.0) | 97 (18.0) | 77 (14.0) | <0.001 |
| No | 6860 (92.3) | 5558 (80.9) | 717 (10.5) | 585 (8.5) | |
|
| |||||
| Cognitive impairment | |||||
| Yes | 298 (3.9) | 179 (58.6) | 44 (14.9) | 75 (26.5) | <0.001 |
| No | 7103 (96.1) | 5746 (80.8) | 770 (10.9) | 587 (8.2) | |
|
| |||||
| Major psychiatric disorders | |||||
| Yes | 67 (0.9) | 46 (65.6) | 11 (17.1) | 10 (17.3) | 0.014 |
| No | 7334 (99.1) | 5879 (80.1) | 803 (11.0) | 652 (8.9) | |
Sample sizes (Ns) are un-weighted and the proportions (%'s) are weighted. The first column is N (sample weighted column %). The remaining 3 columns are N (sample weighted row %).
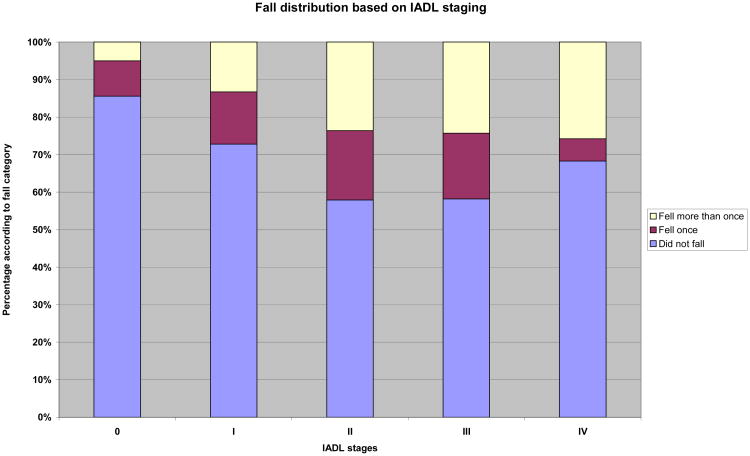
After sample weights were applied, it was found that among those at IADL-0, 85.6% (N=4,415) reported no falls, 9.4% (N=482) reported falling once, and 5.0% (N=254) reported falling more than once. People with moderate difficulties at IADL-II demonstrated the highest likelihoods of falling once: 57.9% (N=270) claimed they did not fall while 18.5% (N=83) fell once, and 23.6% (N=109) fell multiple times. While the percentage who fell once increased from IADL-0 to IADL-II, it stabilized at IADL-III then declined at IADL-IV. Overall, those at IADL-IV were less likely to fall than those at IADL-0 but those who did fall at IADL-IV tended to fall multiple times. Rather than declining at the most limited stage as seen amongst respondents who fell once, the distribution amongst those who fell more than once formed a plateau at IADL-II, -III, and −IV. Figure 1 shows this distribution.
Figure 1.
The percentage of respondents who recalled falling once and more than once according to IADL stages-0, -I, -II, -III, and −IV.
Gender, age, education, living situation, perceived lack of home accessibility features, a history of stroke, cardiopulmonary disorders, diabetes, hypertension, cancer, arthritis, osteoporosis, cognitive impairment, and psychiatric disorders were all significantly associated with increased likelihood of falls history. Of particular note, 11.1% of those who lived alone compared to 7.7% who lived with family fell multiple times (p<0.001). Remarkably, 23.8% of those who perceived unmet needs for accessibility features in their homes fell multiple times compared to 8.0% who did not (p<0.001).
Table 3 shows the associations of each covariate and history of falling adjusting all covariates in the model. Compared to respondents with no IADL limitations, those at stage II had a RRR of 2.0 (95% CI 1.5-2.6) and those at stage III had a RRR of 1.8 (95% CI, 1.3-2.6) of falling once. Those with mild limitations at IADL stage I and those with severe limitations at IADL stage IV did not have relative risk ratios of falling once that differed significantly from those with no limitations. The RRR of falling more than once was 2.1 (95% CI, 1.7-2.6), 4.0 (95% CI, 3.0-5.3), 3.7 (95% CI, 2.8-5.0), and 2.7 (95% CI, 1.5-4.9) for IADL stage I, II, III, and IV, respectively, compared to those with no IADL limitations.
Table 3.
The adjusted association between IADL stage limitation and history of falling.
| Predictor Variables | Number of Falls | |||
|---|---|---|---|---|
|
| ||||
| Fall 1 time (N=814) | Fall > 1 time (N=662) | |||
|
| ||||
| IADL stage (ref: stage 0) | <.0001 | <.0001 | ||
| Stage I | 1.2 (1.0-1.6) | .07 | 2.1 (1.7-2.6) | <.0001 |
| Stage II | 2.0 (1.5-2.6) | <.0001 | 4.0 (3.0-5.3) | <.0001 |
| Stage III | 1.8 (1.3-2.6) | <.01 | 3.7 (2.8-5.0) | <.0001 |
| Stage IV | 0.5 (0.2-1.1) | .09 | 2.7 (1.5-4.9) | <.01 |
|
| ||||
| Gender (ref: male) | ||||
| Female | 1.4 (1.2-1.7) | <.01 | 0.9 (0.7-1.1) | .39 |
|
| ||||
| Race (ref: white) | .09 | .72 | ||
| Black | 0.8 (0.5-1.0) | .07 | 0.9 (0.6-1.2) | .42 |
| Other | 0.7 (0.4-1.1) | .13 | 1.0 (0.6-1.6) | .92 |
|
| ||||
| Age, yrs (ref: 70-74) | .12 | .04 | ||
| 75-79 | 1.1 (0.9-1.4) | .17 | 1.0 (0.8-1.3) | .83 |
| 80-84 | 1.2 (0.9-1.5) | .23 | 1.3 (1.0-1.8) | .05 |
| >85 | 1.4 (1.0-1.8) | .03 | 1.5 (1.1-2.1) | .01 |
|
| ||||
| High school graduate (ref: no) | ||||
| Yes | 1.1 (1.0-1.3) | .12 | 1.0 (0.8-1.2) | .95 |
|
| ||||
| Lives alone (ref: no) | ||||
| Yes | 1.2 (1.0-1.4) | .07 | 1.4 (1.1-1.7) | <.01 |
|
| ||||
| Lack of home accessibility features (ref: no) | ||||
| Yes | 1.3 (0.9-1.9) | .11 | 1.7 (1.3-2.3) | <.0001 |
|
| ||||
| Stroke (ref: no) | ||||
| Yes | 1.4 (1.1-1.9) | .02 | 1.8 (1.3-2.4) | <.0001 |
|
| ||||
| Cardiopulmonary (ref: no) | ||||
| Yes | 1.1 (0.9-1.3) | .21 | 1.1 (0.9-1.3) | .36 |
|
| ||||
| Diabetes (ref: no) | ||||
| Yes | 1.2 (0.9-1.5) | .22 | 1.5 (1.2-1.9) | <.01 |
|
| ||||
| Hypertension (ref: no) | ||||
| Yes | 1.1 (0.9-1.3) | .33 | 1.1 (0.9-1.3) | .31 |
|
| ||||
| Cancer (ref: no) | ||||
| Yes | 1.0 (0.8-1.2) | .86 | 1.3 (1.1-1.6) | .01 |
|
| ||||
| Arthritis (ref: no) | ||||
| Yes | 1.4 (1.2-1.7) | <.0001 | 1.6 (1.3-2.0) | <.0001 |
|
| ||||
| Osteoporosis (ref: no) | ||||
| Yes | 1.4 (1.1-1.8) | .02 | 1.2 (0.9-1.6) | .24 |
|
| ||||
| Cognitive impairment (ref: no) | ||||
| Yes | 1.4 (0.9-2.1) | .15 | 1.6 (1.1-2.4) | .01 |
|
| ||||
| Major psychiatric disorders (ref: no) | ||||
| Yes | 1.6 (0.8-3.1) | .18 | 1.3 (0.6-2.8) | .48 |
After adjusting for IADL stage and all other variables, females compared to males, those 85 years of age or older compared to those younger than 75, and those with strokes, arthritis, or osteoporosis had a higher relative risk of falling once. Those 80 years or older compared to those younger than 75, living alone, perceiving lack of home accessibility features, and those who had strokes, diabetes, cancer, arthritis, or cognitive impairments had a relatively higher relative risk of falling more than once.
Discussion
According to findings from this population-based study and as reported previously,20 statistically and clinically significant associations were found between IADL stages and history of falling once and multiple times among the sampled elderly community-dwelling persons. These associations, initially expected to be ordered turned out to be more complex than anticipated since associations with history of falling were not ordered and non-linear for both activity limitation staging components. There were dramatic differences between falling once and multiple times within the IADL stages. Moreover, associations with falling once and multiple times showed both similarities and differences across the ADL and IADL staging components. These differences provide new insights about how experienced limitations in functional activities appear to differ with regards to impact on falling risk.
The adjusted relative risk ratio of having a history of falling once was increased at IADL-II compared to IADL-0, declined slightly at IADL-III then showed a marked drop off at the highest stage of limitation, IADL-IV. There was a stronger independent association between IADL stage and risks of multiple falls than for single falls, with risks significantly higher for people with IADL limitations than for those without. By the nature of defining functional thresholds, ADL and IADL stages take into account severity of limitation in skills basic to independent self-care and community living, respectively. IADLs are generally recognized as more complex, requiring both physical and cognitive abilities and typically become limited before ADLs.28,30 Thus, some people with complete IADL limitations may still be able to perform some ADLs which places them at an elevated risk of falling multiple times as they continue to attempt self-care activities.
Both in the unadjusted and adjusted patterns, IADL-II, which refers to moderate IADL limitation, appears to be an important threshold since at that stage people have the highest likelihood of having a history of falling both once and multiple times. Then associations diverge between the two types of falls histories suggesting that the factors that trigger a single fall versus multiple falls may differ particularly at the higher stages of IADL limitation.
To our knowledge, this is the first presentation of these kinds of non-linear associations between IADL stage and of the distinctions between histories of falling once and multiple times. The associated patterns between functional status and falling and distinctions between falling once and multiple times seem to reinforce the complicated nature of human behavior and functionally induced opportunities for falling. We believe falls risk assessment requires a broader assessment approach because it must occur relative to the environments within people live along with full appreciation of the presence of basic human needs that drive the performance of functional activities. It is logical that by IADL-III people were less likely to be mobile and may not be venturing out from their homes into their community environments to perform IADLs thus decreasing their exposure to falling opportunities and therefore probability of falling. But they can still perform at least one IADL so their likelihood of falling inevitably remains high. By IADL-IV, all IADLs are difficult and most people will need to be living in circumstances where they no longer attempt these functional tasks, thus dramatically lowering overall risk.
This work has limitations. Recall bias can occur particularly for questions which enquire about events spanning a year or more from the time of the interview. Thus, there may be falsely low incidence with reporting falls. Under-reporting, due to recall bias, however; will likely be greatest in non-serious falls of less significance.31 The answers, provided by self or proxy to questions about IADL functioning, may differ from answers provided by clinicians. Yet, the use of self- or proxy-reported functioning reflects a general movement towards patient-reported outcome measures (PROs).32 Missing data on IADLs occurred in just over 20% of persons, primarily among those for whom one or more IADLs were not relevant because someone else already in their lives normally performed the activities. Thus, findings cannot be considered relevant to the entire elderly US population. The data was interpreted from a period of time that differs from the current timeframe, however; there has been no data collected more recently that addresses important elements related to ADLs and IADLs making it one of the most comprehensive data sources available for addressing the implication of different functional states. Federal civil rights laws that ensure equal opportunity and access for people with disabilities were in place prior to the data collection period with no further additional laws added since 1996.33 Amendments have been made to these laws recently, however; it is not clear how the changes would have affected those with perceived lack of home accessibility features. Finally, it is important to recognize the limitations of the cross-sectional design of this study. Direction of causality is unknown. A fall could have occurred previously while the individual was at a more functional IADL stage and been a primary trigger of the individual transitioning to a higher (currently stated) stage of IADL limitation. Alternatively, the individual's current stated stage could have contributed to the falling episode.
Generally, a single fall in the previous year can be a random event. However, the multiple falls pattern may be most clinically telling since it suggests systemic or repeating problems. It is clinically significant that history of falling more than once more than doubled at IADL-I compared to IADL-0, nearly doubled again at IADL-II compared to IADL-I then began to decline. It is also telling that those at IADL-IV who fall tended to fall multiple times. A history of multiple falls is worrisome particularly among those at the highest stages of IADL limitation as it may suggest unmet needs associated with patients' living circumstances, inaccessible home features, or an insufficient support network. Although this retrospective analysis was based on surveying people about their falling history, we believe that the distinct stage patterns of risk may prove useful in patient screening and in understanding why certain groups of community living older people fall. Further studies should be conducted to determine if IADL staging can be used as a falls risk assessment tool and possibly as a mechanism to better explain important patient-centered outcomes such as falling and their consequences. Also, our findings highlight that in designing further surveys and studies, it will be important to focus more on persons' perceived lack of home accessibility features and home accessibility modifications already present in the home as these are elements that can potentially be modified.
Acknowledgments
The research for this manuscript was supported in part by the National Institute of Aging (NIA) of the National Institutes of Health (AG032420-01A1, R01AG040105-01A1, and R01 AG 040115-01A1).
We certify that no party having a direct interest in the results of the research supporting this article has or will confer a benefit on us or on any organization with which we are associated AND, if applicable, we certify that all financial and material support for this research (i.e., NIH grants) and work are clearly identified in the title page of the manuscript. The views of the authors do not necessarily reflect those of the funding organizations. The analyses, interpretations, and conclusions reached are those of the authors and not those of the National Center for Health Statistics (NCHS), which is responsible only for the initial data.
Footnotes
Disclosures: Parts of the material in the manuscript were presented at the 2011 AAPM&R Annual Assembly, November 17-20, 2012 in Orlando, Florida.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Department of Health and Human Services, Administration of Aging. Aging Statistics. [Accessed July 23, 2012]; http://www.aoa.gov/aoaroot/aging_statistics/index.aspx.
- 2.Davis JC, Robertson MC, Ashe MC, Liu-Ambrose T, Khan KM, Marra CA. International comparison of falls in older adults living in the community: a systematic review. Osteoporos Int. 2010;21:1295–1306. doi: 10.1007/s00198-009-1162-0. [DOI] [PubMed] [Google Scholar]
- 3.Tinetti ME, Speechley M, Ginter S. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319(26):1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 4.Vellas BJ, Wayne SJ, Garry PJ, Baumgartner RN. A two-year longitudinal study of falls in 482 community-dwelling elderly adults. Journal of Gerontology: Medical Sciences. 1998;53A(4):M264–M274. doi: 10.1093/gerona/53a.4.m264. [DOI] [PubMed] [Google Scholar]
- 5.Quandt SA, Stafford JM, Bell RA, Smith SL, Snively BM, Arcury TA. Predictors of falls in a multiethnic population of rural adults with diabetes. Journal of Gerontology: Medical Sciences. 2006;61A(4):394–398. doi: 10.1093/gerona/61.4.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fuller GF. Falls in the elderly. Am Fam Physician. 2000;61(7):2159–2168. [PubMed] [Google Scholar]
- 7.Chu LW, Chi I, Chiu AYY. Incidence and predictors of falls in the Chinese elderly. Ann Acad Med Singapore. 2005;34:60–72. [PubMed] [Google Scholar]
- 8.Sudip N, Parsons S, Cryer C, Underwood M, Rashbrook E, Carter Y, Eldridge S, Close J, Skelton D, Taylor S, Feder G. Development and preliminary examination of the predictive validity of the Falls Risk Assessment Tool (FRAT) for use in primary care. Journal of Public Health. 2004;26(2):138–143. doi: 10.1093/pubmed/fdh132. [DOI] [PubMed] [Google Scholar]
- 9.Tiedemann A, Lord SR, Sherrington C. The development and validation of a brief performance-based fall risk assessment tool for use in primary care. J Gerontol A Biol Sci Med Sci. 2010 Aug;65(8):896–903. doi: 10.1093/gerona/glq067. [DOI] [PubMed] [Google Scholar]
- 10.Renfro MO, Fehrer S. Multifactorial screening for fall risk in community-dwelling older adults in the primary care office: development of the fall risk assessment & screening tool. J Geriatr Phys Ther. 2011;34:174–183. doi: 10.1519/JPT.0b013e31820e4855. [DOI] [PubMed] [Google Scholar]
- 11.van Henbroek PB, van Dijk N, van Breda GF, Scheffer AC, van der Cammen TJ, Lips P, Goslings JC, de Rooij SE. The CAREFALL triage instrument identifying risk factors for recurrent falls in elderly patients. American Journal of Emergency Medicine. 2009;27:23–36. doi: 10.1016/j.ajem.2008.01.029. [DOI] [PubMed] [Google Scholar]
- 12.Russell MA, Hill KD, Day LM, Blackberry I, Gurrin LC, Dharmage SC. Development of the falls risk for older people in the community (FROP-Com) screening tool. Age and Ageing. 2009;38:40–46. doi: 10.1093/ageing/afn196. [DOI] [PubMed] [Google Scholar]
- 13.Lamb SE, McCabe C, Becker C, Fried LP, Guralnik JM. The optimal sequence and selection of screening test items to predict fall risk in older disabled women: the women's health and aging study. Journal of Gerontology: Medical Sciences. 2008;63A(10):1082–1088. doi: 10.1093/gerona/63.10.1082. [DOI] [PubMed] [Google Scholar]
- 14.Panel on Prevention of Falls in Older Persons, American Geriatrics Society and British Geriatrics Society. Summary of the updated American geriatrics society/British geriatrics society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59:148–157. doi: 10.1111/j.1532-5415.2010.03234.x. [DOI] [PubMed] [Google Scholar]
- 15.Bloch F, Thibaud M, Dugué B, Brèque C, Rigaud AS, Kemoun G. Episodes of falling among elderly people: a systematic review and meta-analysis of social and demographic pre-disposing characteristics. Clinics. 2010;65(9):895–903. doi: 10.1590/S1807-59322010000900013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Activities of daily living, definition of Stedman's medical dictionary. 28th. Lippincott Williams and Wilkins; copyrights 2006. [Google Scholar]
- 17.Bookman A, Harrington M, Pass L, Reisner E. Family caregiver handbook: Finding elder care resources in Massachusetts. Cambridge, MA: Massachusetts Institute of Technology; 2007. [Google Scholar]
- 18.Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies of illness in the aged. The index of ADL: a standardized measure of biological and psychosocial function. JAMA. 1963;185(12):914–919. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- 19.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. The Gerontologist. 1969;9(3):179–186. [PubMed] [Google Scholar]
- 20.Henry-Sanchez JT, et al. Do elderly people at more severe activity of daily living limitation stages fall more? Am J of Phys Med Rehabil. 2012;91:601–610. doi: 10.1097/PHM.0b013e31825596af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Njegovan V, Man-Son-Hing M, Mitchell SL, Molnar FJ. The hierarchy of functional loss associated with cognitive decline in older persons. Journal of Gerontology. 2001;56A(10):M638–M643. doi: 10.1093/gerona/56.10.m638. [DOI] [PubMed] [Google Scholar]
- 22.Stineman MG, et al. Staging activity limitation and participation restriction in elderly community-dwelling persons according to difficulties in self-care and domestic life functioning. Am J Phys Med Rehabil. 2012;91:126–140. doi: 10.1097/PHM.0b013e318241200d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stineman MG, Streim JE. The biopsycho-ecological paradigm: a foundational theory for medicine. PM&R. 2010;2(11):1035–1045. doi: 10.1016/j.pmrj.2010.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.National Center for Health Statistics (1998) Data File Documentation-National Health Interview Second Supplement on Aging-1994 (Machine Readable Data File and Documentation) Hyattsville, MD: National Center for Health Statistics; 1998. [Google Scholar]
- 25.Stineman MG, Ross RN, Fiedler R, et al. Functional independence staging: conceptual foundation, face validity, and empirical derivation. Arch Phys Med Rehabil. 2003;84:29–37. doi: 10.1053/apmr.2003.50061. [DOI] [PubMed] [Google Scholar]
- 26.Stineman MG, Ross RN, Fiedler R, et al. Staging functional independence validity and applications. Arch Phys Med Rehabil. 2003;84:38–45. doi: 10.1053/apmr.2003.50060. [DOI] [PubMed] [Google Scholar]
- 27.International Classification of Functioning, Disability, and Health (ICF), World Health Organization. [Accessed September 4, 2012]; www.who.int/classifications/icf/en/
- 28.Ng TP, Niti M, Chiam PC, Kua EH. Physical and cognitive domains of the Instrumental Activities of Daily Living: validation in a multiethnic population of Asian older adults. J Gerontol A Biol Sci Med Sci. 2006;61(7):726–735. doi: 10.1093/gerona/61.7.726. [DOI] [PubMed] [Google Scholar]
- 29.Woods SP, Weinborn M, Velnoweth A, Rooney A, Bucks RS. Memory for intentions is uniquely associated with instrumental activities of daily living in healthy older adults. J Int Neuropsychol Soc. 2012;18(1):134–138. doi: 10.1017/S1355617711001263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Spector WD, Katz S, Murphy JB, Fulton JP. The hierarchical relationship between activities of daily living and instrumental activities of daily living. J Chronic Dis. 1987;40(6):481–9. doi: 10.1016/0021-9681(87)90004-x. [DOI] [PubMed] [Google Scholar]
- 31.Lee Y. The predictive value of self assessed general, physical, and mental health on functional decline and mortality in older adults. J Epidemiol Community Health. 2000;54(2):123–9. doi: 10.1136/jech.54.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Carle AC, Cella D, Cai L, Choi SW, Crane PK, Curtis SM, Gruhl J, Lai JS, Mukherjee S, Reise SP, Teresi JA, Thissen D, Wu EJ, Hays RD. Advancing PROMIS's methodology: results of the Third Patient-Reported Outcomes Measurement Information System (PROMIS(([REGISTERED])) Psychometric Summit. Expert Rev Pharmacoecon & Outcomes Res. 2011;11:677–84. doi: 10.1586/erp.11.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Americans with Disabilities Act Title II Regulations. [Accessed June 11, 2013]; http://www.asa.gov/regs2010/titleII_2010/titleII_2010_regulations.pdf.
- 34.Stata Data Analysis Examples: Ordered Logistic Regression Stata 12 Institute for Digital Research and Education. [Accessed Aug 8, 2013.]; http://www.ats.ucla.edu/stat/stata/dae/ologit.htm.
- 35.StataCorp. Stata 13 Base Reference Manual. College Station, TX: Stata Press; 2013. Survey- Introduction to Survey Commands. http://www.stata.com/manuals13/svysurvey.pdf. [Google Scholar]